Summary
Enhancing immunity to tuberculosis in animal models after exposure to the infection has proved difficult. In this study we used a newly described flow cytometric technique to monitor changes in cell populations accumulating in the lungs of guinea pigs challenged by low dose aerosol infection with Mycobacterium tuberculosis and vaccinated ten days later. On day forty after infection the fusion protein F36 and a pool of Ag85A and ESAT-6 vaccines had significant effects on the bacterial load, showed increased expression of the activation marker CD45+ on CD4+ T cells, and reduced numbers of heterophils. Lung pathology and pathology scores were marginally improved in animals given these vaccines, but lymph node pathology was not influenced. Despite early effects no changes in long term survival were seen. These results suggest that a single post-exposure vaccination can initially slow the disease process. However, this effect is transient, but this could be of use in an multidrug resistant/extremely drug resistant outbreak situation because it could potentially slow the infection long enough to complete drug susceptibility testing and initiate effective chemotherapy.
Keywords: Post-exposure vaccination, tuberculosis, guinea pig model
Introduction
Considerable progress has been made over the past few years in the development of new tuberculosis vaccine candidates designed either for direct prophylactic effects or BCG prime boosting strategies. 1–3 However, no head-way has been made in terms of vaccines that could be used to vaccinate against latent tuberculosis, or given therapeutically in a post-exposure mode in the context of new outbreak situations. In fact, most studies reported to date have shown an absence of changes in bacterial load and pathology during immunotherapeutic vaccines or in the case of repeated Heat Shock Protein DNA vaccination a worsened disease state. 4, 5
However, from the results of the studies reported, two pieces of information have been hypothesized. The first is that antigens that are strongly recognized during the initial emergence of the acquired response do not appear to boost existing immunity once the animal is well into the chronic phase of the infection. This may indicate that these antigens no longer predominate or that immunity is already maximally being expressed in the animal. 4 The second is that even though antigen-specific T cells could potentially be expanded by post-exposure vaccination, the gradual degeneration and necrosis in the lungs may physically prevent adequate penetration of these cells, confounding the expression of resistance.
This latter parameter is particularly pertinent to the guinea pig, a useful small animal model that has several similarities to the pathogenesis of the disease in humans. 6–12 In unpublished studies our laboratory tried several promising vaccines without any protective effects. However, it quickly became apparent that we were administering these vaccines during a late chronic phase of disease when the caseous necrotic process in the guinea pig lung was already non-reversible. In the present study therefore we looked at the potential for post-exposure vaccination given soon after primary exposure. Two of the vaccine candidates assayed, Ag85A and ESAT mixture and the other a Toll-like receptor [TLR] designed agonist F36 fusion vaccine, 13 demonstrated favorable results. The fusion protein designated F36 consisted of acylated Rv1411, a potent Toll-like receptor-2 agonist, fused to ESAT-6, a well-characterized immunogenic protein from Mycobacterium tuberculosis.13 Our previous studies have shown that F36 fusion protein strongly induced IL-12 secretion from macrophages and induced the increased accumulation of CD4 T cells capable of secreting IFN-γ in the lungs of M. tuberculosis infected mice. These mice were significantly protected from low-dose aerosol challenge with M. tuberculosis.
The Ag85A and ESAT mixture and the F36 fusion vaccine, 13 had protective post-exposure vaccination effects in the guinea pig model. The protective effects seen were reduced bacterial load, increased expression of the activation marker CD45+ on CD4+ T cells, and reduced numbers of heterophils. However, these effects were transient as improved long term survival was not evident. Because of the latter this approach would probably not be useful in established active disease, but could be applied to emergency outbreak situations where exposure was recent.
Methods
Guinea pigs
Female outbred Hartley guinea pigs (approximately 500g in weight) were purchased from the Charles River Laboratories (North Wilmington, MA, USA) and held under barrier conditions in a Biosafety Level III animal laboratory. The specific pathogen-free nature of the guinea pig colonies was demonstrated by testing sentinel animals. All experimental protocols were approved by the Animal Care and Usage Committee of Colorado State University. Animals were vaccinated with BCG Pasteur [103 intradermal], or with protein antigens delivered in an emulsion of 25ug MPL and 250ug DDA [monophosphoryl lipid A/dimethyldioctadecylammonium bromide]. The F36 [Rv1411/ESAT] fusion, as well as two others based upon fusions of Rv3841 with Rv2031 or Rv2032, were made as previously described.13 Controls were given adjuvant only. Animals were vaccinated once only, ten days after aerosol infection.
Experimental infection
Guinea pigs were challenged using a Madison chamber aerosol generation device, by delivering Mycobacterium tuberculosis H37Rv at a low-dose aerosol of 20 bacilli. Animals were then assayed for post-exposure protective effects on day 40 of the infection. Bacterial counts in the organs of guinea pigs (n = 5) were determined by plating serial dilutions of homogenates of lungs on nutrient 7H11 agar and counting colony-forming units after 3 weeks incubation at 37°C.
Histological analysis
The lung lobes and spleens from each guinea pig were fixed with 4% paraformaldehyde in phosphate buffered saline (PBS). Sections from these tissues were stained using haematoxylin and eosin and the Ziehl-Neelsen stain for acid-fast bacilli. In guinea pigs the concurrent progression of lung and spleen lesions was evaluated using a histological grading system. 14 The method for grading ganulomatous lesions was based on inflammatory cell numbers and their infiltrative distribution pattern in the organs assayed. Briefly, scoring of the pathology of lung and spleen sections to provide a cumulative score is done as follows: Primary lesion scoring, 0 – no primary lesion present, 1 – sparse to few foci of primary lesions present, 2 – multiple foci of primary lesions present, 3 – multiple foci of primary lesions present with the majority coalescing.
Primary lesions with necrosis, 0 – Primary lesion with the majority showing no necrosis, mineralization or fibrosis, 1 – primary lesions present with < 30% necrosis, 2 –primary lesions present with 35–65% necrosis, 3 – primary lesions present with 70–100% necrosis. Primary lesions with mineralization, 0 – Primary lesion with the majority showing no necrosis, mineralization or fibrosis, 1 – primary lesions present with < 30% minerlization, 2 – primary lesions present with 35–65% minerlization, 3 – primary lesions present with 70–100% minerlization. Primary lesions with fibrosis, 0 – Primary lesion with the majority showing no necrosis, mineralization or fibrosis, 1 – primary lesions present with < 30% fibrosis, 2 – primary lesions present with 35–65% fibrosis, 3 –primary lesions present with 70–100% fibrosis. Secondary lesion scoring, 0 – no secondary lesions present, 1 – sparse to few foci of secondary lesions present, 2 –multiple foci of secondary lesions present, 3 – multiple foci of secondary lesions present with the majority coalescing. A veterinary pathologist completed the blind scoring of lung and spleen lesions which was based on randomly selected sections in the experiment from five guinea pigs from each experimental group at forty days after infection.
Lung cell digestion
To prepare single cell suspensions the lungs were perfused with 20.0 ml of a solution containing PBS and heparin (50 U/ml; Sigma-Aldrich, St. Louis, MO) through the pulmonary artery and the caudal lobe aseptically removed from the pulmonary cavity, weighted and placed in media and dissected. The dissected lung tissue was incubated with complete DMEM (cDMEM media) containing collagenase XI (0.7 mg/ml; Sigma-Aldrich) and type IV bovine pancreatic DNase (30 ug/ml; Sigma-Aldrich) for 30 minutes at 37°C. The digested lungs were further disrupted by gently pushing the tissue twice through a cell strainer (BD Biosciences, Lincoln Park, NJ). Red blood cells were lysed with ACK buffer, washed and resuspended in cDMEM. Total cell numbers per lung were determined by using a haemocytometer and then calculating the cell number per 1.0 gram of tissue.
Flow cytometric analysis of cell surface markers
Single cell suspensions from the lungs were prepared as recently described.15–19 Thereafter cell suspensions from each individual guinea pig were incubated first with antibodies to CD4+ (clone FITC CT7), CD8+ (clone FITC CT6), pan T cell (clone APC CT5), CD45+ (clone RPE IH-1), neutrophils and eosinophils (clone RPE MIL4), B cell (clone FITC MsGP9) antibodies at 4°C for 30 minutes in the dark and after washing the cells with PBS containing 0.1% sodium azide (Sigma-Aldrich).18 An isotype control was utilized in every experiment. Data acquisition and analysis were done using a FACscalibur (BD Biosciences, Mountain View, CA) and CellQuest software (BD Biosciences, San Jose, CA). Compensation of the spectral overlap for each fluorochrome was done using CD4+ or MIL4+ or CD3+ antigens from cells gated in the FSClow versus SSClow; FSCmid/high versus SSCmid/high; SSClow versus MIL4+; SSChigh versus MIL4neg and SSChigh versus MIL4+ region respectively. Analyses were performed with an acquisition of at least T cells 100,000 total events.
Statistical analysis
The Student t-test test was used to assess statistical significance between groups of data. Kaplan Meier log Rank analysis was applied to the survival curves.
Results
Vaccine induced protection
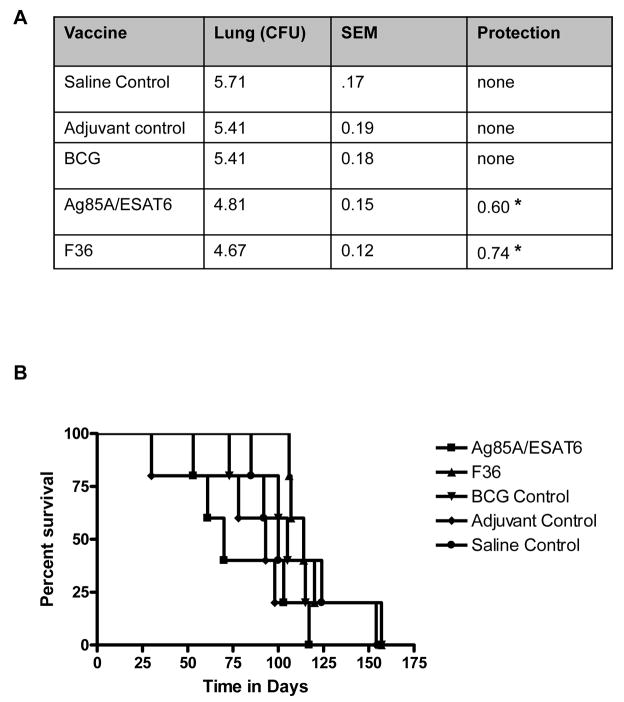
The effects of the post-exposure vaccines on the bacterial load in the lung and animal survival are shown in Figure 1A and B. Because the adjuvant by itself had a mild protective effect [0.4 log] we calculated protection values against this control rather than the saline control. The F36 fusion and the Ag85A/ESAT6 mixture demonstrated significantly reduced bacterial loads compared to the adjuvant control by 0.74 log [P=0.02] and 0.59 log [P=0.03]. Two other fusions (data not shown) and the BCG controltested were not protective [P>0.05].
Figure 1.
Bacterial growth in the lungs and Kaplan-Meier analysis of the survival of guinea pigs infected with M. tuberculosis and receiving post-exposure vaccines. Bacterial counts in the lungs (panel A), on day 40 from guinea pigs infected with a low dose of M. tuberculosis and receiving post exposure vaccine 10 days after infection were compared. Results are expressed as the average (n=5) of the bacterial load in each group expressed as Log10CFU, standard error mean (SEM) and protection. Median survival days (panel B) of Hartley guinea pigs (n=10) vaccinated with, Ag85/ESAT6 (solid square), F36 (solid triangle), BCG control (solid inverted triangle), adjuvant control (solid diamond), and saline control (solid circle) are compared.
We then studied a separate set of animals to determine if the post-exposure vaccines had any effect on the subsequent survival time of the infected animals. As shown in Figure 1B, there was a definite trend towards increased survival in guinea pigs vaccinated with F36, but soon after day 110 these animals also started to die, and were subsequently not statistically significant [P=0.057] by Kaplan Meier analysis. It is also important to note that the animals immunized with the Ag85A/ESAT-6 vaccine showed a trend for decreased survival.
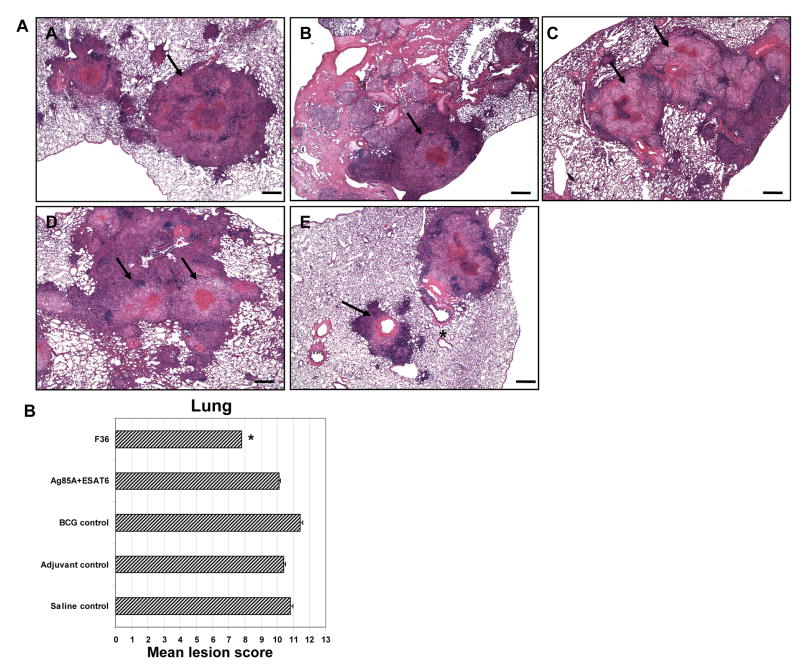
Differences in the lung granulomatous response with post-exposure vaccinated guinea pigs
The differences in the relative size and lesion progression on day 40 in the lungs of guinea pigs infected with M. tuberculosis and 10 days later vaccinated with the saline control (Figure 2A, A), adjuvant control (Figure 2A, B), BCG control (Figure 2A, C), Ag85A+ESAT6 (Figure 2A, D) and F36 (Figure 2A, E) are shown. In addition, the mean total lesion scores for each group were calculated as described in the materials and methods section (Figure 2B). On day 40 of the infection, interestingly, the BCG control vaccine showed the worst lung pathology denoted by increased lesion size, coalescing inflammatory granulomas, extensive necrosis and fibrosis and an increased lesion score. Similar lung pathology and lesion scores were present in the saline control, adjuvant control, and Ag85A+ESAT6 which consisted of well-delineated foci of granulomatous inflammation characterized by sheets of epithelioid macrophages and occasional multinucleated giant cells mixed with fewer numbers of lymphocytes, plasma cells and occasional neutrophils and eosinophils with a moderate amount of necrosis. The saline control, adjuvant control, Ag85A+ESAT6 and BCG control lesion scores were not significantly different [P>0.05] from one another. The animals receiving the F36 fusion protein vaccine showed smaller lesion size, reduce inflammatory infiltrates and significantly reduced lesion scores [P<0.02] compared to the adjuvant control.
Figure 2.
Light photomicrographs of lungs (panel A, A–E) from representative guinea pigs that were guinea pigs infected with M. tuberculosis and receiving post-exposure vaccines saline control (A, A), adjuvant control (A, B), BCG control (A, C), Ag85A+ESAT6 (A, D) and F36 (A, E) on day 40 are shown. [bar denotes H&E staining, 20X]. The lesion scores (panel B) of lungs were calculated as described in Materials and methods section for all the four groups on day 40 of the infection. The scores are presented as total mean lesion values. On day 40, smaller lesions (arrows) and reduced lesion scores were seen in the animals vaccinated with the F36 fusion protein compared to the saline control, adjuvant control, BCG control, Ag85A+ESAT6. Results are expressed as the mean lesion scores (±SEM, n=4). (Student t-test, *p≤0.05) compared to adjuvant control guinea pigs.
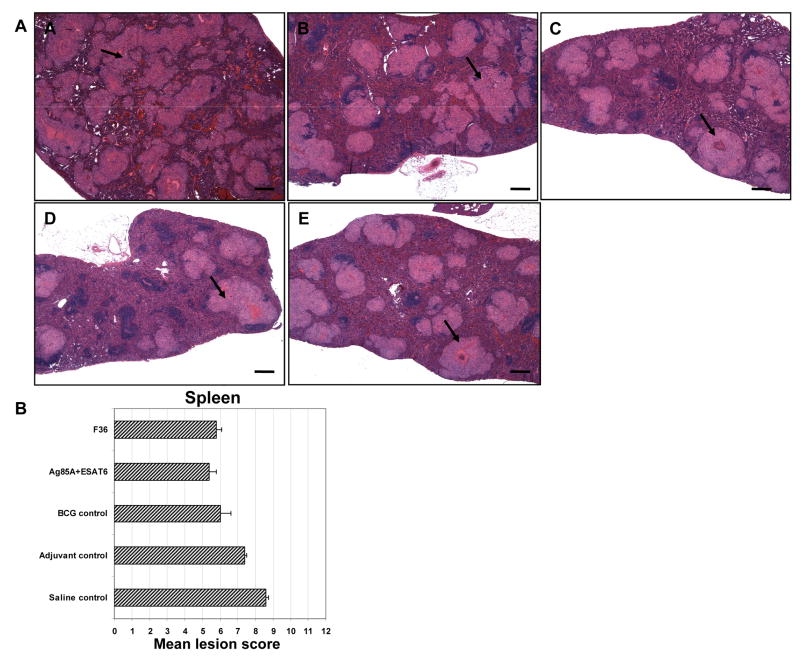
Differences in the spleen granulomatous response with post-exposure vaccinated guinea pigs
The differences in the relative size and lesion progression on day 40 in the spleens of guinea pigs infected with M. tuberculosis and 10 days later vaccinated with the saline control (Figure 3A, A), adjuvant control (Figure 3A, B), BCG control (Figure 3A, C), Ag85A+ESAT6 (Figure 3A, D) and F36 (Figure 3A, E) are shown. In addition, the mean total lesion scores for each group were calculated as described in the materials and methods section (Figure 3B). The lesion scores reflected more spleen lesion development in the saline control and adjuvant control guinea pigs compared to the BCG control, F36 and Ag85/ESAT6 in post-exposure vaccinated guinea pigs. Although, the BCG control, F36 and Ag85/ESAT6 vaccinated guinea pigs showed reduced lesion scores compared to the saline control and adjuvant control these values and were not statistically significant [P>0.05].
Figure 3.
Light photomicrographs of spleens (panel A, A–E) from representative guinea pigs that were guinea pigs infected with M. tuberculosis and receiving post-exposure vaccines saline control (A, A), adjuvant control (A, B), BCG control (A, C), Ag85A+ESAT6 (A, D) and F36 (A, E) on day 40 are shown. [bar denotes H&E staining, 20X]. The lesion scores (panel B) of spleens were calculated as described in Materials and methods section for all the four groups on day 40 of the infection. The scores are presented as total mean lesion values. On day 40, smaller lesions (arrows) and reduced lesion scores were seen in the animals post-exposure vaccinated with the BCG control, F36 fusion protein and Ag85/ESAT6 compared to the saline control and adjuvant control. Results are expressed as the mean lesion scores (±SEM, n=4). (Student t-test, *p≤0.05) compared to adjuvant control guinea pigs.
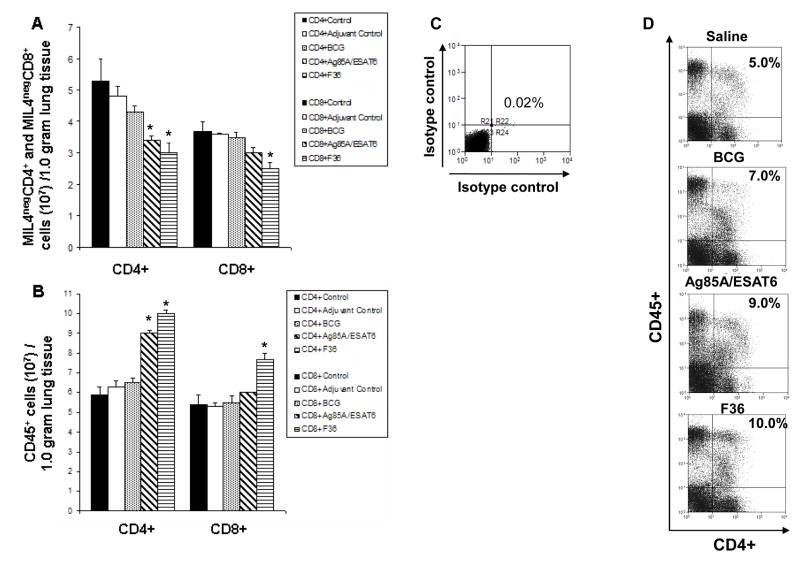
Protection was associated with an increase in lung CD4+ cells expressing CD45+
We have recently developed a flow cytometric method with which to analyze the influx of T cell populations into the infected lungs, and our studies18, 19 indicate that CD45+ expression can be used to potentially track activated T cells. Previous studies evaluating protective immunity in animals receiving a single BCG vaccination prior to infection with M. tuberculosis showed protection was associated with reduced bacterial loads and reduced numbers of CD4+ and CD8+ T cell influx into the lungs. In addition, those CD4+ and CD8+ T cells coming into the lungs of animals demonstrated an increased ability to express CD45+ in BCG vaccinated animals, compared to the non-vaccinated saline controls.19
As shown in Figure 4A, on day 40 of the infection we observed significantly reduced numbers of CD4+ T cells in the lungs of guinea pigs receiving the post-exposure vaccines Ag85A/ESAT6 [P=0.03] and F36 [P=0.02] compared to the adjuvant control. Although reduced numbers of CD8+ T cells were observed in the lungs of guinea pigs receiving the post-exposure vaccines Ag85A/ESAT6 [P=0.06] and F36 [P=0.04] only the F36 was significant. These reduced T cell numbers observed in the Ag85/ESAT6 and F36 post-exposure vaccinated animals was coincident with an observed decline in bacterial numbers. Saline control, adjuvant control and BCG control animal’s demonstrated increased numbers of CD4+ and CD8+ T cells, reflective of the increased lung pathology, increased inflammatory cellular infiltration, increased lesion score and disease progression.
Figure 4.
Numbers of T cell expressing CD45+ in the lungs of guinea pigs infected with M. tuberculosis and receiving post-exposure vaccines. Lungs obtained from guinea pigs infected with M. tuberculosis and receiving post-exposure vaccines saline control (solid bar), adjuvant control (open bar), BCG control (dotted bar), Ag85A+ESAT6 (hatched bar) and F36 (line bar) on day 40 are shown. Guinea pig lungs (n=5) were assayed by flow cytometry, and numbers of cells per 1.0 gram of tissue were calculated from these assays. Panels A show the total numbers of MIL4neg CD4+ cells and MIL4neg CD8+ cells respectively. Panels B show the totalcells/1.0 gram of tissue of CD4+ CD45+ in the lungs of post-exposure vaccinated guinea pigs. Panel C and D shows a representative flow cytometric dot plot from isotype control and guinea pigs receiving post-exposure vaccines saline control, adjuvant control, BCG control, Ag85A+ESAT6 and F36. Results are expressed as the mean cells/1.0 gram of tissue of each analyzed cell population (±SEM, n=4). (Student t-test, *p≤0.05) compared to adjuvant control guinea pigs.
The up-regulation of CD45 (leukocyte common antigen) molecules on T cells indicates signal transduction of antigen receptor signalling during immune responses and hence is an indication of T cell activation.21 We took advantage of an available monoclonal antibody to evaluate the percentage of cells expressing CD45+ on CD4+ and CD8+ T cells over the course of the infection in the post-exposure vaccinated guinea pigs. As shown in Figure 4B, significantly increased expression of CD45+ on both CD4+ [P=0.01] and CD8+ T cells [P=0.03] was present in the F36 post-exposure vaccinated animals compared to the adjuvant control. The Ag85A/ESAT6 post-exposure vaccinated animals demonstrated a significant increase in CD45+ expression on CD4+ T cell [P=0.03], however, CD8+ T cells [P=0.06] were not significantly increased compared to the adjuvant control. Representative flow cytometric plots are shown in Figure 4C isotype control and Figure 4D showing the increased percentages of CD4+CD45+ expression in Ag85A/ESAT and F36 post-exposure vaccinated guinea pigs. It is interesting to note that the CD45 expression shown in Figure 4D has distinct CD45high and CD45low subpopulations. These two subpopulations exist in the human and mouse as CD45RO [memory cell] and CD45RA [naïve cell] subpopulations and represent functionally different populations. In the guinea pig model little has been done to elucidate the functional role of these CD45high and CD45low subpopulations. However, it warrants future studies to understand the functional roles of these subpopulations of cells in the guinea pig.
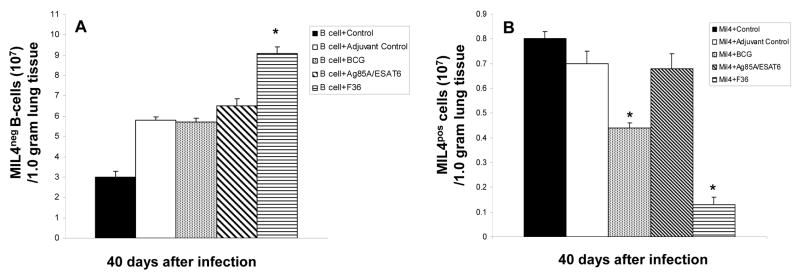
Kinetics of influx of B lymphocytes and heterophils
We previously have demonstrated that both B cells and heterophils enter the lung lesions, accumulating in numbers in infected guinea pigs.18 In addition, we have shown that heterophils enter the lung lesions accumulate in decreased numbers in guinea pigs receiving BCG prior to infection with M. tuberculosis compared to non BCG vaccinated guinea pigs. 18, 19 To determine if these cells could still accumulate in post-exposure vaccinated guinea pigs we analyzed tissues by flow cytometry to clearly delineate the MIL4+ and B cell populations. As shown in Figure 5A, significantly increased numbers of B cells was seen in the F36 post-exposure [P=0.03] vaccinated guinea pigs compared to the adjuvant control. Figure 5B, demonstrates significantly reduced numbers of heterophils [MIL4+] [P=0.02] in the F36 and Ag85A/ESAT [P=0.04] post-exposure vaccinated guinea pigs.
Figure 5.
Numbers of B cell and MIL4+ heterophil (granulocyte) of guinea pigs infected with M. tuberculosis and receiving post-exposure vaccines. Lung obtained from guinea pigs infected with M. tuberculosis and receiving post-exposure vaccines saline control (solid bar), adjuvant control (open bar), BCG control (dotted bar), Ag85A+ESAT6 (hatched bar) and F36 (line bar) on day 40 are shown. Guinea pig lungs (n=4) were assayed by flow cytometry, and numbers of cells per 1.0 gram of tissue were calculated from these assays. Panels A show the total numbers of MIL4neg B cells+ cells and panel B shows the MIL4+ cells respectively. Results are expressed as the numbers of MIL4neg B cells and MIL4+ granulocytes (±SEM, n=4). (Student t-test, *p≤0.05) compared to adjuvant control guinea pigs.
Discussion
The results of this study show that the two vaccine candidates, F36 and Ag85A/ESAT6, significantly reduced the bacterial loads in the lungs after guinea pigs were given a single post-exposure vaccination ten days after a low dose aerosol challenge with virulent M. tuberculosis. The protective properties of these two vaccines were associated with improvements in lung pathology, increased expression of the activation marker CD45+ on CD4+ T cells and reduced heterophil accumulation in the lungs. However, post-exposure vaccination with F36 and Ag85A/ESAT6, does not result in subsequent long-term survival of these guinea pigs. Despite these modest effects, the approach does seem to have promise and warrants further investigation.
In guinea pigs receiving the F36 and Ag85A/ESAT6 post-exposure vaccines lesions were smaller at day 40, but early inflammatory cellular infiltrates and the initial phase of necrosis could be noted. The long term survival study of animals receiving the F36 post-exposure vaccine mortality was delayed, but not quite sufficiently long enough to ensure significance by statistical Kaplan Meier analysis. However, animals immunized with the Ag85A/ESAT-6 vaccine showed a trend for decreased survival.
Murine studies evaluating the safety of post-exposure vaccination of mice infected with M. tuberculosis suggest that the risk of Koch-like reactions is low.22 However, these studies demonstrated exposure of mice with a low dose aerosol of M. tuberculosis and subsequent post-exposure vaccination with BCG evoked increased lung inflammation one month after the vaccinations. In these studies significant reactivation of diseases did not occur and no differences in animal survival were detected in the controls and post-exposure vaccinated mice. 22 Other murine studies confirm these results as delivery of immunotherapeutic vaccines after infection with M. tuberculosis results in no changes in bacterial load and pathology during infection.4 The one notable disadvantage of the mouse model is that the pulmonary and extra-pulmonary pathology lacks early granuloma necrosis which is an important morphologic feature present in guinea pigs and humans.18, 19 The pathological differences in the murine and guinea pigs models may be the reason for the decreased guinea pig survival during post-exposure vaccination.
The small ESAT molecule is a primary T cell target early in the course of the infection, and here two vaccines, the first a mixture of Ag85A and ESAT, and the second a fusion of Rv1411 and ESAT [F36], were both effective in reducing the lung bacterial load and inducing increased CD4+ expression of the activation marker CD45+. The F36 fusion is a polyprotein made using the lipoprotein Rv1411 at the N-terminus and expressed in M. smegmatis. This process ensures correct acylation and glycosylation of the molecule, resulting in a recombinant vaccine that is a potent TLR-2 agonist, driving a substantial IL-12 response by macrophages, 13 thus in turn driving a potent TH1 response. This may imply, when the F36 and Ag85A/ESAT6 vaccines were delivered 10 days after M. tuberculosis infection that these vaccines boost the IL-12 response and in turn cause increased activation of CD4+ T cell expression of CD45+ during this very early stage of the infection.
Unexpectedly, we observed an increase in numbers of B cells in the lungs of the F36 post-exposure vaccinated guinea pigs. B cells are known to produce pro-inflammatory cytokines, and express chemokine receptors such as CXCR5 and CCR7 that may promote their migration to inflammatory sites, although in the mouse model at least there is no evidence these cells interfere with protective immunity.23, 24 Perhaps more importantly, F36 and Ag85A/ESAT6 vaccination reduced heterophil influx in the lung, cells which we think make a central contribution to granuloma inflammation and subsequent necrosis. Heterophils are also strongly associated with TH2 immunity, and play a major role in the immunopathogenesis of asthma and allergic rhinitis.25 In vitro at least, TH2 cytokines can interfere with macrophage activation, decrease toll-like receptor 2 (TLR2) signaling and reduce production of nitric oxide synthase (iNOS).26, 27
Our experiment did not address the issues such as dosing or frequency of vaccine administration. It is possible that the bacterial load could be kept low and the long term survival of the animal increased by additional boosting with the F36 and Ag85A/ESAT6 vaccines. It is also possible that cocktails of vaccines made from fusions of Rv1411 with other key target antigens could be more effective in reducing bacterial loads and improving lung pathology.
Our experience to date however seems to indicate that once the pathologic process in the lungs is fully engaged it is probably impossible to reverse by post-exposure vaccination. On the other hand, chemotherapy clearly can halt and sometimes reverse this process. 19 There is room for optimism however that such information could be applied to an outbreak situation in which exposure is known to be recent. A combination of post-exposure vaccines and chemotherapy could be applied while drug susceptibility testing is completed. In situations where the isolate is unknowingly highly MDR or XDR this approach could in fact be life saving.
Acknowledgments
Funding. This work was supported by U01 AI070456 from the NIAID, NIH.
Footnotes
Competing interests. None
Ethical. Not applicable
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Skeiky YA, Sadoff JC. Advances in tuberculosis vaccine strategies. Nat Rev Microbiol. 2006;4:469–76. doi: 10.1038/nrmicro1419. [DOI] [PubMed] [Google Scholar]
- 2.Kaufmann SH. Is the development of a new tuberculosis vaccine possible? Nat Med. 2000;6:955–60. doi: 10.1038/79631. [DOI] [PubMed] [Google Scholar]
- 3.Orme IM. Preclinical testing of new vaccines for tuberculosis: a comprehensive review. Vaccine. 2006;24:2–19. doi: 10.1016/j.vaccine.2005.07.078. [DOI] [PubMed] [Google Scholar]
- 4.Turner J, Rhoades ER, Keen M, Belisle JT, Frank AA, Orme IM. Effective preexposure tuberculosis vaccines fail to protect when they are given in an immunotherapeutic mode. Infect Immun. 2000;68:1706–9. doi: 10.1128/iai.68.3.1706-1709.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor JL, Turner OC, Basaraba RJ, Belisle JT, Huygen K, Orme IM. Pulmonary necrosis resulting from DNA vaccination against tuberculosis. Infect Immun. 2003;71:2192–8. doi: 10.1128/IAI.71.4.2192-2198.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMurray DN. Determinants of vaccine-induced resistance in animal models of pulmonary tuberculosis. Scand J Infect Dis. 2001;33:175–8. doi: 10.1080/00365540151060743. [DOI] [PubMed] [Google Scholar]
- 7.McMurray DN, Collins FM, Dannenberg AM, Jr, Smith DW. Pathogenesis of experimental tuberculosis in animal models. Curr Top Microbiol Immunol. 1996;215:157–79. doi: 10.1007/978-3-642-80166-2_7. [DOI] [PubMed] [Google Scholar]
- 8.Ly LH, Russell MI, McMurray DN. Cytokine profiles in primary and secondary pulmonary granulomas of Guinea pigs with tuberculosis. Am J Respir Cell Mol Biol. 2008;38:455–62. doi: 10.1165/rcmb.2007-0326OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palanisamy GS, Smith EE, Shanley CA, Ordway DJ, Orme IM, Basaraba RJ. Disseminated disease severity as a measure of virulence of Mycobacterium tuberculosis in the guinea pig model. Tuberculosis. 2008;00:000–000. doi: 10.1016/j.tube.2007.12.003. [E-published] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Basaraba RJ, Smith EE, Shanley CA, Orme IM. Pulmonary lymphatics are primary sites of Mycobacterium tuberculosis infection in guinea pigs infected by aerosol. Infect Immun. 2006;74:5397–401. doi: 10.1128/IAI.00332-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Basaraba RJ, Dailey DD, McFarland CT, Shanley CA, Smith EE, McMurray DN, et al. Lymphadenitis as a major element of disease in the guinea pig model of tuberculosis. Tuberculosis. 2006;86:386–94. doi: 10.1016/j.tube.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Turner OC, Basaraba RJ, Orme IM. Immunopathogenesis of pulmonary granulomas in the guinea pig after infection with Mycobacterium tuberculosis. Infect Immun. 2003;71:864–71. doi: 10.1128/IAI.71.2.864-871.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang B, Henao-Tamayo M, Harton M, Ordway-Rodrigues D, Shanley CA, Basaraba RJ, et al. A Toll-like Receptor-2 directed fusion protein vaccine against tuberculosis. Clin Vaccine Immunol. 2007;14:902–906. doi: 10.1128/CVI.00077-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basaraba RJ, Izzo AA, Brandt L, Orme IM. Decreased survival of guinea pigs infected with Mycobacterium tuberculosis after multiple BCG vaccinations. Vaccine. 2006;24:280–286. doi: 10.1016/j.vaccine.2005.07.103. [DOI] [PubMed] [Google Scholar]
- 15.Ordway D, Costa L, Martins M, Silveira H, Amaral L, Arroz MJ, et al. Increased Interleukin-4 Production by CD8 and T Cells in Health-Care Workers Is Associated with the Subsequent Development of Active Tuberculosis. J Infect Dis. 2004;190:756–766. doi: 10.1086/422532. [DOI] [PubMed] [Google Scholar]
- 16.Ordway DJ, Pinto L, Costa L, Martins M, Leandro C, Viveiros M, et al. Gamma delta T cell responses associated with the development of tuberculosis in health care workers. FEMS Immunol Med Microbiol. 2005;43:339–350. doi: 10.1016/j.femsim.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 17.Wilcox CEDB, Butter C, Willoughby DA, Turk JL. Differential expression of guinea pig class II major histocompatibility complex antigens on vascular endothelial cells in vitro and in experimental allergic encephalomyelitis. Cell Immunol. 1989;120:82–91. doi: 10.1016/0008-8749(89)90176-7. [DOI] [PubMed] [Google Scholar]
- 18.Ordway D, Palanisamy G, Henao-Tamayo M, Smith EE, Shanley CA, Orme IM, et al. The cellular immune response to Mycobacterium tuberculosis infection in the guinea pig. J Immunol. 2007;179:2532–2541. doi: 10.4049/jimmunol.179.4.2532. [DOI] [PubMed] [Google Scholar]
- 19.Ordway D, Henao-Tamayo M, Shanley C, Smith EE, Palanisamy GS, Wang B, et al. The influence of BCG vaccination on the cellular immune response in immune guinea pigs infected with Mycobacterium tuberculosis. Clin Vaccine Immunol. 2008;15:1248–1258. doi: 10.1128/CVI.00019-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lenaerts AJ, Hoff D, Aly S, Ehlers S, Andries K, Cantarero L, et al. Location of persisting mycobacteria in a Guinea pig model of tuberculosis revealed by r207910. Antimicrob Agents Chemother. 2007;51:3338–45. doi: 10.1128/AAC.00276-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hart IJ, Schafer H, Scheper RJ, Stevenson GT. Subpopulations of guinea-pig T lymphocytes defined by isoforms of the leucocyte common antigen. Immunology. 1992;77:377–84. [PMC free article] [PubMed] [Google Scholar]
- 22.Derrick SC, Dheenadhayalan V, Yang A, Kolibab K, Morris SL. The safety of post-exposure vaccination of mice with Mycobacterium tuberculosis. Vaccine. 2008 Sept 19; doi: 10.1016/j.vaccine.2008.09.011. Epub in press. [DOI] [PubMed] [Google Scholar]
- 23.Kahnert A, Hopken UE, Stein M, Bandermann S, Lipp M, Kaufmann SH. Mycobacterium tuberculosis triggers formation of lymphoid structure in murine lungs. J Infect Dis. 2007;195:46–54. doi: 10.1086/508894. [DOI] [PubMed] [Google Scholar]
- 24.Johnson CM, Cooper AM, Frank AA, Bonorino CB, Wysoki LJ, Orme IM. Mycobacterium tuberculosis aerogenic rechallenge infections in B cell-deficient mice. Tuber Lung Dis. 1997;78:257–261. doi: 10.1016/s0962-8479(97)90006-x. [DOI] [PubMed] [Google Scholar]
- 25.Wardlaw AJMR, Kay AB. Eosinophils: Biology and role in disease. Adv Immunol. 1995;60:151–266. doi: 10.1016/s0065-2776(08)60586-6. [DOI] [PubMed] [Google Scholar]
- 26.Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 27.Rook GA, HPR The pathogenesis of tuberculosis. Annu Rev Microbiol. 1996;50:259–284. doi: 10.1146/annurev.micro.50.1.259. [DOI] [PubMed] [Google Scholar]