Abstract
Ninety seven outpatients with schizophrenia spectrum disorders (SSDs) were randomly assigned to the Walk, Address Sensations, Learn About Exercise, Cue Exercise Behavior for SSDs (WALC-S), a motivational intervention designed to increase exercise in SSDs (n =48), or a time and attention control group (TAC, n =49). WALC-S and TAC groups met weekly for four weeks before a 16 week walking program was offered to all subjects. We compared the exercise attendance, persistence and compliance of the groups during the walking program. WALC-S recipients attended more walking groups, for more weeks and walked more minutes than those receiving TAC. Percent of WALC-S or TAC groups attended was significantly correlated with overall attendance (r = 0.38, p = 0.001) and persistence (r = −.29, p = 0.01), as well as number of minutes walked. This study is among the first to examine interventions designed to enhance exercise motivation in SSDs.
Keywords: schizophrenia, community, exercise, motivation
Introduction
Death rates from diabetes, respiratory/cardiovascular, and other obesity-related illnesses are significantly higher among the nearly 2 million Americans with schizophrenia spectrum disorders (SSDs=schizophrenia, schizoaffective disorder and schizophreniform disorder) than in the general population (American Psychiatric Association, 2000). The most effective medications for managing SSDs (second generation antipsychotics (SGAs) such as clozapine and olanzapine) are associated with weight gain, glucose dysregulation and diabetes (Ananth, et al, 2004; Jin, Meyer & Jeste, 2004; Newcomer, 2004). Yet, despite the well-known benefits of exercise and the health dangers associated with obesity, persons with SSDs seldom exercise; they are less physically active and fit than people with no mental illness or with other mental illnesses (Beebe, 2005; Chamove, 1986 Hogdon & Reimer, 1960; Morgan, 1974; Lindquist, 1981). Exercise barriers in this group include amotivation, poor concentration, sedative effects of medication, poverty, and lack of access to exercise education and programs.
A few mostly quasi-experimental studies using small numbers of SSD subjects consistently document both psychiatric (reduced depression and anxiety—Acil, Dogan and Dogan, 2008;Chamove, 1986;Gimino and Levin, 1985;Pelham, Campagna, Ritvo, and Birnie,1993) and physical (flexibility, weight loss and/or body mass index) health improvements(Centorrino, et al, 2006;Chen,Chen, and Huang, 2009;Fogarty, Happell, and Pininkahana, 2004;Kwon, et al, 2006 Pendlebury, Haddad, and Dursun, 2005;Vreeland, et al, 2003;) in response to exercise, but investigations were plagued by difficulties. Every investigation reporting attendance or attrition documented significant problems motivating subjects-attrition rates up to 36% after only 8 weeks and exercise attendance as low as 23% (Centorrino, et al, 2006;Chen, Chen, and Huang, 2009;Kwon, et al,2006; Pelham, Campagna, Ritvo, and Birnie,1993;Pendlebury, Haddad, and Dursun, 2005;Vreeland, et al,2003;). The single study not reporting health improvements (Ball, Coons, and Buchanan, 2001) had extreme motivation problems, including, low attendance (no one attended more than 50% of sessions) and high attrition (33% in 10 weeks). These studies demonstrate the necessity of including motivation in examinations of exercise behavior in this group.
Two studies have addressed exercise motivation in SSDs. Archie and colleagues (2003) provided free access to a fitness facility to 20 outpatients for 6 months and monitored their exercise. Dropout was 40% after 4 months, 70% after 5 months and 90% after 6 months. These rates compare unfavorably with general population exercise cessation (50% after 6 months). The main reason given for dropout was lack of motivation. Menza, et al (2004) tested a one-year weight control program of counseling and exercise in 51 SSD outpatients. Weight and BMI decreased significantly in experimental subjects; study attrition was 34% and average exercise attendance was 69%. This study shows that interventions can increase exercise in SSDs, however, because the control group did not participate in exercise, it is not possible to separate the motivational effects of the intervention from the effects of the attention and reinforcement subjects would have received by virtue of exercise alone. Further, the inclusion of multiple treatments in the Menza, et al (2004) intervention prohibits conclusions as to which specific component(s) were responsible for outcomes.
This modest body of literature has numerous limitations. Most studies were single group investigations of 40 subjects or less. Among only three randomized studies, the longest follow up period was 12 weeks. A significant issue in every investigation in which such data were reported, was difficulty motivating subjects to attend, adhere and complete planned exercises. It is imperative that researchers turn their attention to interventions to enhance motivation, to support persons with SSDs to garner maximum health benefits. This study tested the Walk, Address sensations, Learn about exercise, Cue exercise behavior for Schizophrenia Spectrum Disorders (WALC-S), a motivational group intervention designed to increase exercise behavior. We hypothesized that, compared to a time and attention control (TAC) group, WALC-S subjects would have higher exercise attendance, persistence and compliance at a community-based walking program.
Methods
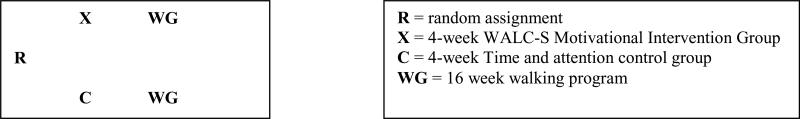
Ninety seven outpatients with SSDs were randomly assigned to WALC-S or TAC. WALC-S and TAC groups met for one hour weekly for four weeks prior to a 16 week walking program that was offered to all subjects. We compared the attendance, persistence and compliance of WALC-S and TAC subjects during the walking program. See Figure 1.
Figure 1.
Study Design.
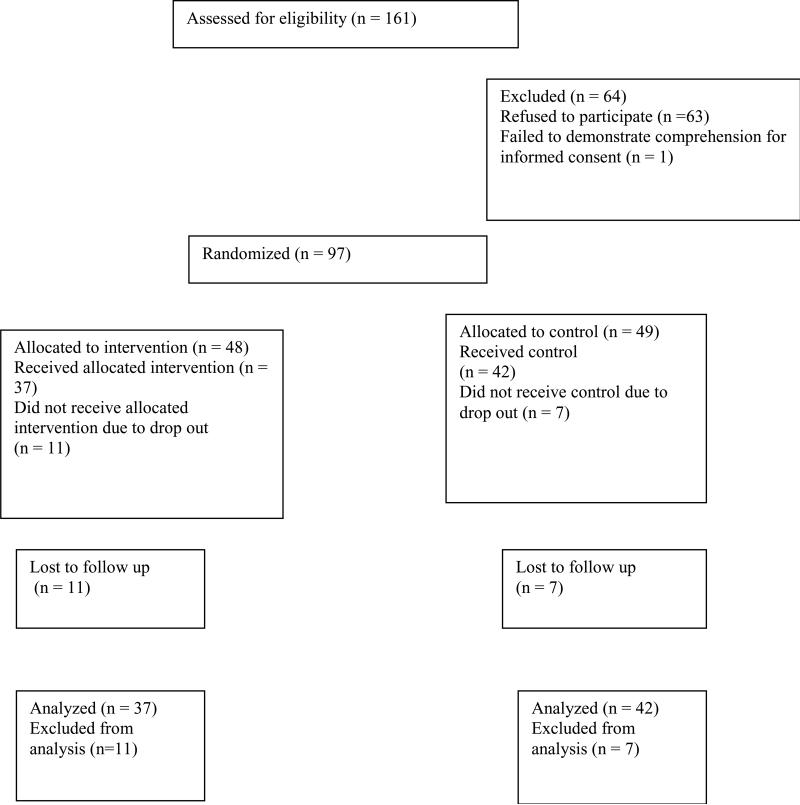
Subjects were outpatients with SSDs receiving care at a community mental health center (CMHC) located in the Southeastern United States. After verifying that subjects met study criteria, we documented basic understanding of study purposes and procedures using an assessment of capacity for research consent developed at the Maryland Psychiatric Research Center and used in our prior work (Beebe & Smith, in press; Carpenter et al., 2000; DeRenzo, Conley, & Love, 1998). After potential subjects demonstrated consent capacity, written informed consent was obtained. Inclusion criteria were: 1) a chart diagnosis of schizophrenia, schizoaffective disorder or schizophreniform disorder, any subtype, according to the criteria described in the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV, American Psychiatric Association, 2000), 2) English speaking, 3) Stable medication regimen (no medication changes within the last month), and 4) medical clearance for moderate exercise in writing from primary care provider. Exclusion criteria included chart documentation of mental retardation, developmental delay, uncorrected visual, hearing impairments or the following physical conditions: 1) hospitalization within the past 12 months for angina pectoris, myocardial infarction, or cardiac surgery, 2) congestive heart failure, 3) cardiac pacemaker, 4) heart rate > 100 or < 50 at rest, 5) uncontrolled hypertension (blood pressure exceeding 140/90 on 3 consecutive readings despite adequate treatment), 6) history of spinal or hip fractures or hip or knee arthroplasty, 7) neuromuscular/orthopedic limitations to normal, unassisted ambulation. We approached 161 persons over 20 months. See figure 2. We used a computer-generated random number table to assign patients to WALC-S or TAC in a 1:1 ratio.
Figure 2.
Study enrollment and Completion Rates.
Sixty-nine (71.1%) subjects were diagnosed with schizoaffective disorder and the remainder with schizophrenia. A slight majority were Caucasian (n = 53, 54.6%) and male (n = 51, 52.6%). Most subjects lived with family members (n = 42, 43.35%); their average age was 46.9 years (SD = 2.0). The most commonly prescribed medications were oral SGAs (n = 68, 65.9%) followed by antiparkinsonian medications (n = 54, 55.6%) and antidepressants (n = 46, 47.4%). See table 1.
Table 1.
Characteristics of subjects with schizophrenia spectrum disorders (N = 97).
| Characteristic | All Subjects (N = 97) | WALC-S Subjects (n = 48) | TAC Subjects (n = 49) |
|---|---|---|---|
| Diagnosis | n,% | n,% | n,% |
| Schizoaffective | 69(71.1) | 30(62.5) | 39(79.6) |
| Schizophrenia | 28 (28.9) | 18(37.5) | 10(20.4) |
| Sex | |||
| Female | 46(47.4) | 25(52.1) | 21(42.9) |
| Male | 51(52.6) | 23(47.9) | 28(57.1) |
| Race | |||
| Caucasian | 53(54.6) | 23(47.9) | 30(61.2) |
| African American | 43(44.4) | 24(50) | 19(38.8) |
| Asian | 1(1) | 1(2.1) | 0(0) |
| Living Arrangement | |||
| Alone | 36(37.1) | 15(31.3) | 21(42.9) |
| With family | 42(43.3) | 23(47.9) | 19(38.8) |
| With paid caregiver | 19(19.6) | 10(20.8) | 9(18.4) |
| Educational Level * | |||
| Less than HS | 36(40.9) | 21(48.8) | 15(33.3) |
| HS graduate | 36(40.9) | 15(34.8) | 21(46.6) |
| More than HS | 16(18.2) | 7(16.4) | 9(20.1) |
| Prescribed Medications | |||
| Oral SGAs | 68 (65.9) | 23(48) | 20(40.8) |
| Oral FGAs | 5 (5.2) | 2(4.2) | 2(4.1) |
| Depot FGAs | 38(39.2) | 13(27.1) | 12(24.5) |
| Depot SGAs | 10(10.3) | 3(6.3) | 5(10.2) |
| Antidepressants | 46(47.4) | 15(31.3) | 11(22.4) |
| Mood stabilizers | 29(29.8) | 17(35.4) | 12(24.5) |
| Antianxiety | 26(26.8) | 10(20.8) | 6(12.2) |
| Antiparkinsonian | 54(55.6) | 22(45.8) | 21(42.8) |
| Hypnotics | 13(13.4) | 4(8.3) | 3(6.1) |
| Other* | 75(77.3) | 27(56.3) | 20(40.1) |
Notes:
other = Medications prescribed for physical illnesses, most commonly antihypertensives (n = 35), proton pump inhibitors (n = 31) and lipid lowering agents (n = 27).
# = missing data
HS = high school
SGAs = second-generation antipsychotics
FGAs = first generation antipsychotics
Treatment groups
WALC-S. Details of the WALC-S have been published elsewhere (Beebe & Smith, 2010). In brief, the WALC-S consisted of four weekly, hour-long groups (8 subjects per group) incorporating content based upon self efficacy theory and conducted by K Smith. In brief, groups included: W (Walking information)-- The WALC-S did not include walking, merely a discussion of the basics of walking for exercise and information on walking safely (i.e. stay hydrated, wear layers of clothing, warm up muscles before walking). Warm up/cool down exercises were performed at each WALC-S group. Assistance was provided to assist with setting individualized exercise and/or attendance goals and group content was supplemented by written materials. A (Address sensations)—Subjects were queried about discomforts during warm up and cool down exercises and observed for nonverbal indications of discomfort. Written materials provided suggestions on reducing exercise discomforts, such as using heat or massage for muscular soreness. L (learn about exercise)—Subjects were provided information about exercise benefits and overcoming barriers to exercise, supplemented by written materials, and assisted to generate solutions to barriers if necessary. C (cue exercise)—Subjects were provided calendars with walking days and times clearly marked to cue walking group attendance. Reminder calls were made before each WALC-S group; subjects who missed group received a follow up call.
TAC. The TAC group consisted of four weekly, hour long groups (8–9 subjects per group) conducted by K. Smith. TAC groups focused on health behaviors such as medication adherence, smoking cessation, the use of humor and progressive muscle relaxation, but included no exercise or motivational content. Reminder calls were made before each TAC group; subjects who missed group received a follow up call.
16-week walking program (all subjects). Since the purpose of this study was to examine the effect of the WALC-S intervention on exercise behavior, walking groups were identical in activities and content. Two different blinded graduate students provided walking groups to experimental and control subjects. Walking groups met on Mondays, Wednesdays and Fridays at the recruitment site and walked outdoors (weather permitting) for 16 consecutive weeks. Walking groups began with warm up stretches followed by walking, beginning with 5 minutes and gradually increasing to 30 minutes over the first four weeks. Cool-down exercises (after each walk) consisted of 5 minutes of slow walking followed by cool-down stretches. Reminder calls were made before each walking group, subjects who missed group received a follow up call.
Measures
Walking group attendance was defined as the ratio of number of walking groups attended to total number of walking groups offered. For example, a person attending 24 walking groups of the total 48 offered had an attendance rate of 50%.
Walking group persistence was defined as the number of weeks the subject attended at least one walking group.
Walking group compliance was defined as the total number of minutes each subject walked during the walking groups each month.
Data collection occurred over two years. Data regarding sociodemographic characteristics, living arrangements and prescribed medications was collected via record review at study entry. Attendance, persistence and compliance (minutes walked) were monitored by study personnel and documented at every walking group. Subjects were provided new athletic shoes at the first WALC-S or TAC meeting, and received a $10.00 grocery gift certificate at weeks one and sixteen of the walking group. Prior to data collection, university Institutional Review Board (IRB) approval as well as the approval of the research committee at the CMHC were obtained. The authors declare no conflicts of interest and all authors certify responsibility for this manuscript.
Results
The characteristics of subjects assigned to WALC-S and TAC groups are presented in Table 1. There were no statistically significant baseline differences between the two groups in any variables examined. Table 2 shows the mean attendance, persistence in weeks and minutes walked per month for subjects in the two groups. Experimental subjects attended more walking groups, persisted for longer time periods, and walked more minutes than controls throughout the walking program. For example, experimental subjects walked, on average, 15 more minutes during month one, 30 more minutes during month two, 36 more minutes during month three and 38 more minutes during month four than controls.
Table 2.
Walking program percent attendance, persistence in weeks, and minutes walked per month of WALC-S (n = 48) and TAC (n = 49) subjects with schizophrenia spectrum disorders.
| Measure | Month 1 Mean, SD | Month 2 Mean, SD | Month 3 Mean, SD | Month 4 Mean, SD |
|---|---|---|---|---|
| Percent attendance | ||||
| WALC-S | 35.2(34.7) | 28.4(35.3) | 27.9(35.4) | 27.3(32.8) |
| TAC | 33.7(35.1) | 25.9(31.6) | 24.0(32.1) | 22.9(32.6) |
| Persistence in weeks | ||||
| WALC-S | 2.7(1.5) | 4.9(3.1) | 6.97(4.9) | 9.1(6.5) |
| TAC | 2.4(1.6) | 4.3(3.1) | 5.95(4.6) | 7.5(6.2) |
| Minutes Walked | ||||
| WALC-S | 76.67(62.6) | 123.19(127.6) | 116.59(127.6) | 116.89(117.3) |
| TAC | 61.88(58.6) | 93.97(108.7) | 80.71(106.2) | 78.83(106.4) |
Note-WALC-S = experimental group, TAC = time-and-attention control group.
To test the hypotheses that subjects receiving the WALC-S would have higher attendance, persistence and minutes walked than those receiving TAC, data were analyzed using a series of repeated measures mixed models considering each outcome over time via the SAS procedure Proc MIX. Models were run with and without adjusting for associated, possibly confounding, variables including basic socio demographic variables. Hypothesis tests from the various models as well as parameter estimates or least squares means were examined. Missing data were excluded, and we considered results significant at P ≤ alpha (.05). Table 3 shows the results of these analyses.
Table 3.
Mixed results for examination of attendance, persistence and compliance over time in the walking program in persons with schizophrenia spectrum disorders.
| Percent attendance per month | Persistence in weeks | Minutes walked per month | ||||
|---|---|---|---|---|---|---|
| Effects | Unadjusted P-value | Adjusteda P-value | Unadjusted P- value | Adjustedb P-value | Unadjusted P-value | Adjustedc P-value |
| Group | 0.831 | 0.083 | 0.739 | 0.860 | 0.409 | 0.139 |
| Time | 0.0005 | 0.0007 | 0.0007 | 0.0001 | 0.0002 | 0.0002 |
| Group * Time | 0.074 | 0.967 | 0.967 | 0.526 | 0.671 | 0.671 |
Note:
adjusted for age, WALC-S attendance, and the prescription of Anti Parkinsonian medications
adjusted for WALC-S attendance, total number of prescriptions, number of prescriptions for physical illnesses, and prescription of anti Parkinsonian medications
adjusted for age, WALC-S attendance, age, race, and the prescription of Anti Parkinson medications
Based on the statistical tests there was no statistically significant time by group interaction for any outcome thus we cannot conclude there was a difference in change over time for the treated group versus the control group. There was a significant time effect overall for attendance, in that reductions in attendance rates were significant over time in both groups. Likewise, there was a significant time effect in that persistence increased over time. Control group persistence increased by 5.1 weeks from month 1 to month 4, while experimental group persistence increased by 6.4 weeks over the same time period. Finally, there was a significant time effect overall for minutes walked, in that experimental subjects walked 47 more minutes during month 2 than month 1, and maintained their minutes walked without decline from month 3 to month 4. In contrast, control subjects walked only 32 minutes more during month 2 than month 1, and minutes walked for control subjects declined during both month 3 and 4.
To further investigate outcomes, additional models were examined, taking into consideration possible confounding variables. We included those variables that were significant in the previous models for each outcome. For the attendance outcome, we included age, WALC-S attendance, and the receipt of antiparkinsonian medication. For the persistence outcome, we included WALC-S attendance, total number of prescriptions, and number of prescriptions for physical illnesses. For the compliance (minutes walked) outcome, we included age, race, WALC-S attendance, and the receipt antiparkinsonian medication. Results remained consistent after controlling selected variables for any effects for any outcome. See Table 3.
Additional analyses. Correlation analyses were undertaken to further examine strength and direction of relationships between variables. Results of this analysis are presented in table 4. Age was positively and significantly correlated with overall attendance and persistence as well as number of minutes walked throughout the walking program. Percent of WALC-S or TAC groups attended was positively and significantly correlated with overall attendance and persistence, as well as number of minutes walked throughout the walking program.
Table 4.
Pearson correlations of walking behavior in persons with schizophrenia spectrum disorders.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Age | 1 | 0.06 | 0.32a | 0.28b | 0.28b | 0.25c | 0.27b | 0.26b |
| 2. % of WALC-S or TAC groups attended | 1 | 0.38a | 0.29b | 0.39 | 034a | 0.34a | 0.30a | |
| 3. % of walking groups attended | 1 | 0.95d | 0.90d | 0.93d | 0.92d | 0.95d | ||
| 4. Persistence in weeks | 1 | 0.85d | 0.89d | 0.86d | 0.88d | |||
| 5. Minutes walked-month 1 | 1 | 0.85d | 0.75d | 0.80d | ||||
| 6. Minutes walked-month 2 | 1 | 0.89d | 0.87d | |||||
| 7. Minutes walked-month 3 | 1 | 0.93d | ||||||
| 8. Minutes walked-month 4 | 1 |
Note:
P value = 0.001
P value = 0.01
P value = 0.027
P value = 0.000
For further details on WALC-S and TAC attendance, we collected data on reasons for missing WALC-S or TAC groups via telephone follow up. Reasons for missing WALC-S or TAC groups are presented in Table 5. Of those contacted (n = 63), the most common reasons given for missing group were transportation problems (n = 14, 22.2%), physical illness (n = 13, 20.6 %) and conflict with another appointment (n = 8, 12.7%). Chi square analyses revealed that experimental subjects were significantly more likely to cite transportation difficulties than controls (χ2 = 4.63, n = 78, df = 1, p = 0.031).
Table 5.
Reasons given by persons with schizophrenia spectrum disorders for missing WALC-S and TAC groups (N = 63).
| Reason | WALC-S Group Subjects Contacted n,% | TAC Group Subjects Contacted n, % | All Subjects Contacted n,% |
|---|---|---|---|
| Transportation problem | 12(28.6) | 2 (9.5) | 14(22.2) |
| Physical illness | 10(23.8) | 3(14.3) | 13(20.6) |
| Conflict with another appointment | 3(7.1) | 5(23.8) | 8(12.7) |
| Forgot | 4(9.5) | 2(9.5) | 6(9.5) |
| Working | 5(11.9) | 1(4.8) | 6(9.5) |
| No reason given | 2(4.8) | 2(9.5) | 4(6.3) |
| Prefer not to | 2(4.8) | 2(9.5) | 4(6.3) |
| Too busy | 2(4.8) | 2(9.5) | 2(3.2) |
| No Babysitter | 0(0) | 2(9.5) | 2(3.2) |
| Hospitalized | 1(2.4) | 0(0) | 1(1.6) |
| Incarcerated | 1(2,4) | 0(0) | 1(1.6) |
| Total | 42 | 21 | 63 |
Note: WALC-S = Experimental group; TAC = Time-and-attention control group.
Discussion
This study adds to a growing body of literature on exercise and exercise motivation in persons with SSDs. Our enrollment rate of 60.6% (97 agreed of 160 eligible) is similar to that observed in our prior work (Beebe, 2001; Beebe& Tian,2004; Beebe et al, 2005), as well as one other study documenting rates of refusal for exercise research in SSDs. Ball, Coons and Buchanan (2001) conducted a single group study in which 15 agreed of 24 eligible (62.5%).
Our attrition rate of 18.6% over four months is lower than documented rates of 36% in studies of two months' duration (Centorrino, et al, 2006;Chen, Chen, and Huang, 2009;Kwon, et al,2006; Pelham, Campagna, Ritvo, and Birnie,1993;Pendlebury, Haddad, and Dursun, 2005;Vreeland, et al,2003;), 33% in a 10 week study (Ball, Coons and Buchanan, 2001), and lower than the 40% drop out noted by Archie et al (2003) over four months. Our relatively low attrition may be the result of the study design, in which the pre-walking groups provided opportunities for the establishment of rapport in both experimental and control groups. The influence of relationship with providers on engagement and appointment attendance in persons with SSDs is well known (Hardeman, Harding & Narasimhan, 2010; Kikkert et al, 2006; Thomas et al, 2009). Finally, our attrition rate was lower than the 34% observed in the one-year Menza et al (2004) investigation. In contrast to the Menza (2004) study however, our intervention was less intensive and our follow up period shorter. Our low attrition may be due to sample characteristics (majority with schizoaffective disorder and living with a support persons), the use of telephone reminders regarding study activities, or other factors.
Our exercise attendance was 38.5% in experimental subjects, and 31.4% in controls over four months, which compares favorably to exercise rates between 23–49% in other investigations (Centorrino, et al, 2006;Chen, Chen, and Huang, 2009;Kwon, et al,2006; Pelham, Campagna, Ritvo, and Birnie,1993;Pendlebury, Haddad, and Dursun, 2005;Vreeland, et al,2003;Ball, Coons and Buchanan, 2001). We observed an overall attendance of 34.95% for all exercisers regardless of group assignment, compared to an attendance of 69% over 1 year for the Menza investigation (2004). Differences observed may in part be explained by intervention intensity; the Menza (2004) study intervention continued throughout the entire follow up period, whereas our intervention was offered before the exercise program only. Our next study will examine the effect of periodic boosters of the motivational intervention upon long-term exercise outcomes.
To our knowledge, this is the first investigation to report correlations related to exercise behavior in SSDs. Our finding that age was correlated with walking program attendance, persistence and minutes walked may be related to increased psychiatric stability and insight over time, a better understanding of health benefits, greater experience accessing transportation options, or greater service engagement in older as compared to younger persons. Our finding of a correlation between pre-group attendance (WALC-S or TAC) and attendance, persistence and minutes walked indicates that attendance at the pre-walking groups (WALC-S or TAC), rather than the specific content or activities during the pre-groups, was positively associated with walking program attendance and performance. Possible explanations include housing, social support or transportation stability associated with the ability to attend the pre-groups, group dynamics such as universality (Yalom, 2005), that occurred independently of content covered during the pre-groups, a high value placed on exercise at the outset of the study or other factors yet to be identified.
In regard to reasons for missed groups, one other study (Archie et al 3002) examined the reasons for nonattendance at an exercise facility by 20 persons with SSDs over 6 months. Archie provided no intervention, but merely monitored reasons for nonattendance at the facility. These authors reported the most common reason for nonattendance was lack of motivation (6 persons), followed by being uncomfortable in the exercise setting and having to exercise alone (2 persons), and finally housing instability, psychiatric symptoms and medication changes (1 person). In contrast, our subjects most commonly cited reasons for nonattendance were transportation problems (n = 14, 22.2%), physical illness (n = 13, 20.6%) and conflict with another appointment (n = 8, 12.7%), none of which were cited by Archie's subjects. The differences in reasons for nonattendance at exercise sessions may relate to study design, since the Archie subjects attended the exercise facility on their own and thus had the option of attending whenever their schedule allowed, whereas our subjects had to accommodate to the group walking schedule, and occasionally our walking schedule conflicted with their other appointments. Likewise, our study design ensured that all subjects had someone with which to exercise, in contrast to Archie's subjects who had to make their way to the facility and perform exercises on their own. Finally, our Chi square analysis revealed that persons assigned to the experimental group were significantly more likely to report transportation problems than those in the control group (χ2 = 4.63, n = 78 df = 1, p = 0.031). No other significant differences were noted between reasons for nonattendance between our two groups. These findings indicate a broad range of reasons for nonattendance that should be taken into account in program planning.
Limitations. There are several reasons our results must be viewed with caution. Our high rate of refusal, while similar to other investigations with this population (Beebe, 2001; Beebe & Tian, 2004; Beebe et al, 2005), may have resulted in a nonrepresentative sample if persons with inherently lower exercise motivation refused to participate. Study attrition resulted in a sample size of 79 at the final measurement point (37 experimental and 42 control subjects). This scenario introduces the possibility of lack of identification of significant relationships due to lack of power. In our initial power analysis, we concluded that a sample size of 32 in each group would have 90% power to detect a 25% increase in attendance; while our final sample met this goal, experimental exercise attendance increased by only 9% at month 4, and thus the sample size may have been inadequate because differences between groups were smaller than anticipated.
This study is among the first to examine interventions designed to enhance exercise motivation in SSDs. Identification of interventions to increase exercise is critical to improve physical health and quality of life. We conclude that, while our intervention shows promise in that all outcomes were in the predicted direction, the effect of the intervention was smaller than anticipated and further, intervention effects appear to be attenuated over time. Our next study will examine the effect of periodic boosters of the motivational intervention and includes a larger number of subjects to enhance detection of small effect sizes. Our ultimate goal is to develop interventions and exercise programs that will be acceptable to persons with SSDs, feasible to deliver as part of available treatment programs, and result in objective improvements in physical health outcomes.
Acknowledgments
Grant support: This study supported by a grant from the National Institutes of Mental Health, 1R03MH79047-02
References
- Acil AA, Dogan S, Dogan O. The effects of physical exercises to mental state and quality of life in patients with schizophrenia. Journal of Psychiatric and Mental Health Nursing. 2008;15:808–815. doi: 10.1111/j.1365-2850.2008.01317.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text revision. [Google Scholar]
- Ananth J, Venkatesh R, Burgoyne K, Gadasalli R, Binford R, Gunatilake S. Atypical antipsychotic induced weight gain: Pathophysiology and management. Annals of Clinical Psychiatry. 2004;16(2):75–85. doi: 10.1080/10401230490453293. [DOI] [PubMed] [Google Scholar]
- Archie W, Wilson JH, Osborne S, Hobbs H, McNiven J. Pilot study: Access to fitness facility and exercise levels in olanzapine-treated patients. Canadian Journal of Psychiatry. 2003;48(9):628–632. doi: 10.1177/070674370304800910. [DOI] [PubMed] [Google Scholar]
- Ball MP, Coons VB, Buchanan RW. A program for treating olanzapine related weight gain. Psychiatric Services. 2001;52:967–969. doi: 10.1176/appi.ps.52.7.967. [DOI] [PubMed] [Google Scholar]
- Beebe LH, Smith K. Describing in formed consent in schizophrenia spectrum disorders. International Journal of Nursing Ethics. doi: 10.1177/0969733010364581. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beebe LH, Smith K. Feasibilty of the Walk,Address, Learn and Cue (WALC) Intervention for schizophrenia spectrum disorders. Archives of Psychiatric Nursing. 2010;24(1):54–62. doi: 10.1016/j.apnu.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beebe LH, Tian L, Morris N, Goodwin A, Swant-Allen S, Kuldau J. Effects of exercise on mental and physical health parameters of persons with schizophrenia. Issues in Mental Health Nursing. 2005;26:661–676. doi: 10.1080/01612840590959551. [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Jr., Gold JM, Lahti AL, Queem LA, Conley RR, Bartko JJ, Kovnick J, Appelbaum PS. Decisional capacity for informed consent in schizophrenia research. Archives of General Psychiatry. 2000;57(6):533–538. doi: 10.1001/archpsyc.57.6.533. [DOI] [PubMed] [Google Scholar]
- Centorrino F, Wurtman JJ, Duca KA, Fellman VH, Fogarty KV, Berry JM, Guay DM, Romeling M, Kidwell J, Cincotta CL, Baldessarini RJ. Weight loss in overweight patients maintained on atypical antipsychotic agents. International Journal of Obesity. 2006;30:1011–1016. doi: 10.1038/sj.ijo.0803222. [DOI] [PubMed] [Google Scholar]
- Chamove AS. Positive short-term effects of activity on behavior in chronic schizophrenic patients. British Journal of Clinical Psychology. 1986;25:125–133. doi: 10.1111/j.2044-8260.1986.tb00681.x. [DOI] [PubMed] [Google Scholar]
- Chen CK, Chen YC, Huang YS. Effects of a 10-week weight control program on obese patients with schizophrenia or schizoaffective disorder: a 12-month follow up. Psychiatry and Clinical Neuroscience. 2009;63(1):17–22. doi: 10.1111/j.1440-1819.2008.01886.x. [DOI] [PubMed] [Google Scholar]
- DeRenzo EG, Conley RR, Love R. Assessment of capacity to give consent for research: state of the art and beyond. Journal of HealthCare Law and Policy. 1998;1:66–87. [PubMed] [Google Scholar]
- Fogarty M, Happell B, Pininkahana J. The benefits of an exercise program for people with schizophrenia: A pilot study. Psychiatric Rehabilitation Journal. 2004;28(2):173–176. doi: 10.2975/28.2004.173.176. [DOI] [PubMed] [Google Scholar]
- Gimino FA, Levin SJ. The effects of aerobic exercise on perceived self-image in post-hospitalized schizophrenic patients. Medicine and Science in Sports and Exercise. 1984;16:139. [Google Scholar]
- Hardeman SM, Harding RK, Narasimhan M. Simplifying adherence in schizophrenia. Psychiatric Services. 2010;61(4):405–8. doi: 10.1176/ps.2010.61.4.405. [DOI] [PubMed] [Google Scholar]
- Henderson DC. Weight gain with atypical antipsychotics: evidence and insights. Journal of Clinical Psychiatry. 2007;28(suppl 12):18–26. [PubMed] [Google Scholar]
- Hogdon RE, Reimer D. Some muscular strength and endurance scores of psychiatric patients. Journal of the Association for Physical and Mental Rehabilitation. 1960;14:38–44. [Google Scholar]
- Jin H, Meyer JM, Jeste DV. Atypical antipsychotics and glucose dysregulation: a systematic review. Schizophrenia Research. 2004;71(2–3):195–212. doi: 10.1016/j.schres.2004.03.024. [DOI] [PubMed] [Google Scholar]
- Kikkert MJ, Schene AH, Koeter MW, Robson D, Born A, Helm H, Nose M, Goss C, Thornicroft G, Gray RJ. Medication adherence in schizophrenia: Exploring patients' carers' and professionals' views. Schizophrenia Bulletin. 2006;32(4):786–794. doi: 10.1093/schbul/sbl011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon JS, Choi JS, Bahk WM, Kim CY, Kim CH, Shin YC, Park BJ, Oh CG. Weight management program for treatment-emergent weight gain in Olanzapine–treated patients with schizophrenia or schizoaffective disorder: A 12-week randomized controlled clinical trial. Journal of Clinical Psychiatry. 2006;67(4):547–553. doi: 10.4088/jcp.v67n0405. [DOI] [PubMed] [Google Scholar]
- Lindquist JE. Activity and vestibular function in chronic schizophrenics. Occupational Therapy Journal of Research. 1981;1:56–78. [Google Scholar]
- Menza M, Vreeland B, Minsky S, Gara M, Radler DR, Sakowitz M. Managing atypical antipsychotic-associated weight gain: 12-month data on a multimodal weight control program. Journal of Clinical Psychiatry. 2004;65(4):471–477. [PubMed] [Google Scholar]
- Morgan WP. Exercise and mental disorders. In: Ryan AJ, Allman JP Jr., editors. Sports Medicine. Academic Press; London: 1974. [Google Scholar]
- Newcomer JW. Abnormalities of glucose metabolism associated with atypical antipsychotic drugs. Journal of Clinical Psychiatry. 2004;65(Suppl. 18):36–46. [PubMed] [Google Scholar]
- Pelham TW, Campagna PD, Ritvo PG, Birnie WA. The effects of exercise therapy on clients in a psychiatric rehabilitation program. Psychosocial Rehabilitation Journal. 1993;16:75–84. [Google Scholar]
- Pendlebury J, Haddad P, Dursun S. Evaluation of a behavioral weight management programme for patients with severe mental illness: 3 year results. Human Psychopharmacology. 2005;20:447–448. doi: 10.1002/hup.707. [DOI] [PubMed] [Google Scholar]
- Vreeland B, Minsk S, Menza M, Rigussio-Radler D, Roemheld-Hamm B, Stern R. A program for managing weight gain associated with atypical antipsychotics. Psychiatric Services. 2003;54(8):1155–1157. doi: 10.1176/appi.ps.54.8.1155. [DOI] [PubMed] [Google Scholar]
- Yalom ID. The theory and practice of group psychotherapy. Basic Books; New York: 2005. [Google Scholar]