Abstract
Slow rates of habituation are related to greater energy intake, and cross-sectionally to body weight. The present study is designed to assess whether slow rates of habituation are prospectively related to zBMI change over a 12 month period in 66 lean 8–12 year-old children, and whether the rate of habituation is a stable behavioral phenotype. Results showed slower rates of habituation predicted greater zBMI change, controlling for child sex, age, initial zBMI, dietary awareness and minority status. In addition, the rate of habituation was stable over the year of observation. These data suggest that slow rates of habituation may be a risk factor for weight gain and the development of obesity. Future research is needed to understand the mechanism for this effect, and assess whether the habituation phenotype interacts with other behavioral phenotypes, such as food reinforcement, to influence increases in zBMI.
Keywords: habituation, weight gain, children
Habituation refers to a progressive decrease in responding with repeated presentation of a stimulus, and the response can be recovered with presentation of a novel stimulus, which may lead to dishabituation of responding to the initial stimulus (Epstein, Temple, Roemmich, & Bouton, 2009). Accordingly, repeated presentation of a food stimulus leads to habituation of responding to that food, and the responding can be recovered by presenting a new food, leading to greater energy intake (Epstein, Temple et al., 2009). The rate of habituation is related to energy intake within a meal (Epstein, Robinson et al., 2009; Temple, Giacomelli, Roemmich, & Epstein, 2008a), and a slow rate of habituation is related to greater energy intake in ad libitum eating sessions (Carr & Epstein, 2010). Consistent with the observation that slow habituation is related to greater energy intake, cross sectional data show that obese people habituate at a slower rate to repeated food cues than leaner peers (Epstein et al., 2008; Temple, Giacomelli, Roemmich, & Epstein, 2007). Prospective data are needed to assess whether habituation is a product of being overweight, or whether slow rates of habituation are a risk factor for weight gain in lean children.
The utility of habituation as a behavioral phenotype that can be used to predict weight gain and the development of obesity is dependent on habituation being a stable behavioral trait. Children were retested for zBMI and the rate of habituation to the same food cues after one year to test both whether the baseline rate of habituation predicts zBMI gain, and whether baseline habituation predicts habituation at one year to assess stability of habituation.
METHODS
Participants
Participants were 66 (36 female, 30 male) children 9–13 years who were non-overweight/obese at baseline recruited from a sample of 103 non-overweight children who had participated in one of three previous experiments with common methods to study habituation (Epstein, Robinson, Roemmich, Marusewski, & Roba, 2010; Epstein, Robinson et al., 2009). The average baseline characteristics of the participants were 10.6 ± 1.5 years of age, BMI of 17.2 ± 0.1.9 (BMI = kg/m2) and zBMI of −0.09 ± 0.75. Based on child race, 82.5% were Caucasian, 11.7% African American, 4.9% other or mixed race, and 1% Asian. The majority of the participants’ parents completed college (78.8%) and had a household income greater than $70,000 per year (63.0%). Exclusionary criteria for the original experiments were: any obesity related chronic diseases (i.e., diabetes), any developmental or psychological disabilities that may impair participant’s ability to complete the experiment; any medications such as methylphenidate that may modify appetite, and prior participation in a laboratory study using similar methodology.
Procedures
Parents of the participants received a telephone call to participate in a 1 year follow-up and to ensure that the child still met the above criteria. Participants were scheduled for one 60-minute visit to the University at Buffalo’s Behavioral Medicine Laboratory on a weekday between the hours of 2:30 and 5:30 pm. Parents were instructed to have their children eat their normal breakfast and lunch, but to not eat or drink anything (except water) 3-hours prior and not to consume study foods 24-hours prior to the visit. Upon arrival to the laboratory, both parents and children completed the same forms from baseline including consent and assent forms, same-day food recall for the child, a demographic form, food liking, hunger and food preference questionnaires. After forms were completed, the parents were escorted to the waiting area and the experimental task commenced. After the experimental task, participants filled out both a hunger scale and a Dutch Eating Behavior Questionnaire adapted for children (Hill & Pallin, 1998) which assesses dietary awareness. Height and weight were then obtained using the procedures outlined below. Finally, both parent and child were debriefed about the purpose of the study and given written materials about the theoretical rationale behind the experiment. Participants were compensated $20.00 US dollars gift card for completing the experiment and parents were compensated $10 gift card for travel and/or child care expenses. All procedures were conducted in accordance with guidelines for the ethical conduct of human research outlined by the National Institutes of Health and with the approval of the University at Buffalo Health Sciences Institutional Review Board.
Habituation Task
All 3 experiments used the same computer generated task to measure habituation of responding for food, programmed at a variable interval 120 ± 42 seconds (VI-120) reinforcement schedule, so that participants were rewarded one point for the first response made after approximately 120s had passed. The computer task consisted of two squares, one that flashed red every time a mouse button is pressed and another square that flashed green when a point was earned. The task was divided into habituation and recovery phases for all three experiments. The habituation phase was 24 minutes, divided into 12, 2-minute trials, during which participants could earn points towards access to 80 kcal – 100 kcal portions of food. The recovery phase lasted 4 minutes, divided into 2, 2-minute trials, during which participants had the opportunity to earn points towards the same food or a different food, depending on the study and experimental design. Participants received the food immediately after each point was earned and could continue to play the computer task while eating. Water was provided ad libitum throughout the duration of the experiment. Participants were instructed that when they no longer wanted to earn access to the food stimulus they could go another table and engage in the activities provided. Activities included age appropriate puzzles, crosswords, word searches, and magazines. Participants could move freely between the computer and activity stations.
Participants in each experiment were studied under the same habituation conditions, with the opportunity to obtain portions of food over a 24 minute period, divided into 12 2-min blocks. In Experiment 1 participants were randomized to earn 80kcal–100kcal portions of Kraft® Macaroni and Cheese or Domino’s® cheese pizza during the habituation phase, while in the other experiments children could earn access to 80–100 kcal portions of Kraft® Macaroni and Cheese. No differences were observed in rate of habituation as a function of presentation of either pizza or macaroni and cheese in Experiment 1. Children could earn 100 kcal portions of Hershey’s® chocolate bars during the recovery phase in Experiment 1 (Epstein et al., 2008). Participants in experiment 2 were randomized to one of three groups differing in the recovery phase food, with the opportunity to earn points towards 100 Kcal portions of either Kraft® Macaroni and Cheese (same food group), Spiral Kraft® Macaroni and Cheese (similar food group), or Chicken nuggets (different food group) (Epstein et al., 2010). In Experiment 3 (unpublished), a memory task was used as a dishabituator after the habituation trials, with participants randomly assigned to one of three groups: 1) Automatic task, 2) Controlled task, 3) No task that differed in the dishabituator tasks. Since the first 24 minutes was common to all the experiments, habituation on those trials was combined across studies. Recovery conditions differed across studies, and the data for these conditions could not be combined.
Laboratory Environment
The laboratory was specially constructed for eating experiments and is equipped with an air delivery system that circulates new air through each room approximately 10 times per hour. The experiment rooms are also constructed with intercom systems so that the participant could communicate with the experimenter throughout the duration of the experiment.
Measures
Habituation
The habituation task was a computer controlled task designed to assess habituation of responding for food over time. The primary outcome measures was the number of consecutive 2-min time blocks in which subjects continued to respond before terminating responding. In addition, the pattern of responses across the 12, 2-min time blocks was recorded.
Same-day Food Recall
Same-day food recalls were conducted as an interview with both the child and parent present to verify adherence to the study protocol by ensuring that the participant had not consumed food or drink (except water) in the 3 hours prior to the appointment and that they had not consumed the study foods that day.
Demographics
A general demographics questionnaire was used to assess education status, annual income, race and ethnicity at baseline and 1 year.
Anthropometrics
Height (cm) and weight (lb) were measured without shoes in light clothing after the participant had voided using a Digi-Kit™ digital stadiometer and a Tanita™ digital weight scale. These measurements were then used to calculate BMI (kg/m2). Children below the 85th BMI percentile were defined as non-overweight.
Dietary Awareness
The Dutch Eating Questionnaire revised for children ages 8–12 was utilized to measure dietary awareness (Hill & Pallin, 1998). Examples of questions asked on the DEBQ are “I have tried to lose weight”; “I try not to eat between meals because I want to be thinner”. The median score on this questionnaire was 6.
Analytic Plan
One way analysis of variance and Chi-Square tests tested for differences in the characteristics of children who completed the one year follow-up (N = 66) versus those who did not complete the one year follow-up (N = 37). The primary analysis was a multiple regression model to assess whether the rate of habituation to food was related to zBMI change, controlling for child age, sex, minority status, dietary awareness and baseline zBMI. zBMI change is an ideal dependent measure for this analysis, since zBMI values are adjusted for child sex and age, and zBMI takes into account height. However, zBMI values may not be readily interpretable, so in addition to zBMI we also calculated regression models to predict BMI, weight change and percent overweight (% over the 50th BMI percentile) change to facilitate interpretation of the results using the same covariates, with the exception that baseline levels of the dependent variable were used as covariates, rather than baseline zBMI.
Multiple regression was also used to compare the relationship between the rate of habituation at baseline and after one year, controlling for child age, sex, minority status, dietary awareness and baseline zBMI. In addition, mixed regression models were used to compare the slope for the changes in 12, 2-min time blocks at baseline versus at one year followup. Mixed regression models allow for correlational analysis on repeated measures data. Baseline values were used to predict one year values over 12 2-min time blocks, with intercept and time blocks as random variables, and sex, age, minority status, dietary awareness and baseline zBMI status as fixed covariate effects.
RESULTS
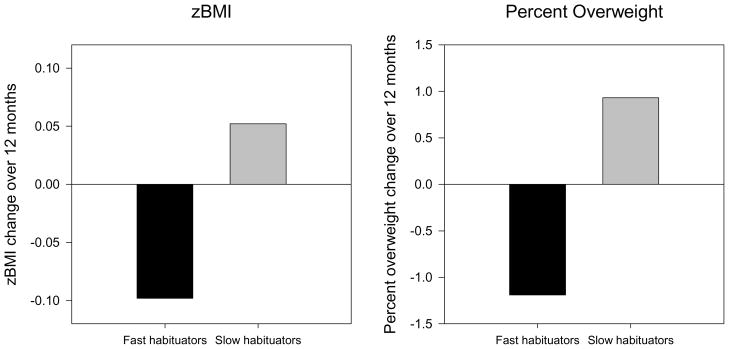
No differences were observed between those children who participated in the follow-up versus those who did not for age, sex, parental education or income, dietary awareness or baseline zBMI, but there were differences in child race (p < 0.05) by follow-up status. Of the 37 children who did not attend follow-up, 27 (78%) were Caucasian, 8 (21.6%) were African American, and 1 (2.7%) was Asian and 1 (2.7%) other or mixed race, while the 66 children who participated in follow-up included 58 (87.8%) Caucasian, 4 (6.1%) African American and 4 (6.1%) mixed race or other. Minority status was included as a covariate in all analysis to control for differences in participation. Additional covariates were age, sex, dietary awareness, and baseline zBMI. Regression analysis for zBMI changes showed the rate of habituation (β = 0.024, S.E. = 0.011, p = 0.040) was the only independent predictor of zBMI change (Table 1). Results of regression models to predict BMI (β = 0.060, S.E. = 0.029, p = 0.046), weight change (β = 0.350, S.E. = 0.164, p = 0.024) and percent overweight change (β = 0.344, S.E. = 0.167, p = 0.042) all showed the same pattern of results, that a longer time to habituate (slower habituation) led to greater increases in BMI, weight or percent overweight. To get an idea of the differences in zBMI and percent overweight change for slow or fast habituators, we calculated changes over one year based on the regression equations for those children who were 1 SD below (fast habituators) or 1 SD above (slow habituators) the average rate of habituation (Figure 1). These results show that fast habituators had decreases in zBMI (−.098) and percent overweight (−1.189), while slow habituators had zBMI and percent overweight gains (0.052, 0.929). Thus, if the rate of change in zBMI or percent overweight were constant over time, a fast habituator would show a reduction in percent overweight of 5.95 percent overweight or −0.49 zBMI units over 5 years, while a slow habituator would gain 4.65 percent overweight or 0.26 zBMI units. Thus, if the same rate of change was observed over five years, the average slow habituator would be 10.6 percent overweight units greater than the average fast habituator, while a slow habituator would be 0.75 zBMI units greater after five years in comparison to a faster habituator.
Table 1.
Regression model predicting changes in zBMI over 12 months (N = 66)
| Predictor | B Coefficient | S.E. | t | p |
|---|---|---|---|---|
| Constant | −0.342 | .302 | −1.133 | 0.26 |
| Rate of habituation | .024 | .011 | 2.083 | .042 |
| Sex | .054 | .071 | 0.764 | .448 |
| Age | .012 | .024 | 0.505 | .616 |
| Baseline zBMI | −.007 | .047 | −.149 | .882 |
| Minority status | −.065 | .103 | −.631 | .530 |
| Dietary awareness | .002 | .015 | .133 | .895 |
Figure 1.
zBMI and percent overweight changes over 12 months for participants who were fast habituators (−1 SD below the average rate of habituation) or slow habituators (1 SD above the average rate of habituation) based on the multiple regression model to predict zBMI change. In the multiple regression, the rate of habituation was an independent predictor of zBMI change (p<.05), controlling for age, sex, baseline zBMI, dietary awareness and minority status.
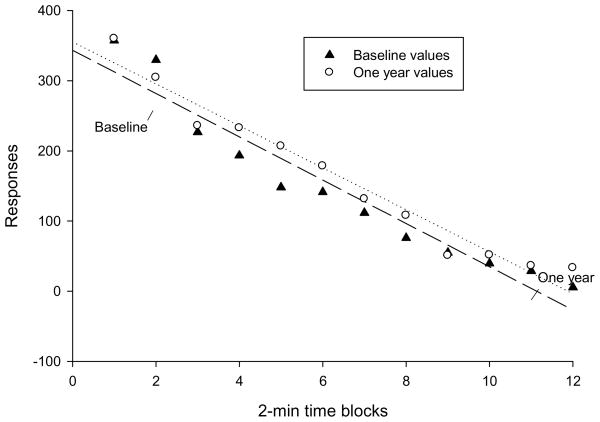
Multiple regression showed a significant relationship between rate of habituation at baseline and after one year (β = 0.76, S.E. = 0.09, p < 0.001). Similarly, mixed regression for the pattern of responses over 2 min-blocks showed (Figure 2) baseline level of habituation was a strong predictor of the rate of habituated responding at one year (estimate = 0.045, S.E. = 0.012, p = 0.0002). As shown in Figure 2, slopes for the rate of change over the 12 2-min trials were very similar at baseline and after one year.
Figure 2.
Regression lines for responding over 12, 2-min time blocks for participants at baseline and after one year of follow-up. Mixed regression models showed a significant relationship between responding over time (p = 0.0002), with a slight increase in responding across 2-min blocks at one year (β = 0.04), but with minimal differences in the slope of the lines.
DISCUSSION
The results of this study show that the rate of habituation at baseline predicted zBMI change after one year of follow-up. Lean children who habituated at a slower rate showed greater weight gain. This is consistent with the cross-sectional data showing that obese children (Temple, Giacomelli, Roemmich et al., 2007) and adults (Epstein, Paluch, & Coleman, 1996) habituate at a slower rate than leaner peers. This slower habituation is associated with greater energy intake during the habituation session (Epstein et al., 2008; Epstein, Robinson et al., 2009), as well as predicting ad libitum energy intake in a separate session (Carr & Epstein, 2010). These data suggests that slow habituation to food should be considered a risk factor for weight gain in children, along with other behavioral risk factors for weight gain, including the reinforcing value of food (Hill, Saxton, Webber, Blundell, & Wardle, 2009) and impulsivity for food (Francis & Susman, 2009; Seeyave et al., 2009).
Habituation is a model for factors that influence the cessation of eating, recovery of eating after cessation has occurred, or the effects of variety on maintaining intake (Epstein, Temple et al., 2009), Habituation may interact with other variables that influence eating, such as the reinforcing value of food (Epstein, Leddy, Temple, & Faith, 2007). The reinforcing value of food is one way to operationalize the reward value of food, which may provide a model for factors that influence the initiation to eat. In previous research we have shown that the reinforcing value of food and habituation are related, such that people who find food more reinforcing may habituate to food at a slower rate (Carr & Epstein, 2010). One avenue for future research would be to assess whether habituation to food and reinforcing value of food are synergistic risk factors, such that weight gain would be greatest for those who are very motivated to eat and habituate at a slow rate to food in comparison to those may be motivated to eat, but habituate to food rapidly, or those who are not very motivated to eat but habituate at a slower rate.
If habituation is a risk factor for some children to gain weight then interventions that hasten habituation may be important for treatment. One factor may be to reduce the variety of food, since increasing variety will slow down the rate of habituation (Epstein et al., 2010; Epstein, Robinson et al., 2009; Temple et al., 2008a). It may be worthwhile to reduce the variety of less healthy, high energy density foods to reduce their intake, while simultaneously increasing variety of healthier, low energy density foods that increase satiation (Rolls et al., 1999; Rolls, Drewnowski, & Ledikwe, 2005). It is also important that reducing variety reduces the reinforcing value of food (Myers Ernst & Epstein, 2002) such that reducing variety may simultaneously influence both food reinforcement and habituation. There are other factors that could speed up the rate of habituation to food, including not eating in combination with sedentary behaviors. Eating while engaged in alternative activities such as television watching can reduce habituation (Temple, Giacomelli, Kent, Roemmich, & Epstein, 2007), and removing these alternative sources of stimulation can enhance habituation.
The repeated assessment of habituation provided an opportunity to examine the stability of the habituation phenotype, with results showing the phenotype is stable over a 12 month period, with no significant differences in the slopes of the regression lines describing the rates of responding over 12 months. It is important to document that the phenotype is stable over time in order to argue that habituation is a behavioral phenotype that can be used to characterize children. Variability in the rate of habituation, such that sometimes children would be fast habituators and sometimes slow habituators would reduce the utility of categorizing a child in regard to their rate of habituation as a predictor of weight gain. However, the stability of the phenotype suggests it may be challenging to modify. The interventions of reducing variety and reducing distractions are environmental manipulations that may reduce the rate of habituation, but will not change the phenotype of habituation. Research is needed on individualized interventions that could modify the phenotype, such that people learn to habituate faster to repeated food stimuli.
This study provides the novel findings that habituation is a stable individual difference characteristic that predicts zBMI change over one year, but there are limitations to consider that may reduce the confidence in the findings. One important limitation is that the participants were a convenience sample of participants who were in other studies and volunteered to return. We were able to study about two-thirds of the original sample, but research is needed to recruit a new sample of subjects who are followed over time. The sample included approximately an equal number of boys and girls, with sex not interacting with habituation to predict zBMI change. Previous research has not shown sex to influence the rate of habituation. Approximately 20% of the sample was ethnic/minority, and again minority status did not interact with habituation to predict zBMI change and there are no data to suggest that minority status would influence habituation. Still, recruiting a larger percentage of subjects as minorities would enhance confidence that the results can be extended to minority populations. Follow-up was measured after one year, and we project growth patterns over five years. It would be preferable to include longer follow-up periods to better establish longer-term effects on zBMI change. Finally, we only studied how the rate of habituation to two types of high fat, dinner entrees predict zBMI change. We have studied habituation to a wide variety of foods (Epstein, Robinson et al., 2009; Epstein, Saad, Giacomelli, & Roemmich, 2005; Epstein et al., 2003; Temple et al., 2008a; Temple, Giacomelli, Roemmich, & Epstein, 2008b), and it is possible that the rate of habituation is different for snack or dessert foods or healthier food options. However, it makes sense to study the rate of habituation to high fat entrée foods as a starting point, with additional research exploring how the rate of habituation to snack foods or food that vary in energy density or macronutrient content are related to zBMI gain.
In summary, these results point to habituation as a stable individual difference characteristic that predicts zBMI change. Research is needed to replicate these findings in a larger sample of children and to consider how factors that manipulate habituation could be used to develop programs to prevent obesity. Research is also needed to assess whether interventions can be developed that modify the basic pattern of habituation, so that children learn to habituate faster when food stimuli are presented, or whether habituation is such a basic response pattern that it is not susceptible to change. Since interventions to alter eating through habituation may be very different than traditional programs to modify energy intake, research on habituation may increase our toolbox of interventions that may prove to be successful in modifying ingestive behavior and thus preventing obesity.
Acknowledgments
Appreciation is expressed to Lora Roba for running subjects. Dr. Epstein is a consultant to Kraft foods and NuVal/ONQI. The other authors do not have any potential conflict of interests. This research was funded in part by a grant from the National Institute of Diabetes and Digestive Diseases, 1U01 DK088380 awarded to Dr. Epstein.
Role of Funding Sources
This research was funded in part by a grant from the National Institute of Diabetes and Digestive Diseases, 1U01 DK088380 awarded to Dr. Epstein. NIDDK had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Appreciation is expressed to Lora Roba for running subjects.
Footnotes
Contributors
Dr. Epstein was involved in study design, procurement of grant funds, statistical analysis and writing the first draft of the manuscript. Ms. Robinson and Ms. Marusewski implemented the study protocol and all authors contributed to and have approved the final manuscript.
Conflict of Interest
Dr. Epstein is a paid consultant to Kraft Foods and NuVal. All other authors declare that they have no conflicts of interest.
Research Highlights
This study shows that the rate of habituation is a prospective predictor of zBMI and weight gain in non-overweight 8–12 year old children.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Carr KA, Epstein LH. Reinforcing value and habituation to food are related. Manuscript submitted for publication 2010 [Google Scholar]
- Epstein LH, Leddy JJ, Temple JL, Faith MS. Food reinforcement and eating: A multilevel analysis. Psychological Bulletin. 2007;133:884–906. doi: 10.1037/0033-2909.133.5.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Paluch R, Coleman KJ. Differences in salivation to repeated food cues in obese and nonobese women. Psychosomatic Medicine. 1996;58:160–164. doi: 10.1097/00006842-199603000-00011. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Robinson JL, Roemmich JN, Marusewski AL, Roba LG. What constitutes food variety? Stimulus specificity of food. Appetite. 2010;54:23–29. doi: 10.1016/j.appet.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Robinson JL, Temple JL, Roemmich JN, Marusewski A, Nadbrzuch R. Sensitization and habituation of motivated behavior in overweight and non-overweight children. Learning and Motivation. 2008;39:243–255. doi: 10.1016/j.lmot.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Robinson JL, Temple JL, Roemmich JN, Marusewski AL, Nadbrzuch RL. Variety influences habituation of motivated behavior for food and energy intake in children. American Journal of Clinical Nutrition. 2009;89:746–754. doi: 10.3945/ajcn.2008.26911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Saad FG, Giacomelli AM, Roemmich JN. Effects of allocation of attention on habituation to olfactory and visual food stimuli in children. Physiology and Behavior. 2005;84:313–319. doi: 10.1016/j.physbeh.2004.12.009. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Saad FG, Handley EA, Roemmich JN, Hawk LW, McSweeney FK. Habituation of salivation and motivated responding for food in children. Appetite. 2003;41:283–289. doi: 10.1016/s0195-6663(03)00106-5. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Temple JL, Roemmich JN, Bouton ME. Habituation as a determinant of human food intake. Psychological Review. 2009;116:384–407. doi: 10.1037/a0015074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Archives of Pediatrics and Adolescent Medicine. 2009;163:297–302. doi: 10.1001/archpediatrics.2008.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill AJ, Pallin V. Dieting awareness and low self-worth: related issues in 8-year-old girls. International Journal of Eating Disorders. 1998;24:405–413. doi: 10.1002/(sici)1098-108x(199812)24:4<405::aid-eat7>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Hill C, Saxton J, Webber L, Blundell J, Wardle J. The relative reinforcing value of food predicts weight gain in a longitudinal study of 7--10-y-old children. American Journal of Clinical Nutrition. 2009;90:276–281. doi: 10.3945/ajcn.2009.27479. [DOI] [PubMed] [Google Scholar]
- Myers Ernst M, Epstein LH. Habituation of responding for food in humans. Appetite. 2002;38:224–234. doi: 10.1006/appe.2001.0484. [DOI] [PubMed] [Google Scholar]
- Rolls BJ, Bell EA, Castellanos VH, Chow M, Pelkman CL, Thorwart ML. Energy density but not fat content of foods affected energy intake in lean and obese women. American Journal of Clinical Nutrition. 1999;69:863–871. doi: 10.1093/ajcn/69.5.863. [DOI] [PubMed] [Google Scholar]
- Rolls BJ, Drewnowski A, Ledikwe JH. Changing the energy density of the diet as a strategy for weight management. Journal of the American Dietetic Association. 2005;105:S98–103. doi: 10.1016/j.jada.2005.02.033. [DOI] [PubMed] [Google Scholar]
- Seeyave DM, Coleman S, Appugliese D, Corwyn RF, Bradley RH, Davidson NS, et al. Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Archives of Pediatrics and Adolescent Medicine. 2009;163:303–308. doi: 10.1001/archpediatrics.2009.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL, Giacomelli AM, Kent KM, Roemmich JN, Epstein LH. Television watching increases motivated responding for food and energy intake in children. American Journal of Clinical Nutrition. 2007;85:355–361. doi: 10.1093/ajcn/85.2.355. [DOI] [PubMed] [Google Scholar]
- Temple JL, Giacomelli AM, Roemmich JN, Epstein LH. Overweight children habituate slower than non-overweight children to food. Physiology and Behavior. 2007;91:250–254. doi: 10.1016/j.physbeh.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL, Giacomelli AM, Roemmich JN, Epstein LH. Dietary variety impairs habituation in youth. Health Psychology. 2008a;27:S10–S19. doi: 10.1037/0278-6133.27.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL, Giacomelli AM, Roemmich JN, Epstein LH. Habituation and within-session changes in motivated responding for food in children. Appetite. 2008b;50:390–396. doi: 10.1016/j.appet.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]