Blocking HVEM–LIGHT interactions on T cells reduces the persistence of antigen-specific memory T cell populations after secondary expansion through decreased Akt activity and loss of Bcl-2 expression.
Abstract
Memory T helper cells (Th cells) play an important role in host defense against pathogens but also contribute to the pathogenesis of inflammatory disorders. We found that a soluble decoy lymphotoxin β receptor (LT-βR)–Fc, which can block tumor necrosis factor (TNF)–related ligands LIGHT (TNFSF14) and LT-αβ binding to the herpesvirus entry mediator (HVEM) and the LT-βR, inhibited the accumulation of memory Th2 cells after antigen encounter and correspondingly reduced inflammatory responses in vivo. Showing that this was a function of the receptor for LIGHT, antigen-specific memory CD4 T cells deficient in HVEM were also unable to persist, despite having a normal immediate response to recall antigen. HVEM−/− memory Th2 cells displayed reduced activity of PKB (protein kinase B; Akt), and constitutively active Akt rescued their survival and restored strong inflammation after antigen rechallenge. This was not restricted to Th2 memory cells as HVEM-deficient Th1 memory cells were also impaired in surviving after encounter with recall antigen. Furthermore, the absence of LIGHT on T cells recapitulated the defect seen with the absence of HVEM, suggesting that activated T cells communicate through LIGHT–HVEM interactions. Collectively, our results demonstrate a critical role of HVEM signals in the persistence of large pools of memory CD4 T cells.
After antigen recognition, naive T cells expand and differentiate into a large pool of effector T cells. Most of the effector T cells die during a phase of contraction after antigen is no longer available; however, a small proportion survive and differentiate into memory T cells that confer protective immunity to the host (Seder and Ahmed, 2003; McKinstry et al., 2008). In some situations, memory T cells also contribute to the development of inflammatory and autoimmune disease (Bradley et al., 2000; Kuchroo et al., 2002). The overall size of the initial memory T cell pool is determined by several factors, including the strength of naive T cell activation, the extent of primary clonal expansion, and the survival of effector T cells during the contraction phase of the primary response. Many studies have clearly demonstrated that co-stimulatory members of the Ig superfamily, like CD28 and ICOS (inducible co-stimulator), and members of the TNF receptor (TNFR) superfamily (TNFRSF), like CD27, OX40 (CD134), and 4-1BB (CD137), can greatly impact the generation of memory CD4 and CD8 T cells, primarily by supporting this clonal expansion of naive T cells and the accumulation of effector populations (Croft, 2003, 2009; Watts, 2005).
Once formed, memory T cells, as a population, need to persist for a long time in the absence of antigen and respond rapidly upon antigen reexposure. Common γ chain cytokines such as IL-7 and IL-15 have been shown to support the maintenance of memory T cells after antigen is no longer available (Lenz et al., 2004; Purton et al., 2007). However, the factors regulating the expansion and persistence of memory cells upon secondary encounter with antigen are less well studied. After recall antigen stimulation, the memory T cell pool also expands to a great size, and again a proportion of these secondary effector T cells need to survive long term to maintain future memory. The requirement for reactivation and homeostasis of memory CD4 T cells has also been thought to require co-stimulatory signals, but the use and dependence on such molecules might be more restricted than in the primary response. In this regard, at least one study has suggested that memory CD4 T cell recall responses were less dependent on co-stimulation by B7 and CD40 compared with their naive counterparts (London et al., 2000). However, rather than becoming co-stimulation independent, memory CD4 T cells may shift to being more reliant on inducible co-stimulatory molecules like ICOS and OX40 that are up-regulated on these cells upon reactivation (Gonzalo et al., 2001; Salek-Ardakani et al., 2003; Mahajan et al., 2007). Moreover, other members of the TNFRSF such as CD27 and 4-1BB can also determine the extent of secondary expansion of memory T cells, although in these cases, it appears mostly through imprinting future responsiveness during the initial priming of naive T cells (Bertram et al., 2004; Hendriks et al., 2005).
The TNF family members LIGHT (TNFSF14; homologous to lymphotoxins, exhibits inducible expression, competes with HSV glycoprotein D for herpesvirus entry mediator [HVEM], and a receptor expressed by T lymphocytes) and membrane lymphotoxin (LT-αβ) have also been shown to promote initial T cell priming in several different models (Harrop et al., 1998; Mauri et al., 1998; Tamada et al., 2000, 2002; Scheu et al., 2002; Summers-DeLuca et al., 2007) either through HVEM (TNFRSF14) or lymphotoxin β receptor (LT-βR). Whereas LT-βR is largely on APCs such as DCs and on stromal cells and might regulate the function of these cells, thus only indirectly affecting T cell priming, HVEM is expressed on most T cells (Ware, 2009). Ligation of HVEM by LIGHT can provide signals that also impact activation, differentiation, or survival of naive CD4 and CD8 T cells (Harrop et al., 1998; Mauri et al., 1998; Tamada et al., 2000; Scheu et al., 2002; Xu et al., 2007), possibly through targeting the induction of NF-κB and AP-1 (Marsters et al., 1997; Harrop et al., 1998). In contrast, HVEM can also bind the inhibitory molecules BTLA (B and T lymphocyte attenuator) or CD160, and these molecules on T cells can recruit the tyrosine phosphatases SHP-1 and SHP-2, which subsequently attenuate TCR signaling (Watanabe et al., 2003; Sedy et al., 2005; Cai and Freeman, 2009). Therefore, HVEM might display a dual functional activity during primary responses depending on ligand availability and might positively or negatively impact memory T cell generation.
Whether LIGHT or HVEM controls the secondary response of memory T cells or their homeostasis after antigen reencounter is not known. In this study, we performed a systematic analysis to identify the precise function of these molecules in recall responses of CD4 T cells. We mainly focused on Th2 cells as prior data have shown that these are highly dependent on molecules like OX40 and ICOS for their reactivation (Gonzalo et al., 2001; Salek-Ardakani et al., 2003). In contrast to the function of these latter molecules that support expansion of memory T cells after antigen encounter, the presence or absence of HVEM on Th cells had no effect on their proliferation and immediate accumulation and function during recall responses. However, blocking of the HVEM–LIGHT interactions or the absence of HVEM on T cells severely reduced the persistence of antigen-reactive memory T cell pools after their secondary expansion. Th1 memory cells were similarly impaired when HVEM could not be expressed. This was found to correlate with reduced activity of PKB (protein kinase B; Akt) and an inability to maintain expression of Bcl-2. Adoptive transfer experiments also revealed the importance of LIGHT–HVEM interactions between neighboring T cells in regulating the size of persisting T cell memory populations. Thus, HVEM and its partner LIGHT play a pivotal role in the persistence of memory Th cells after antigen reactivation, which provides novel strategies for modulating adaptive immunity during inflammatory/allergic reactions.
RESULTS
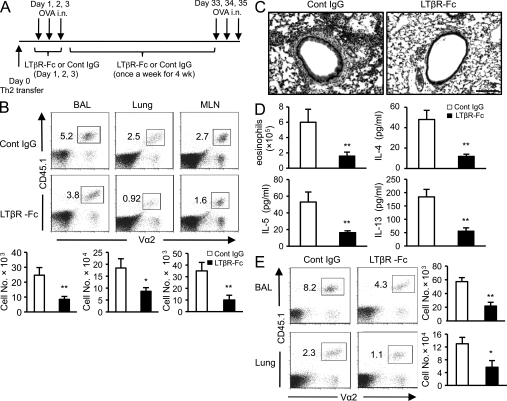
Administration of LT-βR fusion protein suppresses the persistence of memory Th2 cells
LIGHT binds HVEM and LT-βR, and LT-αβ additionally binds LT-βR, suggesting possible common activities of these molecules. Their function in regulating the response of memory T cells is unknown, and so we set up a model to specifically focus on already primed T cell populations to determine whether LIGHT, HVEM, or LT-αβ might control their activity. OVA-specific Th2 cells were generated from naive CD4+ TCR transgenic cells in vitro, rested, and then transferred into CD45.2+ congenic mice. A feature of primed/memory T cells is their ability to respond to soluble antigen in the absence of adjuvant. We therefore challenged the recipient mice with soluble OVA given intranasally (i.n.) over 3 d (Fig. 1 A). To test the effects of blocking the interactions of LIGHT or LT-αβ on these Th2 populations, LT-βR fusion protein (LT-βR–Fc) or control human IgG was given at the time of i.n. OVA challenge. Interestingly, the accumulation of donor Th2 cells was similar between LT-βR–Fc- and control IgG–treated groups immediately after the OVA challenges, and this was regardless of whether the cells were analyzed in the lung or draining LNs (Fig. S1 A). This result implied that none of these pathways regulated the immediate reactivity of Th2 cells to recall antigen.
Figure 1.
LT-βR fusion protein suppresses the accumulation of memory Th2 cells. (A) Experimental protocol. OVA-specific Th2 cells were generated in vitro from CD45.1+ OT-II mice as described in Material and methods. Rested Th2 cells (>99% CD4+Vα2+Vβ5+) were transferred into naive WT or LT-βR−/− CD45.2+ congenic mice. Recipients were challenged with soluble OVA i.n. on a consecutive 3 d. 4 wk later, all mice were rechallenged i.n. with OVA on a consecutive 3 d. Groups of mice were treated with either human IgG or 100 µg LT-βR–Fc as indicated. Samples were collected 24 h after the last OVA challenge. (B) The percentage (top) and absolute numbers (bottom) of donor (CD45.1+Vα2+) memory Th2 cells 24 h after the second recall response in BAL, lung, and MLNs of WT mice. Results are the mean ± SD from six to eight mice. (C) Representative H&E-stained lungs sections from WT mice treated with control (Cont) IgG or LT-βR–Fc. Bar, 100 µm. (D) Numbers of BAL eosinophils and levels of BAL cytokines (IL-4, IL-5, and IL-13) from WT mice. (E) The percentage (left) and absolute numbers (right) of donor Th2 memory cells 24 h after the second recall response in BAL and lungs of LT-βR−/− mice. (D and E) Mean values ± SD from four to six mice per group and representative of two independent experiments are shown. *, P < 0.01; **, P < 0.001.
To determine whether the interactions might be required for later responses, groups of mice were challenged with i.n. OVA and then were kept for another 4 wk without further antigen challenge but with LT-βR–Fc given once a week during this time (Fig. 1 A). These mice were then challenged again with i.n. OVA to induce a further recall response. Strikingly, the percentage and absolute number of persisting memory T cells were substantially reduced in mice treated with LT-βR–Fc, regardless of whether the cells were in the lung, the airways, or the draining mediastinal LNs (MLNs; Fig. 1 B). Along with the reduced numbers of memory T cells, the inflammatory response in the lung as assessed by histology was markedly inhibited in mice receiving LT-βR–Fc, and airway eosinophilia and Th2 cytokines were similarly reduced (Fig. 1, C and D). However, LT-βR–Fc treatment did not alter the ability of the remaining donor T cells to produce cytokines as intracellular staining (ICS) for IL-5 and IL-13 showed similar levels to those of T cells from control mice (Fig. S1 B). These data demonstrate that blocking LIGHT or LT-αβ inhibited the persistence of memory Th2 cells as a population but did not alter the effector function of individual cells.
Because LT-βR–Fc prevents LIGHT–LT-βR, LIGHT–HVEM, and LT-αβ–LT-βR interactions (Browning, 2008), we wanted to address which pathway was the primary mediator regulating the persistence of the memory cells. To address this question, in vitro generated Th2 cells were adoptively transferred into LT-βR−/− mice, and LT-βR–Fc or control IgG was administrated as in Fig. 1 (B–D). In this system, the LT-αβ–LT-βR pathway is disrupted, but the LIGHT–HVEM pathway is intact, as T cells do not express LT-βR (Force et al., 1995; Murphy et al., 1998) and the host also could not provide LT-βR. A higher number of total donor T cells was found in the lungs and airways of these mice because they do not possess LNs (Fütterer et al., 1998), resulting in greater trafficking to this organ. However, similar to a WT host (Fig. 1 B), the percentage and absolute number of memory Th2 cells were significantly reduced in LT-βR−/− hosts treated with LT-βR–Fc (Fig. 1 E). This suggested that LIGHT–HVEM interactions have a fundamental role in controlling the persistence of Th2 memory cells after recall antigen stimulation.
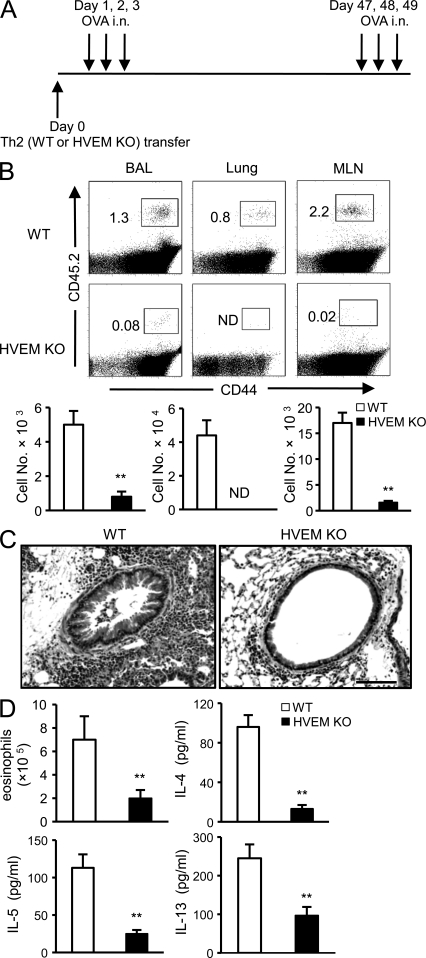
Nonredundant role for HVEM signals in T cells in the persistence of memory Th2 populations
To investigate whether HVEM needed to be expressed on the responding T cells, OVA-specific Th2 cells were generated from naive CD4+ T cells isolated from WT or HVEM−/− OT-II mice (Fig. S2). These cells were then transferred into CD45.1+ congenic WT recipient mice, followed by soluble OVA recall challenges at days 1–3 and 47–49 (Fig. 2 A). Similar to mice treated with LT-βR–Fc, the percentage and absolute number of donor HVEM−/− memory Th2 cells were severely reduced in the airways, lungs, and MLNs of recipient mice after the second round of antigen challenges (Fig. 2 B). Again, showing this was physiologically relevant, analysis of the accompanying inflammatory response showed a profound reduction of cellular infiltrates and eosinophils in the lung compared with mice receiving WT T cells, and levels of Th2 cytokines in the airways were markedly lower (Fig. 2, C and D). To show this was not simply a function of the TCR transgenic system, HVEM−/− mice primed with OVA/alum and challenged with recall antigen also revealed defective endogenous memory Th2 responses (Fig. S3). Altogether, these results demonstrate that HVEM expressed on the CD4 T cell is required for the long-term accumulation of high frequencies of memory T cells that can mediate allergic inflammatory responses.
Figure 2.
T cell–expressed HVEM is required for accumulation of large populations of memory Th2 cells. (A) OVA-specific Th2 cells were generated in vitro from CD45.2+ WT or HVEM−/− OT-II mice. After resting, Th2 cells (>99% CD4+Vα2+Vβ5+) were injected i.v. into naive WT CD45.1+ congenic mice. Recipient mice were subsequently challenged with soluble OVA i.n. on a consecutive 3 d. 6 wk later, all mice were rechallenged a second time with i.n. OVA on a consecutive 3 d. Samples were collected 24 h after the last OVA challenge. (B) The percentage and absolute numbers of donor memory Th2 cells in BAL, lungs, and MLNs. ND, not detected. (C) Representative H&E-stained lungs sections from the recipients of WT or HVEM−/− Th2 cells. Bar, 100 µm. (D) Numbers of eosinophils and levels of Th2 cytokines (IL-4, IL-5, and IL-13) in BAL of recipients of WT and HVEM−/− Th2 cells. (B and D) Results are the mean ± SD from six to eight mice per group and representative of two independent experiments. **, P < 0.001.
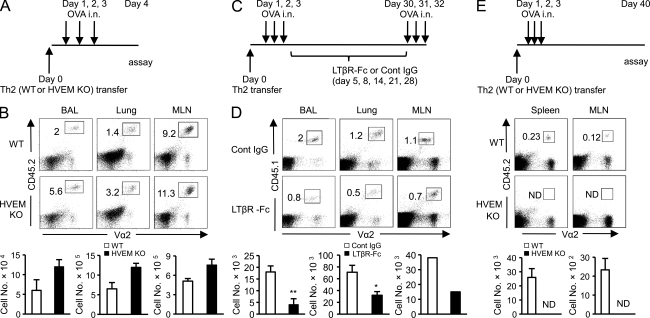
HVEM signals are dispensable for the expansion and function of Th2 cells but determine the survival of effector cells that transition into memory populations
The severe reduction of the memory Th2 population in the absence of HVEM raised the question of whether HVEM also controlled initial expansion of Th2 cells to recall antigen. Our initial data with LT-βR–Fc suggested that this was not the case (Fig. S1 A). To address this more carefully, naive WT or HVEM−/− OVA-specific Th2 cells were transferred into CD45.1+ congenic WT mice as in Fig. 2, and their response was tracked immediately after the recipients were exposed to i.n. antigen (Fig. 3 A). We have previously shown that in this scenario, effector T cells expand in number in the draining LNs of the lung and then migrate to the lung to induce inflammation (Salek-Ardakani et al., 2003). In contrast to our previous results assessing the long-term response (Fig. 2), a modest increase in accumulation of HVEM−/− Th2 cells was found in the airways, lungs, and MLNs 1 d after the last antigenic challenge, without any obvious defect (Fig. 3 B). In parallel, recipients of HVEM−/− Th2 cells exhibited a relatively normal airway inflammatory response, with similar numbers of eosinophils and similar levels of Th2 cytokines (Fig. S4 A). Further confirming that HVEM was not essential for effector function, direct analysis of the donor T cells revealed little production of IFN-γ and IL-17 and normal production of IL-2 and Th2 cytokines during the initial phase of antigen encounter (Fig. S4 B). Flow analyses also did not reveal significant differences in the expression of effector/differentiation markers such as CD27, CD44, CD62L, CD127, and CXCR5 between WT and HVEM−/− donor cells (Fig. S4 C), suggesting that defective long-term survival was not linked to HVEM controlling the early ratio of central/effector memory subsets formed.
Figure 3.
HVEM is not required for the expansion of Th2 cells to recall antigen but supports the persistence of memory T cell populations. (A) Protocol for B. Th2 cells were generated in vitro from CD45.2+ WT or HVEM−/− OT-II mice as in Fig. 2. Rested Th2 cells were transferred i.v. into congenic CD45.1+ WT mice, which were challenged with soluble OVA i.n. on a consecutive 3 d. (B) The percentage and absolute numbers of donor Th2 memory cells in BAL, lungs, and MLNs on day 4, 24 h after the last OVA challenge. (C) Protocol for D. OVA-specific Th2 cells were generated in vitro from CD45.1+ OT-II mice and transferred into naive WT CD45.2+ congenic mice as in Fig. 1. Recipients were challenged with soluble OVA i.n. on a consecutive 3 d. 4 wk later, all mice were rechallenged i.n. with OVA on a consecutive 3 d. Groups of mice were treated with either human IgG or 150 µg LT-βR–Fc as indicated. (D) The percentage (top) and absolute numbers (bottom) of donor (CD45.1+Vα2+) memory Th2 cells 24 h after the second recall response in BAL, lung, and pooled MLNs of WT mice. (B and D) Results are the mean ± SD from four to five mice per group and representative of two independent experiments. (E) Recipients as in A were challenged with OVA for 3 d. 40 d later, the percentage (middle) and absolute numbers (bottom) of donor (CD45.2+Vα2+) WT and HVEM−/− memory Th2 cells were analyzed in spleen and MLNs. Results are the mean ± SD from six to eight mice. Cont, control; ND, not detected. *, P < 0.01; **, P < 0.001.
To show that HVEM signals were active at the peak or after this initial effector response, WT Th2 cells were transferred into congenic hosts, and LT-βR–Fc treatment was started 2 d after the last i.n. OVA challenge (i.e., day 5 after Th2 transfer; Fig. 3 C). The percentage and absolute number of persisting memory T cells after a further recall response were again significantly reduced in the mice treated with LT-βR–Fc, regardless of whether the cells were examined in the lung, the airways, or the draining LNs (Fig. 3 D). Additionally, recipients of HVEM−/− Th2 cells were challenged with antigen as before (Figs. 2 A and 3 A), and then the subsequent memory T cell population was analyzed after 40 d but without another recall challenge (Fig. 3 E). WT Th2 cells survived over this time period and retained their cytokine profiles (Fig. S5), but this resting memory population did not develop efficiently when HVEM was absent (Fig. 3 E). Therefore, late HVEM–LIGHT interactions at or after the peak expansion phase of the recall response determine the number of T cells that survive during the transition from memory effector back to resting memory cell.
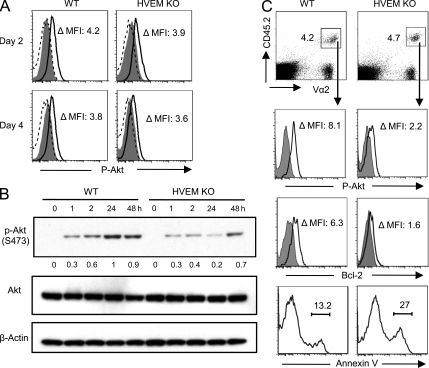
HVEM signals in T cells prolong Akt activity during recall responses and support T cell survival
Previously, we showed that in the absence of another TNFRSF molecule, OX40, antigen-activated CD4 T cells were short-lived because the activity of PKB (also known as Akt) was not maintained (Song et al., 2004). HVEM recruits the same intracellular TRAF (TNFR-associated factor) adaptor proteins as OX40, suggesting possible similarities in signaling. To see whether the absence of HVEM could also affect the activity of Akt, we initially stimulated naive WT and HVEM−/− OT-II T cells in vitro with antigen under Th2 conditions, and the phosphorylation of Akt was analyzed using ICS. Maximum Akt phosphorylation in recently activated naive T cells is observed by day 2 and can be maintained up to day 4 (Song et al., 2004). Over this time, WT and HVEM−/− T cells had comparable levels of phosphorylated Akt (Fig. 4 A). To determine whether HVEM then regulates Akt activation during recall responses, Th2 cells generated from WT and HVEM−/− OT-II CD4 T cells were rested in fresh media and then restimulated with peptide-pulsed APCs. T cells were separated from APCs, and Akt phosphorylation was analyzed. Although initial phosphorylation was similar over 1–2 h, HVEM−/− T cells were deficient in expressing the phosphorylated form of Akt at later times (Fig. 4 B). Thus, HVEM directly or indirectly regulates Akt activity in Th2 cells undergoing a recall response to antigen.
Figure 4.
HVEM signals sustain phosphorylation of AKT in Th2 cells during secondary responses and support T cell survival. (A) Naive CD4 T cells from WT or HVEM−/− OT-II mice were cultured with OVA peptide–loaded APCs under Th2 conditions. 2 (top) and 4 d (bottom) later, primed Th2 cells were stained for surface CD4 and intracellular phosphorylated Ser-473 Akt (pAkt; solid line) or isotype control (closed histogram). As controls for pAkt staining specificity, separate groups of Th2 cells were treated with 10 µM LY294002 (a PI3 kinase inhibitor) for the last 2 h of culture and then stained (dashed line). (B) OVA-specific Th2 cells were generated as in A. After 3 d, live cells were rested in complete media without further stimulation for an additional 5 d and then subsequently restimulated with OVA-pulsed APCs. At different times, CD4+ T cells were isolated, and pAkt (Ser-473), total Akt, and β-actin in lysates were analyzed by Western blotting. The amount of phosphorylated Akt was determined by densitometry. (C) OVA-specific Th2 cells were generated as in A. After resting, Th2 cells were transferred into congenic CD45.1+ WT mice, which were subsequently challenged with soluble OVA i.n. on a consecutive 3 d. MLNs were collected 48 h after the last OVA challenge (5 d after transfer) and stained for surface CD45.2, Vα2, and intracellular pAkt, Bcl-2, or annexin V (open histograms). Closed histograms show isotype control staining. Results are representative of at least two independent experiments. MFI, mean fluorescent intensity.
To evaluate whether HVEM also prolonged Akt activity in vivo, rested Th2 cells generated from WT and HVEM−/− OT-II mice were adoptively transferred into congenic WT mice that were subsequently challenged with i.n. OVA over 3 d, as in Fig. 3 A. 2 d after the last OVA challenge (i.e., 5 d after transfer), Akt phosphorylation was analyzed by ICS in donor Th2 cells recovered from MLNs of the recipient mice. Correlating with the in vitro results, we found reduced expression of phosphorylated Akt in HVEM−/− T cells (Fig. 4 C). AKT phosphorylation was not detected 7 d after challenge, indicating that its activation is prolonged in vivo but still transient (Fig. S6 A). Activated Akt can support T cell survival through induction of antiapoptotic molecules (Stahl et al., 2002; Song et al., 2004), so we assessed the expression of Bcl-2, and T cell apoptosis was also analyzed in donor Th2 cells recovered from the MLNs of recipient mice at different time points after antigenic challenge. Paralleling reduced Akt phosphorylation, the absence of HVEM on T cells resulted in lower levels of Bcl-2 and enhanced T cell apoptosis during the later phase of the recall response at and after the peak of effector expansion (days 5–7; Fig. 4 C and Fig. S6 B).
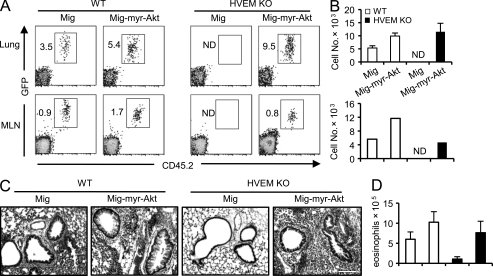
Sustained Akt activity reverses defective survival of HVEM-deficient T cells and restores their ability to promote inflammation
Altogether, these observations implied that sustained Akt activity, brought about by HVEM signaling at a relatively late time in Th2 cells responding to recall antigen, was required to maintain large populations of memory cells. To test this hypothesis, we used a bicistronic GFP retroviral vector expressing active (myristoylated) Akt. WT or HVEM−/− OT-II CD4 T cells were transduced with active Akt or empty vector in the primary Th2 cultures (Fig. S7). Equal numbers of GFP-positive T cells were adoptively transferred into CD45.1+ congenic WT mice that were subsequently challenged with soluble OVA i.n. as in Fig. 3 A. 6 wk after the initial antigen challenge, the donor T cells were evaluated based on expression of the CD45.2 congenic marker and GFP (Fig. 5 A). HVEM−/− T cells transduced with the control vector did not survive as before (Fig. 5, A and B). However, ectopic expression of active Akt completely reversed this defect, and a similar frequency of persisting memory T cells was found in these mice compared with mice that received WT T cells expressing control vector or myr-Akt (Fig. 5, A and B). To show that this effect was physiologically relevant, inflammation was analyzed after mice were further rechallenged with antigen. Severe lung cellular infiltration and airway eosinophilia were found in recipients of HVEM−/− Th2 cells expressing myr-Akt, similar to that observed in recipients of WT Th2 cells (Fig. 5, C and D). Therefore, sustained Akt activation restores the in vivo inflammatory response driven by memory Th2 populations by regulating T cell longevity.
Figure 5.
Active Akt reverses defective survival of HVEM−/− Th2 memory cells. Naive WT or HVEM−/− OT-II cells were stimulated under Th2 conditions, transduced with retroviral vectors expressing either GFP alone (Mig) or GFP with myristoylated Akt (Mig-myr-Akt), and then equivalent numbers of GFP+ cells were transferred into groups of 8–10 naive congenic CD45.1+ WT mice. Recipient mice were challenged with soluble OVA i.n. on a consecutive 3 d. 6 wk later, some mice were analyzed (memory), and some were rechallenged with OVA i.n. on a consecutive 3 d (recall memory). (A and B) The percentage (A) and absolute numbers (B) of donor (Vα2+CD45.2+GFP+) memory Th2 cells 6 wk after the primary OVA challenges (memory) in lung and MLNs. Results are the mean ± SD from four to six individual mice, except for the MLNs which are pooled. ND, not detected. (C) Representative H&E-stained lungs sections from the recipient mice after the recall memory challenge. Bar, 100 µm. (D) Mean numbers of BAL eosinophils ± SD from four to six recipients after the recall memory challenge. Results are representative of two experiments.
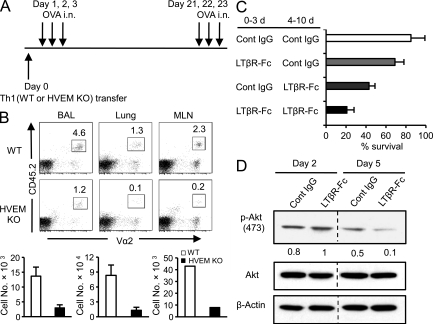
Blocking HVEM–LIGHT interactions between CD4 T cells inhibits their survival
Next, to address whether HVEM was also required for the maintenance of memory Th1 populations, OVA-specific Th1 cells were generated from naive CD4+ T cells isolated from WT or HVEM−/− OT-II mice. These cells were again transferred into CD45.1+ congenic WT recipient mice, followed by soluble OVA recall challenges as in Fig. 2 (Fig. 6 A). Similar to HVEM−/− Th2 cells (Fig. 2), the percentage and absolute number of donor HVEM−/− memory Th1 cells were severely reduced in the airways, lungs, and MLNs of recipient mice (Fig. 6 B), showing that the requirement for HVEM was not restricted to the Th2 phenotype.
Figure 6.
Blocking HVEM–LIGHT interactions between CD4 T cells suppresses their survival. (A) OVA-specific Th1 cells were generated in vitro from CD45.2+ WT or HVEM−/− OT-II mice and transferred into naive WT CD45.1+ congenic mice. Recipient mice were subsequently challenged with soluble OVA i.n. on a consecutive 3 d. 3 wk later, all mice were rechallenged a second time with i.n. OVA on a consecutive 3 d. Samples were collected 24 h after the last OVA challenge. (B) The percentage and absolute numbers of donor memory Th1 cells in BAL, lungs, and pooled MLNs. Results are the mean ± SD from four to five mice per group and representative of two independent experiments. (C) Naive OT-II CD4+ T cells were stimulated with plate-bound anti-CD3 in the absence of APCs over 3 d. After being washed with PBS, cells were resuspended in complete fresh medium and cultured an additional 7 d. LT-βR–Fc or control (Cont) Ig was added for 3 d starting at the beginning of the culture period or during the last 7 d. On day 10, the percentage of T survival was calculated. Data are the mean (±SD) of triplicate cultures, and similar results were obtained in at least two independent experiments. (D) Purified naive OT-II CD4+ T cells were stimulated as in C in the presence of LT-βR–Fc or control Ig. After 2 or 5 d, T cell lysates were analyzed for pAkt (Ser-473), total Akt, and β-actin. Densitometry was performed with 1 as a reference of the highest level of pAkt normalized to actin expression.
Several sources of LIGHT have been described, including immature DCs, monocytes, B cells, and activated T cells (Mauri et al., 1998; Zhai et al., 1998; Yu et al., 1999; Tamada et al., 2000; Duhen et al., 2004). We reasoned that T cells might provide LIGHT to ligate HVEM on neighboring T cells. To initially test whether this was possible, naive CD4+ T cells (CD25−, CD44lo, CD62Lhi) were purified from OT-II mice and stimulated in vitro with immobilized anti-CD3 in the absence of APCs. To block LIGHT–HVEM interaction, LT-βR–Fc was added during T cell activation. In this APC-free system, LT-βR–Fc only targets LIGHT–HVEM because LT-αβ on T cells does not have a receptor to engage. 3 d after stimulation, CD4 T cells proliferated equally, regardless of treatment with LT-βR–Fc or IgG, indicating that LIGHT did not contribute to the primary expansion of T cells (Fig. S8 A). However, when already primed T cells were restimulated with immobilized anti-CD3, those cells cultured with LT-βR–Fc showed reduced proliferation during recall response (Fig. S8 B). To address whether LT-βR–Fc treatment affected T cell survival, naive OT-II T cells were stimulated with anti-CD3 in the absence of APCs for 3 d and then rested in fresh media for an additional 7 d. LT-βR–Fc was added during the initial 3 d, the last 7 d, or during the whole 10 d of culture, and T cell viability was monitored at the end. Blocking LIGHT–HVEM interaction during the early phase of T cell stimulation had little effect, but blocking later significantly diminished long-term survival of CD4 T cells (Fig. 6 C). The addition of LT-βR–Fc for the entire 10 d of culture had the most suppressive effect on T cell survival. Lastly, to evaluate whether this correlated with Akt activity, the T cells from these cultures were harvested at days 2 and 5, and phosphorylation of Akt assessed. At day 2, no difference was detected, but T cells cultured with LT-βR–Fc did not sustain the phosphorylation of Akt at day 5 (Fig. 6 D). Thus, although this was an artificial in vitro system, the results suggested that LIGHT–HVEM interactions between T cells might be functionally relevant to long-term survival in vivo through maintaining Akt activity.
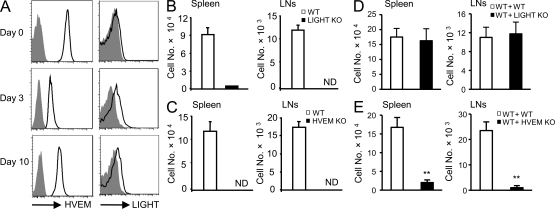
LIGHT–HVEM interactions between CD4 T cells support their long-term survival in vivo
To address whether LIGHT–HVEM signaling between T cells can impact T cell survival in vivo, we first examined the expression of HVEM and LIGHT on T cells. Naive OT-II CD4 T cells were adoptively transferred into congenic WT mice followed by immunization with OVA. HVEM was highly expressed on naive T cells, down-regulated 3 d after antigen stimulation, and then up-regulated by day 10 d. LIGHT was not expressed on naive CD4 T cells but was induced by day 3 after antigen stimulation, and interestingly, expression was maintained up to day 10 after immunization (Fig. 7 A). Thus, LIGHT can be available on T cells to partner with HVEM.
Figure 7.
T cell–expressed LIGHT binding to HVEM supports the generation of memory T cell pools. (A) Purified naive CD45.2+ WT, LIGHT−/−, or HVEM−/− OT-II T cells were adoptively transferred into congenic WT CD45.1+ mice. Before (day 0) and after immunization with OVA (day 3 and 10), the expression of HVEM and LIGHT (open histograms) on donor T cells was examined as described in Materials and methods (closed histograms represent LIGHT and HVEM staining of LIGHT−/− and HVEM−/− OT-II T cells, respectively). (B) Purified naive WT or LIGHT−/− OT-II T cells were adoptively transferred into congenic WT CD45.1+ mice. (C) Purified naive WT or HVEM−/− OT-II T cells were adoptively transferred into congenic WT CD45.1+ mice. (B and C) Recipients were immunized with OVA peptide, and 45 d later, numbers of donor (CD45.2+Vα2+) T cells were determined in spleen and peripheral LNs. (D) Equal numbers of CD45.2+ WT or LIGHT−/− OT-II T cells were cotransferred along with CD45.1+ WT OT-II CD4 T cells into congenic WT CD45.1+ mice. (E) Equal numbers of CD45.2+ WT or HVEM−/− OT-II T cells were cotransferred along with CD45.1+ WT OT-II CD4 T cells into congenic WT CD45.1+ mice. (D and E) After immunization with OVA, numbers of donor CD45.2+ cells were calculated 45 d later. (B–E) Results are the mean ± SD from four individual mice per group and representative of two independent experiments. ND, not detected. **, P < 0.001.
To address whether LIGHT expressed on T cells is functional as a co-stimulatory ligand regulating the development of memory populations, WT or LIGHT−/− OT-II T cells were adoptively transferred into congenic WT mice that were then immunized with OVA. Although WT and LIGHT−/− T cells expanded equivalently within 3 d after activation (Fig. S8 C), few memory T cells were found in recipients of LIGHT−/− T cells 45 d later, regardless of location analyzed (Fig. 7 B). Similar results were also found comparing WT with HVEM−/− T cells, which expanded normally (Fig. S8 D) but failed to generate large numbers of memory cells (Fig. 7 C). Thus, LIGHT and HVEM expression were required in T cells for memory cell generation. To address this issue further and investigate which molecule was the key signaling molecule in antigen-responding T cells, we performed coadoptive transfer experiments. WT or LIGHT−/− (CD45.2+) T cells were cotransferred at a 1:1 ratio with WT (CD45.1+) T cells into WT CD45.1+ mice. Recovery of donor CD45.2+ cells was assessed 45 d after antigen immunization. WT and LIGHT−/− donor T cells generated comparable numbers of long-lived T cells (Fig. 7 D), contrasting with the results of the single transfer of LIGHT−/− T cells (Fig. 7 B). This indicated that the WT T cells (expressing LIGHT) rescued the survival defect of LIGHT−/− T cells, implying that HVEM was the signaling partner. In contrast, when WT and HVEM−/− T cells were cotransferred, few memory cells were generated from the HVEM−/− donors (Fig. 7 E), similar to the defect with the single transfer of HVEM−/− cells (Fig. 7 C). Therefore, these results demonstrate that HVEM is the key co-stimulatory molecule that promotes survival of large pools of memory T cells, through interacting with LIGHT expressed on neighboring antigen-specific T cells.
DISCUSSION
Targeting antigen-experienced T cells may be an effective therapeutic strategy for treatment of ongoing or recurring inflammation. Previous studies have shown that LT-βR–Fc decoy protein has potent suppressive effects in controlling disease in several Th1/Th17 autoimmune models (Mackay et al., 1998; Wu et al., 2001; Tamada et al., 2002; Gommerman et al., 2003), suggesting that LT-αβ–LT-βR, LIGHT–HVEM, or LIGHT–LT-βR interactions (Browning, 2008) might be highly active in promoting inflammation. We now add to our understanding of the importance of these pathways by showing that inflammation driven by primed Th2 cells as well as Th1 cells can be dampened by administration of LT-βR–Fc during antigen recall responses. Studies using LT-βR–deficient mice or in vivo treatment with LT-βR–Fc have shown that LT-βR signaling can control DC homeostasis and function (Gommerman and Browning, 2003; Summers-DeLuca et al., 2007), suggesting that LT-βR signals on APCs could indirectly regulate the recall response of memory T cells. However, we now show an APC-independent mechanism to control inflammation via targeting LIGHT–HVEM interactions between memory T cells responding after recall antigen stimulation.
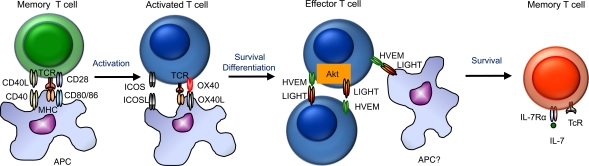
The requirement for co-stimulatory signals for reactivation of antigen-experienced CD4 T cells was initially debated more than a decade ago. We and others suggested that these T cells were more reactive to antigen and TCR signals and less dependent on signals from APC, suggesting a reduced requirement for co-stimulation compared with their naive counterparts (Croft et al., 1994; Viola and Lanzavecchia, 1996; London et al., 2000). However, with more defined assays and the emergence of newer co-stimulatory interactions, this opinion has changed, and several molecules including CD28/B7, OX40/OX40L, and ICOS/ICOSL have been shown to contribute to memory CD4 T cell reactivity in various situations (Rogers et al., 2000; Gonzalo et al., 2001; Salek-Ardakani et al., 2003; Mahajan et al., 2007). Our data now add HVEM and LIGHT to this growing list of molecules essential for some aspect of memory T cell response. In contrast to these aforementioned interactions that primarily determine the extent of secondary expansion and reactivity of memory T cells after antigen reencounter, HVEM–LIGHT signals allow a high frequency pool of T cells to persist after the effector phase of the recall response but with little/no impact on the immediate expansion and functional activity elicited by the recall antigen (Fig. 8).
Figure 8.
Model depicting how HVEM–LIGHT interactions control recall antigen responses, acting at or after the peak phase of expansion of effector T cells, to provide survival signals to allow the persistence of high numbers of memory T cells.
Both HVEM and LIGHT have been reported to function as signaling molecules on T cells. Soluble LIGHT binding to HVEM or endogenous HVEM–LIGHT interactions can have a potent co-stimulatory action in initial T cell priming and early expansion of effector T cells in some situations (Harrop et al., 1998; Mauri et al., 1998; Tamada et al., 2000; Shaikh et al., 2001; Wang et al., 2001). For example, a recent study demonstrated that expression of HVEM on T cells controlled the size of alloreactive CD4 and CD8 T cell pools that formed over a 10-d period in a graft-versus-host disease model (Xu et al., 2007). In contrast, cross-linking LIGHT on T cells has also been shown to enhance T cell proliferation and cytokine production after triggering the TCR (Shi et al., 2002; Wan et al., 2002). In line with these studies, we found that HVEM−/− and LIGHT−/− CD4 T cells displayed identical defects in generating long-lived memory T cells when responding separately in adoptive hosts. The common phenotype indicated that LIGHT–HVEM form a signaling pathway but did not resolve in this setting which molecule served as the signaling element regulating memory T cells. However, when WT and LIGHT−/− T cells were cotransferred and stimulated together in vivo, comparable numbers of long-lived T cells accumulated, which contrasted sharply with the defect when WT and HVEM−/− T cells were cotransferred. These results strongly support the conclusion that HVEM serves as the primary signaling element and also suggest that it is T cell–derived LIGHT that is sufficient to provide the necessary HVEM signal. Our conclusions are also in line with prior data in vitro, which showed that blocking this interaction reduced T cell proliferation to anti-CD3, and data in vivo, in which constitutive expression of LIGHT on T cells resulted in several autoimmune symptoms typical of T cell driven responses (Shaikh et al., 2001; Wang et al., 2001). Based on these observations and our data, we therefore propose a model for Th memory in which engagement of HVEM on these activated cells by trans interaction with LIGHT expressed on adjacent effector T cells provides late co-stimulatory signals that promote T cell survival after the recall immune response is established (Fig. 8). Although expression of LIGHT on APCs such as DCs and B cells also could provide HVEM signals in some scenarios, sustained expression of LIGHT in antigen-responsive T cells clustered in the niche of the T cell zone of secondary and tertiary lymphoid organs is likely to represent a major source of LIGHT, allowing direct T cell–T cell communication.
The precise function of HVEM as either a stimulatory or inhibitory receptor has been the subject of debate for some time. HVEM is ubiquitously expressed on many different types of cells and also can bind to multiple ligands (Cheung et al., 2009b). Although one study showed that blocking HVEM in vitro led to a reduction in T cell proliferation (Wang et al., 2001), another suggested that HVEM−/− T cells were hyper-responsive to anti-CD3–mediated stimulation (Wang et al., 2005). In line with this potential suppressive action, HVEM−/− mice were more susceptible to Con A–mediated T cell–dependent autoimmune hepatitis and myelin oligodendrocyte glycoprotein peptide–induced experimental autoimmune encephalomyelitis (Wang et al., 2005). The explanation for the latter phenotypes is that HVEM can also bind to BTLA and CD160, and these molecules can induce inhibitory signals into T cells when expressed in cis or in trans in T cells (Watanabe et al., 2003; Sedy et al., 2005; Cai and Freeman, 2009; Cheung et al., 2009b). Therefore, the time of availability of LIGHT and other ligands may determine the overall signaling activity of HVEM. We also found some evidence of hyper-responsiveness in the initial response to recall antigen with increased accumulation of HVEM−/− Th2 cells in the airways, lungs, and MLNs (Fig. 3 B). However, over time, a lack of HVEM translated into the loss of memory T cells. This suggests that although BTLA or CD160 might have been active initially, LIGHT is the primary stimulus that dictated the overall size of the antigen-reactive T cell population that subsequently resulted after the antigen cleared.
There are few studies that have addressed the signaling events downstream of HVEM. Cross-linking HVEM on human T cells was found to recruit TRAF adaptor molecules, leading to activation of NF-κB and AP-1 (Marsters et al., 1997; Harrop et al., 1998). Also, activation of HVEM on monocytes induced the phosphorylation of phospholipase Cγ1 after a rapid elevation of intracellular calcium (Heo et al., 2007), and ligation of HVEM by LIGHT induced macrophage migration and smooth muscle proliferation that was associated with the activation of several signaling pathways, including mitogen-activated protein kinases, phosphoinositide 3-kinase/Akt, and NF-κB (Wei et al., 2006). In this study, we found both in vitro and in vivo that HVEM-deficient T cells did not maintain Akt activity during recall responses that paralleled defective expression of the antiapoptotic molecule Bcl-2 and reduced T cell survival. Determining whether HVEM directly recruits Akt to its intracellular tail or enhances TCR-driven Akt activity or only indirectly prolongs Akt activity by regulating the expression of other membrane receptors that can target this pathway requires further analysis. However, defective T cell survival in the absence of HVEM could be fully rescued by ectopic expression of an active form of Akt, indicating the central role of sustaining Akt activation in regulating T cell longevity and the size of persisting memory T cell pools.
In summary, our experiments show a critical role for LIGHT–HVEM signals in the generation and maintenance of long-lived memory Th cell populations after the recall response to soluble antigen. Because both Th2 and Th1 cells have been shown to play a critical role in perpetuating inflammation, our findings indicate that targeting the LIGHT–HVEM pathway may lead to effective therapeutic strategies in which memory Th2 and Th1 cells are pathogenic.
MATERIALS AND METHODS
Mice.
6–8-wk-old female C57BL/6 (CD45.2+) and C57BL/6-SJL (CD45.1+) WT mice were purchased from the Jackson Laboratory. LIGHT-deficient (LIGHT−/−), HVEM-deficient (HVEM−/−), and LT-βR–deficient (LT-βR−/−) mice (CD45.2+) were generated by K. Pfeffer and bred in-house at La Jolla Institute for Allergy and Immunology and have been described previously (Cheung et al., 2009a). OT-II TCR transgenic mice (CD45.2+) were a gift from W. Heath (Walter and Eliza Hall Institute of Medical Research, Melbourne, Australia) and were used as a source of Vα2+Vβ5+ CD4 T cells responsive to the OVA 323–339 peptide (Barnden et al., 1998). CD45.1+ OT-II transgenic mice were generated by backcrossing OT-II mice with CD45.1+ mice. CD45.2+ HVEM−/− and LIGHT−/− OT-II mice were generated in-house by intercrossing. All mice were backcrossed at least 10 times. The experiments reported in this study conform to the principles outlined by the animal Welfare Act and the National Institutes of Health guidelines for the care and use of animals in biomedical research. All experiments were performed in compliance with the regulations of the La Jolla Institute Animal Care committee in accordance with the guidelines by the Association for Assessment and Accreditation of Laboratory Animal Care.
Adoptive transfer and induction of lung inflammation.
Naive CD4 T cells were purified from spleen and peripheral LNs of WT or HVEM−/− OT-II mice using a naive CD4 T cell isolation kit II (Miltenyi Biotec) and AutoMACS Pro cell separator (Miltenyi Biotec). In some cases, naive CD4 T cells (CD62LhiCD44loCD25−) were purified using a FACSAria II cell sorter (BD). To generate Th2 cells, naive CD4 T cells were stimulated either with 1 µg/ml plate-bound anti-CD3 and 5 µg/ml soluble anti-CD28 or with 1 µM OVA peptide (Abgent)–pulsed T cell–depleted splenic APCs in the presence of 20 ng/ml IL-4, 10 µg/ml anti–IFN-γ, and 10 µg/ml anti–IL-12 for 3 d. To generate Th1 cells, naive CD4 T cells were stimulated with 1 µM OVA peptide–pulsed T cell–depleted splenic APCs in the presence of 2 ng/ml IL-12 and 10 µg/ml anti–IL-4 for 3 d. Highly activated Th2/Th1 cells were washed and rested in fresh complete media for another 3–6 d without further stimulation. Rested Th cells (2–3 × 106; >99% CD4+Vα2+Vβ5+) were injected i.v. into congenic naive mice. 1 d after transfer of cells, mice were challenged i.n. with 20–50 µg/ml soluble OVA protein (chicken egg OVA grade V; Sigma-Aldrich) for a consecutive 3 d. Some animals were sacrificed for analysis 1 d later to assess secondary recall responses. Some mice were kept for 45–60 d to study secondary memory cells and further challenged i.n. with OVA for a consecutive 3 d to evaluate tertiary recall responses. To block LIGHT–HVEM interactions, mice were injected i.p. with 100–150 µg LT-βR–Fc or human IgG (Bethyl Laboratories, Inc.) as an isotype control antibody on the indicated days, 24 h before OVA challenge.
In other experiments, congenic CD45.1 naive mice received i.v. 2.5 × 104 purified WT, HVEM−/−, or LIGHT−/− naive CD45.2+ OT-II CD4+ T cells by adoptive transfer. In some cases, 2.5 × 104 CD45.1+ WT OT-II CD4 T cells were cotransferred with 2.5 × 104 CD45.2+ T cells. In both cases, recipient mice were immunized i.v. with 100 µg OVA 323–339 peptide plus 50 µg LPS (Enzo Life Sciences) 1 d after T cell transfer. At different time points, the percentage and absolute number of donor CD45.2+ T cells and surface expression of HVEM and LIGHT on donor cells were determined.
Analysis of lung inflammation.
Mice were killed 1 d after the last OVA challenge, and bronchoalveolar lavage (BAL) fluid, lungs, and lung-draining LNs were obtained. BAL was performed by intratracheal insertion of catheter, lavaging with 0.8–0.9 ml of 2% filtered BSA (Sigma-Aldrich). BAL differential cell counts, FACS analysis, and ELISA for cytokines were performed as described previously (Salek-Ardakani et al., 2003). The right hilum was tied off, and right lungs were isolated and digested for cellular analysis as described previously (Doherty et al., 2009). The left lung was instilled with 0.4 ml of 4% paraformaldehyde for histology. Fixed lung sections were stained with hematoxylin and eosin (H&E). Slides were blinded, and peribronchial regions, six to eight per mouse, were evaluated at ×200, and inflammatory infiltrates around airways were graded for severity. All data unless otherwise stated were collected 24 h after the final antigen challenge.
Antibodies and flow cytometry.
The following antibodies were purchased from BD: anti–CD4-allophycocyanin, anti–CD4-PerCp, anti–CD8-allophycocyanin, anti–CD25-biotin, anti–CD27 biotin, anti–CD44-PE, anti–CD62L-FITC, anti–CD62L-allophycocyanin, anti–CD127-biotin, anti–CXCR5-biotin, anti–Vα2-PE, anti–Vβ5-FITC, anti–CD45.2-FITC or -allophycocyanin, anti–CD45.1-FITC or -allophycocyanin, anti–Bcl-2–PE, and isotype match control antibody. Streptavidin-allophycocyanin (BD) was used to visualize biotin-labeled antibodies. Human IgG was purchased from Bethyl Laboratories, Inc. LT-βR fused with the Fc portion of human IgG (LT-βR–Fc) was made in-house (De Trez et al., 2008). Anti–HVEM-PE, anti–human IgG (heavy chain), anti–IL-2, anti–IL-4, anti–IL-5, anti–IL-13 (all PE or allophycocyanin conjugated), and annexin V detection kit were obtained from eBioscience. Anti–phospho-Ser (473) Akt, anti-Akt, anti–β actin, isotype match control antibody, LY294002 (PI3 kinase inhibitor), and peroxidase-conjugated anti–rabbit-Ig were obtained from Cell Signaling Technology. Reagents for cell fixation and permeabilization for detecting intracellular cytokines, Bcl-2, and phospho-Akt were obtained from BD, and staining was performed according to the manufacturer’s instructions. For LIGHT staining, LT-β expression was first blocked on donor CD4 T cells with anti–LT-β (BBF6; a gift from J. Browning [Biogen Idec, Cambridge, MA] to the Ware laboratory), followed by incubation with LT-βR–Fc and PE-conjugated anti–human Ig (Summers-DeLuca et al., 2007). Cells were examined by flow cytometry by using the FACSCalibur (BD) and analyzed with FlowJo software (Tree Star).
In vitro T cell stimulation and immunoblotting.
Naive CD4 T cells were isolated from spleen and peripheral LNs of WT or HVEM−/− OT-II mice as described previously (Song et al., 2004) and stimulated with plate-bound anti-CD3 or OVA-pulsed APCs under Th2 or neutral conditions. After resting in fresh media, effector T cells were restimulated with OVA-pulsed APCs followed by isolation of CD4+ T cells using CD4 MicroBeads (Miltenyi Biotec). Purified CD4+ T cells were lysed and then subjected to immunoblotting as described previously (Song et al., 2004). To block LIGHT–HVEM interactions, 10 µg/ml LT-βR–Fc was added during CD4 T cell stimulation in the absence of APC as indicated. In some cases, proliferation was measured in triplicate by the incorporation of [3H]thymidine (1 µCi/well; ICN Pharmaceuticals) during the last 8 h of each culture. In vitro T cell survival was determined by Trypan blue exclusion, and the percent recovery was calculated based on the input number of cells.
Retroviral transduction.
Internal ribosome entry site GFP (Mig) retroviral vectors with constitutively active (myristoylated) Akt (Mig-myr-Akt) were described previously (Song et al., 2004). Transduction of CD4 T cells was performed as described previously with some minor changes (Song et al., 2004). In brief, the virus was produced by chloroquine-mediated calcium phosphate transfection of the Plat E packaging cell. Supernatants were collected after 3 d, titered by GFP expression, and used directly for transducing T cells. Naive CD4+ T cells were stimulated with plate-bound anti-CD3 and soluble anti-CD28 under Th2 conditions as described in Adoptive transfer and induction of lung inflammation. After 2 d, the supernatant was replaced with 500 µl of viral supernatant containing 5 g/ml polybrene. The cells were spun for 2 h at 32°C and then incubated at 32°C for 8 h. This procedure was repeated the following day. Viral supernatant was removed and replaced with fresh medium containing 2 ng/ml IL-4, and T cells were recultured. Expression of GFP was determined by flow cytometry on CD4 T cells.
Online supplemental material.
Fig. S1 shows that LT-βR–Fc treatment does not affect accumulation or cytokine secretion of Th2 cells immediately after recall antigen. Fig. S2 shows the cytokine profile of Th2 cells before transfer into the mice. Fig. S3 shows that HVEM signals support optimal generation of endogenous polyclonal memory Th2 populations. Fig. S4 shows that HVEM is not required for the differentiation and effector function of Th2 cells. Fig. S5 shows the cytokine profile and phenotype of memory Th2 cells. Fig. S6 shows the reduction of Bcl-2 expression and increased apoptosis of Th2 cells in the absence of HVEM signals. Fig. S7 shows the efficiency of retroviral transduction of Th2 cells with active Akt. Fig. S8 shows that LIGHT and HVEM do not affect primary expansion of CD4 T cells. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20101562/DC1.
Acknowledgments
We thank M. Macauley and N. Huang for the production of LT-βR–Ig.
This work was supported by National Institutes of Health grants AI070535 and AI49453 to M. Croft and AI067890 and AI033068 to C. Ware. This is manuscript #1305 of the La Jolla Institute for Allergy and Immunology.
The authors have no conflicting financial interests.
Footnotes
Abbreviations used:
- BAL
- bronchoalveolar lavage
- BTLA
- B and T lymphocyte attenuator
- HVEM
- herpesvirus entry mediator
- ICOS
- inducible co-stimulator
- ICS
- intracellular staining
- i.n.
- intranasal(ly)
- LT-βR
- lymphotoxin β receptor
- MLN
- mediastinal LN
- TNFR
- TNF receptor
- TNFRSF
- TNFR superfamily
References
- Barnden M.J., Allison J., Heath W.R., Carbone F.R. 1998. Defective TCR expression in transgenic mice constructed using cDNA-based alpha- and beta-chain genes under the control of heterologous regulatory elements. Immunol. Cell Biol. 76:34–40 10.1046/j.1440-1711.1998.00709.x [DOI] [PubMed] [Google Scholar]
- Bertram E.M., Dawicki W., Sedgmen B., Bramson J.L., Lynch D.H., Watts T.H. 2004. A switch in costimulation from CD28 to 4-1BB during primary versus secondary CD8 T cell response to influenza in vivo. J. Immunol. 172:981–988 [DOI] [PubMed] [Google Scholar]
- Bradley L.M., Harbertson J., Freschi G.C., Kondrack R., Linton P.J. 2000. Regulation of development and function of memory CD4 subsets. Immunol. Res. 21:149–158 10.1385/IR:21:2-3:149 [DOI] [PubMed] [Google Scholar]
- Browning J.L. 2008. Inhibition of the lymphotoxin pathway as a therapy for autoimmune disease. Immunol. Rev. 223:202–220 10.1111/j.1600-065X.2008.00633.x [DOI] [PubMed] [Google Scholar]
- Cai G., Freeman G.J. 2009. The CD160, BTLA, LIGHT/HVEM pathway: a bidirectional switch regulating T-cell activation. Immunol. Rev. 229:244–258 10.1111/j.1600-065X.2009.00783.x [DOI] [PubMed] [Google Scholar]
- Cheung T.C., Oborne L.M., Steinberg M.W., Macauley M.G., Fukuyama S., Sanjo H., D’Souza C., Norris P.S., Pfeffer K., Murphy K.M., et al. 2009a. T cell intrinsic heterodimeric complexes between HVEM and BTLA determine receptivity to the surrounding microenvironment. J. Immunol. 183:7286–7296 10.4049/jimmunol.0902490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung T.C., Steinberg M.W., Oborne L.M., Macauley M.G., Fukuyama S., Sanjo H., D’Souza C., Norris P.S., Pfeffer K., Murphy K.M., et al. 2009b. Unconventional ligand activation of herpesvirus entry mediator signals cell survival. Proc. Natl. Acad. Sci. USA. 106:6244–6249 10.1073/pnas.0902115106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croft M. 2003. Co-stimulatory members of the TNFR family: keys to effective T-cell immunity? Nat. Rev. Immunol. 3:609–620 10.1038/nri1148 [DOI] [PubMed] [Google Scholar]
- Croft M. 2009. The role of TNF superfamily members in T-cell function and diseases. Nat. Rev. Immunol. 9:271–285 10.1038/nri2526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croft M., Bradley L.M., Swain S.L. 1994. Naive versus memory CD4 T cell response to antigen. Memory cells are less dependent on accessory cell costimulation and can respond to many antigen-presenting cell types including resting B cells. J. Immunol. 152:2675–2685 [PubMed] [Google Scholar]
- De Trez C., Schneider K., Potter K., Droin N., Fulton J., Norris P.S., Ha S.W., Fu Y.X., Murphy T., Murphy K.M., et al. 2008. The inhibitory HVEM-BTLA pathway counter regulates lymphotoxin receptor signaling to achieve homeostasis of dendritic cells. J. Immunol. 180:238–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty T.A., Soroosh P., Broide D.H., Croft M. 2009. CD4+ cells are required for chronic eosinophilic lung inflammation but not airway remodeling. Am. J. Physiol. Lung Cell. Mol. Physiol. 296:L229–L235 10.1152/ajplung.90543.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duhen T., Pasero C., Mallet F., Barbarat B., Olive D., Costello R.T. 2004. LIGHT costimulates CD40 triggering and induces immunoglobulin secretion; a novel key partner in T cell-dependent B cell terminal differentiation. Eur. J. Immunol. 34:3534–3541 10.1002/eji.200425598 [DOI] [PubMed] [Google Scholar]
- Force W.R., Walter B.N., Hession C., Tizard R., Kozak C.A., Browning J.L., Ware C.F. 1995. Mouse lymphotoxin-beta receptor. Molecular genetics, ligand binding, and expression. J. Immunol. 155:5280–5288 [PubMed] [Google Scholar]
- Fütterer A., Mink K., Luz A., Kosco-Vilbois M.H., Pfeffer K. 1998. The lymphotoxin beta receptor controls organogenesis and affinity maturation in peripheral lymphoid tissues. Immunity. 9:59–70 10.1016/S1074-7613(00)80588-9 [DOI] [PubMed] [Google Scholar]
- Gommerman J.L., Browning J.L. 2003. Lymphotoxin/light, lymphoid microenvironments and autoimmune disease. Nat. Rev. Immunol. 3:642–655 10.1038/nri1151 [DOI] [PubMed] [Google Scholar]
- Gommerman J.L., Giza K., Perper S., Sizing I., Ngam-Ek A., Nickerson-Nutter C., Browning J.L. 2003. A role for surface lymphotoxin in experimental autoimmune encephalomyelitis independent of LIGHT. J. Clin. Invest. 112:755–767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalo J.A., Tian J., Delaney T., Corcoran J., Rottman J.B., Lora J., Al-garawi A., Kroczek R., Gutierrez-Ramos J.C., Coyle A.J. 2001. ICOS is critical for T helper cell-mediated lung mucosal inflammatory responses. Nat. Immunol. 2:597–604 10.1038/89739 [DOI] [PubMed] [Google Scholar]
- Harrop J.A., McDonnell P.C., Brigham-Burke M., Lyn S.D., Minton J., Tan K.B., Dede K., Spampanato J., Silverman C., Hensley P., et al. 1998. Herpesvirus entry mediator ligand (HVEM-L), a novel ligand for HVEM/TR2, stimulates proliferation of T cells and inhibits HT29 cell growth. J. Biol. Chem. 273:27548–27556 10.1074/jbc.273.42.27548 [DOI] [PubMed] [Google Scholar]
- Hendriks J., Xiao Y., Rossen J.W., van der Sluijs K.F., Sugamura K., Ishii N., Borst J. 2005. During viral infection of the respiratory tract, CD27, 4-1BB, and OX40 collectively determine formation of CD8+ memory T cells and their capacity for secondary expansion. J. Immunol. 175:1665–1676 [DOI] [PubMed] [Google Scholar]
- Heo S.K., Yoon M.A., Lee S.C., Ju S.A., Choi J.H., Suh P.G., Kwon B.S., Kim B.S. 2007. HVEM signaling in monocytes is mediated by intracellular calcium mobilization. J. Immunol. 179:6305–6310 [DOI] [PubMed] [Google Scholar]
- Kuchroo V.K., Anderson A.C., Waldner H., Munder M., Bettelli E., Nicholson L.B. 2002. T cell response in experimental autoimmune encephalomyelitis (EAE): role of self and cross-reactive antigens in shaping, tuning, and regulating the autopathogenic T cell repertoire. Annu. Rev. Immunol. 20:101–123 10.1146/annurev.immunol.20.081701.141316 [DOI] [PubMed] [Google Scholar]
- Lenz D.C., Kurz S.K., Lemmens E., Schoenberger S.P., Sprent J., Oldstone M.B., Homann D. 2004. IL-7 regulates basal homeostatic proliferation of antiviral CD4+T cell memory. Proc. Natl. Acad. Sci. USA. 101:9357–9362 10.1073/pnas.0400640101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- London C.A., Lodge M.P., Abbas A.K. 2000. Functional responses and costimulator dependence of memory CD4+ T cells. J. Immunol. 164:265–272 [DOI] [PubMed] [Google Scholar]
- Mackay F., Browning J.L., Lawton P., Shah S.A., Comiskey M., Bhan A.K., Mizoguchi E., Terhorst C., Simpson S.J. 1998. Both the lymphotoxin and tumor necrosis factor pathways are involved in experimental murine models of colitis. Gastroenterology. 115:1464–1475 10.1016/S0016-5085(98)70025-3 [DOI] [PubMed] [Google Scholar]
- Mahajan S., Cervera A., MacLeod M., Fillatreau S., Perona-Wright G., Meek S., Smith A., MacDonald A., Gray D. 2007. The role of ICOS in the development of CD4 T cell help and the reactivation of memory T cells. Eur. J. Immunol. 37:1796–1808 10.1002/eji.200636661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsters S.A., Ayres T.M., Skubatch M., Gray C.L., Rothe M., Ashkenazi A. 1997. Herpesvirus entry mediator, a member of the tumor necrosis factor receptor (TNFR) family, interacts with members of the TNFR-associated factor family and activates the transcription factors NF-kappaB and AP-1. J. Biol. Chem. 272:14029–14032 10.1074/jbc.272.22.14029 [DOI] [PubMed] [Google Scholar]
- Mauri D.N., Ebner R., Montgomery R.I., Kochel K.D., Cheung T.C., Yu G.L., Ruben S., Murphy M., Eisenberg R.J., Cohen G.H., et al. 1998. LIGHT, a new member of the TNF superfamily, and lymphotoxin alpha are ligands for herpesvirus entry mediator. Immunity. 8:21–30 10.1016/S1074-7613(00)80455-0 [DOI] [PubMed] [Google Scholar]
- McKinstry K.K., Strutt T.M., Swain S.L. 2008. The effector to memory transition of CD4 T cells. Immunol. Res. 40:114–127 10.1007/s12026-007-8004-y [DOI] [PubMed] [Google Scholar]
- Murphy M., Walter B.N., Pike-Nobile L., Fanger N.A., Guyre P.M., Browning J.L., Ware C.F., Epstein L.B. 1998. Expression of the lymphotoxin beta receptor on follicular stromal cells in human lymphoid tissues. Cell Death Differ. 5:497–505 10.1038/sj.cdd.4400374 [DOI] [PubMed] [Google Scholar]
- Purton J.F., Tan J.T., Rubinstein M.P., Kim D.M., Sprent J., Surh C.D. 2007. Antiviral CD4+ memory T cells are IL-15 dependent. J. Exp. Med. 204:951–961 10.1084/jem.20061805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers P.R., Dubey C., Swain S.L. 2000. Qualitative changes accompany memory T cell generation: faster, more effective responses at lower doses of antigen. J. Immunol. 164:2338–2346 [DOI] [PubMed] [Google Scholar]
- Salek-Ardakani S., Song J., Halteman B.S., Jember A.G., Akiba H., Yagita H., Croft M. 2003. OX40 (CD134) controls memory T helper 2 cells that drive lung inflammation. J. Exp. Med. 198:315–324 10.1084/jem.20021937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheu S., Alferink J., Pötzel T., Barchet W., Kalinke U., Pfeffer K. 2002. Targeted disruption of LIGHT causes defects in costimulatory T cell activation and reveals cooperation with lymphotoxin β in mesenteric lymph node genesis. J. Exp. Med. 195:1613–1624 10.1084/jem.20020215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seder R.A., Ahmed R. 2003. Similarities and differences in CD4+ and CD8+ effector and memory T cell generation. Nat. Immunol. 4:835–842 10.1038/ni969 [DOI] [PubMed] [Google Scholar]
- Sedy J.R., Gavrieli M., Potter K.G., Hurchla M.A., Lindsley R.C., Hildner K., Scheu S., Pfeffer K., Ware C.F., Murphy T.L., Murphy K.M. 2005. B and T lymphocyte attenuator regulates T cell activation through interaction with herpesvirus entry mediator. Nat. Immunol. 6:90–98 10.1038/ni1144 [DOI] [PubMed] [Google Scholar]
- Shaikh R.B., Santee S., Granger S.W., Butrovich K., Cheung T., Kronenberg M., Cheroutre H., Ware C.F. 2001. Constitutive expression of LIGHT on T cells leads to lymphocyte activation, inflammation, and tissue destruction. J. Immunol. 167:6330–6337 [DOI] [PubMed] [Google Scholar]
- Shi G., Luo H., Wan X., Salcedo T.W., Zhang J., Wu J. 2002. Mouse T cells receive costimulatory signals from LIGHT, a TNF family member. Blood. 100:3279–3286 10.1182/blood-2002-05-1404 [DOI] [PubMed] [Google Scholar]
- Song J., Salek-Ardakani S., Rogers P.R., Cheng M., Van Parijs L., Croft M. 2004. The costimulation-regulated duration of PKB activation controls T cell longevity. Nat. Immunol. 5:150–158 10.1038/ni1030 [DOI] [PubMed] [Google Scholar]
- Stahl M., Dijkers P.F., Kops G.J., Lens S.M., Coffer P.J., Burgering B.M., Medema R.H. 2002. The forkhead transcription factor FoxO regulates transcription of p27Kip1 and Bim in response to IL-2. J. Immunol. 168:5024–5031 [DOI] [PubMed] [Google Scholar]
- Summers-DeLuca L.E., McCarthy D.D., Cosovic B., Ward L.A., Lo C.C., Scheu S., Pfeffer K., Gommerman J.L. 2007. Expression of lymphotoxin-alphabeta on antigen-specific T cells is required for DC function. J. Exp. Med. 204:1071–1081 10.1084/jem.20061968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamada K., Shimozaki K., Chapoval A.I., Zhai Y., Su J., Chen S.F., Hsieh S.L., Nagata S., Ni J., Chen L. 2000. LIGHT, a TNF-like molecule, costimulates T cell proliferation and is required for dendritic cell-mediated allogeneic T cell response. J. Immunol. 164:4105–4110 [DOI] [PubMed] [Google Scholar]
- Tamada K., Tamura H., Flies D., Fu Y.X., Celis E., Pease L.R., Blazar B.R., Chen L. 2002. Blockade of LIGHT/LTbeta and CD40 signaling induces allospecific T cell anergy, preventing graft-versus-host disease. J. Clin. Invest. 109:549–557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viola A., Lanzavecchia A. 1996. T cell activation determined by T cell receptor number and tunable thresholds. Science. 273:104–106 10.1126/science.273.5271.104 [DOI] [PubMed] [Google Scholar]
- Wan X., Zhang J., Luo H., Shi G., Kapnik E., Kim S., Kanakaraj P., Wu J. 2002. A TNF family member LIGHT transduces costimulatory signals into human T cells. J. Immunol. 169:6813–6821 [DOI] [PubMed] [Google Scholar]
- Wang J., Lo J.C., Foster A., Yu P., Chen H.M., Wang Y., Tamada K., Chen L., Fu Y.X. 2001. The regulation of T cell homeostasis and autoimmunity by T cell-derived LIGHT. J. Clin. Invest. 108:1771–1780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Subudhi S.K., Anders R.A., Lo J., Sun Y., Blink S., Wang Y., Wang J., Liu X., Mink K., et al. 2005. The role of herpesvirus entry mediator as a negative regulator of T cell-mediated responses. J. Clin. Invest. 115:711–717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware C.F. 2009. Targeting the LIGHT-HVEM pathway. Adv. Exp. Med. Biol. 647:146–155 10.1007/978-0-387-89520-8_10 [DOI] [PubMed] [Google Scholar]
- Watanabe N., Gavrieli M., Sedy J.R., Yang J., Fallarino F., Loftin S.K., Hurchla M.A., Zimmerman N., Sim J., Zang X., et al. 2003. BTLA is a lymphocyte inhibitory receptor with similarities to CTLA-4 and PD-1. Nat. Immunol. 4:670–679 10.1038/ni944 [DOI] [PubMed] [Google Scholar]
- Watts T.H. 2005. TNF/TNFR family members in costimulation of T cell responses. Annu. Rev. Immunol. 23:23–68 10.1146/annurev.immunol.23.021704.115839 [DOI] [PubMed] [Google Scholar]
- Wei C.Y., Chou Y.H., Ho F.M., Hsieh S.L., Lin W.W. 2006. Signaling pathways of LIGHT induced macrophage migration and vascular smooth muscle cell proliferation. J. Cell. Physiol. 209:735–743 10.1002/jcp.20742 [DOI] [PubMed] [Google Scholar]
- Wu Q., Salomon B., Chen M., Wang Y., Hoffman L.M., Bluestone J.A., Fu Y.X. 2001. Reversal of spontaneous autoimmune insulitis in nonobese diabetic mice by soluble lymphotoxin receptor. J. Exp. Med. 193:1327–1332 10.1084/jem.193.11.1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Flies A.S., Flies D.B., Zhu G., Anand S., Flies S.J., Xu H., Anders R.A., Hancock W.W., Chen L., Tamada K. 2007. Selective targeting of the LIGHT-HVEM costimulatory system for the treatment of graft-versus-host disease. Blood. 109:4097–4104 10.1182/blood-2006-09-047332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu K.Y., Kwon B., Ni J., Zhai Y., Ebner R., Kwon B.S. 1999. A newly identified member of tumor necrosis factor receptor superfamily (TR6) suppresses LIGHT-mediated apoptosis. J. Biol. Chem. 274:13733–13736 10.1074/jbc.274.20.13733 [DOI] [PubMed] [Google Scholar]
- Zhai Y., Guo R., Hsu T.L., Yu G.L., Ni J., Kwon B.S., Jiang G.W., Lu J., Tan J., Ugustus M., et al. 1998. LIGHT, a novel ligand for lymphotoxin beta receptor and TR2/HVEM induces apoptosis and suppresses in vivo tumor formation via gene transfer. J. Clin. Invest. 102:1142–1151 10.1172/JCI3492 [DOI] [PMC free article] [PubMed] [Google Scholar]