Abstract
Spontaneous intratumoral hemorrhage associated with a meningioma is an extremely rare event and has a very high rate of morbidity and mortality. We report a patient with a history of subtotal resection of a petroclival meningioma followed by gamma knife radiosurgery who presented with sudden neurological deterioration following intratumoral hemorrhage after 4 asymptomatic years. The patient underwent early resection of this atypical meningioma and evacuation of hematoma via a retrosigmoid transpetrosal approach and had rapid neurological improvement.
Keywords: Petroclival meningioma, intratumoral hemorrhage, atypical meningioma
OBJECTIVE AND IMPORTANCE
Meningiomas are the most common nonglial intracranial tumor with an incidence of 2.3 to 5.5 per 100,000 people,1,2 accounting for 20 to 30% of all primary adult brain tumor diagnoses.3,4,5 They are benign, slow-growing, and highly vascular tumors. Approximately 20% of intracranial meningiomas reside at the skull base.6,7
Spontaneous intracranial hemorrhage occurs in 3.9% of all brain tumors, mostly metastatic tumors or malignant gliomas.8 Intratumoral hemorrhage associated with a meningioma is a much rarer event, occurring in 1.3 to 2.4% of those lesions.9,10,11,12 Most reported intracranial hemorrhages associated with meningiomas are found in the subarachnoid and subdural spaces.11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26 Tumoral bleeding is associated with higher morbidity and mortality rates. Mortality rates of hemorrhagic meningiomas have been found to be 21.1% overall and 9.5% in surgically treated patients.27
We report the case of a 62-year-old woman who presented with sudden neurological deterioration secondary to an intratumoral hemorrhage associated with a petroclival atypical meningioma.
CLINICAL PRESENTATION
A 62-year-old woman with a history of a subtotal resection of a left petroclival meningioma in January 2003 (Fig. 1) and gamma knife radiosurgery in 2004 presented in December 2008 after a 4-year asymptomatic interval with a sudden headache, neuropathies of ipsilateral cranial nerves V to XI, and quadriparesis. She reported no recent trauma nor was she taking anticoagulants. The patient was evaluated at another local emergency department where computed tomography and magnetic resonance (MR) imaging scanning demonstrated a large intratumoral hemorrhage and subarachnoid hemorrhage (Figs. 2 and 3). The patient was monitored in their intensive care unit, and then transferred to our institution for further evaluation and treatment.
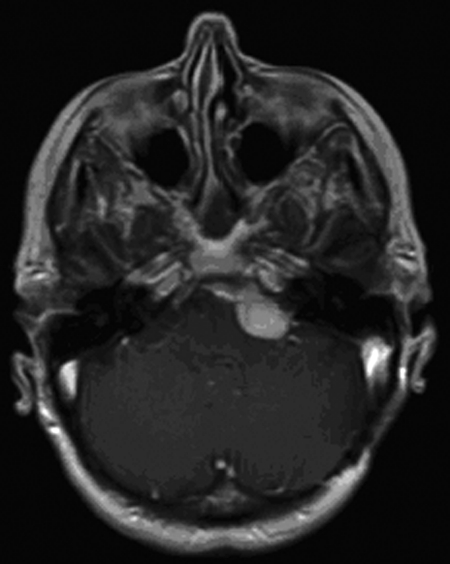
Figure 1.
T1-weighted postcontrast MR imaging done 3 months prior to intratumoral hemorrhage demonstrates a grossly stable homogeneously enhancing extra-axial mass arising along the left aspect of the clivus extending into the left cerebellopontine angle cistern.
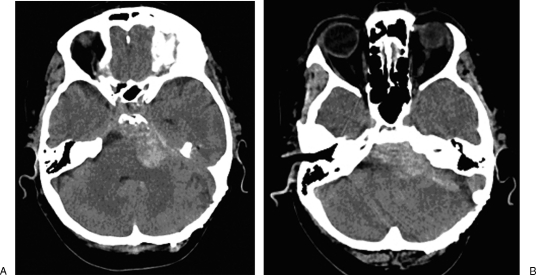
Figure 2.
Postintratumoral hemorrhage computed tomography scans demonstrate a hyperdense extra-axial collection that has increased in size with hyperdensity extending into the adjacent cisterns suggesting subarachnoid hemorrhage (A). The mass effect on the brainstem and fourth ventricle were also more pronounced (B).
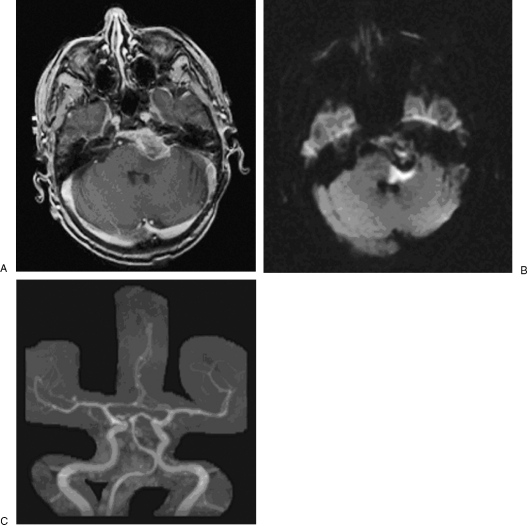
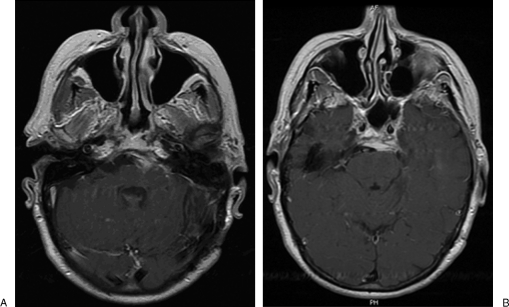
Figure 3.
T1-weighted postcontrast magnetic resonance images demonstrate an area of relatively decreased enhancement centrally within the lesion with increased overall diameter, which may reflect central necrosis and associated hemorrhage within the tumor (A). Adjacent to the mass there is restricted diffusion in the left cerebellar peduncle compatible with cytotoxic edema (B). The mass effect on the pons, left cerebellar peduncle, and fourth ventricle was mildly increased secondary to tumor swelling. MR angiogram demonstrated a dominant left vertebral artery and patent basilar artery adjacent to the tumor without apparent vascular malformations (C).
Upon transfer, the patient did have some initial improvement in her seventh nerve palsy; however, her other deficits persisted, continuing to have deficits in gait and coordination, quadriparesis, and neuropathies of ipsilateral cranial nerves V to XI. Given the fact that the patient's neurological deficits had reached a plateau, surgical removal of the hematoma and debulking of the tumor was planned.
In our institution, preoperative MR angiography (Fig. 2C) failed to demonstrate any vascular abnormalities, which was later confirmed by formal four vessel cerebral angiography.
INTERVENTION
The patient's original operation in 2003 was performed at our institution. Surgery was aborted prior to achieving total resection due to the very vascular nature of the tumor and intraoperative loss of somatosensory-evoked potentials and brainstem auditory–evoked responses. Postoperatively, the patient awoke without any deficits.
The patient underwent a retrosigmoid transpetrosal craniotomy to again enter this highly vascular tumor and evacuate the hematoma (Fig. 4). Tumor resection was performed to near total removal, leaving only a portion of tumor capsule adherent to cranial nerve VI, the pons, and the basilar artery. Postoperative MR imaging confirmed near total resection, demonstrating mild residual enhancement along the posterior clivus and medial left petrous apex (Fig. 5).
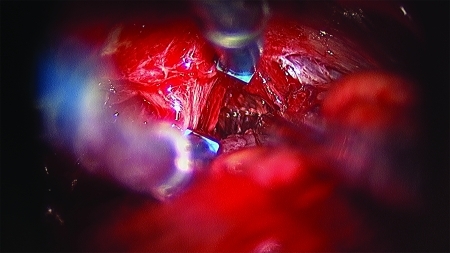
Figure 4.
Intraoperative photograph demonstrates a very vascular meningioma found in the cerebellopontine angle after dissecting down toward the foramen magnum via a retrosigmoid transpetrosal approach.
Figure 5.
Postoperative T1-weighted postcontrast MR image demonstrates near-total resection with residual enhancement along the posterior clivus and medial left petrous apex in the region of surgery, reflecting a small amount of residual tumor and/or postsurgical dural enhancement (A). There is decreased mass effect on the brainstem (B).
Pathology revealed an atypical meningioma with progesterone receptor positivity and an elevated MIB of 14%.
Postoperatively, the patient noted immediate improvement in her quadriparesis and coordination. She progressed in inpatient rehabilitation to independent ambulation, with resolution of her cranial neuropathies with the exception of a left partial cranial nerve VI palsy at 6 months follow-up.
DISCUSSION
Intratumoral hemorrhage associated with a meningioma is a rare event. Intratumoral hemorrhage of a skull base meningioma is even more infrequent. In a review of 47 literature-derived cases of intracranial/intratumoral hemorrhages associated with meningiomas, 13% of those patients had their lesion located at the skull base.27 Due to the rarity of these events, the clinicopathological features of tumor bleeding propensity are poorly defined. In our above case, risk factors for intratumoral hemorrhage possibly include a history of radiosurgery and atypical tumor histopathology.
The relationship, however, between intratumoral hemorrhage and stereotactic radiosurgery is controversial and studies are limited. Kwon et al28 reported a 10-year period in which 173 meningiomas were treated with gamma knife stereotactic radiosurgery. Intratumoral bleeding was observed in four cases (2.3%) during a follow-up period of 1 to 8 years. The authors concluded that the rate of intratumoral hemorrhage was not significantly higher than that reported to occur spontaneously (2.3% versus 1.3 to 2.4%, respectively), suggesting that gamma knife surgery is not a significant factor in the development of intratumoral bleeding.
Bošnjak et al27 reviewed 145 literature-derived cases, noting several factors that may increase the risk of intracranial hemorrhage of a meningioma, particularly age, location, and histopathologic type. Their study suggested that patients with meningiomas who were older than 70 or younger than 30 years of age had a twofold higher bleeding propensity. This review reconfirmed an increased tendency for bleeding in intraventricular meningiomas,26 and suggested a threefold increased propensity for spontaneous bleeding found on the convexity. In terms of histopathology, there was an increased bleeding tendency for fibrous, malignant, and angioblastic meningiomas.
Other suggested factors that may increase the propensity of meningiomas to bleed include the use of anticoagulant medications, hypertension, and traumatic brain injury.27 Presence of microcysts, intratumoral necrosis, and a high proliferation rate may also predispose lesions to hemorrhage.12,29 However, the great majority of meningiomas manifesting hemorrhage are benign variants.11
Mechanisms responsible for bleeding into a benign tumor are unknown; although, several hypotheses have been proposed. First, highly vascular meningiomas may possess abnormal tangles of vessels. As the tumor grows, stretching of the vessels leads to weakening of the vascular walls and rupture of the abnormal vascular networks.26 This hypothesis is based on certain histopathological findings, such as weak, thin-walled vessels and direct peritumoral vascular erosion by tumor.19,20,21,26,30,31 However, not every case reports such abnormal vessel changes. Second, the cerebral edema and venous obstruction commonly found with meningiomas may cause tumor infarction which may cause a direct breakdown of tumor vessels and subsequent hemorrhage.18,26,30 Third, Askenasy et al suggested that enlarged feeding arteries become tortuous and less resistant to blood pressure changes, increasing the susceptibility to rupture under stress.19,32 Other proposed mechanisms of spontaneous hemorrhage include intratumoral coagulopathy, seizure, and malignant transformation.18,19
CONCLUSION
Although rare, major intratumoral hemorrhage in a skull base meningioma is a life-threatening event of which clinicians need to be aware as a possible risk during surveillance of these lesions. This case illustrates how early hematoma evacuation and tumor resection can lead to rapid neurological improvement in the patient. Due to the rarity of this condition, clinicopathological features and mechanisms for hemorrhage are unclear. However, other etiologies for hemorrhage should be excluded prior to surgical exploration.
References
- Kurland L T, Schoenberg B S, Annegers J F, Okazaki H, Molgaard C A. The incidence of primary intracranial neoplasms in Rochester, Minnesota, 1935–1977. Ann N Y Acad Sci. 1982;381:6–16. doi: 10.1111/j.1749-6632.1982.tb50361.x. [DOI] [PubMed] [Google Scholar]
- Sutherland G R, Florell R, Louw D, Choi N W, Sima A A. Epidemiology of primary intracranial neoplasms in Manitoba, Canada. Can J Neurol Sci. 1987;14(4):586–592. [PubMed] [Google Scholar]
- Statistical report. Primary brain tumors in the United States 1998–2002. Central Brain Tumor Registry of the United States. 2005. Available from: http://www.CBTRUS.org Available from: http://www.CBTRUS.org
- McGregor J M, Sarkar A. Stereotactic radiosurgery and stereotactic radiotherapy in the treatment of skull base meningiomas. Otolaryngol Clin North Am. 2009;42(4):677–688. doi: 10.1016/j.otc.2009.04.010. [DOI] [PubMed] [Google Scholar]
- McGovern S L, Aldape K D, Munsell M F, Mahajan A, DeMonte F, Woo S Y. A comparison of World Health Organization tumor grades at recurrence in patients with non-skull base and skull base meningiomas. J Neurosurg. 2010;112(5):925–933. doi: 10.3171/2009.9.JNS09617. [DOI] [PubMed] [Google Scholar]
- Gorman L, Ruben J, Myers R, Dally M. Role of hypofractionated stereotactic radiotherapy in treatment of skull base meningiomas. J Clin Neurosci. 2008;15(8):856–862. doi: 10.1016/j.jocn.2007.05.020. [Epub 2008 Jun 12] [DOI] [PubMed] [Google Scholar]
- Elia A E, Shih H A, Loeffler J S. Stereotactic radiation treatment for benign meningiomas. Neurosurg Focus. 2007;23(4):E5. doi: 10.3171/FOC-07/10/E5. [DOI] [PubMed] [Google Scholar]
- Salcman M. Intracranial hemorrhage caused by brain tumour. In: In: Kaufman HH, editor. Intracerebral Hematomas. New York: Raven Press; 1992. pp. 95–106. [Google Scholar]
- Martínez-Lage J F, Poza M, Martínez M, Esteban J A, Antúnez M C, Sola J. Meningiomas with haemorrhagic onset. Acta Neurochir (Wien) 1991;110(3-4):129–132. doi: 10.1007/BF01400680. [DOI] [PubMed] [Google Scholar]
- Wakai S, Yamakawa K, Manaka S, Takakura K. Spontaneous intracranial hemorrhage caused by brain tumor: its incidence and clinical significance. Neurosurgery. 1982;10(4):437–444. doi: 10.1227/00006123-198204000-00004. [DOI] [PubMed] [Google Scholar]
- Kim D G, Park C K, Paek S H, et al. Meningioma manifesting intracerebral haemorrhage: a possible mechanism of haemorrhage. Acta Neurochir (Wien) 2000;142(2):165–168. doi: 10.1007/s007010050019. [DOI] [PubMed] [Google Scholar]
- Niiro M, Ishimaru K, Hirano H, Yunoue S, Kuratsu J. Clinico-pathological study of meningiomas with haemorrhagic onset. Acta Neurochir (Wien) 2003;145(9):767–772. doi: 10.1007/s00701-003-0089-z. [DOI] [PubMed] [Google Scholar]
- Sunada I, Nakabayashi H, Matsusaka Y, Yamamoto S. Meningioma associated with acute subdural hematoma—case report. Radiat Med. 1998;16(6):483–486. [PubMed] [Google Scholar]
- Jones N R, Blumbergs P C. Intracranial haemorrhage from meningiomas: a report of five cases. Br J Neurosurg. 1989;3(6):691–698. doi: 10.3109/02688698908992693. [DOI] [PubMed] [Google Scholar]
- Waga S, Shimizu T, Shimosaka S, Tochio H. Intratumoral hemorrhage after a ventriculoperitoneal shunting procedure. Neurosurgery. 1981;9(3):249–252. [PubMed] [Google Scholar]
- Yapor W Y, Gutierrez F A. Cocaine-induced intratumoral hemorrhage: case report and review of the literature. Neurosurgery. 1992;30(2):288–291. doi: 10.1227/00006123-199202000-00028. [DOI] [PubMed] [Google Scholar]
- Roux-Vaillard S, Mercier P, Fournier H D, Hayek G, Menei P, Guy G. Intracranial meningiomas revealed by hemorrhage. Report of three cases and literature review. Neurochirurgie. 1999;45(5):407–412. [PubMed] [Google Scholar]
- Lazaro R P, Messer H D, Brinker R A. Intracranial hemorrhage associated with meningioma. Neurosurgery. 1981;8(1):96–101. doi: 10.1227/00006123-198101000-00018. [DOI] [PubMed] [Google Scholar]
- Bloomgarden G M, Byrne T N, Spencer D D, Heafner M D. Meningioma associated with aneurysm and subarachnoid hemorrhage: case report and review of the literature. Neurosurgery. 1987;20(1):24–26. doi: 10.1227/00006123-198701000-00006. [DOI] [PubMed] [Google Scholar]
- Chaskis C, Raftopoulos C, Noterman J, Flament-Durand J, Brotchi J. Meningioma associated with subdural haematoma: report of two cases and review of the literature. Clin Neurol Neurosurg. 1992;94(3):269–274. doi: 10.1016/0303-8467(92)90103-a. [DOI] [PubMed] [Google Scholar]
- Pluchino F, Lodrini S, Savoiardo M. Subarachnoid haemorrhage and meningiomas. Report of two cases. Acta Neurochir (Wien) 1983;68(1-2):45–53. doi: 10.1007/BF01406201. [DOI] [PubMed] [Google Scholar]
- Okuno S, Touho H, Ohnishi H, Karasawa J. Falx meningioma presenting as acute subdural hematoma: case report. Surg Neurol. 1999;52(2):180–184. doi: 10.1016/s0090-3019(97)00028-1. [DOI] [PubMed] [Google Scholar]
- Lieu A S, Howng S L. Intracranial meningioma with hemorrhage. Kaohsiung J Med Sci. 1999;15(2):69–74. [PubMed] [Google Scholar]
- Russell E J, George A E, Kricheff I I, Budzilovich G. Atypical computed tomography features of intracranial meningioma: radiological-pathological correlation in a series of 131 consecutive cases. Radiology. 1980;135(3):673–682. doi: 10.1148/radiology.135.3.7384454. [DOI] [PubMed] [Google Scholar]
- Koumtchev Y, Petkov S, Gozmanov G. Meningioma accompanied by a subdural hematoma. A case report. Review of 17 cases in the literature. Folia Med (Plovdiv) 1993;35(3-4):61–63. [PubMed] [Google Scholar]
- Helle T L, Conley F K. Haemorrhage associated with meningioma: a case report and review of the literature. J Neurol Neurosurg Psychiatry. 1980;43(8):725–729. doi: 10.1136/jnnp.43.8.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bošnjak R, Derham C, Popović M, Ravnik J. Spontaneous intracranial meningioma bleeding: clinicopathological features and outcome. J Neurosurg. 2005;103(3):473–484. doi: 10.3171/jns.2005.103.3.0473. [DOI] [PubMed] [Google Scholar]
- Kwon Y, Ahn J S, Jeon S R, et al. Intratumoral bleeding in meningioma after gamma knife radiosurgery. J Neurosurg. 2002;97(Suppl 5):657–662. doi: 10.3171/jns.2002.97.supplement. [DOI] [PubMed] [Google Scholar]
- Kuzeyli K, Cakir E, Usul H, et al. Intratumoral haemorrhage: a clinical study. J Clin Neurosci. 2004;11(5):490–492. doi: 10.1016/j.jocn.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Gruszkiewicz J, Doron Y, Gellei B, Peyser E. Massive intracerebral bleeding due to supratentorial meningioma. Neurochirurgia (Stuttg) 1969;12(3):107–111. doi: 10.1055/s-0028-1095292. [DOI] [PubMed] [Google Scholar]
- Nakao S, Sato S, Ban S, Inutsuka N, Yamamoto T. Massive intracerebral hemorrhage caused by angioblastic meningioma. Surg Neurol. 1977;7(4):245–248. [PubMed] [Google Scholar]
- Askenasy H M, Behmoaram A D. Subarachnoid hemorrhage in meningiomas of the lateral ventricle. Neurology. 1960;10:484–489. doi: 10.1212/wnl.10.5.484. [DOI] [PubMed] [Google Scholar]