Abstract
Background
The putative goal of sac surgery in Meniere’s syndrome is to promote the flow of endolymph from the labyrinth to the endolymphatic sac, and thereby relieving hydrops. There is scant published histopathological data whether sac surgery actually accomplishes this goal.
Objective
To determine if sac surgery relieves hydrops by examining the histopathologic changes in temporal bones obtained from individuals who had undergone sac surgery during life for Meniere’s syndrome.
Methods
Temporal bones were examined from 15 patients who had sac surgery. Data was collected on presence and severity of hydrops, histology of the sac, and whether the procedure relieved vertigo.
Results
The surgery failed to expose the sac in 5 cases; 4 of the 5 had relief from vertigo. The sac was exposed, but the shunt failed to reach the lumen of the sac in 8 cases; 4 of the 8 had relief from vertigo. The shunt was successfully placed within the lumen of the sac in two cases; both cases failed to experience relief from vertigo. Endolymphatic hydrops was present in all 15 cases.
Conclusion
Endolymphatic sac surgery does not relieve hydrops in patients with Meniere’s syndrome. Yet, sac surgery relieves vertigo in some patients, but the mechanism of such symptomatic relief remains unknown.
INTRODUCTION
Meniere’s syndrome is characterized by symptoms of episodic vertigo, fluctuating sensorineural hearing loss, tinnitus and aural fullness (1). Many different medical and surgical treatments have been described to ameliorate the vestibular complaints in Meniere’s syndrome. Surgery of the endolymphatic sac was described by Portmann in 1927 (2), 11 years before the description of endolymphatic hydrops as the pathologic correlate of Meniere’s syndrome by Hallpike and Cairns (3) and Yamakawa (4). The sac procedure was revived in the 1960s by William House (5) and has been extensively used over the past five decades to prevent disabling episodic vertigo. Technical details of sac surgery have varied (6), including decompression of the sac alone, placement of a shunt between the endolymphatic sac and cerebrospinal fluid (CSF) space, and placement of a shunt between the endolymphatic sac and the mastoid. The putative goal of sac surgery is to promote the flow of endolymph from the labyrinth to the endolymphatic sac, and thereby relieve hydrops. There is scant published histopathological data as to whether sac surgery actually accomplishes the goal of relieving hydrops. The aim of the present study was to examine the histopathologic changes in temporal bones obtained from individuals who had undergone sac surgery for Meniere’s syndrome during life.
MATERIAL AND METHODS
The material for the study consisted of 15 cases of Meniere’s syndrome with sac surgery contained within the temporal bone collections at Massachusetts Eye and Ear Infirmary (4 cases), the House Ear Institute (10 cases) and University of California at Los Angeles (1 case). All temporal bones were processed in the standard manner for light microscopy (7) which consists of fixation using formalin, decalcification using acid or EDTA, embedding using celloidin, serial sectioning at a thickness of 20 microns and staining of every tenth section using hematoxylin and eosin.
Clinical data collected from each case included age and sex, details of sac surgery, and its effects on vertigo, hearing loss and tinnitus. Control of vertigo was based on clinical documentation of cessation of episodic vertigo after the procedure. We did not use the AAO-HNS 1995 guidelines for vertigo control as the sac surgery in our cases was done prior to the formulation of these criteria, and the medical records did not contain sufficient detail to make the determination using the AAO guidelines. Histopathologic data collected included: 1) Presence or absence of hydrops in the cochlea, saccule, utricle and the ampullae; 2) Severity of hydrops in each location: hydrops was graded as absent, mild, moderate or severe, using a grading scheme that has been previously described (8,9). In brief, mild hydrops consisted of an outward bulging of the labyrinthine membrane in question (e.g. Reissner’s membrane, saccular wall, ampullary wall, utricular wall), severe hydrops consisted of distention of the membrane to become apposed to the bony walls of the surrounding otic capsule, and moderate hydrops was distention in between mild and severe. 3) Patency of the endolymphatic system at the level of the ductus reuniens, saccular duct, utricular duct and the endolymphatic duct, similar to that described by Schuknecht and Ruther (10). 4) Histologic appearance of the sac itself: was it exposed by the surgery? If exposed, did the shunt enter the lumen of the sac?
RESULTS
Table 1 shows detailed results of all 15 cases. Endolymphatic hydrops affecting the cochlea and saccule was present in all 15 cases (100%), with majority of the ears showing moderate or severe hydrops. Utricular hydrops was present in 10 cases (66%), as was ampullary hydrops. Blockage of the lumen of the endolymphatic system was seen in 10 cases (66%). Table 2 summarizes the relationship between sac surgery, presence or absence of hydrops, and relief from vertigo. The 15 cases could be divided into three groups. Group 1: Surgery failed to expose the sac (5 cases). In two of these cases, the sac was hypoplastic and far too anterior for surgical access to be anatomically feasible. In the remaining three cases, the mastoidectomy did not expose the sac, although the latter was in its usual anatomical position. Endolymphatic hydrops was present in all 5 cases; four of the five patients had relief from episodic vertigo after the sac procedure. Group 2: Sac surgery exposed the outside of the sac (the sac was decompressed) but the shunt failed to reach the lumen of the sac. There were 8 such cases; all 8 had endolymphatic hydrops. Of the 8 cases, 4 had relief from vertigo after the procedure. Group 3: The shunt successfully entered the lumen of the sac, 2 cases. Endolymphatic hydrops was present in both. The procedure failed to relieve vertigo in both cases. Figures 1 through 5 illustrate examples of the histologic findings from the three groups. Clinical documentation was not always available regarding the effect of the surgery on improvement in hearing and/or tinnitus; no auditory benefit was noted in the cases where the data was available.
TABLE 1.
Details of Clinical and Histologic Findings for Each Case
| Case Details | Endolymphatic Hydrops* | Patency of Endolymphatic System | Endolymphatic Sac Surgery | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Sex/Age | Cochlea | Saccule | Utricle | Ampullae | Ductus Reuniens |
Saccular Duct |
Utricular Duct |
Endolymph Duct |
Age at Surgery |
Histology of Sac |
Relief from Vertigo |
| 1 (MEEI) | F/91 | + | +++ | + | − | blocked | blocked | blocked | patent | 53 | exposed, not entered | no |
| 2 (MEEI) | M/71 | +++ | + | − | − | blocked | patent | patent | blocked | 63 | not exposed | yes |
| 3 (MEEI) | M/91 | +++ | +++ | + | + | blocked | patent | patent | patent | 60 | not exposed | yes |
| 4 (MEEI) | M/81 | +++ | +++ | − | +++ | blocked | patent | patent | patent | 74 | not exposed | no |
| 5 (HEI) | M/54 | ++ | +++ | + | + | patent | CNA | patent | patent | 52 | not exposed | yes |
| 6 (HEI) | F/71 | ++ | + | + | − | CNA | blocked | blocked | patent | 67 | not exposed | yes |
| 7 (HEI) | F/69 | ++ | +++ | + | + | blocked | patent | Patent | blocked | 55 | exposed, not entered | yes |
| 8 (HEI) | F/67 | ++ | CNA | − | + | patent | patent | patent | patent | 63 | exposed, not entered | no |
| 9 (HEI) | F/56 | + | + | − | − | patent | CNA | patent | patent | 42 | exposed, not entered | no |
| 10 (HEI) | M/51 | +++ | +++ | + | + | patent | patent | patent | patent | 46 | exposed, entered | no |
| 11 (HEI) | M/77 | +++ | +++ | + | + | blocked | patent | patent | patent | 66 | exposed, not entered | no |
| 12 (HEI) | F/82 | ++ | ++ | + | − | patent | patent | patent | patent | 57 | exposed, not entered | yes |
| 13 (HEI) | M/65 | +++ | +++ | ++ | + | CNA | patent | blocked | patent | 56 | exposed, not entered | yes |
| 14 (HEI) | M/69 | +++ | CNA | + | + | blocked | blocked | patent | patent | 50 | exposed, not entered | yes |
| 15 (UCLA) | F/63 | +++ | ++ | ++ | + | CNA | patent | blocked | patent | 46 | exposed, entered | no |
hydrops grading: − none; + mild; ++ moderate; +++ severe
CNA – could not assess
MEEI- Massachusetts Eye and Ear Infirmary; HEI- House Ear Institute; UCLA- University of California, Los Angeles
Table 2.
Summary of Relationship between Sac Procedure, Hydrops and Relief from Vertigo
| Approach to Sac | No. of Cases | Hydrops | Relief from Vertigo |
|---|---|---|---|
| Not exposed | 5 | 5 | 4 |
| Exposed, lumen not entered | 8 | 8 | 4 |
| Lumen entered | 2 | 2 | 0 |
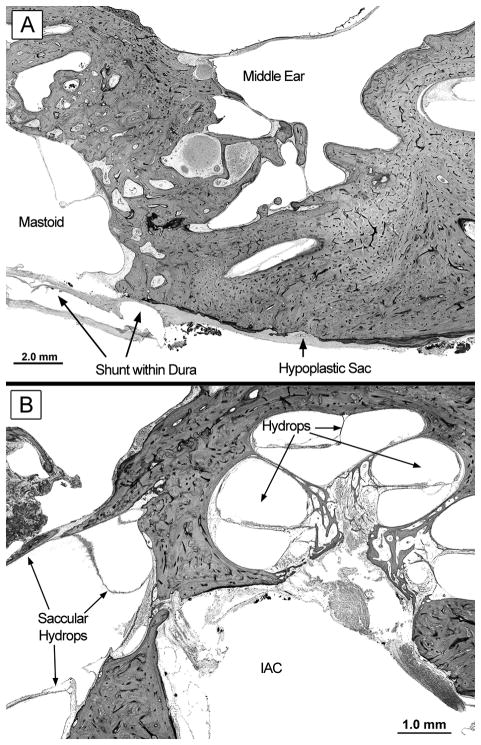
Figure 1.
Case #4 in Table 1. Surgery failed to relieve vertigo.
A. The endolymphatic sac was hypoplastic and situated more anteriorly than normal. The sac was not exposed by the surgery. A silhouette of the shunt is seen within layers of dura.
B. There was diffuse hydrops involving the cochlea and saccule. IAC, internal auditory canal.
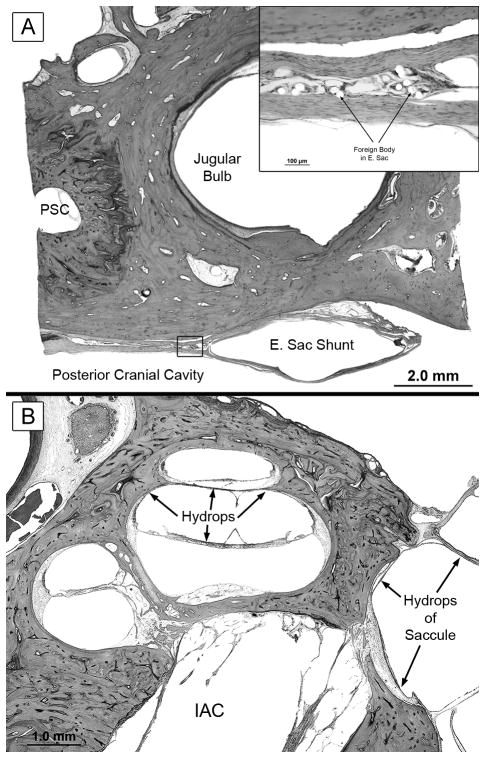
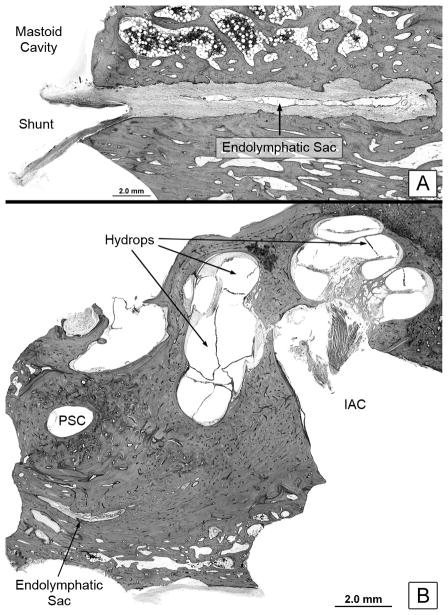
Figure 5.
Case #10 from Table 1. There was no relief from vertigo after sac surgery in this patient.
A. The shunt was correctly placed within the lumen of the sac. Inset shows a high power view of the sac’s lumen showing foreign body reaction to the silastic material of the shunt. PSC, posterior semicircular canal
B. There was severe hydrops involving the cochlea and saccule. Other sections showed hydrops involving the utricle and ampullae. IAC, internal auditory canal.
DISCUSSION
The major finding of the present study was that every case had endolymphatic hydrops. Furthermore, there was no apparent difference in the extent or severity of hydrops whether the surgery exposed the sac or not (Table 1). There was also no difference in hydrops between cases where the anatomical pathway of endolymphatic flow (endolymphatic duct, utricular and saccular ducts, ductus reuniens) was blocked or patent (Table 1). The logical conclusion is that sac surgery did not relieve endolymphatic hydrops in these patients. One limitation of our study is that there was an interval of time between the surgery and death.
The study also showed that successful placement of a shunt within the sac lumen may not occur. Scrutiny of the operative notes of our cases indicated that the surgeon felt that the sac had been decompressed and the shunt placed in the proper location in all cases. On the other hand, the histopathology showed that the surgery failed to expose the sac in 33% of the cases. We did not observe formation of new bone that could have given the appearance of the surgery failing to expose the sac. Furthermore, in the 10 cases where the sac was indeed exposed, the shunt was correctly placed within the sac lumen in only two cases. Part of the difficulty may be the fact that the sac is hypoplastic and anteriorly located in some cases in Meniere’s syndrome (11,12), so that surgical access is not anatomically feasible, as was seen in two of our cases. Another reason for the surgical difficulty may be because the sac flattens out at the level of the posterior fossa dura where its lumen is only a potential space. In trying to locate the sac within the dura, a surgeon might dissect between dural fibers and create a false space that could be mistaken for the sac lumen.
It is interesting that 8 of the 15 cases (53%) obtained relief from episodic vertigo after the sac surgery. In fact, our data suggest an inverse relationship between symptomatic relief and correct anatomical placement of the shunt. As shown in Table 2, relief from vertigo occurred in 4 out of 5 cases when the surgery failed to expose the sac, in 4 out of 8 cases when the sac was exposed but the lumen was not entered, and in no case when the shunt was correctly placed within the lumen of the sac.
Why did 8 of the 15 patients get relief from vertigo? We found that relief from vertigo cannot be ascribed to resolution of hydrops. It has been proposed that sac surgery may help by inducing a mild labyrinthitis or destroying sac function (13). However, our data do not support these hypotheses since more patients got relief when surgery failed to even expose the sac compared to those when the sac was indeed exposed or entered.
A possible explanation for the observed symptomatic relief from vertigo is a placebo effect (14). Alternately, the procedure may have had a real biologic effect, either locally or systemically, that reset the threshold for attacks of vertigo to a higher level. We point out that the pathophysiology of episodic vertigo in Meniere’s syndrome remains unknown. Insight into the mechanism of vertigo and the observed relief from sac surgery needs further research.
CONCLUSION
Endolymphatic sac surgery does not relieve endolymphatic hydrops in patients with Meniere’s syndrome. Yet, sac surgery does relieve vertigo in some patients, but the mechanism of such symptomatic relief remains unknown.
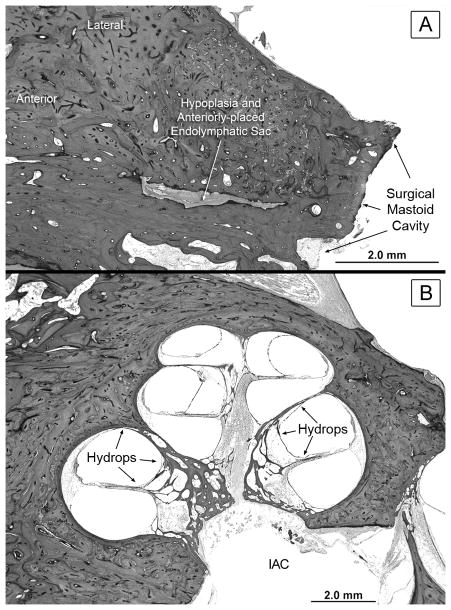
Figure 2.
Case #2 in Table 1. The surgery relieved this patient’s vertigo.
A. The sac was hypoplastic and anteriorly placed, and was not exposed by the surgery.
B. There was diffuse hydrops in all three turns of the cochlea. The saccule was also hydropic (not shown). IAC, internal auditory canal.
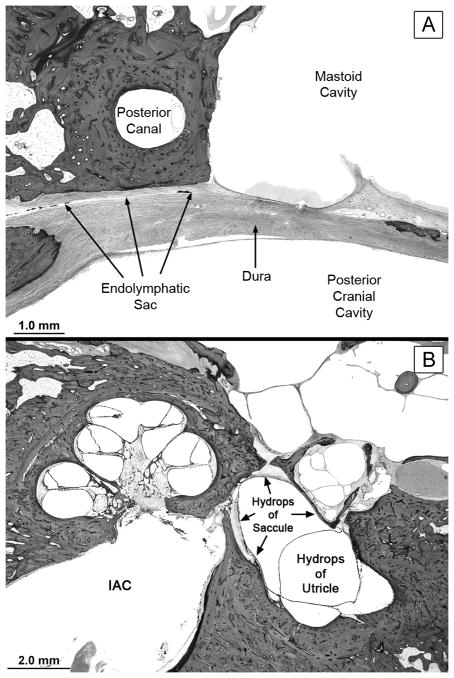
Figure 3.
Case #1 from Table 1. Surgery failed to relieve vertigo.
A. The endolymphatic sac was exposed at surgery but the shunt was not placed within the sac’s lumen.
B. There was hydrops involving the cochlea, saccule and utricle. IAC, internal auditory canal.
Figure 4.
Case #12 from Table 1. The surgery relieved this patient’s vertigo.
A. The sac was exposed, but the shunt failed to enter its lumen.
B. There was hydrops involving the cochlea, saccule, and utricle. PSC, posterior semicircular canal. IAC, internal auditory canal.
Acknowledgments
Supported by the NIDCD Human Temporal Bone Consortium for Research Resource Enhancement (U24 DC 008559).
References
- 1.Ménière P. Sur une forme de surdité grave dépendant d'une lésion de l'oreille interne. Gaz Méd de Paris. 1861;16:29. [Google Scholar]
- 2.Portmann G. Vertigo: Surgical treatment by opening saccus endolymphaticus. Arch Otolaryngol. 1927;6:309–315. doi: 10.1001/archotol.1969.00770020811005. [DOI] [PubMed] [Google Scholar]
- 3.Yamakawa K. Uber die pathologisch Veranderung bei einem Ménière -Kranken. J Otorhinolaryng Soc Japan. 1938;4:2310–2312. [Google Scholar]
- 4.Hallpike CS, Cairns H. Observations on the pathology of Ménière's syndrome. J Laryngol Otol. 1938;53:625–655. doi: 10.1177/003591573803101112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.House WF. Subarachnoid shunt for drainage of endolymphatic hydrops. A preliminary report. Laryngoscope. 1962;72:713–29. doi: 10.1288/00005537-196206000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Schuknecht HF, McKenna MJ. Shunt procedures. In: Nadol JB, McKenna MJ, editors. Surgery of the Ear and Temporal Bone. Lippincott, Williams and Wilkins; Philadelphia: 2004. pp. 378–380. [Google Scholar]
- 7.Merchant SN. Schuknecht's Pathology of the Ear. 3. PMPH USA; Shelton, Connecticut: 2010. Methods of Removal, Preparation and Study; pp. 3–51. [Google Scholar]
- 8.Rauch SD, Merchant SN, Thedinger BA. Meniere's syndrome and endolymphatic hydrops--a double blind temporal bone study. Ann Otol Rhinol Laryngol. 1989;98:873–83. doi: 10.1177/000348948909801108. [DOI] [PubMed] [Google Scholar]
- 9.Lin MY, Timmer FCA, Oriel BS, Zhou G, Guinan JJ, Kujawa SG, Herrmann BS, Merchant SN, Rauch SD. Vestibular evoked myogenic potential (VEMP) can detect asymptomatic saccular hydrops. Laryngoscope. 2006;116:987–992. doi: 10.1097/01.mlg.0000216815.75512.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schuknecht HF, Rüther A. Blockage of longitudinal flow in endolymphatic hydrops. Eur Arch Otorhinolaryngol. 1991;248:209–217. doi: 10.1007/BF00173659. [DOI] [PubMed] [Google Scholar]
- 11.Khetarpal U, Schuknecht HF. Temporal bone findings in a case of bilateral Meniere's disease treated by parenteral streptomycin and endolymphatic shunt. Laryngoscope. 1990;100:407–14. doi: 10.1288/00005537-199004000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Feghali JG, Linthicum FH, Jr, Xenellis JE. Is the endolymphatic sac always accessible? Otolaryngol Head Neck Surg. 1985;93:21–3. doi: 10.1177/019459988509300104. [DOI] [PubMed] [Google Scholar]
- 13.Welling DB, Pasha R, Roth LJ, Barin K. The effect of endolymphatic sac excision in Meniere's disease. Am J Otol. 1996;17:278–82. [PubMed] [Google Scholar]
- 14.Thomsen J, Bretlau P, Tos M, Johnsen NJ. Placebo effect in surgery for Meniere's disease. A double-blind, placebo-controlled study on endolymphatic sac shunt surgery. Arch Otolaryngol. 1981;107:271–7. doi: 10.1001/archotol.1981.00790410009002. [DOI] [PubMed] [Google Scholar]