Abstract
Until the development of the ileal pouch-anal anastomosis in the early 1980s, proctocolectomy with end ileostomy was the only definitive surgery for ulcerative colitis and colectomy with ileorectal anastomosis was the procedure of choice for affected patients who were reluctant to have a permanent ileostomy. Currently, ileal pouch-anal anastomosis is the most common procedure for patients with ulcerative colitis requiring surgical treatment. However, there is still a role for ileorectal anastomosis and proctocolectomy with end ileostomy for a selected group of patients. In this review, the authors summarize the current indications for ileorectal anastomosis and proctocolectomy with end ileostomy in patients with ulcerative colitis.
Keywords: Ulcerative colitis, proctocolectomy, ileostomy, ileorectal anastomosis
OVERVIEW
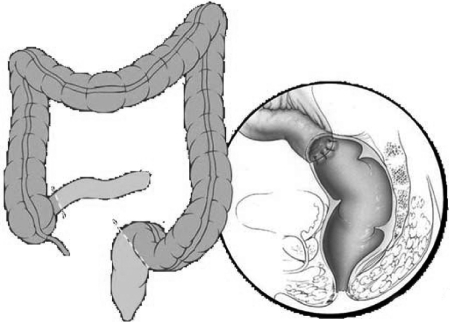
The main objectives of surgical treatment for ulcerative colitis are to alleviate symptoms and minimize cancer risk while avoiding a permanent stoma and preserving good bowel function. Until the development of the ileal pouch-anal anastomosis (IPAA) in the early 1980s, total proctocolectomy with end ileostomy (TPC) was the only definitive surgery for ulcerative colitis and colectomy with ileorectal anastomosis (IRA) (Fig. 1) was the procedure of choice for affected patients who needed surgery, but were reluctant to have a permanent ileostomy.1,2,3 Currently, IPAA is the most commonly performed operation for patients with ulcerative colitis because of the acceptable and durable functional outcomes associated with the avoidance of a permanent stoma. Consequently, IRA has been abandoned by many surgeons and TPC has become a safe alternative for selected patients who are not good candidates for IPAA. IPAA, however, carries its own risk, including postoperative portal vein thrombosis, pelvic sepsis causing pouch dysfunction, pelvic nerve damage leading to impaired sexual function, decreased fertility in women and pouchitis.4,5,6,7,8
Figure 1.
Ileorectal anastomosis. Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 1996–2010. All rights reserved.
ILEORECTAL ANASTOMOSIS
The good long-term outcomes for IPAA in major centers associated with symptoms related to a rigid, noncompliant rectum and the fear of rectal cancer explains the reluctance of many surgeons to perform IRA for ulcerative colitis. On the other hand, IRA consists of a less complex procedure with lower morbidity rates and it has been considered in highly selective patients with reasonable clinical results.9,10,11,12,13
Morbidity and Mortality
Prior studies have shown the safety of IRA for ulcerative colitis with low postoperative morbidity and mortality. Overall morbidity has ranged from 8 to 28% and overall mortality between 0 to 4%.9,10,11,12,13 The majority of published data has included mainly primary anastomosis with leak rates ranging from 2 to 7% and diverting ileostomy has been utilized according to surgeon discretion in selective cases.9,10,11 It is logical to believe that since IRA does not involve extensive pelvic dissection, unlike IPAA or TPC, the pelvic nerve damage is minimized, avoiding the sexual and urinary dysfunction. For the same reason, a better fertility rate in IRA patients may be expected when compared with IPAA. Therefore, colectomy with IRA could be offered to young female patients of childbearing age as an interim procedure until they constitute their families. However, better comparative studies are still necessary to better determine this benefit.
Rectal Function and Quality of Life
Rupert B. Turnbull described his IRA technique for patients with ulcerative colitis in 1959; he believed that preservation of grossly involved rectosigmoid portion was the main cause of IRA failure.1 Therefore, he recommended creating the anastomosis at 6 cm or less above the anterior peritoneal reflexion. He also observed a surprising improvement in the rectal inflammation during the first months after the IRA in some of his patients. As a matter of fact, patient selection is crucial to minimize the failure rate. Thus, patients with ulcerative colitis considered for an IRA are usually those presenting with a relatively spared rectum, good rectal compliance, and normal anal sphincters tone. These findings can be easily assessed during digital rectal examination and rigid/flexible proctoscopy. Furthermore, patients with poor sphincter function, severe rectal disease, and nondistensible rectum should not be candidates for an IRA. Although rectal sparing in ulcerative colitis is uncommon, this can be seen in a selective group of patients14 and among patients submitted to prior medical therapy. In these patients, some authors have shown acceptable long-term functional outcomes after an IRA. The reported probability of having a functioning IRA has ranged from 74 to 84% at 10 years and from 46 to 69% at 20 years.9,11,12,15 Table 1 summarizes the main clinical outcomes for IRA. In addition, one recent study from the Cleveland Clinic compared 22 IRA with 66 IPAA patients matched for age, gender, and follow-up time, including IRAs performed in the past 25 years. Similar functional outcomes have been demonstrated; IRA patients had more urgency affecting work and diet restrictions while IPAA patients had more night seepage and daytime bowel movements. Quality of life was comparable between the two groups using the Cleveland Clinic Global Quality of Life score (CCGQOL),9 suggesting that IRA is still a viable alternative in the IPAA era, if used selectively.
Table 1.
Clinical Outcomes after Ileorectal Anastomosis for Patients with Ulcerative Colitis
| # of Patients | Study Period | Follow-Up (Average Years) | BM/Day (Average) | Overall Failure Rate (%) | Overall Cancer Rate (%) | |
|---|---|---|---|---|---|---|
| da Luz Moreira et al9 | 86 | 1971–2006 | 9 | 6 | 53 | 8 |
| Pastore et al10 | 48 | 1974–1990 | 6.3 | 6 | 17 | 2 |
| Leijonmarck et al11 | 51 | 1955–1984 | 13 | 4 | 57 | 0 |
| Borjesson et al12 | 32 | 1997–2003 | 3.5 | 5.6 | 12 | 0 |
| Lepisto, Järvinen15 | 20 | 1978–2000 | 18 | — | 35 | 0 |
| Grundfestet al13 | 89 | 1957–1977 | 8 | — | 21 | 4.8 |
BM, bowel movements.
Fate of the Rectum
Despite previous studies showing that a significant number of patients will be able to keep their rectum after 10 years with an acceptable function and quality of life, IRA is not a definitive operation for many patients with ulcerative colitis. Therefore, some patients will require a completion proctectomy for different reasons. The main cause of rectal removal is recurrent proctitis refractive to medical treatment.9,10,11,12,15,16 Other reasons for completion proctectomy are rectal dysplasia, rectal cancer, and the development of Crohn disease in the rectum. The surgical options for patients requiring rectal resection are an IPAA, a Brooke ileostomy, or a continent ileostomy (Kock pouch). Nonetheless, IPAA can be accomplished in the majority of these patients after completion proctectomy preserving the bowel continuity and avoiding a permanent stoma.9
Cancer Risk and Surveillance
Basil C. Morson (1967) defined the concept of mucosal dysplasia as a premalignant state and its potential for carcinomatous transformation in ulcerative colitis.17 This important finding has permitted physicians to identify patients who may be at high risk of carcinoma. Johnson et al has confirmed that patients with dysplasia on rectal biopsy following IRA were at significantly greater risk of the development of rectal adenocarcinoma than those without.18 The rates of dysplasia and cancer in patients with ulcerative colitis increases with time and leaving the rectum in place contributes to maintaining their potential risk. The cumulative probability of rectal dysplasia can increase from 9% at 10 years to 25% at 20 years.9 The overall incidence of rectal cancer after an IRA varies in the literature according to follow-up time and sample size, ranging from 0 to 8% (see Table 1). Another important aspect is that rectal cancer development is also associated with longer duration of colitis and lack of surveillance in patients submitted to an IRA.9 Furthermore, many of these cancers found in the remaining rectum may present with an advanced stage, possibly because of a more aggressive tumor biology making close rectal surveillance imperative.9,19 Therefore, mucosal surveillance with rectal biopsies every 6 to 12 months is advised following IRA in ulcerative colitis patients. If dysplasia is found, completion proctectomy is indicated to prevent the development of rectal cancer. Patients with ulcerative colitis of long duration who are not able to undergo surveillance are not good candidates for an IRA. It is also important to emphasize that colectomy with IRA may be better off avoided in patients with previous diagnosis of colonic dysplasia or cancer because of their increased risk of rectal cancer. Nonetheless, patients with advanced metastatic disease and no curable cancer are an exception. This group of patients may benefit from an IRA because of their short life expectancy and the palliative nature of their treatment.
PROCTOCOLECTOMY WITH END ILEOSTOMY
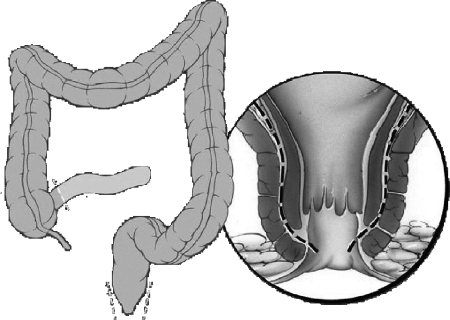
TPC remains a safe and curative alternative with good long-term outcomes and it should still be considered in selected patients. These patients include those who are not good candidates for IPAA or who choose not to undergo a restorative proctocolectomy. Patients with impaired anal sphincters function or severe comorbid disease will not benefit from a restorative operation. These are usually elderly patients and TPC should be indicated when elective surgery for ulcerative colitis is necessary. The main advantage of TPC is the possible removal of all diseased mucosa, preventing rectal dysplasia and cancer. For obvious reasons, TPC will be also necessary for those patients with low rectal cancer when a curable sphincter-saving procedure is not possible. We prefer an intersphincteric technique rather than low stapling technique to avoid any cancer occurrence due to left over ATZ cells in the anal canal (Fig. 2).
Figure 2.
Proctocolectomy with end ileostomy. Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 1996–2010. All rights reserved.
Postoperative Morbidity
TPC can be technically less difficult for the well-trained surgeon and its overall morbidity can be lower when compared with the IPAA.20,21 Phillips et al has published an overall morbidity rate of 39% for TPC, comparable to IPAA, but usually involving less severe complications.22,23 On the other hand, the main disadvantage of TPC is the permanent end ileostomy and its long-term complications such as parastomal hernia, stomal prolapse, and pouching difficulties. Other potential postoperative complications include small bowel obstruction and failure to heal the perineal wound even when the intersphincteric dissection is performed. Delayed healing of the perineal wound is responsible for significant chronic morbidity, it can occur in 18 to 25% of patients leading to persistent perineal sinuses and difficult treatment.24,25 Moreover, the risk of pelvic nerve damage responsible for impaired sexual and urinary function seen in IPAA patients, it is also possible with TPC since the rectal dissection is necessary.
Quality of Life
The possible long-term complications associated with a permanent stoma and the changes in the body image could impact negatively on the patients' quality of life. Camilleri-Brennan et al has shown that IPAA was associated with a significantly better perception of body image than a permanent stoma whereas the quality of life in general was similar when compared with TPC in a carefully matched study.20 Another study using the SF-36 questionnaire has demonstrated that despite having a permanent stoma, the quality of life was restored to the levels of the general population after TPC.26 Finally, Pemberton et al compared IPAA to TPC for performance status after surgery and found significant more advantages in performing daily activities such as sports, sexual and social activities after having an IPAA.27
SUMMARY
In the era of pouch surgery, IPAA is the most appropriate and preferred procedure for patients with ulcerative colitis requiring surgical treatment. However, there is still a role for IRA and TPC for a selected group of patients that may not be good candidates for IPAA. IRA can be considered in advanced uncurable colorectal cancer patients and for young female patients with relatively spared and distensible rectum and no dysplasia or cancer as a possible interim procedure for the concern of increased infertility after IPAA. TPC is the procedure of choice in patients with impaired anal sphincters and high-risk patients for pouch failure as a definite treatment for ulcerative colitis.
References
- 1.Turnbull R B., Jr Surgical treatment of ulcerative colitis: early results after colectomy and low ileorectal anastomosis. Dis Colon Rectum. 1959;2(3):260–263. doi: 10.1007/BF02616889. [DOI] [PubMed] [Google Scholar]
- 2.Hughes E S, Russell I S. Ileorectal anastomosis for ulcerative colitis. Dis Colon Rectum. 1967;10(1):35–39. doi: 10.1007/BF02617384. [DOI] [PubMed] [Google Scholar]
- 3.Aylett S. Ulcerative colitis treated by total colectomy and ileorectal anastomosis: factors associated with its success or failure. Dis Colon Rectum. 1962;5:206–212. doi: 10.1007/BF02616638. [DOI] [PubMed] [Google Scholar]
- 4.Hueting W E, Gooszen H G, Laarhoven C J van. Sexual function and continence after ileo pouch anal anastomosis: a comparison between a meta-analysis and a questionnaire survey. Int J Colorectal Dis. 2004;19(3):215–218. doi: 10.1007/s00384-003-0543-7. [DOI] [PubMed] [Google Scholar]
- 5.Gorgun E, Remzi F H, Goldberg J M, et al. Fertility is reduced after restorative proctocolectomy with ileal pouch anal anastomosis: a study of 300 patients. Surgery. 2004;136(4):795–803. doi: 10.1016/j.surg.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 6.Waljee A, Waljee J, Morris A M, Higgins P D. Threefold increased risk of infertility: a meta-analysis of infertility after ileal pouch anal anastomosis in ulcerative colitis. Gut. 2006;55(11):1575–1580. doi: 10.1136/gut.2005.090316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Remzi F H, Fazio V W, Oncel M, et al. Portal vein thrombi after restorative proctocolectomy. Surgery. 2002;132(4):655–661. discussion 661–662. doi: 10.1067/msy.2002.127689. [DOI] [PubMed] [Google Scholar]
- 8.Sagap I, Remzi F H, Hammel J P, Fazio V W. Factors associated with failure in managing pelvic sepsis after ileal pouch-anal anastomosis (IPAA)—a multivariate analysis. Surgery. 2006;140(4):691–703. discussion 703–704. doi: 10.1016/j.surg.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 9.da Luz Moreira A, Kiran R P, Lavery I. Clinical outcomes of ileorectal anastomosis for ulcerative colitis. Br J Surg. 2010;97(1):65–69. doi: 10.1002/bjs.6809. [DOI] [PubMed] [Google Scholar]
- 10.Pastore R L, Wolff B G, Hodge D. Total abdominal colectomy and ileorectal anastomosis for inflammatory bowel disease. Dis Colon Rectum. 1997;40(12):1455–1464. doi: 10.1007/BF02070712. [DOI] [PubMed] [Google Scholar]
- 11.Leijonmarck C E, Löfberg R, Ost A, Hellers G. Long-term results of ileorectal anastomosis in ulcerative colitis in Stockholm County. Dis Colon Rectum. 1990;33(3):195–200. doi: 10.1007/BF02134178. [DOI] [PubMed] [Google Scholar]
- 12.Börjesson L, Lundstam U, Oresland T, Brevinge H, Hultén L. The place for colectomy and ileorectal anastomosis: a valid surgical option for ulcerative colitis? Tech Coloproctol. 2006;10(3):237–241. discussion 241. doi: 10.1007/s10151-006-0286-x. [DOI] [PubMed] [Google Scholar]
- 13.Grundfest S F, Fazio V, Weiss R A, et al. The risk of cancer following colectomy and ileorectal anastomosis for extensive mucosal ulcerative colitis. Ann Surg. 1981;193(1):9–14. doi: 10.1097/00000658-198101000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spiliadis C A, Spiliadis C A, Lennard-Jones J E. Ulcerative colitis with relative sparing of the rectum. Clinical features, histology, and prognosis. Dis Colon Rectum. 1987;30(5):334–336. doi: 10.1007/BF02555449. [DOI] [PubMed] [Google Scholar]
- 15.Lepistö A, Järvinen H J. Fate of the rectum after colectomy with ileorectal anastomosis in ulcerative colitis. Scand J Surg. 2005;94(1):40–42. doi: 10.1177/145749690509400110. [DOI] [PubMed] [Google Scholar]
- 16.Oakley J R, Lavery I C, Fazio V W, Jagelman D G, Weakley F L, Easley K. The fate of the rectal stump after subtotal colectomy for ulcerative colitis. Dis Colon Rectum. 1985;28(6):394–396. doi: 10.1007/BF02560219. [DOI] [PubMed] [Google Scholar]
- 17.Morson B C, Pang L S. Rectal biopsy as an aid to cancer control in ulcerative colitis. Gut. 1967;8(5):423–434. doi: 10.1136/gut.8.5.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson W R, McDermott F T, Pihl E, Hughes E S. Mucosal dysplasia. A major predictor of cancer following ileorectal anastomosis. Dis Colon Rectum. 1983;26(11):697–700. doi: 10.1007/BF02554974. [DOI] [PubMed] [Google Scholar]
- 19.Johnson W R, McDermott F T, Hughes E S, Pihl E A, Milne B J, Price A B. The risk of rectal carcinoma following colectomy in ulcerative colitis. Dis Colon Rectum. 1983;26(1):44–46. doi: 10.1007/BF02554679. [DOI] [PubMed] [Google Scholar]
- 20.Camilleri-Brennan J, Munro A, Steele R J. Does an ileoanal pouch offer a better quality of life than a permanent ileostomy for patients with ulcerative colitis? J Gastrointest Surg. 2003;7(6):814–819. doi: 10.1016/s1091-255x(03)00103-3. [DOI] [PubMed] [Google Scholar]
- 21.Jimmo B, Hyman N H. Is ileal pouch-anal anastomosis really the procedure of choice for patients with ulcerative colitis? Dis Colon Rectum. 1998;41(1):41–45. doi: 10.1007/BF02236894. [DOI] [PubMed] [Google Scholar]
- 22.Phillips R K, Ritchie J K, Hawley P R. Proctocolectomy and ileostomy for ulcerative colitis: the longer term story. J R Soc Med. 1989;82(7):386–387. doi: 10.1177/014107688908200705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mikkola K, Luukkonen P, Järvinen H J. Restorative compared with conventional proctocolectomy for the treatment of ulcerative colitis. Eur J Surg. 1996;162(4):315–319. [PubMed] [Google Scholar]
- 24.Oakley J R, Fazio V W, Jagelman D G, Lavery I C, Weakley F L, Easley K. Management of the perineal wound after rectal excision for ulcerative colitis. Dis Colon Rectum. 1985;28(12):885–888. doi: 10.1007/BF02554295. [DOI] [PubMed] [Google Scholar]
- 25.Corman M L, Veidenheimer M C, Coller J A, Ross V H. Perineal wound healing after proctectomy for inflammatory bowel disease. Dis Colon Rectum. 1978;21(3):155–159. doi: 10.1007/BF02586557. [DOI] [PubMed] [Google Scholar]
- 26.Camilleri-Brennan J, Steele R J. Objective assessment of quality of life following panproctocolectomy and ileostomy for ulcerative colitis. Ann R Coll Surg Engl. 2001;83(5):321–324. [PMC free article] [PubMed] [Google Scholar]
- 27.Pemberton J H, Phillips S F, Ready R R, Zinsmeister A R, Beahrs O H. Quality of life after Brooke ileostomy and ileal pouch-anal anastomosis. Comparison of performance status. Ann Surg. 1989;209(5):620–626. discussion 626–628. doi: 10.1097/00000658-198905000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]