The authors describe a technique that allows suture of the abdominal fascia at sites using a transcurtaneous approach and standard surgical instruments.
Keywords: Laparoscopic surgery, Port-site closure, Trocar-site hernia
Abstract
Background and Objectives:
Fascial closure of port sites represents a challenging issue in laparoscopic surgery. The aim of this article is to introduce a procedure that allows the safe suturing of the abdominal fascia in these wounds.
Methods:
We herein describe a simple technique for fascial closure after laparoscopy using a transcutaneous approach and standard surgical instruments for suture.
Results:
The method was used in 34 patients with no intraoperative incidents and no port-site hernias during a mean follow-up of 23.9 months (median 20.5, range 5 to 47).
Conclusion:
The procedure is easy to perform, safe, fast, and inexpensive.
INTRODUCTION
New technical challenges have emerged since the introduction of the laparoscopic approach in surgery. One of these is fascial closure at port sites, which is necessary especially when large trocars are used or after dilation of a port site for organ extraction (ie, gallbladder, appendix). New developments, such as single-port laparoscopic surgery, and the need for small esthetic incisions render fascial closure a current issue. Since the first report of herniation at a trocar site after laparoscopy,1 many techniques and devices have been introduced into practice to minimize the risk of port-site complications, which occur in 1% to 6% of cases.2,3 The standard closure technique for fascia at the port site through a small skin incision can be tricky and frustrating, often requiring blind suturing of the fascial defect (with consequent risk of incomplete suture and lesions of intraperitoneal organs) or larger skin incisions.
We herein propose a new method for safe suturing of the abdominal fascia in port-site wounds.
MATERIALS AND METHODS
The surgical procedure may be performed in 1 step or in 2 steps.
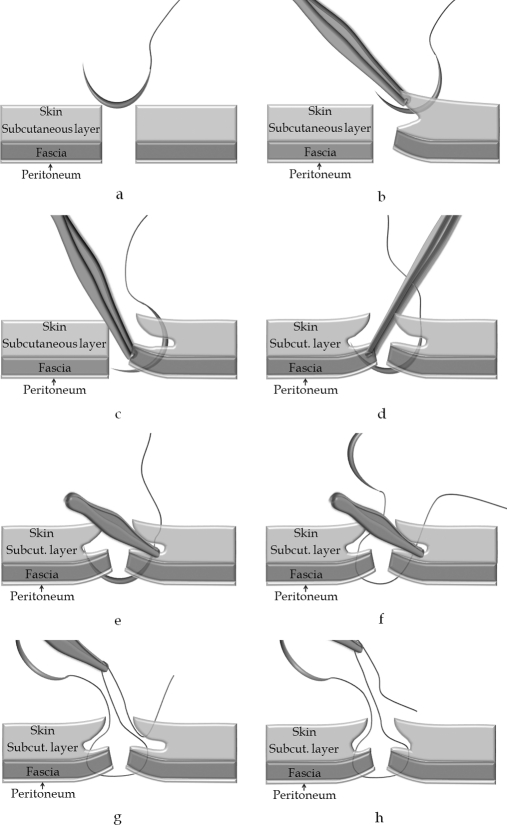
The 1-step technique (Figure 1) is performed as follows:
The needle is passed through the skin and part of the adjacent subcutaneous layer, a few centimeters away from the wound margin, and exits into the wound (Figure 1b).
While the fascia and peritoneum are pulled up with a tissue forceps, the needle is passed through them on both sides of the wound, one at a time (Figure 1c and 1d).
The needle is then grasped with the tissue forceps in the portion exposed between the skin and the fascia (Figure 1e).
The needle is pulled out of the wound while the tissue forceps is kept in place (Figure 1f).
The tissue forceps is pulled out from the wound along with the grasped surgical thread (Figures 1g and 1h).
Figure 1.
One-step technique for fascial closure.
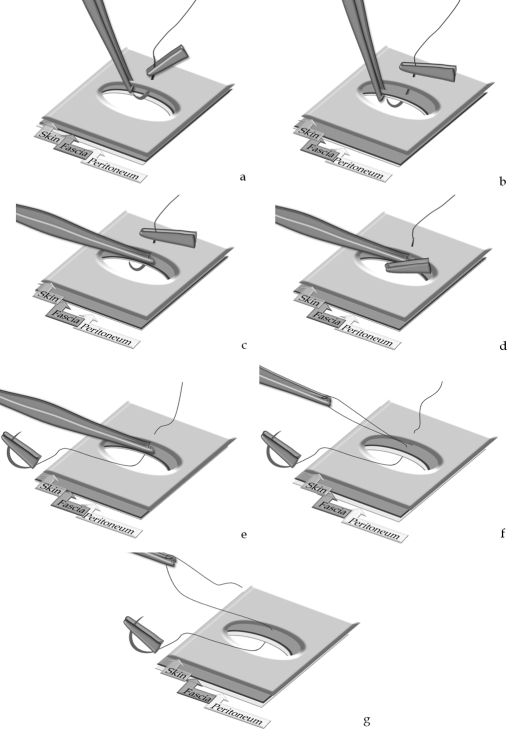
The 2-step technique (Figure 2) is performed as follows:
The needle is passed through the skin and part of the subcutaneous layer, a few centimeters away from the wound margin, and exits into the wound (Figure 2a).
While the fascia and peritoneum are pulled up with a tissue forceps, the needle is passed through them, one at a time (Figure 2b).
The needle is then grasped with the tissue forceps in the exposed portion between the skin and fascia (Figures 2c and 2d).
The needle is pulled out of the wound while the tissue forceps is kept in place (Figure 2e).
The tissue forceps is pulled out along with the grasped surgical thread (Figures 2f and 2g).
The same steps are repeated for the other side of the wound, but in an inside-out direction.
Figure 2.
Two-step technique for fascial closure.
The sequence of transcutaneous and transfascial passages of the needle allows the subsequent withdrawal of the surgical thread from the superficial plane (skin and part of the adjacent subcutaneous layer) leaving it only at the level of the deep plane (fascia and peritoneum). This transcutaneous approach enables the needle to enter the fascia and peritoneum in an acute angle (Figure 1c), which is safer than the standard technique.
Such an approach assures optimal access to the fascial plane, otherwise impossible to obtain by using the common retraction maneuvers. The method allows suturing the fascia close to the angles of incision, which may be unfeasible if the standard technique is used; consequently, 2 lateral sutures may be placed instead of a medial one, which is usually done when the standard technique is used. Additionally, it allows the use of larger needles that are easier to manipulate, making the suturing maneuvers safer and faster.
RESULTS
The method was used in 34 patients with no intraoperative incidents; in 31 of 34 patients (91.2%) 2 lateral sutures were made (instead of a medial one). No port-site hernias occurred during a mean follow-up of 23.9 months (median, 20.5; range, 4 to 50) consisting of clinical examination and ultrasound (when an incisional hernia was clinically suspected). The median body weight was 80kg (mean, 82.9; range, 59 to 121), and the median body mass index was 27kg/m2 (mean, 26.3; range, 22.5 to 37.8).
DISCUSSION
Failure to adequately suture the fascial defect, infection, or suture disruption may lead to an incisional hernia or to ascitic fluid leakage in case of cirrhotic patients.4
Trocar diameter and design, preexisting fascial defects, certain surgical procedures and patient-related factors have been identified as risk factors for port-site hernias.2
Incisional hernias on trocar sites can occur even with incisions as small as 3mm.5 Although some authors avoid fascial closure by using special trocars,6,7 closing the 10- and 12-mm port sites is recommended.8
Beside the classical hand-sutured technique, 29 original methods have been described for fascial closure.9,10
The port-closure techniques were classified by Shaher9 into 3 groups: (a) techniques that use assistance from inside the abdomen (requiring 2 additional ports), (b) techniques that use extracorporeal assistance (requiring 1 additional port), and (c) closure techniques that can be performed with or without visualization (without additional ports). As disadvantages, the majority of these techniques need special devices; some of them are time consuming, or need assistance from inside the abdomen, or are both time consuming and need assistance.
The technique herein described can be listed in the third group according to Shaher's classification. We could not find any article in the literature that describes a similar technique. Its principle may seem odd, as all the other techniques using common surgical instruments aim to hold back the skin and subcutaneous tissue of the surgical wound as much as possible to better expose the fascia and to allow access of the instruments to the fascial level. On the contrary, this method involves minimal retraction of the surgical wound by using transcutaneous access of the needle. The final result is an optimal suture of the fascia through a minimal skin incision, allowing the placement of 2 sutures instead of one, thus assuring a stronger fascial closure. The method is also safer than the standard technique, because the tip of the needle enters the peritoneal cavity in an acute angle, rather than perpendicularly as occurs when the standard technique is used, reducing the risk of visceral injuries; in this way, the capacity of the needle to puncture intraperitoneal structure is reduced, the needle tip is better exposed during its course through the peritoneal cavity, and the intraperitoneal course of the needle is shortened, thus increasing the safety of the procedure.
We believe that this method may find other applications in surgery when sutures are placed in narrow spaces.
The fact that the series described in this article is relatively small may be considered a study drawback, because it is not statistically representative. However, the purpose of our study was not to prove the efficacy of this new technique by the statistical analysis of a large series. In our opinion, the efficacy of this new procedure in preventing port-site hernias is proven by the technique itself, which allows performance of an optimal fascial closure: large fascial margins included in the suture, and 2 sutures on small fascial wounds instead of only one (in comparison with the classical technique). Moreover, we considered that even the safety of this procedure did not need statistical confirmation, because the improved angle of the needle as it enters the peritoneal cavity passing through the fascia (an acute angle rather than a 90° angle) minimizes the risk of internal injuries. These technical advantages prove the efficacy of this new method for port-site closure.
CONCLUSION
This procedure is safe, easy to perform, virtually costless (uses common surgical instruments), and is not time consuming.
Contributor Information
Florin Botea, Liver Surgery Unit, 3rd Department of General Surgery, University of Milan, Faculty of Medicine, Humanitas Clinical Institute, Milan, Italy.; 2nd Clinic of Surgery, “Ovidius” University of Constanta, Faculty of Medicine, Emergency Clinical Hospital, Constanta, Romania.
Guido Torzilli, Liver Surgery Unit, 3rd Department of General Surgery, University of Milan, Faculty of Medicine, Humanitas Clinical Institute, Milan, Italy..
Vasile Sarbu, 2nd Clinic of Surgery, “Ovidius” University of Constanta, Faculty of Medicine, Emergency Clinical Hospital, Constanta, Romania..
References:
- 1. Fear R. Laparoscopy, a valuable aid in gynecologic diagnosis. Obstet Gynecol. 1968;31:297. [DOI] [PubMed] [Google Scholar]
- 2. Holzinger F, Klaiber C. Trocar-site hernias: a rare but potentially dangerous complication of laparoscopic surgery. Chirurg. 2002;73:899–904 [DOI] [PubMed] [Google Scholar]
- 3. Nezhat C, Nezhat F, Seidman DS, Nezhat C. Incisional hernias after operative laparoscopy. J Laparoendosc Adv Surg Tech A. 1997;7:111–115 [DOI] [PubMed] [Google Scholar]
- 4. Contarini O. Complication of trocar wounds. In: Meinero M, Melotti G, Mouret Ph. (eds). Laparoscopic surgery. Milano, Italy: Masson S.p.A; 1994:38–44 [Google Scholar]
- 5. Bergemann JL, Hibbert ML, Harkins G, Narvaez J, Asato A. Omental herniation through a 3-mm umbilical trocar site:unmasking a hidden umbilical hernia. J Laparoendosc Adv Surg Tech A. 2001;11:171–173 [DOI] [PubMed] [Google Scholar]
- 6. Rosenthal RJ, Szomstein S, Kennedy CI, Zundel N. Direct visual insertion of primary trocar and avoidance of fascial closure with laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2007;21(1):124–128 [DOI] [PubMed] [Google Scholar]
- 7. Liu CD, McFadden DW. Laparoscopic port sites do not require fascial closure when nonbladed trocars are used. Am Surg. 2000;66(9):853–854 [PubMed] [Google Scholar]
- 8. Di Lorenzo N, Coscarella G, Lirosi F, Gaspari A. Port-site closure: a new problem, an old device. JSLS. 2002;6(2):181–183 [PMC free article] [PubMed] [Google Scholar]
- 9. Shaher Z. Port closure techniques. Surg Endosc. 2007;21:1264–1274 [DOI] [PubMed] [Google Scholar]
- 10. Ng WT. A full review of port-closure techniques. Surg Endosc. 2007;21:1895–1897 [DOI] [PubMed] [Google Scholar]