Abstract
Objective
To provide family physicians with a practical, evidence-based approach to fall prevention in the elderly.
Sources of information
MEDLINE was searched using terms relevant to falls among the elderly in the community and in institutions. Relevant English-language papers published from 1980 to July 2010 were reviewed. Relevant geriatric society guidelines were reviewed as well.
Main message
Falls are a common and serious health problem with devastating consequences. Several risk factors have been identified in the literature. Falls can be prevented through several evidence-based interventions, which can be either single or multicomponent interventions. Identifying at-risk patients is the most important part of management, as applying preventive measures in this vulnerable population can have a profound effect on public health.
Conclusion
Family physicians have a pivotal role in screening older patients for risk of falls, and applying preventive strategies for patients at risk.
Résumé
Objectif
Proposer au médecin de famille une démarche pratique, fondée sur des données probantes, pour prévenir les chutes chez les personnes âgées.
Sources de l’information
On a consulté MEDLINE à l’aide des termes en rapport avec les chutes chez les vieillards qui vivent dans la communauté ou en institution. Les articles pertinents en anglais publiés entre 1980 et juillet 2010 ont été révisés, de même que les directives des sociétés de gériatrie.
Principal message
Les chutes sont un problème de santé fréquent et sérieux dont les conséquences sont dévastatrices. Plusieurs facteurs de risque ont déjà été identifiés dans la littérature. Les chutes peuvent être prévenues grâce à diverses interventions reposant sur des preuves qui peuvent être simples ou plus complexes. La partie la plus importante du traitement consiste à identifier les patients à risque, puisque l’application de mesures préventives à cette population vulnérable peut avoir des effets considérables sur le plan de la santé publique.
Conclusion
Le médecin de famille a un rôle primordial à jouer pour dépister les patients âgés à risque de chutes et pour appliquer des mesures préventives.
Case
Ms M., an 82-year-old independent woman, presents to her family doctor for a regular checkup. She is asymptomatic and states that she is doing well. However, when asked about falls, she describes falling 3 times in the past 6 months. Her falls were at home shortly after getting out of bed and were not associated with a loss of consciousness or an injury. Her history includes an old lacunar stroke, hypertension, knee osteoarthritis, and depression. Ms M. takes 25 mg of hydrochlorothiazide, 100 mg of atenolol, and 200 mg of ibuprofen all once daily, and 2 mg of lorazepam twice daily.
Falls are a main cause of morbidity and disability in the elderly. More than one-third of persons 65 years of age or older fall each year, and in half of such cases the falls are recurrent.1 The risk doubles or triples in the presence of cognitive impairment or history of previous falls.2 In Canada, falls are the most common cause (85%) of injury-related hospital admissions among those aged 65 years or older.3
Many view falls as merely a risk factor for fractures, disregarding the fact that falls can lead to irreversible health, social, and psychological consequences, with profound economic effects.4
Sources of information
MEDLINE was searched using terms relevant to falls among the elderly in the community and in institutions. Relevant English-language papers published from 1980 to July 2010 were reviewed. Relevant geriatric society guidelines were reviewed as well.
Pathophysiology
A fall is a complex multifactorial phenomenon. In order to understand the mechanism of falls, it is essential to understand the prerequisites of normal gait. Essential substrates for a normal gait include fine neural networks such as the cortical–basal ganglia loop and the basal ganglia–brainstem system, exquisite musculoskeletal structures with appropriately regulated muscle tone, and proper processing of sensory information (ie, cerebral cortex, vision, hearing, fine touch, and proprioception).5 Effective coordination of those components, along with adequate cognition and concentration, is needed to prevent falls and maintain gait.
It is not surprising that many of those functions show at least some decline with aging, thus increasing the risk of falls. Moreover, as a person ages, the likelihood of accumulating medical problems and their associated medications increases, and so does the risk of falling. Many changes occur in gait with aging, such as a decrease in gait velocity and step length, a wider base, and a decrease in lower limb strength. These changes are most pronounced when older people walk on irregular surfaces.6
A fall usually results from interactions between long-term or short-term predisposing factors and short-term precipitating factors (such as a trip, an acute illness, or an adverse drug reaction) in a person’s environment.7
Risk factors
Independent risk factors for falling include the following (arranged in order of evidence strength): previous falls, balance impairment, decreased muscle strength, visual impairment, polypharmacy (more than 4 medications) or psychoactive drugs, gait impairment and walking difficulty, depression, dizziness or orthostasis, functional limitations, age older than 80 years, female sex, incontinence, cognitive impairment, arthritis, diabetes, and pain.1 The risk of falling increases with the number of risk factors: 1-year risk of falling doubles with each additional factor, starting from 8% with none, and reaching 78% with 4 risk factors.1 A recent meta-analysis identified the following risk factors as having the strongest association with falling: history of falls, gait problems, walking aid use, vertigo, Parkinson disease, and antiepileptic drug use.8
A recent study has shown that the risk of falling increases in proportion to the severity of chronic musculoskeletal pain, the number of joint groups affected, and the amount of interference with daily activities.9
In a prospective study, white-matter lesions seen on magnetic resonance imaging were found to be strong predictors of risk factors for falls.10
Postural hypotension is common among the elderly, and can predispose to gait problems and falls.11 Measuring postural blood pressure is easy, noninvasive, inexpensive, and quick; however, it is performed in less than 40% of older adults admitted with syncope, and is much more likely to affect diagnosis and management than more expensive and cumbersome tests are.12 Postural hypotension is defined as a decrease in systolic pressure of at least 20 mm Hg or in diastolic pressure of at least 10 mm Hg within 3 minutes of standing. Patients should remain supine for at least 2 minutes before measuring supine vital signs, and remain standing for at least 1 minute before measuring standing vital signs.13
Obstructive sleep apnea was reported recently to be a reversible culprit in 4 elderly patients with daytime sleepiness and falling-asleep-related injurious falls.14
The risk of falling quadruples for the first 2 weeks after discharge from hospital,15 highlighting the vulnerability of this patient population and the adverse effects hospitalization might have on older adults. Moreover, in patients who have sustained falls while in hospital, 29% will fall at home, 35% will be readmitted for falls, and 5% will die within a month.16 This might be related to a variety of precipitating factors, such as acute illness, environment change, or adverse drug reactions.
Medications
Medications are a well established risk factor for falls. However, it is important to consider the reason for taking a medication before deciding to stop or withdraw a medication for the purpose of fall prevention, because the condition the drug is used to treat might itself be a risk factor for falling. Depression, pain, and cognitive impairment are examples. Therefore, each medication should be examined individually, and the benefits and risks of stopping or continuing its use should be weighed carefully.
Medication classes that have been associated with an increased risk of falls include the following: antihypertensive agents, sedatives and hypnotics, neuroleptics and antipsychotics, antidepressants, benzodiazepines, and nonsteroidal anti-inflammatory drugs. Narcotics, however, have not been associated with increased risk of falls.17
In a population-based cohort study, which used health care databases from Ontario, the use of cholinesterase inhibitors was associated with increased rates of syncope, bradycardia, pacemaker insertion, and hip fracture in older adults with dementia.18 These findings highlight this class of medications as a potential risk factor for falls; these risks should be weighed carefully and discussed with patients and caregivers.
Screening and assessment
Very quick screening can be carried out in any medical practice by inquiring about falls in the past year and gait or balance problems. Individuals who are 65 years of age or older have an annual pretest probability of falling of 27%. Patients who have fallen in the past year are more likely to fall again (likelihood ratio 2.3 to 2.8), as are those who have clinically detected abnormalities of gait or balance (likelihood ratio 1.7 to 2.4). The presence of any of these factors brings the annual risk to 50%, and therefore should prompt a full assessment.13
A full assessment should include the following.
History
Careful attention should be paid to the circumstances of the falls and evaluation of risk factors. A careful medication review is of great importance, as are functional and environmental assessments.
Physical examination
Physical examination should include gait assessment, sensory assessment (including hearing and vision), measurement of orthostatic vital signs, and neurologic and musculoskeletal assessment, as well as depression and cognitive impairment screening.19 The examination should also include a review of footwear and gait aid appropriateness.
Further assessment or investigations are guided by the findings from the history and physical examination.
Guidelines
In 2010, the American Geriatrics Society (AGS) and the British Geriatrics Society (BGS) issued fall prevention guidelines, which have been endorsed by the American Medical Association, the American Occupational Therapy Association, and the American Physical Therapy Association.20 Recommendations in this review are in keeping with those guidelines.19 The guidelines urge primary care physicians to screen their patients yearly and to implement tailored, multifaceted interventions for at-risk patients.20 The guidelines, however, are somewhat conservative in what would prompt a full falls assessment, requiring the patient to have either a history of at least 2 falls in the past year or to present with a fall. It is not unreasonable to have a lower threshold (ie, a single fall in the past year) for initiating a full assessment.19
Prevention
Various interventions have been shown to decrease the risk and the rate of falls. They are generally divided into single and multicomponent interventions.
Vitamin D
Vitamin D supplementation, particularly if given in doses of 800 IU/d or more, has been shown to reduce falls: number needed to treat of 14 to prevent 1 fall.21,22 Moreover, vitamin D supplementation is the only intervention that has been shown to decrease the rate of falls in long-term care.23
Interestingly, when vitamin D was supplemented in a single annual dose of 500 000 IU, falls and fractures increased,24 perhaps through a reduced tissue level or through increased activity and mobility.25
Exercise
Several exercise modalities have been studied. In a Cochrane review, multicomponent group exercises reduced the rate and risk of falling (rate ratio [RR] 0.78), as did Tai Chi (RR 0.63) and individually prescribed multicomponent home-based exercises (RR 0.66).26
A 2008 meta-analysis showed the greatest effects on fall rates were from programs that included a combination of a higher total dose of exercise (> 50 hours during the trial period) and challenging balance exercises (eg, standing with feet together or on one leg, minimizing the use of hands to assist, and practising controlled movements of the centre of mass), and did not include a walking program.27
The 2010 AGS and BGS guidelines recommend the development of an individualized exercise regimen (strength, gait, and balance exercises; eg, Tai Chi or physiotherapy) for all patients at risk (grade A recommendation).19
Tai Chi is a low-impact exercise. It is available through many senior centres throughout Canada for as little as $4 a session,28 and has documented benefits for fall prevention,26 as well as other possible health benefits.29
Medications
Gradual withdrawal of psychotropic medication reduces the rate of falls, and a prescribing modification program implemented by primary care physicians substantially reduces the risk of falling among elderly patients.26 However, great caution and patience should be exercised when weaning patients off medications, particularly when they have been used chronically. A statewide policy to reduce benzodiazepine prescribing resulted in an immediate reduction in benzodiazepine use but not in a reduction of hip fractures, perhaps owing to the use of alternative sedatives. This highlights the importance of managing each patient individually.30
Vision
Visual impairment is an important risk factor for falls. However, a comprehensive vision assessment and management program that resulted mainly in new eyeglasses prescriptions found an increased rate of falls, particularly in the first few months, perhaps owing to difficulty adjusting to new glasses or to increased activity.31
On the other hand, expedited cataract surgery reduces falls in older women having the operation on the first affected eye but not the second.26
Those who wear multifocal lenses are more than twice as likely to fall, particularly outside their homes, than those who do not wear multifocal lenses.32 Providing older people who are active outdoors with single-lens distance glasses (instead of multifocals) reduces falls. However, this increases falls in individuals who have limited outdoor activities; they might be better off using their multifocal lenses in their familiar environments.33
Cardiac pacing
One study addressed dual-chamber pacing in patients with cardioinhibitory carotid sinus hypersensitivity (defined as 3 or more seconds of asystole after carotid massage) and unexplained falls. Pacing resulted in a reduction in the total number of falls by more than two-thirds.34
Environment
Home safety interventions (eg, home visits by occupational therapists) have a role in secondary prevention (patients with previous falls). The role of home safety in primary prevention is limited to those with the highest risk.26
Use of antislip shoe devices in those who have experienced previous falls substantially reduced outside falls during wintertime: number needed to treat of 6.35
Preliminary data suggest that delirium prevention in hospitals, through multicomponent strategies, is effective in reducing falls.36
Multicomponent interventions
A large body of evidence for multicomponent interventions shows mixed results.26,37 Overall, interventions were effective if they actively provided treatments; those that provided only knowledge or referrals were not effective.1,38–40
The 2010 AGS and BGS guidelines give a grade A recommendation to multifactorial interventions. The guidelines further grade the evidence behind each component, with the strongest evidence for home modification and exercise, followed by psychoactive medication adjustment, then other medication adjustment, postural hypotension management, and foot problem and foot-wear management.19
Fall prevention clinics were shown in 2 studies (non-randomized controlled) to reduce the risk of falls and injurious falls.41,42 In Canada, multicomponent interventions are usually offered through fall clinics or day hospitals. The Regional Geriatric Programs of Ontario’s website (http://rgps.on.ca) is an excellent resource to find those services in Ontario. Similar resources are available in other provinces.
Boxes 121,22,26 and 21,26,33–35 summarize the interventions with the best evidence to prevent falls.
Box 1. Single interventions with proven benefits for prevention of falls.
Interventions with the best evidence to prevent falls include the following:
Box 2. Interventions that are likely to be beneficial for prevention of falls.
The following interventions are likely to be effective in preventing falls:
Review medications, minimizing psychoactive medications and reducing the total number of medications26
Assess and treat postural hypotension1
Expedite cataract surgery on the first affected eye26
Suggest single-lens distance-vision glasses for outdoor use in multifocal-lens users who participate in regular outdoor activities33
Consider pacing in cardioinhibitory carotid sinus hypersensitivity and recurrent falls34
Recommend use of antislip shoe devices for the outdoors in the winter35
Recommend multifactorial interventions that assess an individual person’s risk of falling, and carry out interventions to reduce that risk26
Conclusion
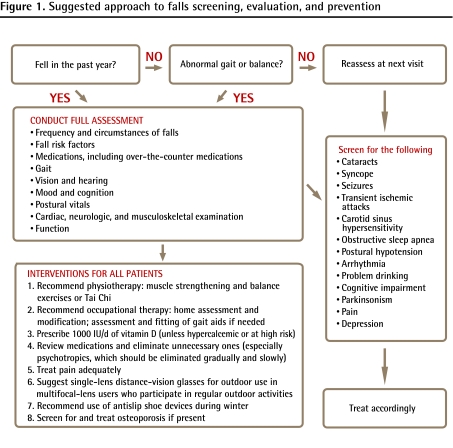
Ms M. has a 50% annual risk of falling again; therefore, a full assessment is warranted (Figure 1). This should include assessment of her depression. Gradual reduction of her antihypertensive medications should be attempted to eliminate the orthostatic blood pressure drop, perhaps starting with the β-blocker, given her low heart rate. Gradual and slow withdrawal of benzodiazepines should be tried as well. She should be evaluated for the presence of pain and treated accordingly. Regular use of acetaminophen is a safer alternative than ibuprofen, and low-dose narcotics could be considered. Ms M. should be referred to occupational therapy for a home assessment and intervention, as well as to physical therapy for structured exercises. Tai Chi is a reasonable alternative. She should also be prescribed 1000 IU of vitamin D daily. Ms M. should be screened for osteoporosis in order to minimize fracture risk from future falls.
Figure 1.
Suggested approach to falls screening, evaluation, and prevention
When Ms M. presented to her family doctor, she did not volunteer her history of falls, which is not uncommon. It therefore behooves medical professionals to be proactive in inquiring about falls, given how common this problem is, its high likelihood of recurrence, and the profound effects of its consequences. Risk factors for falls should be viewed as potentially reversible, and falls should not be perceived as an inevitable part of aging.
Further resources
The following resources provide helpful information on home safety for both health workers and patients:
Canada Safety Council [website]. Home adaptation checklist. Ottawa, ON: Canada Safety Council; 2011. Available from: http://safety-council.org/safety/public-safety/seniors/home-adaptation-checklist/.
Centers for Disease Control and Prevention. Check for safety. Atlanta, GA: Centers for Disease Control and Prevention; 2005. Available from: www.cdc.gov/ncipc/pub-res/toolkit/Falls_ToolKit/DesktopPDF/English/booklet_Eng_desktop.pdf.
Canada Mortgage and Housing Corporation [website]. Accessible housing by design—ramps. Ottawa, ON: Canada Mortgage and Housing Corporation; 2010. Available from: www.cmhc-schl.gc.ca/en/co/renoho/refash/refash_025.cfm.
Acknowledgments
I thank Dr Laura Diachun for reviewing this article and Ms Kelly McIntyre Muddle for helping with online resources.
KEY POINTS
Falls are a main cause of morbidity and disability in the elderly. Oftentimes elderly patients will not volunteer their history of falls. It is therefore important that family physicians proactively inquire about falls, given how common the problem is, its high likelihood of recurrence, and the profound effects of its consequences. Interventions that are likely to prevent falls include home assessment and modification for high-risk individuals, exercise programs that include strength, gait, and balance exercises (eg, Tai Chi), and vitamin D supplementation in doses greater than 700 IU/d (in community-dwelling or long-term care residents). Risk factors for falls should be viewed as potentially reversible, and falls should not be perceived as an inevitable part of aging.
POINTS DE REPÈRE
Les chutes sont une importante cause de morbidité et d’incapacité chez les personnes âgées. Souvent, ces patients sont réticents à raconter leurs chutes. Il est donc primordial que le médecin s’informe de façon proactive de ces chutes, compte tenu de leur fréquence, d’une forte probabilité de récidive et des conséquences sérieuses qu’elles entraînent. Les interventions qui sont susceptibles de prévenir les chutes incluent l’évaluation et la modification du domicile pour ceux qui présentent un risque élevé, les programmes de conditionnement comprenant des exercices de renforcement, de démarche et d’équilibre (p. ex. le tai chi), et l’ajout de suppléments de vitamine D en doses supérieures à 700 UI/d (pour les sujets vivant dans la communauté ou les résidents des centres d’hébergement de longue durée). Les facteurs qui augmentent les risques de chute devraient être considérés comme potentiellement réversibles, et les chutes ne devraient pas être vues comme une conséquence inévitable du vieillissement.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
Competing interests
None declared
References
- 1.Tinetti ME, Kumar C. The patient who falls: “It’s always a trade-off.”. JAMA. 2010;303(3):258–66. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Institute for Health Information . National Trauma Registry 2003 report. Hospital injury admissions (included 2000/2001 data) Ottawa, ON: Canadian Institute for Health Information; 2003. Available from: http://secure.cihi.ca/cihiweb/products/NTR_HospitalInjury_2003.pdf. Accessed 2011 May 13. [Google Scholar]
- 4.Czerwinski E, Białoszewski D, Borowy P, Kumorek A, Białoszewski A. Epidemiology, clinical significance, costs and fall prevention in elderly people. Ortop Traumatol Rehabil. 2008;10(5):419–28. [PubMed] [Google Scholar]
- 5.Takakusaki K, Tomita N, Yano M. Substrates for normal gait and pathophysiology of gait disturbances with respect to the basal ganglia dysfunction. J Neurol. 2008;255(Suppl 4):19–29. doi: 10.1007/s00415-008-4004-7. [DOI] [PubMed] [Google Scholar]
- 6.Scherder E, Eggermont L, Swaab D, van Heuvelen M, Kamsma Y, de Greef M, et al. Gait in ageing and associated dementias; its relationship with cognition. Neurosci Biobehav Rev. 2007;31(4):485–97. doi: 10.1016/j.neubiorev.2006.11.007. Epub 2007 Feb 15. [DOI] [PubMed] [Google Scholar]
- 7.Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42–9. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 8.Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–68. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- 9.Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302(20):2214–21. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srikanth V, Beare R, Blizzard L, Phan T, Stapleton J, Chen J, et al. Cerebral white matter lesions, gait, and the risk of incident falls: a prospective population-based study. Stroke. 2009;40(1):175–80. doi: 10.1161/STROKEAHA.108.524355. Epub 2008 Oct 16. [DOI] [PubMed] [Google Scholar]
- 11.Mosnaim AD, Abiola R, Wolf ME, Perlmuter LC. Etiology and risk factors for developing orthostatic hypotension. Am J Ther. 2010;17(1):86–91. doi: 10.1097/MJT.0b013e3181a2b1bb. [DOI] [PubMed] [Google Scholar]
- 12.Mendu ML, McAvay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169(14):1299–305. doi: 10.1001/archinternmed.2009.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297(1):77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 14.Onen F, Higgins S, Onen SH. Falling-asleep-related injured falls in the elderly. J Am Med Dir Assoc. 2009;10(3):207–10. doi: 10.1016/j.jamda.2008.10.008. Epub 2009 Jan 9. [DOI] [PubMed] [Google Scholar]
- 15.Mahoney J, Sager M, Dunham NC, Johnson J. Risk of falls after hospital discharge. J Am Geriatr Soc. 1994;42(3):269–74. doi: 10.1111/j.1532-5415.1994.tb01750.x. [DOI] [PubMed] [Google Scholar]
- 16.Davenport RD, Vaidean GD, Jones CB, Chandler AM, Kessler LA, Mion LC, et al. Falls following discharge after an in-hospital fall. BMC Geriatr. 2009;9:53. doi: 10.1186/1471-2318-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952–60. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 18.Gill SS, Anderson GM, Fischer HD, Bell CM, Li P, Normand SL, et al. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: a population-based cohort study. Arch Intern Med. 2009;169(9):867–73. doi: 10.1001/archinternmed.2009.43. [DOI] [PubMed] [Google Scholar]
- 19.American Geriatrics Society [website] AGS/BGS clinical practice guideline: prevention of falls in older persons (2010) New York, NY: American Geriatrics Society; 2011. Available from: www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/2010/. Accessed 2011 May 13. [Google Scholar]
- 20.Kuehn BM. Primary care screening and intervention helps prevent falls among elderly. JAMA. 2010;303(20):2019–20. doi: 10.1001/jama.2010.640. [DOI] [PubMed] [Google Scholar]
- 21.Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692. doi: 10.1136/bmj.b3692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalyani RR, Stein B, Valiyil R, Manno R, Maynard JW, Crews DC. Vitamin D treatment for the prevention of falls in older adults: systematic review and meta-analysis. J Am Geriatr Soc. 2010;58(7):1299–310. doi: 10.1111/j.1532-5415.2010.02949.x. Epub 2010 Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev. 2010;(1):CD005465. doi: 10.1002/14651858.CD005465.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, et al. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303(18):1815–22. doi: 10.1001/jama.2010.594. [DOI] [PubMed] [Google Scholar]
- 25.Dawson-Hughes B, Harris SS. High-dose vitamin D supplementation: too much of a good thing? JAMA. 2010;303(18):1861–2. doi: 10.1001/jama.2010.598. [DOI] [PubMed] [Google Scholar]
- 26.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Gates S, Cumming RG, et al. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003;(4):CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 27.Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(12):2234–43. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 28.City of London [website] Ontario recreational programs guide (2010) London, ON: City of London; 2011. Available from: www.london.ca/d.aspx?s=/Sports_and_Recreation/spectrum.htm. Accessed 2010 Jul 23. [Google Scholar]
- 29.Hall A, Maher C, Latimer J, Ferreira M. The effectiveness of Tai Chi for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Arthritis Rheum. 2009;61(6):717–24. doi: 10.1002/art.24515. [DOI] [PubMed] [Google Scholar]
- 30.Wagner AK, Ross-Degnan D, Gurwitz JH, Zhang F, Gilden DB, Cosler L, et al. Effect of New York State regulatory action on benzodiazepine prescribing and hip fracture rates. Ann Intern Med. 2007;146(2):96–103. doi: 10.7326/0003-4819-146-2-200701160-00004. [DOI] [PubMed] [Google Scholar]
- 31.Cumming RG, Ivers R, Clemson L, Cullen J, Hayes MF, Tanzer M, et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc. 2007;55(2):175–81. doi: 10.1111/j.1532-5415.2007.01046.x. [DOI] [PubMed] [Google Scholar]
- 32.Lord SR, Dayhew J, Howland A. Multifocal glasses impair edge-contrast sensitivity and depth perception and increase the risk of falls in older people. J Am Geriatr Soc. 2002;50(11):1760–6. doi: 10.1046/j.1532-5415.2002.50502.x. [DOI] [PubMed] [Google Scholar]
- 33.Haran MJ, Cameron ID, Ivers RQ, Simpson JM, Lee BB, Tanzer M, et al. Effect on falls of providing single lens distance vision glasses to multifocal glasses wearers: VISIBLE randomised controlled trial. BMJ. 2010;340:c2456. doi: 10.1136/bmj.c2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kenny RA, Richardson DA, Steen N, Bexton RS, Shaw FE, Bond J. Carotid sinus syndrome: a modifiable risk factor for nonaccidental falls in older adults (SAFE PACE) J Am Coll Cardiol. 2001;38(5):1491–6. doi: 10.1016/s0735-1097(01)01537-6. [DOI] [PubMed] [Google Scholar]
- 35.McKiernan FE. A simple gait-stabilizing device reduces outdoor falls and nonserious injurious falls in fall-prone older people during the winter. J Am Geriatr Soc. 2005;53(6):943–7. doi: 10.1111/j.1532-5415.2005.53302.x. [DOI] [PubMed] [Google Scholar]
- 36.Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. N Engl J Med. 2009;360(23):2390–3. doi: 10.1056/NEJMp0900963. [DOI] [PubMed] [Google Scholar]
- 37.Gates S, Fisher JD, Cooke MW, Carter YH, Lamb SE. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta-analysis. BMJ. 2008;336(7636):130–3. doi: 10.1136/bmj.39412.525243.BE. Epub 2007 Dec 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tinetti ME. Multifactorial fall-prevention strategies: time to retreat or advance. J Am Geriatr Soc. 2008;56(8):1563–5. doi: 10.1111/j.1532-5415.2008.01800.x. [DOI] [PubMed] [Google Scholar]
- 39.Spivack BS. Preventing falls: direct intervention is needed. BMJ. 2008;336(7640):343. doi: 10.1136/bmj.39486.498866.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mahoney JE. Why multifactorial fall-prevention interventions may not work: comment on “multifactorial intervention to reduce falls in older people at high risk of recurrent falls.”. Arch Intern Med. 2010;170(13):1117–9. doi: 10.1001/archinternmed.2010.193. [DOI] [PubMed] [Google Scholar]
- 41.Sze PC, Cheung WH, Lam PS, Lo HS, Leung KS, Chan T. The efficacy of a multidisciplinary falls prevention clinic with an extended step-down community program. Arch Phys Med Rehabil. 2008;89(7):1329–34. doi: 10.1016/j.apmr.2007.11.044. [DOI] [PubMed] [Google Scholar]
- 42.Moore M, Williams B, Ragsdale S, Logerfo JP, Goss JR, Schreuder AB, et al. Translating a multifactorial fall prevention intervention into practice: a controlled evaluation of a fall prevention clinic. J Am Geriatr Soc. 2010;58(2):357–63. doi: 10.1111/j.1532-5415.2009.02683.x. [DOI] [PMC free article] [PubMed] [Google Scholar]