Abstract
Background & objectives:
Vibration perception threshold (VPT) is considered as a gold standard for diagnosis of diabetic peripheral neuropathy. However, the data are sparse comparing the VPT with commonly used bedside modalities. This study was carried out to evaluate the usefulness of simple bed side screening modalities for peripheral neuropathy in patients with diabetes mellitus.
Methods:
A total of 1044 patients with diabetes mellitus attending the Diabetes clinic from January 2007 to May 2008, were included in this study. All subjects had a detailed clinical assessment including Diabetic Neuropathy Symptom (DNS) score, Diabetic Neuropathy Examination (DNE) score, ankle reflex, vibration sensation with a 128 Hz tuning fork, 10g Semmes-Weinstein monofilament and vibration perception threshold (VPT).
Results:
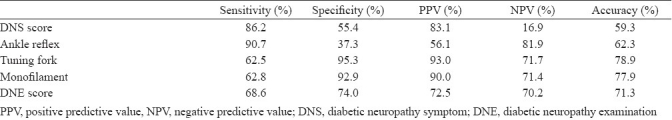
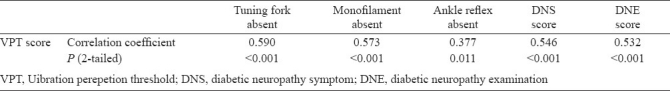
The prevalence of peripheral neuropathy was 34.9 per cent with VPT. Foot care practices were followed by only 214 (20.5%) of the study population. When compared with VPT, ankle reflex was the most sensitive (90.7%) but least specific (37.3%). The tuning fork and monofilament tests respectively had lower sensitivity (62.5 and 62.8%) but better specificity (95.3 and 92.9%) and accuracy (78.9 and 77.9%). Significant correlations were observed between the VPT score and the DNE (r = 0.532, P<0.001) and DNS (r = 0.546, P<0.001) scores and absent tuning fork sensation (r= 0.590; P<0.001), monofilament sensation (r= 0.573; P<0.001) and ankle reflex (r = 0.377, P= 0.01).
Interpretation & conclusions:
The present findings show that simple bed side tests are useful for assessing peripheral diabetic neuropathy, even in those subjects in whom foot care practices are not followed.
Keywords: Ankle reflex, monofilament, neuropathy, tuning fork, VPT
The number of patients with diabetes mellitus is increasing by epidemic proportions in the world, particularly in India. Lower extremity disease, including peripheral neuropathy, foot ulceration, peripheral arterial disease, or lower extremity amputation, is twice as common in diabetic persons compared with non diabetic persons and it affects 30 per cent of diabetic persons who are older than 40 yr1. In persons with diabetes mellitus, the annual population-based incidence of foot ulcer ranges from 1.0 to 4.1 per cent and the prevalence ranges from 4 to 10 per cent, which suggests that the lifetime incidence may be as high as 25 per cent1.
Screening and early identification of neuropathy offer a crucial opportunity for the patient with diabetes to actively modulate the course of suboptimal glycaemic control to currently recommended targets, and to implement improved foot care before the onset of significant morbidity. Clinical trial evidence for the efficacy of screening strategies have demonstrated reduced incidence of amputation and ulceration and screening for neuropathy is recommended in clinical practice guidelines2. Most of the available modalities have been evaluated in developed countries where foot care practices are widely followed. Contrary to it, in developing countries barefoot walking is still prevalent and foot care practices are hardly followed3, which can result in alteration in cutaneous morphology. This may influence the outcome of commonly used tools to identify neuropathy like the Diabetic Neuropathy Symptom (DNS) Score, 10-g Semmes-Weinstein monofilament, vibration testing by 128 Hz tuning fork, ankle reflex and the Diabetic Neuropathy Examination (DNE) score. Therefore, this study was planned to evaluate the usefulness of the above modalities with the standard well validated screening method of measuring vibration perception threshold (VPT) with a biothesiometer in a population where foot care practices are scantly followed.
Material & Methods
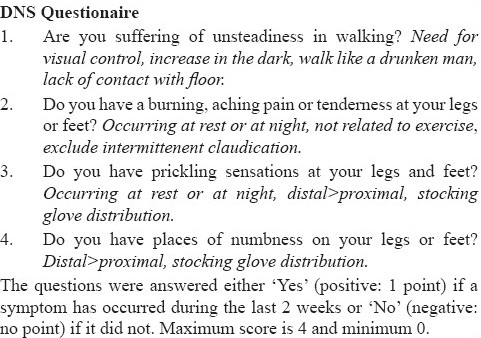
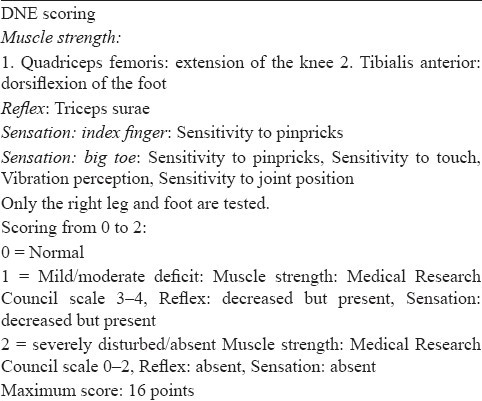
The study was conducted in the Diabetes Clinic of Postgraduate Institute of Medical Education and Research (PGIMER), a tertiary care hospital in Chandigarh, north India, from January 2007 to May 2008. Patients with diabetes mellitus according to the American Diabetes Association (ADA) criteria2 and who had at least two visits in the last six months were included consecutively into the study. Institutional ethics committee approved the study protocol. An informed written consent was obtained from the study participants. Detailed history regarding the type, duration and treatment of diabetes was recorded. History regarding foot care was taken - whether using footwear or not, the type of footwear(s) used and whether foot care practices were followed daily or not, were assessed by a questionnaire. Symptoms of diabetic neuropathy were scored with the Diabetic Neuropathy Symptom (DNS) score4 and a score ≥ 1 was considered significant (Annexure I). Vibration perception threshold (VPT) was measured with a biothesiometer – Vibrometer-VPT® (Diabetic Foot Care, Madras Engineering Service, India) in a standardized fashion by a single observer. The biothesiometer probe, which vibrates at an amplitude proportional to the square of the applied voltage, was applied perpendicular to the test site with a constant and firm pressure. Subjects were initially familiarized with the sensation by holding the probe against the distal palmar surface of hand. VPT was then measured at the distal plantar surface of great toe of both the legs. If great toe was affected by ulcer, VPT was measured at the base of the first, third or fifth metatarsals. The voltage was slowly increased at the rate of 1 mV/sec and the VPT value was defined as the voltage level when the subject indicated that he or she first felt the vibration sense. The mean of three records was taken and neuropathy was diagnosed if the VPT was ≥ 25mV5. Evaluation for peripheral neuropathy was done using 10 g Semmes-Weinstein monofilament. The filament was placed perpendicular to the skin and pressure was applied until the filament just buckles with a contact time of 2 sec. The patient was prevented from seeing if and where the examiner applied the filament. Monofilament was applied to the plantar surface of great toe and base of first, third, and fifth metatarsals of both foot. Areas affected by ulceration or thick callus formation were omitted. The patient was asked to say whether he can feel the pressure applied (yes/no) and in which foot it was applied (right/left foot). Inability to perceive the sensation at any one site was considered abnormal. Assessment of vibration sensation was also done with a 128 Hz tuning fork applied at the distal plantar surface of big toe of both legs. The response was considered abnormal when the patient loses vibratory sensation while the examiner still perceived it. Ankle reflex was assessed with a tendon hammer and was recorded as either present or absent. The Diabetic Neuropathy Examination (DNE) score was used to quantify the neuropathy (Annexure II) and a score > 3 was considered significant for presence of neuropathy6.
Annexure I.
Annexure II.
Statistical analysis: The data were analyzed using SPSS statistical package, version 13 (Chicago, IL). Correlations were assessed with Spearman's correlation. BY constructing Receiver operating characteristic curve, sensitivity, specificity, positive and negative predictive values and accuracy were calculated for the various tests using VPT >25 mV as the gold standard definition of neuropathy. P<0.05 was considered as statistically significant.
Results
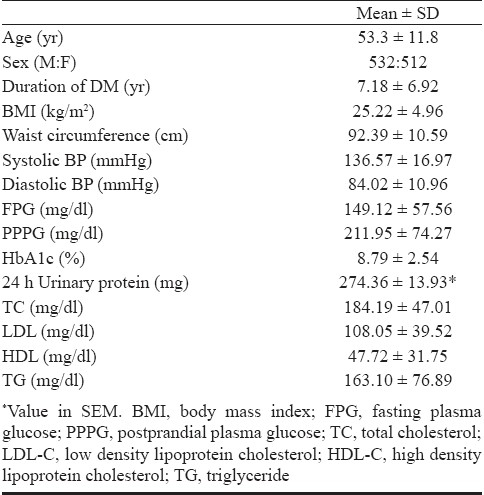
A total of 1044 patients were included. The mean age was 53.3 ± 11.8 years, (range 13 - 86 yr) with almost equal gender distribution (M:F :: 1.02:1.0). Baseline characteristics of the study group are given in Table I. Among the study group, 37 (3.5%) were having type1 diabetes mellitus and the rest had type 2 diabetes. The mean duration of diabetes mellitus was 7.18 ± 6.92 yr and 42.2 per cent were receiving insulin and/or oral antidiabetic drugs. Foot care practices were followed by only 214 (20.5%) patients of the study population. While 182 (17.4%) were self doing, in 20 (1.9%) foot care was done by a family member and only 13 (1.2%)patients of the study population had foot care done by a trained chiropodist. Twenty three (2.2%) subjects were not using any footwear outdoor while 473 (45.3%) did not use any footwear indoor. Only 242 (23.2%) patients were using closed footwear like shoes while the remaining were using open footwear, majority (64.6%) of which was sandals. On evaluating for the symptoms of neuropathy with the DNS questionnaire, 375 (35.9%) patients were having a score of zero which indicated that they did not have symptoms of neuropathy, 148 (14.2%) had a DNS score of one, 187 (17.9%) had a score of two, 267 (25.6%) had a score of three and 67 (6.4%) had the maximum score of four thus, 669 (64.1%) were having significant DNS score indicating that the vast majority of patients with diabetic neuropathy were symptomatic. In patients with a DNS score of zero, 91.1 per cent had a VPT score of < 25 mV and monofilament sensation, tuning fork sensation and ankle reflex were preserved in 895 (85.7%), 909 (87.1%) and 765 (73.3%) patients respectively.
Table 1.
Characteristics of the study population (n = 1044)
Evaluation for neuropathy with biothesiometry showed a VPT ≥ 25 mV in 364 patients, thus showing a prevalence of peripheral neuropathy of 34.9 per cent in the study population. Using other testing modalities, neuropathy was found in 321 (30.7%) patients with monofilament and in 323 (30.9%) with tuning fork. The ankle reflex was absent in 471 (45.1%) patients. The DNE score was significant (>3) in 496 (47.5%) of patients.
Table II gives the sensitivity, specificity and positive predictive value of each diagnostic modality compared with biothesiometry which is taken as the gold standard. Tuning fork test and monofilament were the most specific and accurate of all the diagnostic tests. Though the ankle reflex was most sensitive it had poor specificity and positive predictive value.
Table II.
Diagnostic accuracy of different tests compared to vibration perception threshold (VPT)
As shown in Table III, there was significant correlation between the VPT score and the DNE (r = 0.532, P<0.001) and DNS (r = 0.546, P<0.001) scores and absent tuning fork sensation (r= 0.590; P< 0.001), monofilament sensation (r= 0.573; P < 0.001) and ankle reflex (r = 0.377, P=0.01).
Table III.
Correlations between VPT score and absent tuning fork, monofilament and ankle reflex, and DNS and DNE score
Discussion
The present study has used VPT of > 25 mV as the standard for the diagnosis of neuropathy and the prevalence of peripheral neuropathy was 34.9 per cent. The use of VPT for the diagnosis of neuropathy has been well validated by clinical studies with a sensitivity and specificity of 80 and 98 per cent respectively7. This is further substantiated by large epidemiological prospective studies showing that a VPT more than 25 mV had a sensitivity of 83 per cent, a specificity of 63 per cent, a positive likelihood ratio of 2.2 (95% CI, 1.8-2.5), and a negative likelihood ratio of 0.27 (95% CI, 0.14-0.48) for predicting a foot ulceration over 4 years6.
Since peripheral sensory neuropathy is a pivotal element in the causal pathway to both foot ulceration and amputation, selecting a quick, inexpensive, and accurate instrument to evaluate the high-risk patient is essential to make decisions. So, apart from VPT, we also assessed monofilament, tuning fork, ankle reflex, the DNS and DNE scores for evaluation of peripheral neuropathy.
The most frequently used modality for detecting neuropathy in clinical practice is the nylon Semmes-Weinstein monofilament8. Inability to perceive the 10 g of force a 5.07 monofilament applies is associated with clinically significant large-fiber neuropathy. Various case control studies have reported variable sensitivity and specificity for monofilament sensation up to 95 and 82 per cent respectively9,10. However, another case-control study has shown sensitivity and specificity of 77 and 96 per cent respectively, which was attributed to lack of blinding of examiners for individual screening maneuvers7. Our study has shown sensitivity of 63 per cent and specificity of 93 per cent for monofilament sensation for the diagnosis of neuropathy which is lower as compared to the western data possibly because of lack of blinding of examiner for screening maneuver and the subjective variation in this modality. In 3 prospective studies, the Semmes-Weinstein monofilament identified persons at increased risk of foot ulceration with a sensitivity of 66 to 91 per cent, a specificity of 34 to 86 per cent, a positive predictive value of 18 to 39 per cent, and a negative predictive value of 94 to 95 per cent11–13.
The 128 Hz tuning fork provides an easy and inexpensive test of vibratory sensation. The sensitivity and specificity of vibration testing for peripheral neuropathy has been estimated to be 53 and 99 per cent, respectively1,7. The present study showed a better sensitivity (62.5%) but a lower specificity (95%) compared to the above studies. A graded tuning fork is better than a conventional tuning fork and correlates more strongly with biothesiometer results14.
Our study had also used ankle reflex for assessing peripheral neuropathy. Absent ankle reflex showed a significant correlation with VPT, though it was highly sensitive, ankle reflex had poor specificity, positive predictive value and accuracy. However, in one study sensitivity and specificity for absent ankle reflex was 75 and 89 per cent15. The disadvantage of relying purely on absent ankle reflex for peripheral neuropathy diagnosis is the high prevalence of absent ankle reflex even in normal population6. This possibly happens because of associated obesity, oedematous state, concurrent micronutrient deficiency and various drugs like beta blockers. There is age dependent increase in prevalence of absent ankle reflex, which is substantiated by a study of 1074 normal adults, in which proportion of subjects with absent ankle reflex increased rapidly from 5 per cent at 40 to 50 yr of age to 80 per cent at 90 to 100 yr of age16.
The DNS and DNE scores are simple clinical scores useful to diagnose peripheral neuropathy in patients with diabetes. As expected, the symptom score was sensitive but was not specific for making the diagnosis of neuropathy. However, a study showed a sensitivity of 79 per cent and specificity of 78 per cent for DNS score as compared to VPT4. The DNE score was significant (>3) in 47.5 per cent of patients and was well correlated with VPT score but had a low sensitivity compared to another study which showed a sensitivity of 96 per cent and specificity of 51 per cent6. However, both these scores are more subjective which may result in variability of these indices. Meijer et al17 have shown a strong relation between the DNS and DNE scores and electro-diagnostic investigations in both nerve and muscle fiber conduction studies. But the relatively time consuming DNE scoring did not give any additional specificity or accuracy in diagnosis compared to easy to use monofilament and tuning fork.
In conclusion, the good correlation between VPT score with tuning fork, monofilament and ankle reflex shows that simple bed side tests are useful in clinical practice, even in those subjects in whom foot care practices are not followed.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293:217–28. doi: 10.1001/jama.293.2.217. [DOI] [PubMed] [Google Scholar]
- 2.[No authors listed]. Executive summary: Standards of Medical Care in Diabetes-2010. Diabetes Care. 2010;33:S4–S10. doi: 10.2337/dc10-S004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Viswanathan V, Thomas N, Tandon N, Asirvatham A, Rajasekar S, Ramachandran A, et al. Profile of diabetic foot complications and its associated complications – a multicentric study from India. J Assoc Physicians India. 2005;53:933–6. [PubMed] [Google Scholar]
- 4.Meijer JWG, Smit AJ, Sonderen EV, Groothoff JW, Eisma WH, Links TP. Symptom scoring systems to diagnose distal polyneuropathy in diabetes: the Diabetic Neuropathy Symptom score. Diabet Med. 2002;19:962–5. doi: 10.1046/j.1464-5491.2002.00819.x. [DOI] [PubMed] [Google Scholar]
- 5.Young MJ, Breddy JL, Veves A, Boulton AJM. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds. A prospective study. Diabetes Care. 1994;17:557–60. doi: 10.2337/diacare.17.6.557. [DOI] [PubMed] [Google Scholar]
- 6.Meijer JW, Sonderen EV, Blaauwwiekel EE, Links TP, Groothoff JW, Eisma WH, et al. Diabetic Neuropathy Examination: a hierarchical scoring system to diagnose distal polyneuropathy in diabetes. Diabetes Care. 2000;23:750–3. doi: 10.2337/diacare.23.6.750. [DOI] [PubMed] [Google Scholar]
- 7.Perkins BA, Olaleye D, Zinman B, Bril V. Simple screening tests for peripheral neuropathy in the diabetes clinic. Diabetes Care. 2001;24:250–6. doi: 10.2337/diacare.24.2.250. [DOI] [PubMed] [Google Scholar]
- 8.Armstrong DG. The 10-g monofilament: the diagnostic divining rod for the diabetic foot? Diabetes Care. 2000;23:687. doi: 10.2337/diacare.23.7.887. [DOI] [PubMed] [Google Scholar]
- 9.Armstrong DG, Lavery LA, Vela SA, Quebedeaux TL, Fleischli JG. Choosing a practical screening instrument to identify patients at risk for diabetic foot ulceration. Arch Intern Med. 1998;158:289–92. doi: 10.1001/archinte.158.3.289. [DOI] [PubMed] [Google Scholar]
- 10.de Sonnaville JJ, Colly JLP, Wijkel D, Heine RJ. The prevalence and determinants of foot ulceration in type II diabetic patients in a primary health care setting. Diabetes Res Clin Pract. 1997;35:149–56. doi: 10.1016/s0168-8227(97)01380-6. [DOI] [PubMed] [Google Scholar]
- 11.Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Davignon DR, Smith DG. A prospective study of risk factors for diabetic foot ulcer. The Seattle Diabetic Foot Study. Diabetes Care. 1999;22:1036–42. doi: 10.2337/diacare.22.7.1036. [DOI] [PubMed] [Google Scholar]
- 12.Rith-Najarian SJ, Stolusky T, Gohdes DM. Identifying diabetic patients at risk for lower extremity amputation in a primary health care setting.A prospective evaluation of simple screening criteria. Diabetes Care. 1992;15:1386–9. doi: 10.2337/diacare.15.10.1386. [DOI] [PubMed] [Google Scholar]
- 13.Pham H, Armstrong DG, Harvey C, Harkless LB, Giurini JM, Veves A. Screening techniques to identify people at high risk for diabetic foot ulceration: a prospective multicenter trial. Diabetes Care. 2000;23:606–11. doi: 10.2337/diacare.23.5.606. [DOI] [PubMed] [Google Scholar]
- 14.Liniger C, Albeanu A, Bloise D, Assal JP. The tuning fork revisited. Diabet Med. 1990;7:859–64. doi: 10.1111/j.1464-5491.1990.tb01319.x. [DOI] [PubMed] [Google Scholar]
- 15.Tres GS, Lisbôa HR, Syllos R, Canani LH, Gross JL. Prevalence and characteristics of diabetic polyneuropathy in Passo Fundo, South of Brazil. Arq Bras Endocrinol Metabol. 2007;51:987–92. doi: 10.1590/s0004-27302007000600014. [DOI] [PubMed] [Google Scholar]
- 16.Bowditch MG, Sanderson P, Livesey JP. The significance of an absent ankle reflex. J Bone Joint Surg Br. 1996;78:276–9. [PubMed] [Google Scholar]
- 17.Meijer JW, Bosma E, Lefrandt JD, Links TP, Smit AJ, Stewart RE, et al. Clinical diagnosis of diabetic polyneuropathy with the diabetic neuropathy symptom and siabetic neuropathy examination scores. Diabetes Care. 2003;26:697–701. doi: 10.2337/diacare.26.3.697. [DOI] [PubMed] [Google Scholar]


