Abstract
Background:
Persons with schizophrenia are reported to be more likely to die from cardiovascular illness than those in the general population, and are at a greater risk of developing obesity, diabetes type 2, hypertension and dyslipidemias. Antipsychotic drugs used in the treatment of schizophrenia and other psychotic illnesses can induce weight gain, with some agents having a greater propensity to do so than others. These adverse effects associated with second-generation antipsychotics are also part of the metabolic syndrome.
Aims:
The aim of this study was to evaluate the emergence of metabolic syndrome due to second-generation antipsychotics as compared with conventional (typical) antipsychotics.
Settings and Design:
A prospective interventional study was conducted at the Psychiatric Centre, Jaipur. The study included 120 patients, both indoor and outdoor, suffering from schizophrenia diagnosed using the ICD-10 criteria. The patients were grouped into four categories, i.e. control group and three study groups, each group having 30 patients.
Materials and Methods:
Thirty patients were given conventional antipsychotics and 90 were given second-generation antipsychotics, including risperidone, olanzapine and clozapine. Metabolic parameters were taken before onset of drug treatment therapy and after 4 months. The changes in metabolic parameters were compared using appropriate statistical tools.
Statistical Analysis:
Chi square chart and Unpaired t-test were used for statistical analysis using a computer.
Results:
11.66% of the patients developed metabolic syndrome after 4 months of antipsychotic medication.
Conclusions:
Second-generation antipsychotics cause significantly more changes in the metabolic parameters, increasing the chances of developing metabolic syndrome and associated disorders like diabetes mellitus type-II and cerebrovascular accidents. Olanzapine is the antipsychotic drug that has the maximum potential to cause metabolic syndrome.
Keywords: Atypical antipsychotics, metabolic syndrome, schizophrenia
INTRODUCTION
Persons suffering from severe mental illness, particularly schizophrenia, suffer from increased morbidity and mortality compared with the general population, having a life expectancy that is approximately 20% shorter.[1,2]
Schizophrenia has been described as a “life-shortening disease,” and there is growing evidence to support this claim.[3,4]
Without discounting suicide, which accounts for less than one-third of premature deaths, people diagnosed with schizophrenia can expect to live 9–12 years lesser, on average, than those in the general population.[5]
Most of the excess mortality in persons suffering from schizophrenia is attributed to physical illness, with cardiovascular illness being the major contributor. Persons with schizophrenia are reported to be twice as likely to die from cardiovascular illness as those in the general population. They are at a greater risk of developing obesity, diabetes type 2, hypertension and dyslipidemia as compared with the normal population.[6]
A serious concern for physicians is the development of metabolic syndrome, also known as syndrome X, in patients suffering from schizophrenia, which encompasses medical conditions such as obesity, hypertension, hypertriglyceridemia and impaired glucose tolerance.
Metabolic syndrome is a collection of risk factors that are associated with increased morbidity and mortality due to type 2 diabetes mellitus and cardiovascular disease.[7]
In the general adult population, the metabolic syndrome is an intermediate step toward the final endpoint of type II diabetes and cardiovascular disease.[8,9]
Individuals with the metabolic syndrome have higher rates of coronary heart disease, myocardial infarction and stroke than individuals with any one of the components of hypertension, insulin resistance, dyslipidemia or obesity.[10,11]
At present, it is not clear whether the metabolic syndrome has a single cause, and it appears that it can be precipitated by multiple underlying risk factors. The most important of these underlying risk factors are abdominal obesity and insulin resistance.[12,13] Accumulating evidence suggests that simply varying degrees of insulin resistance may be the common etiological factor for the individual components of metabolic syndrome.[14]
Some of the studies attribute metabolic syndrome in mentally ill patients to their sedentary life style, lack of exercise and physical work, poor nutrition, chronic stress, smoking as well as abnormalities of the hypothalamic-pituitary–adrenal axis.[6,15–18]
Because of the lower rates of extra pyramidal side-effects[19] and tardive dyskinesia[20] as well as superior[21] and potentially broader efficacy than conventional neuroleptics,[22] second-generation antipsychotics are widely prescribed for psychotic and nonpsychotic disorders. However, reports of significant weight gain dyslipidemia and hyperglycemia have caused considerable concern.[23–27] These adverse effects associated with second-generation antipsychotics are also part of the metabolic syndrome.
The metabolic potential of weight is location dependent. Intra-abdominal fat is relatively insulin resistant. Large amounts of intra-abdominal fat are typically associated with adverse metabolic consequences.
No study has so far conclusively indicated the etiology of metabolic syndrome in psychiatric patients, although it is generally believed that the disease itself, the associated lifestyle and dietary habits and antipsychotic drug therapy contribute to the genesis of this disorder.
There are limited data on the prevalence of metabolic syndrome in patients with schizophrenia at the onset of the disorder and, specifically, no data on patients treated in the era when only first-generation antipsychotics were available.
No study has been performed so far to find out the attribution of atypical antipsychotics in the causation of metabolic syndrome in drug naïve patients suffering from schizophrenia who are physically fit and “metabolically normal.”
MATERIALS AND METHODS
The aim of the study was to find out drug-emergent metabolic syndrome in psychiatric patients receiving second-generation antipsychotics.
Study design
A prospective interventional study was conducted in patients receiving antipsychotics (atypical antipsychotics) at Psychiatric Centre, Jaipur. Both indoor patients and outdoor patients were included in the study.
Patients attending the outpatient department as well patients admitted in the indoor ward were screened for diagnosis of schizophrenia using the ICD-10 criteria. The diagnosis of all the patients was confirmed by two consultant psychiatrists at Psychiatric Centre, Jaipur.
The study included 120 consecutive patients suffering from schizophrenia diagnosed using the ICD-10 criteria. Pharmacy and medical records were reviewed to obtain demographic, clinical and drug treatment data.
Each patient included in the study was subjected to measurements of blood pressure, fasting blood glucose, fasting blood triglycerides, fasting high-density lipoprotein (HDL) and waist circumference (measured midway between the lowest rib and the iliac crest with the subjects standing using a tape with a spring-loaded mechanism to standardize tape tension during measurement).
The study group comprised of 90 patients who were either drug treatment naïve or who had not received antipsychotic treatment in the last 6 months (long washout period). The group was further divided into three subgroups, i.e. subgroup A, subgroup B and subgroup C, with each group having 30 patients.
The patients included in the study were given second-generation antipsychotics (risperidone, olanzapine and clozapine to subgroups A, B and C, respectively) for a period of 4 months.
No typical antipsychotic or mood stabilizer drug will be given for whatsoever reason to the study group patients. In case of agitated or hostile patients, only benzodiazepines (injectable or tablet form) will be given to sedate the patient.
The control group comprised of 30 treatment naïve patients or patients who had not received any antipsychotic treatment in the last 6 months, diagnosed with schizophrenia as per the ICD-10 criteria. These patients received haloperidol, which is a typical antipsychotic, for a period of 4 months.
Measurements of blood pressure, fasting blood glucose, fasting HDL levels, fasting triglycerides level and waist circumference were repeated after 1 month and 4 months, respectively.
After 4 months of receiving antipsychotic treatment, all patients will be subjected to the Adult Treatment Panel-III (ATP-III)-defined criteria for metabolic syndrome to find out the incidence of metabolic syndrome in patients receiving atypical antipsychotics.
Inclusion criteria
Adult males/females of age between 18 and 60 years, who were cases of schizophrenia diagnosed as per the ICD-10 criteria. Only physically active patients were included (patients were considered to be physically active if they regularly engaged in an aerobic type of activity at least twice per week for 20 min; these activities included walking, jogging, swimming or garden/yard work).
Exclusion criteria
Patients who had received prior antipsychotic medication in the last 6 months. Patients having any of the five features of metabolic syndrome, patients having any type of cardiovascular disorder, whether under treatment or not, and known patients of diabetes (even if having fasting blood sugar controlled below 110 mg/dl by any diabetic medication) were excluded.
Patients with history of co-morbid substance abuse, pregnant patients, patients having family history of diabetes and patients having co-morbid chronic medical illness were also excluded.
Tools and instruments
The Tenth Revision of the International Classification of Diseases and Related Health Problems (ICD-10) classification of mental and behavioural disorders.
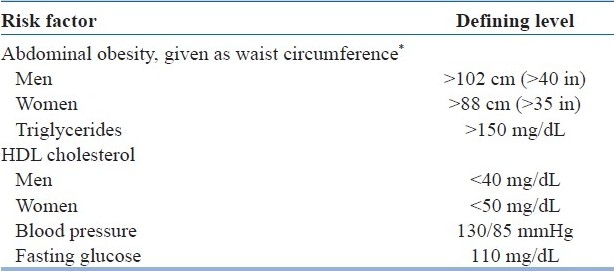
Adult Treatment Panel (ATP III) diagnostic guidelines for metabolic syndrome [Table 1]. Patients having three or more than three of the risk factors with values higher than the defining levels were considered to be having metabolic syndrome.
Chi-square test and unpaired t-test were used for statistical analysis.
Table 1.
Risk factors and defining levels
RESULTS AND DISCUSSION
This study is probably the first to study the metabolic effects of typical and atypical antipsychotics in drug naïve patients suffering from schizophrenia who were having no metabolic abnormalities or other significant illness before commencement of the drug treatment. There is relative paucity of studies on the metabolic side-effects of antipsychotics on treatment naïve patients suffering from schizophrenia. This study is unique in the sense that the subjects recruited were not only treatment naïve but were also physically fit and devoid of any medical disorder or metabolic derangement.
Of the 120 patients recruited in the study, 68 (56.66%) had never taken any antipsychotic treatment in their life, i.e. treatment naïve patients, and 52 (43.33%) of the patients had not taken any antipsychotic medication for the last 6 months.
Out of the 120 patients included in the study, 14 (11.66%) patients developed metabolic syndrome after 4 months of continuous antipsychotic drug therapy [Table 2]. No patient who received haloperidol developed metabolic syndrome, while seven out of 30 (23.3%) patients belonging to the olanzapine group developed metabolic syndrome. Three (10%) and four (13%) patients who received risperidone and clozapine respectively fulfilled the criteria of metabolic syndrome. This difference between the four treatment groups is highly statistically significant.
Table 2.
Drug-emergent metabolic syndrome in different treatment groups
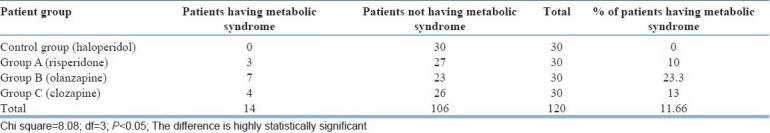
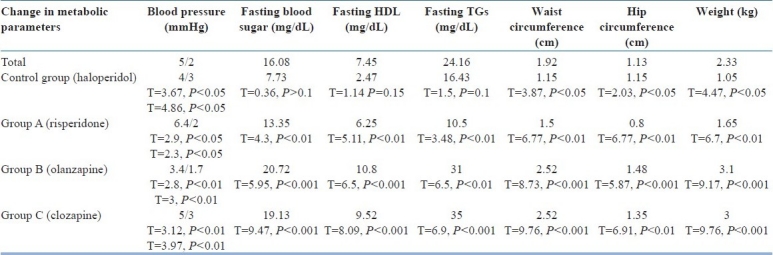
Table 3 shows the change in metabolic parameters after completion of the study. It was found that maximum change in blood pressure occurred in group A (risperidone) while maximum change in other metabolic parameters occurred in group B, except for fasting TGs, which increased maximally in group C. The mean change in blood pressure is statistically significant but, physiologically, almost insignificant as it is as little as 6 mmHg in systolic value and 2.4 mmHg in diastolic value.
Table 3.
Change in metabolic parameters after 4 months
Almost all the antipsychotics are associated with weight gain, while olanzapine and clozapine have been identified as the drugs causing maximum weight gain [Tables 4 and 5]. The mechanisms by which antipsychotic medications produce weight gain may include stimulating appetite, reducing physical activity and directly impairing metabolic regulation. The pathophysiology of weight gain is mediated through monoaminergic, cholinergic and histaminergic neurotransmission. Differential affinities for the serotonin 5-HT2C and H1 receptors may explain the greater weight gain seen with clozapine and olanzapine.
Table 4.
Mean baseline metabolic parameters
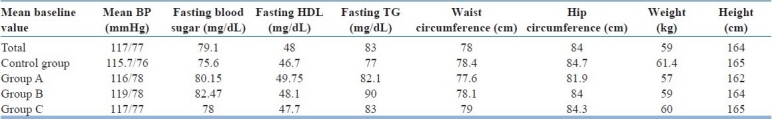
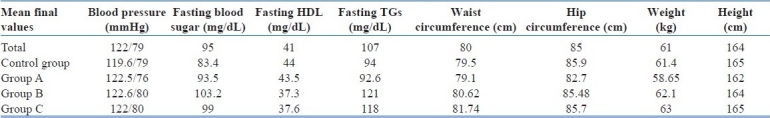
Table 5.
Mean final parameters
Previous studies have suggested that second-generation antipsychotics vary in their propensity to induce weight gain; clozapine and olanzapine produce the most weight gain, quetiapine and risperidone produce intermediate weight gain while aripipirazole and ziprasidone has the least propensity to do so.[18,26] Similar results were achieved by studies conducted by Perez Iglesias[27] and Manjunatha et al.,[28] but the absolute weight gain was higher in this study (5.1 kg in the olanzapine group, 4 kg in the risperidone group and 2.8 kg in the haloperidol group).
The landmark CATIE's first phase study also replicated similar results, and it states that the weight gain potential of olanzapine is approximately 2 pound/month.[29]
Bustillo,[30] in a 4-month study, found that the mean weight gain in patients receiving olanzapine was 3.5 kg and in those receiving haloperidol was 1.5 kg, which was similar to the findings in this study.
It was found that maximum increase in mean fasting sugar levels occurred in the olanzapine and clozapine treatment groups, while the increment was less significant in the risperidone group and in the control (haloperidol) group. These findings were similar to those of Jean-Pierre et al.,[31] who also compared the change in blood glucose and lipid profile after giving the above-mentioned drug treatment to his patients for 14 weeks. Perez Iglasias[27] found a similar pattern of increase in the fasting glucose level after a 12-week study with treatment naïve patients, but the increase was statistically insignificant for any other treatment group. Newcomer[26] found that patients treated with olanzapine and clozapine had the highest propensity to develop glucose intolerance while patients taking either haloperidol or risperidone has the least propensity for the same.
An increase in the fasting TG levels is highest in group C (clozapine group), followed by group B (olanzapine group), while it was minimum in the risperidone group.
The following conclusions were drawn from the study:
11.66% patients developed metabolic syndrome after 4 months of antipsychotic medication.
Olanzapine is the antipsychotic drug that has the maximum potential to cause metabolic syndrome. Haloperidol has the least potential to cause metabolic syndrome. Clozapine and risperidone also have the potential to cause metabolic syndrome but have a lower potential to do so as compared with olanzapine. Olanzapine causes maximum weight gain while haloperidol causes least weight gain among the four antipsychotics studied. There is no significant difference between haloperidol and risperidone in their propensity to cause one or more metabolic derangements and weight gain. The potential to cause weight gain and other metabolic derangement is almost similar with olanzapine and clozapine. Risperidone can be regarded as the safest antipsychotic among the three atypical antipsychotic drugs when the metabolic side-effects of three second-generation antipsychotics are taken into consideration.
Both drug-free patients and treatment naïve patients have almost the same propensity to develop metabolic syndrome. It also implies that schizophrenia per se does not increase the propensity to cause metabolic syndrome.
Patients with schizophrenia receive little or no medical care. Such care is important given the risk of metabolic abnormalities associated with antipsychotic medications. In response to these issues, it is recommended that monitoring of body mass index, lipid levels, fasting blood glucose levels and blood pressure should be performed regularly. Regular monitoring may be especially critical for patients taking atypical antipsychotics given the high prevalence of metabolic syndrome reported in this study and in others.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Osby U, Correia N, Brandt L, Ekbom A, Sparén P. Mortality and causes of death in schizophrenia in Stockholm county, Sweden. Schizophr Res. 2000;29:21–8. doi: 10.1016/s0920-9964(99)00191-7. [DOI] [PubMed] [Google Scholar]
- 2.Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150:1115–21. doi: 10.1016/j.ahj.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 3.Allebeck P. Schizophrenia: A life shortening disease. Schizophr Bull. 1989;15:81–9. doi: 10.1093/schbul/15.1.81. [DOI] [PubMed] [Google Scholar]
- 4.Black DW, Fisher R. Mortality in DSM-III-R schizophrenia. Schizophr Res. 1992;7:109–16. doi: 10.1016/0920-9964(92)90040-c. [DOI] [PubMed] [Google Scholar]
- 5.Lambert TJ, Velakoulis D, Pantelis C. Medical comorbidity in schizophrenia. Med J Aust. 2003;178:S67–70. doi: 10.5694/j.1326-5377.2003.tb05311.x. [DOI] [PubMed] [Google Scholar]
- 6.Casey DE. Metabolic issues and cardiovascular diseases in patients with psychiatric disorders. Am J Med. 2005;118:15s–22. doi: 10.1016/j.amjmed.2005.01.046. [DOI] [PubMed] [Google Scholar]
- 7.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 8.Lempiäinen P, Mykkänen L, Pyörälä K, Laakso M, Kuusisto J. Insulin-resistance syndrome predicts coronary heart disease events in elderly nondiabetic men. Circulation. 1999;100:123–8. doi: 10.1161/01.cir.100.2.123. [DOI] [PubMed] [Google Scholar]
- 9.Kekäläinen P, Sarlund H, Pyörälä K, Laakso M. Hyperinsulinemia cluster predicts the development of Type 2 diabetes independent of a family history of diabetes. Diabetes Care. 1999;22:86–92. doi: 10.2337/diacare.22.1.86. [DOI] [PubMed] [Google Scholar]
- 10.Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–9. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 11.Trevisan M, Liu J, Bahsas FB, Menotti A. (Risk Factor and Life Expectancy Research Group): Syndrome X and mortality: A population-based study. Am J Epidemiol. 1998;148:958–66. doi: 10.1093/oxfordjournals.aje.a009572. [DOI] [PubMed] [Google Scholar]
- 12.Citrome L. Metabolic syndrome and cardiovascular disease. J psychopharma. 2004;19:84–93. doi: 10.1177/0269881105058375. [DOI] [PubMed] [Google Scholar]
- 13.Liese A, Mayer-Davis E, Haffner S. Development of the multiple metabolic syndrome: An epidemiologic perspective. Epidemiol Rev. 1998;20:157–72. doi: 10.1093/oxfordjournals.epirev.a017978. [DOI] [PubMed] [Google Scholar]
- 14.Lieberman JA., 3rd Metabolic changes associated with antipsychotic use. Prim Care Companion J Clin Psychiatry. 2004;6:8–13. [PMC free article] [PubMed] [Google Scholar]
- 15.Brown S, Birtwistle J, Roe L, Thompson C. The unhealthy lifestyle of people with schizophrenia. Psychol Med. 1999;29:697–701. doi: 10.1017/s0033291798008186. [DOI] [PubMed] [Google Scholar]
- 16.Ryan MC, Collins P, Thakore JH. Impaired fasting glucose tolerance in first-episode, drug-naive patients with schizophrenia. Am J Psychiatry. 2003;160:284–9. doi: 10.1176/appi.ajp.160.2.284. [DOI] [PubMed] [Google Scholar]
- 17.Holmberg SK, Kane C. Health and self-care practices of persons with schizophrenia. Psychiatr Serv. 1999;50:827–9. doi: 10.1176/ps.50.6.827. [DOI] [PubMed] [Google Scholar]
- 18.American Diabetic Association. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004;27:596–601. doi: 10.2337/diacare.27.2.596. [DOI] [PubMed] [Google Scholar]
- 19.Kane JM. Extrapyramidal side effects are unacceptable. Eur Neuropsychopharmacol. 2001;11:S397–403. doi: 10.1016/s0924-977x(01)00109-2. [DOI] [PubMed] [Google Scholar]
- 20.Correll CU, Leucht S, Kane JM. Lower risk for tardive dyskinesia associated with second-generation antipsychotics: A systematic review of 1-year studies. Am J Psychiatry. 2004;161:414–25. doi: 10.1176/appi.ajp.161.3.414. [DOI] [PubMed] [Google Scholar]
- 21.Leucht S, Pitschel-Walz G, Abraham D, Kissling W. Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo.A meta-analysis of randomized controlled trials. Schizophr Res. 1999;35:51–68. doi: 10.1016/s0920-9964(98)00105-4. [DOI] [PubMed] [Google Scholar]
- 22.Buckley PF. Broad therapeutic uses of atypical antipsychotic medications. Biol Psychiatry. 2001;50:912–24. doi: 10.1016/s0006-3223(01)01256-2. [DOI] [PubMed] [Google Scholar]
- 23.Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, et al. Antipsychotic-induced weight gain: A comprehensive research synthesis. Am J Psychiatry. 1999;156:1686–96. doi: 10.1176/ajp.156.11.1686. [DOI] [PubMed] [Google Scholar]
- 24.Masand PS. Relative weight gain among antipsychotics. J Clin Psychiatry. 1999;60:706–8. doi: 10.4088/jcp.v60n1014. [DOI] [PubMed] [Google Scholar]
- 25.Wetterling T. Bodyweight gain with atypical antipsychotics: A comparative review. Drug Saf. 2001;24:59–73. doi: 10.2165/00002018-200124010-00005. [DOI] [PubMed] [Google Scholar]
- 26.Newcomer JW, Haupt DW, Fucetola R, Melson AK, Schweiger JA, Cooper BP, et al. Abnormalities in glucose regulation during antipsychotic treatment of schizophrenia. Arch Gen Psychiatry. 2002;59:337–45. doi: 10.1001/archpsyc.59.4.337. [DOI] [PubMed] [Google Scholar]
- 27.Perez-Iglesias R, Crespo-Facorro B, Amado JA, Garcia-Unzueta MT, Ramirez-Bonilla ML, Gonzalez-Blanch C, et al. A 12-week randomized clinical trial to evaluate metabolic changes in drug-naive, first-episode psychosis patients treated with haloperidol, olanzapine, or risperidone. J Clin Psychiatry. 2007;68:1733–40. doi: 10.4088/jcp.v68n1113. [DOI] [PubMed] [Google Scholar]
- 28.Saddichha S, Manjunatha N, Ameen S, Akhtar S. Effect of olanzapine, risperidone, and haloperidol treatment on weight and body mass index in first episode schizophrenia patients in India: A randomized, double-blind, controlled, prospective study. J Clin Psychiatry. 2007;68:1793–8. doi: 10.4088/jcp.v68n1120. [DOI] [PubMed] [Google Scholar]
- 29.Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209–23. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- 30.Bustillo JR, Buchanan RW, Irish D, Breier A. Differential effect of clozapine on weight: A controlled study. Am J Psychiatry. 1996;153:817–9. doi: 10.1176/ajp.153.6.817. [DOI] [PubMed] [Google Scholar]
- 31.Lindenmayer JP, Czobor P, Volavka J, Citrome L, Sheitman B, McEvoy JP, et al. changes in glucose and cholesterol levels in patients with schizophrenia treated with typical or atypical antipsychotics. Am J Psychiatry. 2003;160:290–6. doi: 10.1176/appi.ajp.160.2.290. [DOI] [PubMed] [Google Scholar]


