Abstract
We sought to determine the sex- and age-specific risk of mortality associated with scores on the 3-item Alcohol Use Disorder Identification Test–Consumption (AUDIT-C) questionnaire using data from a national sample of Veterans Health Administration (VHA) patients. Men (N = 215,924) and women (N = 9168) who completed the AUDIT-C in a patient survey were followed for 24 months. AUDIT-C categories (0, 1–4, 5–8, 9–12) were evaluated as predictors of mortality in logistic regression models, adjusted for age, race, education, marital status, smoking, depression, and comorbidities. For women, AUDIT-C scores of 9–12 were associated with a significantly increased risk of death compared to the AUDIT-C 1-4 group (odds ratio [OR] 7.09; 95% confidence interval [CI] = 2.67, 18.82). For men overall, AUDIT-C scores of 5–8 and 9–12 were associated with increased risk of death compared to the AUDIT-C 1-4 group (OR 1.13, 95% CI = 1.05, 1.21, and OR 1.63, 95% CI = 1.45, 1.84, respectively) but these associations varied by age. These results provide sex- and age-tailored risk information that clinicians can use in evidence-based conversations with patients about the health-related risks of their alcohol consumption. This study adds to the growing literature establishing the AUDIT-C as a scaled marker of alcohol-related risk or “vital sign” that might facilitate the detection and management of alcohol-related risks and problems. (Population Health Management 2010;13:263–268)
Introduction
Despite extensive epidemiological evidence linking alcohol consumption to health and disease,1–4 far fewer studies have evaluated whether validated alcohol screening questionnaires employed in clinical practice can be used to assess patients' levels of risk for adverse medical outcomes.5–12 The ability to judge a patient's risk of adverse outcomes from a brief alcohol misuse screening instrument allows clinicians to provide timely and individually tailored feedback about the potential medical consequences of the patient's drinking. This feedback and advice to reduce drinking are critical components of empirically supported brief alcohol counseling.13 A screening instrument that provides patient-specific risk information might act as an alcohol-related “vital sign” that could be used not only to identify patients at elevated risk for alcohol-related problems, but also possibly to guide the selection of interventions and track responses to treatment.14
The Alcohol Use Disorders Identification Test–Consumption (AUDIT-C) is a brief screen for alcohol misuse designed and validated for use in primary care settings.15–19 For men, recent evidence links AUDIT-C scores to subsequent medical problems that are the consequence of both chronic alcohol use (eg, liver disease, upper GI bleeding, pancreatitis) and acute alcohol use (eg, traumatic injury), as well as to mortality.5–10 However, the association between AUDIT-C scores and health problems in women is unknown. Also, previous research with male samples has found that the link between AUDIT-C scores and medical outcomes may vary substantially by age,5–7 but the relatively small sample sizes in studies to date have permitted evaluation of only 3 broad age groups (<50, 50–64, >65).
Therefore, the aim of this study is to determine the sex- and age-specific risks of 2-year mortality associated with AUDIT-C scores using data from a national sample of patients from the Veterans Health Administration (VHA). Such sex- and age-tailored risk information, currently unavailable, might persuade clinicians that alcohol misuse and alcohol misuse screening scores are medically relevant, provide an evidence base for recommendations to patients about the potential health-related risks of their alcohol consumption, and facilitate improved management of a broad spectrum of alcohol misuse associated with drinking above recommended limits.
Methods
Data sources and key variables
The VHA's population-based Survey of Health Experiences of Patients (SHEP) was designed to collect data on patients' satisfaction, functional status, and health behaviors. All patients who received ambulatory care in 2004 and 2005 and who had not been selected for participation in a previous SHEP survey in the past 12 months were eligible. A survey was mailed to selected patients in the month after an outpatient visit.
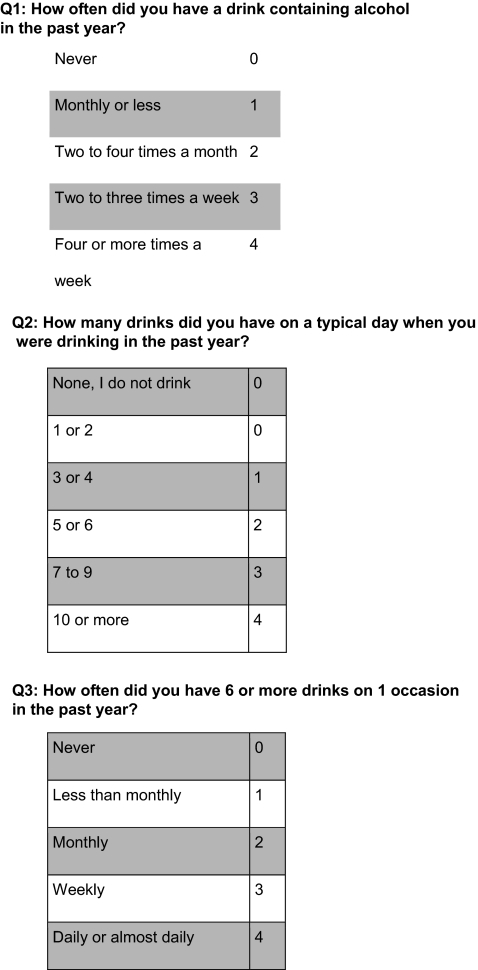
The AUDIT-C, the main predictor variable for this study, was included in the SHEP in 2004 and 2005. The 3 AUDIT-C questions ask about the frequency of drinking, typical quantity of drinking, and the frequency of drinking 6 or more drinks on an occasion in the past year (Fig. 1). Each AUDIT-C response is scored 0 to 4, with total AUDIT-C scores ranging from 0 to 12 points.16 Patients who have AUDIT-C scores of 0 are past year nondrinkers; patients who have AUDIT-C scores of 1–4 reported generally low-level drinking; patients who have AUDIT-C scores of 5–8 screen positive for mild-to-moderate alcohol misuse (having 3 or more drinks most days or 6 or more drinks on some days in the past year); and patients who have AUDIT-C scores of 9 + report severe alcohol misuse (having 5 or more drinks most days). The AUDIT-C has been validated as a brief alcohol screening questionnaire for the spectrum of alcohol misuse including risky drinking and active alcohol use disorders.15
FIG. 1.
AUDIT-C items and scoring.
The SHEP also included questions about race (African American, Hispanic, white, other), education (less than high school, high school graduate, college graduate), marital status (no/yes), past year depression, and cigarette smoking (current, past year, 1–5 years ago, over 5 years ago, or never). Data on patients' age at the time of the survey and comorbidities were obtained from the VHA National Patient Care Databases (NPCD). The Deyo Comorbidity Index, adapted from the Charlson Index for use with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) administrative data, was constructed from the NPCD based on patients' past-year inpatient and outpatient ICD-9-CM diagnostic codes.20 Fact of death (no/yes) was defined as the occurrence of death within 2 years of the survey return date as determined by the VHA Vital Status File, which merges death data from several sources (ie, Beneficiary Identification Records Locator Subsystem Death File, the Social Security Administration Death Master File, the Medicare Vital Status File, and the VHA Medical SAS Inpatient Datasets) and has been shown to have a high correspondence to death ascertainment with the National Death File.21
Analysis Strategy
Based on the fact that low-level drinkers are known to have lower mortality risk than nondrinkers,4,22,23 we categorized AUDIT-C scores into 4 risk groups (0, 1–4, 5–8, and 9–12) with 1–4 as the reference group. The initial analyses described the study sample, evaluated associations between each covariate and AUDIT-C group with chi-square tests, and calculated the unadjusted prevalence of 2-year mortality for each AUDIT-C group. Then, covariate-adjusted logistic regression models were used to assess the odds of death based on AUDIT-C risk group. A priori interaction effects (AUDIT-C group by sex and age) were evaluated. Where significant interaction effects were found, subsequent analyses were stratified for ease of interpretation.
Results
Sample characteristics and bivariate associations with the AUDIT-C risk group
Overall, 391,111 unique outpatients were selected for the survey in 2004 and 2005 combined and 270,710 responded (69.2%). From the sample of responders, 225,092 provided usable AUDIT-C data; of these 44.9% had an AUDIT-C score of 0, 42.2% had an AUDIT-C score of 1–4, 10.2% had an AUDIT-C score of 5–8, and 2.7% had an AUDIT-C score of 9–12.
Characteristics of the VHA patients who completed the AUDIT-C are presented in Table 1. Females were more highly represented in the AUDIT-C 0 and 1–4 groups (4.3% and 4.5% respectively) compared to the AUDIT-C 5–8 and 9–12 groups (1.8% and 1.6%, respectively; P < 0.001). Patients in the AUDIT-C 0 and 1–4 groups were more likely to be older than patients in the AUDIT-C 5–8 and 9–12 groups (P < 0.001). White patients were most highly represented in the AUDIT-C 1–4 group (88.0%) and least represented in the AUDIT-C 9–12 group (79.2%; P < 0.0001). In contrast, African American patients and Hispanic patients were most highly represented in the AUDIT-C 9–12 group (8.6% and 8.3%, respectively) and least represented in the AUDIT-C 1–4 group (5.3% and 3.9%, respectively; both P's < 0.0001).
Table 1.
Characteristics of VHA Outpatients in Study Sample (N = 225,092) by AUDIT-C Scores
| |
|
AUDIT-C |
AUDIT-C |
AUDIT-C |
AUDIT-C |
|
|---|---|---|---|---|---|---|
| Total Sample (225,092) | 0 (101,109) | 1–4 (95,001) | 5–8 (22,973) | 9–12 (6009) | P value | |
| N(%) | N (%) | N (%) | N (%) | N (%) | ||
| Demographics | ||||||
| Female | 9168 (4.1) | 4393 (4.3) | 4268(4.5) | 409 (1.8) | 98 (1.6) | <0.001 |
| Age <30 | 1162 (0.5) | 239 (0.2) | 651 (0.7) | 218 (0.9) | 54 (0.9) | |
| 30–39 | 3107 (1.4) | 923 (0.9) | 1610 (1.7) | 452 (2.0) | 122 (2.0) | |
| 40–49 | 11681 (5.2) | 4518 (4.5) | 4887 (5.1) | 1671 (7.3) | 605 (10.1) | |
| 50–59 | 47241 (21.0) | 19880 (19.7) | 17760 (18.7) | 6993 (30.4) | 2608 (43.4) | |
| 60–69 | 53028 (23.6) | 22880 (22.6) | 22020 (23.2) | 6553 (28.5) | 1575 (26.2) | |
| 70–79 | 72771 (32.3) | 33930 (33.6) | 32280 (34.0) | 5685 (24.8) | 876 (14.6) | |
| >80 | 36009 (16.0) | 18700 (18.5) | 15750 (16.6) | 1394 (6.1) | 165 (2.8) | <0.001 |
| White | 189007 (85.8) | 83390 (84.7) | 82130 (88.0) | 18800 (83.0) | 4687 (79.2) | <0.001 |
| African American | 14168 (6.4) | 6966 (7.0) | 4952 (5.3) | 1744 (7.7) | 506 (8.6) | |
| Hispanic | 9905 (4.5) | 4404 (4.4) | 3639 (3.9) | 1372 (6.1) | 490 (8.3) | |
| Education | ||||||
| Less than 12th | 40227 (18.2) | 24050 (24.3) | 12140 (13.0) | 3109 (13.7) | 928 (15.7) | |
| HS graduate | 140823 (63.7) | 61710 (62.4) | 59330 (63.5) | 15520 (68.4) | 4263 (72.1) | |
| College Grad | 39900 (18.1) | 13120 (13.3) | 22010 (23.5) | 4047 (17.8) | 723 (12.2) | <0.001 |
| Married | 148846 (66.1) | 67540 (66.8) | 65520 (69.0) | 13070 (56.9) | 2716 (45.2) | <0.001 |
| Health behaviors | ||||||
| Last Regular Smoking | ||||||
| Never | 61271 (27.2) | 29450 (29.1) | 25700 (27.0) | 4876 (21.2) | 1245 (20.7) | |
| Past year | 11450 (5.1) | 4671 (4.6) | 4416 (4.7) | 1805 (7.9) | 558 (9.3) | |
| 1–5 years ago | 10745 (4.8) | 5021 (5.0) | 4163 (4.4) | 1235 (5.4) | 326 (5.4) | |
| Over 5 years ago | 113772 (50.5) | 50790 (50.2) | 50830 (53.4) | 10260 (44.7) | 1892 (31.5) | |
| Current | 27846 (12.4) | 11170 (11.1) | 9894 (10.4) | 4794 (20.9) | 1988 (33.1) | <0.001 |
| Medical conditions | ||||||
| Past year Depression | 74041 (32.9) | 36140 (35.7) | 26470 (27.9) | 8267 (36.0) | 3164 (52.7) | <0.001 |
| Deyo Comorbidity Score Mean (SD) | 1.01 (1.34) | 1.20 (1.44) | 0.89 (1.25) | 0.73 (1.12) | 0.72 (1.11) | <0.001 |
HS = High school graduate.
Education was also significantly associated with AUDIT-C group (P < 0.001). Patients with less than 12 years of education constituted a greater proportion of the nondrinkers (24.3%), whereas patients who had graduated from college were more highly represented in the AUDIT-C 1–4 and 5–8 groups (23.5% and 17.8%, respectively) compared to the AUDIT-C 0 and 9–12 groups (13.3% and 12.2%, respectively). The proportion of married patients was highest in the AUDIT-C 1–4 group (69.0%) and lowest in the AUDIT-C 9–12 group (45.2%; P < 0.0001).
Period of last regular smoking was also significantly associated with AUDIT-C group (P < 0.001). Current smokers were most highly represented in the AUDIT-C 9–12 group (33.1%) compared to other groups, and lifetime nonsmokers were most highly represented in the nondrinking group (29.1%). With respect to depression in the past year, depressed patients were most highly represented in the AUDIT-C 9–12 group (52.7%) and least represented in the AUDIT-C 1–4 group (27.9%). Average Deyo comorbidity scores were highest in the AUDIT-C 0 group (mean = 1.20) and the lowest in the AUDIT-C 9–12 group (mean = 0.72).
Association between AUDIT-C risk group and mortality in females
In a covariate-adjusted logistic regression model that predicted death in the 2-year follow-up period, a significant interaction between sex and AUDIT-C group was found. Therefore, we stratified the sample by sex and conducted separate analyses for males and females. In the sample of 9168 female patients, the interaction between age and AUDIT-C group was not significant and therefore was dropped from subsequent analyses (although age was retained as a control variable).
Table 2 presents the results of the logistic regression analysis examining the association between 2-year mortality and AUDIT-C risk group for women, with the AUDIT-C 1-4 (2-year death rate = 0.01998) as the reference, controlling for age, race, education, marital status, past year depression, and Deyo comorbidity index scores. Women in the AUDIT-C 0 group (odds ratio [OR] 1.34; 95% confidence interval [CI] = 1.01–1.78), and those in the AUDIT-C 9–12 group (OR 7.09; 95% CI = 2.67–18.82), had a significantly increased mortality risk. The latter figure represents a 6-fold increase in odds of death compared to women in the AUDIT-C 1–4 group. No significant increase in mortality risk was observed among women in the AUDIT-C 5–8 group.
Table 2.
Association between AUDIT-C Score and Mortality†
| |
AUDIT-C |
AUDIT-C |
AUDIT-C |
AUDIT-C |
|---|---|---|---|---|
| |
0 |
1–4 |
5–8 |
9–12 |
| HR (95% CI) | 2-Year Death Rate | HR (95% CI) | HR (95% CI) | |
| Female Sample | 1.34 (1.01, 1.78) | 0.01998 | 0.89 (0.35, 2.24) | 7.09 (2.67, 18.82) |
| Male Total Sample | 1.34 (1.29, 1.39) | 0.05222 | 1.13 (1.05, 1.21) | 1.63 (1.45, 1.84) |
| 18–39 years old | 0.73 (0.21, 2.49) | 0.00522 | 0.33 (0.04, 2.67) | 1.03 (0.13, 8.45) |
| 40–49 years old | 1.34 (0.93, 1.93) | 0.01308 | 1.19 (0.74, 1.92) | 1.12 (0.56, 2.24) |
| 50–59 years old | 1.41 (1.22, 1.63) | 0.01883 | 1.35 (1.12, 1.63) | 2.00 (1.59, 2.52) |
| 60–69 years old | 1.31 (1.18, 1.45) | 0.03140 | 1.22 (1.05, 1.42) | 1.77 (1.41, 2.23) |
| 70–79 years old | 1.34 (1.26, 1.43) | 0.06004 | 1.09 (0.97, 1.23) | 1.60 (1.26, 2.02) |
| >80 years old | 1.36 (1.27, 1.45) | 0.11660 | 1.10 (0.93, 1.32) | 1.54 (1.27, 1.45) |
All models include age, race, education, marital status, smoking status, comorbidity index, and previous year depression. CI, confidence interval; HR, hazard ratio.
Association between AUDIT-C risk group and mortality in males
In the sample of 215,924 male patients, there was a significant interaction between age group and AUDIT-C group in the prediction of 2-year mortality. Therefore, we stratified the male sample by the 6 age categories and conducted analyses separately for each (Table 2). In the age 18–39 and 40–49 groups, AUDIT-C group was not associated with 2-year mortality risk. In the age 50–59 group, compared to the AUDIT-C 1–4 group, the AUDIT-C 0 group had significantly increased odds of death (OR 1.41; 95% CI = 1.22–1.63), as did the AUDIT-C 5–8 group (OR 1.35; 95% CI = 1.12–1.63) and the AUDIT-C 9–12 group (OR 2.00; 95% CI = 1.59–2.52). In the age 60–69 group, compared to the AUDIT-C 1–4 group, the AUDIT-C 0 group had significantly increased odds of death (OR 1.31; 95% CI = 1.18–1.45), as did the AUDIT-C 5–8 group (OR 1.22; 95% CI = 1.05–1.42) and the AUDIT-C 9–12 group (OR 1.77; 95% CI = 1.41–2.23).
In the age 70–79 group, compared to the AUDIT-C 1–4 group, the AUDIT-C 0 group had significantly increased odds of death (OR 1.34; 95% CI = 1.26–1.43), as did the AUDIT-C 9–12 group (OR 1.60; 95% CI = 1.26–2.02). In patients 80 years old or older, compared to the AUDIT-C 1–4 group, the AUDIT-C 0 group had significantly increased odds of death (OR 1.36; 95% CI = 1.27–1.45), as did the AUDIT-C 9–12 group (OR 1.54; 95% CI = 1.27–1.45). In these oldest 2 age groups, the AUDIT-C 5–8 group did not differ significantly from the AUDIT-C 1–4 group in terms of 2-year mortality.
Discussion
These results significantly extend prior research that has evaluated whether validated alcohol screening questionnaires employed in clinical practice can be used to assess patients' level of risk for adverse health outcomes, in particular mortality. As in a recent study of a smaller sample of male VHA patients,5 we found that male nondrinkers (AUDIT-C 0) older than 50 years of age have an increased risk of death compared to low-level drinkers (AUDIT-C 1–4). This apparently robust result is consistent with the broader literature linking alcohol consumption to mortality risk4,22 and has several possible explanations. First, patients with a greater number of medical comorbidities are more likely to be nondrinkers (Table 1) and this is probably more pronounced in older cohorts. People often stop drinking when they get sick or become more frail. Some current nondrinkers might be former problem drinkers and, therefore, part of the higher death rate among abstainers might be a result of individuals who incurred alcohol-related harm from their former heavy drinking.24
Furthermore, low-level drinking, such as reported by the AUDIT-C 1–4 group, has been associated with cardiovascular protective effects,24–26 suggesting another explanation for the elevated mortality risk among abstainers. Younger patients have lower cardiovascular risk, so the potential cardiovascular benefits of alcohol use might not be apparent in these patients. Younger patients also may be less likely to abstain due to chronic diseases and may abstain for other reasons, perhaps including religious proscriptions against drinking, that may be associated with other protective factors (eg, social support, religious service attendance).27,28 In the female sample, nondrinkers (AUDIT-C 0) had increased risk of death compared to low-level drinkers (AUDIT-C 1–4), with an identical OR (1.34) as that observed in the non-age-stratified male estimate.
The high level of drinking in the AUDIT-C 9–12 group was associated with a 7-fold increase in mortality risk for women; however, there is a large CI around this estimate (2.67, 18.82). Although we cannot be certain why heavy drinking appears to be more risky for females than males, a previous study also found that females with a positive CAGE score at mean age 43 had a higher risk of death than males during the 21 years of the study.12 These findings might be explained, in part, by several factors, including that the overall smaller physical stature and lower total body water of females causes them to achieve higher blood alcohol content, and thereby more negative consequences, with the same level of consumption as males.29–32
For men, the risk of mortality associated with the AUDIT-C 9–12 group varied by age, from nonsignificance in the age 18 to 49 range to a 2-fold increased odds of death in the age 50–59 group, and then remaining significant but declining in magnitude for men in the older age groups. This result differs somewhat from a previous study that found increased mortality risk in men younger than age 50, but the previous population included patients actively engaged in primary care who might have had greater medical comorbidity.5 However, the general decrease of risk with age associated with heavy drinking was confirmed and may reflect a “survivor bias”—that is, that heavy drinkers who are susceptible to alcohol-related harms either get sick and reduce their drinking or die before reaching these older age categories.
These results need to be understood in light of several limitations. Incomplete or differential ascertainment of death could have biased study results. For example, deaths among patients in the higher AUDIT-C categories may be less likely to be recorded because of homelessness, biasing results toward the null. However, rates of ascertainment are expected to be high for this sample of patients because all were actively engaged in VHA outpatient care. Although we have no reason to suspect it, it is possible that the relationship between AUDIT-C scores and mortality could be different in the SHEP nonresponders (30%). In addition, the AUDIT-C assesses drinking in the past year but provides no data regarding previous alcohol misuse to differentiate lifetime abstainers from previous high-risk or problem drinkers. In addition, VHA data sources used to assess vital status do not include any information on cause of death. Although we did not find an interaction effect with age in the female sample, this may have been related to the relatively small number of women and deaths in our data. Furthermore, AUDIT-C data collected in the course of a mailed survey on patient satisfaction may differ in important ways from screening data collected in the course of clinical care.
Nevertheless, this study provides important new information about sex- and age-specific risks of mortality attributable to AUDIT-C scores using data from a national sample of patients from the VHA. This study adds to the growing literature establishing the AUDIT-C as a scaled marker of alcohol-related risk or “vital sign”33 that can facilitate the improved management of alcohol misuse as well as the management of medical conditions associated with excessive alcohol consumption. Recent research has linked AUDIT-C scores to a host of subsequent medical outcomes including gastrointestinal problems, fractures, medication nonadherence, and surgical complications.6,8,10 Health care systems, such as VHA, that adopt a program of annual alcohol misuse screening with the AUDIT-C can use these data to inform clinicians about alcohol-related risks, educate patients about the potential health-related risks of their alcohol consumption, and potentially to guide the intensity of intervention efforts.
Author Disclosure Statement
Drs. Harris, Bradley, Bowe, and Moos, and Ms. Henderson disclosed no financial conflicts of interest.
This work was made possible through a grant from the National Institute of Alcohol and Alcoholism (R03 AA016793-01) and support from the VA Office of Quality and Performance. The views presented in this paper do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Di Castelnuovo A. Costanzo S. Bagnardi V. Donati MB. Iacoviello L. de Gaetano G. Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006;166:2437–2445. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- 2.Moore AA. Giuli L. Gould R, et al. Alcohol use, comorbidity, and mortality. J Am Geriatr Soc. 2006;54:757–762. doi: 10.1111/j.1532-5415.2006.00728.x. [DOI] [PubMed] [Google Scholar]
- 3.Klatsky AL. Armstrong MA. Friedman GD. Alcohol and mortality. Ann Intern Med. 1992;117:646–654. doi: 10.7326/0003-4819-117-8-646. [DOI] [PubMed] [Google Scholar]
- 4.Dawson D. Alcohol consumption, alcohol dependence, and all-cause mortality. Alcohol Clin Exp Res. 2000;24:72–81. [PubMed] [Google Scholar]
- 5.Kinder LS. Bryson CL. Sun H. Williams EC. Bradley KA. Alcohol screening scores and all-cause mortality in male Veterans Affairs patients. J Stud Alcohol Drugs. 2009;70:253–260. doi: 10.15288/jsad.2009.70.253. [DOI] [PubMed] [Google Scholar]
- 6.Au DH. Kivlahan DR. Bryson CL. Blough D. Bradley KA. Alcohol screening scores and risk of hospitalizations for GI conditions in men. Alcohol Clin Exp Res. 2007;31:443–451. doi: 10.1111/j.1530-0277.2006.00325.x. [DOI] [PubMed] [Google Scholar]
- 7.Bradley KA. Maynard C. Kivlahan DR. McDonell MB. Fihn SD. The relationship between alcohol screening questionnaires and mortality among male veteran outpatients. J Stud Alcohol. 2001;62:826–833. doi: 10.15288/jsa.2001.62.826. [DOI] [PubMed] [Google Scholar]
- 8.Harris AH. Bryson CL. Sun H. Blough D. Bradley KA. Alcohol screening scores predict risk of subsequent fractures. Subst Use Misuse. 2009;44:1055–1069. doi: 10.1080/10826080802485972. [DOI] [PubMed] [Google Scholar]
- 9.Greene CC. Bradley KA. Bryson CL, et al. The association between alcohol consumption and risk of COPD exacerbation in a veteran population. Chest. 2008;134:761–767. doi: 10.1378/chest.07-3081. [DOI] [PubMed] [Google Scholar]
- 10.Bryson CL. Au DH. Sun H. Williams EC. Kivlahan DR. Bradley KA. Alcohol screening scores and medication nonadherence. Ann Intern Med. 2008;149:795–804. doi: 10.7326/0003-4819-149-11-200812020-00004. [DOI] [PubMed] [Google Scholar]
- 11.Conigrave KM. Saunders JB. Reznik RB. Predictive capacity of the AUDIT questionnaire for alcohol-related harm. Addiction. 1995;90:1479–1485. doi: 10.1046/j.1360-0443.1995.901114796.x. [DOI] [PubMed] [Google Scholar]
- 12.Batty GD. Hunt K. Emslie C. Lewars H. Gale CR. Alcohol problems and all-cause mortality in men and women: Predictive capacity of a clinical screening tool in a 21-year follow-up of a large, UK-wide, general population-based survey. J Psychosom Res. 2009;66:317–321. doi: 10.1016/j.jpsychores.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 13.Moyer A. Finney J. Swearingen C. Vergun P. Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine. Improving the Quality of Health Care for Mental and Substance-Use Conditions. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 15.Bradley KA. Bush KR. Epler AJ, et al. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163:821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- 16.Bush K. Kivlahan DR. McDonell MB. Fihn SD. Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 17.Rumpf HJ. Hapke U. Meyer C. John U. Screening for alcohol use disorders and at-risk drinking in the general population: Psychometric performance of three questionnaires. Alcohol Alcohol. 2002;37:261–268. doi: 10.1093/alcalc/37.3.261. [DOI] [PubMed] [Google Scholar]
- 18.Aertgeerts B. Buntinx F. Ansoms S. Fevery J. Screening properties of questionnaires and laboratory tests for the detection of alcohol abuse or dependence in a general practice population. Br J Gen Pract. 2001;51:206–217. [PMC free article] [PubMed] [Google Scholar]
- 19.Dawson DA. Grant BF. Stinson FS. Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res. 2005;29:844–854. doi: 10.1097/01.alc.0000164374.32229.a2. [DOI] [PubMed] [Google Scholar]
- 20.Deyo RA. Cherkin DC. Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 21.Arnold N. Sohn M. Maynard C. Hynes DM. VIReC Technical Report 2: VA-NDI Mortality Data Merge Project. Hines, IL: VA Information Resource Center; 2006. [Google Scholar]
- 22.Klatsky A. Friedman G. Siegelaub A. Alcohol and mortality: A ten year Kaiser Permanente experience. Ann Intern Med. 1981;95:139–145. doi: 10.7326/0003-4819-95-2-139. [DOI] [PubMed] [Google Scholar]
- 23.Marmot M. Shipley M. Rose G. Thomas B. Alcohol and mortality: A U-shaped curve. Lancet. 1981;1:580–583. doi: 10.1016/s0140-6736(81)92032-8. [DOI] [PubMed] [Google Scholar]
- 24.Klatsky A. Armstrong M. Friedman G. Risk of cardiovascular mortality in alcohol drinkers, ex-drinkers and nondrinkers. Am J Cardiol. 1990;66:1237–1242. doi: 10.1016/0002-9149(90)91107-h. [DOI] [PubMed] [Google Scholar]
- 25.Albert CM. Manson JE. Cook NR. Ajani UA. Gaziano JM. Hennekens CH. Moderate alcohol consumption and the risk of sudden cardiac death among US male physicians. Circulation. 1999;100:944–950. doi: 10.1161/01.cir.100.9.944. [DOI] [PubMed] [Google Scholar]
- 26.Li JM. Mukamal KJ. An update on alcohol and atherosclerosis. Curr Opin Lipidol. 2004;15:673–680. doi: 10.1097/00041433-200412000-00008. [DOI] [PubMed] [Google Scholar]
- 27.McCullough ME. Hoyt WT. Larson DB. Koenig HG. Thoresen C. Religious involvement and mortality: A meta-analytic review. Health Psychol. 2000;19:211–222. doi: 10.1037//0278-6133.19.3.211. [DOI] [PubMed] [Google Scholar]
- 28.Strawbridge WJ. Shema SJ. Cohen RD. Kaplan GA. Religious attendance increases survival by improving and maintaining good health behaviors mental health and social relationships. Ann Behav Med. 2001;23:68–74. doi: 10.1207/s15324796abm2301_10. [DOI] [PubMed] [Google Scholar]
- 29.Sugarman DE. Demartini KS. Carey KB. Are women at greater risk? An examination of alcohol-related consequences and gender. Am J Addict. 2009;18:194–197. doi: 10.1080/10550490902786991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davies BT. Bowen CK. Total body water and peak alcohol concentration: A comparative study of young, middle-age, and older females. Alcohol Clin Exp Res. 1999;23:969–975. [PubMed] [Google Scholar]
- 31.Graham K. Wilsnack R. Dawson D. Vogeltanz N. Should alcohol consumption measures be adjusted for gender differences? Addiction. 1998;93:1137–1147. doi: 10.1046/j.1360-0443.1998.93811372.x. [DOI] [PubMed] [Google Scholar]
- 32.Bradley KA. Badrinath S. Bush K. Boyd–Wickizer J. Anawalt B. Medical risks for women who drink alcohol. J Gen Intern Med. 1998;13:627–639. doi: 10.1046/j.1525-1497.1998.cr187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Institute of Medicine. Improving the Quality of Mental Health Care for Mental and Substance-Use Conditions. Washington DC: The National Academies Press; 2006. [Google Scholar]