Abstract
OBJECTIVES:
Endometriosis and uterine fibroids are common gynecological disorders in fertile women. It has been suggested that these two disorders may be associated with each other. In this study, we tested whether this connection exists. In addition, we wanted to evaluate whether they both affect fertility independently of each other.
MATERIALS AND METHODS:
The prevalence of endometriosis and uterine fibroids was investigated in three groups of patients: Symptomatic patients requiring surgery either for endometriosis (n=182), or for uterine fibroids (n=240) and asymptomatic patients undergoing laparoscopic sterilization (n=183). The prevalences were examined in three age groups: 35–39 yrs, 40–44 yrs and ≥ 45 yrs. The significance of both diagnoses on fertility was assessed using logistic regression analysis.
RESULTS:
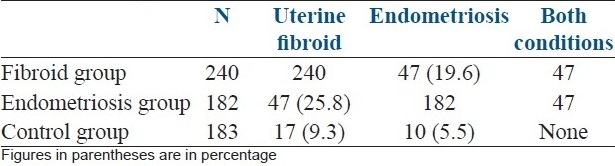
Uterine fibroids were detected in 25.8% (47/182) of patients with endometriosis. Endometriosis was detected in 19.6% (47/240) of patients with uterine fibroids. 5.5% (10/183) women undergoing sterilization had endometriosis and 19.3% (17/183) had uterine fibroids. Both uterine fibroids and endometriosis were, independently of each other, related to subfertility (OR, 95% CI: 3.8, 2.3–6.5; 6.8, 4.0–11.6, respectively).
CONCLUSIONS:
The results suggest that symptomatic endometriosis appears together with symptomatic uterine fibroids. Both diseases seem to decrease female fertility independently of each other.
Keywords: Endometriosis, subfertility, uterine fibroids
INTRODUCTION
Endometriosis and uterine fibroids are common gynecological disorders in fertile women. Uterine fibroids are estimated to occur in 33-77% of women during their reproductive years.[1,2] Even though most fibroids are asymptomatic, they are still the most common reason for hysterectomy.[2–6] The symptoms are related to their size, number and location in the uterus. Common symptoms are menorrhagia, pelvic pressure or pain and urinary symptoms.[2,4,7] The incidence of endometriosis is even more difficult to state because the exact diagnosis requires invasive intervention.[8,9] Within symptomatic women who have had surgery, the incidence has varied between 2 and 18%[10,11] The symptoms of endometriosis are chronic pelvic pain, dysmenorrhea, menorrhagia, vibration pain, dyspareunia and dysuria. The proportion of asymptomatic women is significant.[8–10,12] Both endometriosis and uterine fibroids may cause infertility.[10,13–15]
It has been suggested that these two disorders may be associated with each other and that their etiology has some similarities.[16,17] Both these diseases are steroid hormone-dependent[1–3,11,12,18,19] and they act similarly under the influence of estrogen.[20–22] In one previous study, women with uterine fibroids were reported to have endometriosis more often than those without fibroids.[23] We wanted to test here whether this connection between uterine fibroids and endometriosis exists. In addition, if the connection seems to be apparent, we wanted to evaluate whether they both affect female fertility independently of each other.
MATERIALS AND METHODS
The study was approved by the Ethics Committee of the Oulu University Hospital. We retrospectively studied the hospital records of patients operated on for endometriosis or uterine fibroids (the study groups) or sterilization (the control group) between the years 1990 and 2005 at the Department of Obstetrics and Gynecology, Oulu University Hospital. The search was made for the hospital records based on the diagnosis numbers for endometriosis, uterine fibroids and birth control planning, and on the operation numbers for explorative laparoscopy, laparoscopic excision of peritoneum lesion, abdominal and laparoscopical hysterectomy and sterilization. The subjects undergoing sterilization had no symptoms of endometriosis or uterine fibroids. Only subjects with complete hospital records were included. The diagnosis of endometriosis was based on the pelvic view during laparoscopic sterilization. The diagnosis of fibroids was based on a preoperative transvaginal ultrasonographic examination.
Subjects aged 35 years or older at the time of operation were included. This age limit was chosen because endometriosis has its highest incidence during the early fertile years and it tends to disappear after ovarian function declines.[10] Fibroids, on the contrary, tend to appear more frequently in the late fertile years and they do not disappear after menopause as endometriosis does.[7] The study design is clarified in Figure 1.
Figure 1.

The study design
The association of the diseases was analyzed as follows: The presence of endometriosis, uterine fibroids, or both occurring together was analyzed in all groups. Then an analysis was made among different age groups in the fibroid group and the control group (comparison 1) and between the endometriosis group and the control group (comparison 2). The endometriosis group comprised 182 patients, the uterine fibroid group 240 patients, and the control group 183 patients [Table 1, Figure 1]. Since 47 patients had both conditions they were included in both disease groups. The comparisons are made within the disease group and the control group, so this does not disturb the analysis.
Table 1.
The prevalence of the diseases
Statistical analysis
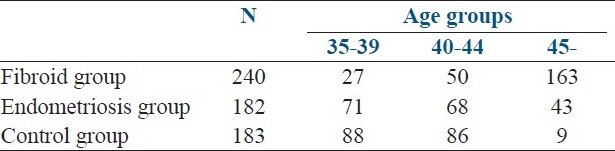
Departure from a normal distribution was assessed using the Kolmogorov-Smirnov test. Paired t-tests were used for normally distributed data, and the Mann-Whitney test (the signed-rank) for skewed data. Proportions were compared by the χ2 test. P<0.05 was considered statistically significant. All values given are the mean±standard deviation (SD). The patients were divided into subgroups according to their age. The age-groups were patients age 35-39, 40-44 and 45 years and older [Table 2].
Table 2.
The study population
A logistic regression analysis was used to identify independent factors affecting parity, which here reflects fertility status. Parity was assessed as either having no deliveries or having at least one delivery. Only statistically significant factors were included in the final model. The Hosmer-Lemeshow goodness-of-fit statistic was used to assess the final model. The factors selected for the final analysis were diagnosis of endometriosis and diagnosis of uterine fibroids at the time of operation. All factors were treated as dichotomous variables: Existence of endometriosis or no endometriosis; existence of fibroids or no fibroids. Statistical analysis was performed using SPSS for Windows 12.01 (SPSS Inc., Chicago, IL).
RESULTS
Comparison 1: Fibroid group vs control group
In the fibroid group, 19.6% (47/240) of the patients and 5.5% (10/183) of the control group had endometriosis. The mean difference of the prevalence between the groups was 14.1% (95%CI 8.1-20.1%).
The comparison in different age groups revealed that the prevalence of endometriosis was increased among fibroid patients compared to the control group in the age groups 35-39 and 40-44: 37.0 vs. 6.8% (difference 30.2%, 95% CI 11.3-49.2%) and 34.0 vs. 4.6% (difference 29.4%, 95% CI 15.6-43.3%), respectively [Figure 2]. After age 45 the prevalence of endometriosis decreased remarkably in the fibroid group, from 34.0 to 12.3% (difference 21.7%, 95% CI 7.7-35.8%).
Figure 2.
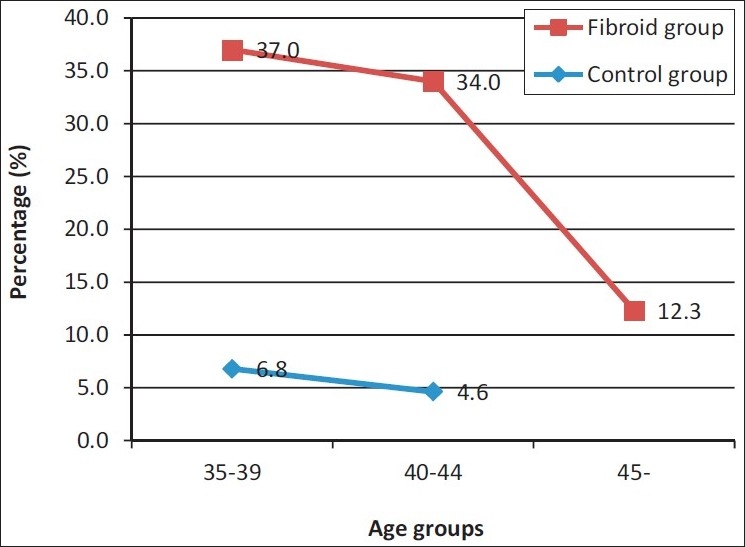
Prevalence of endometriosis
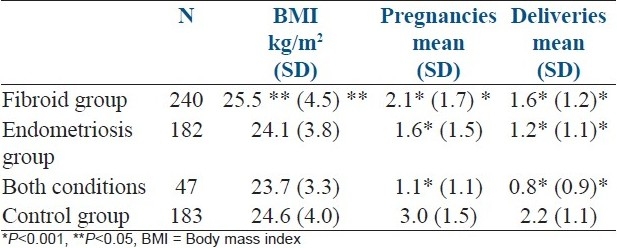
There were fewer deliveries in the fibroid group than in the control group [Table 3]. Patients with fibroids had a slightly higher BMI than the patients in the control group, 25.5 kg/m2 vs 24.6 kg/m2 (P<0.05).
Table 3.
Patient characteristics in the study groups
Comparison 2: Endometriosis group vs control group
In the endometriosis group, 25.8% (47/182) of the patients and 9.3% (17/183) of the control group had fibroids. The mean difference of the prevalence between the endometriosis and control groups was 16.5% (95% CI 8.9-24.2%).
The difference in the prevalence of uterine fibroids in the endometriosis and control group remained stable with advanced female age. The prevalence of uterine fibroids in the endometriosis group increased significantly with advancing age, from 14.1% in age group 35-39 to 46.5% in the age group over 45 (difference 32.4%, 95% CI 15.5-49.4%) [Figure 3].
Figure 3.
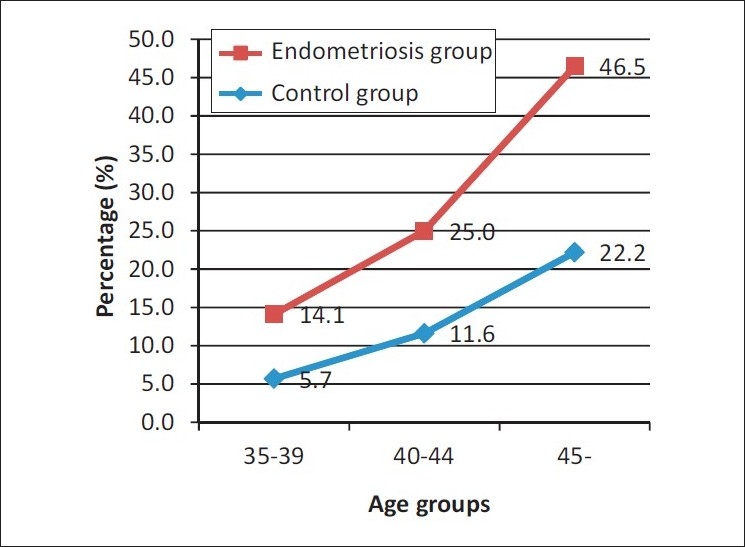
Prevalence of uterine fibroids
There were fewer deliveries in the endometriosis group than in the control group [Table 3]. There was not a statistically significant difference in BMI between these groups.
In the disease groups, there were altogether 47 patients with both conditions. There were no such cases in the control group.
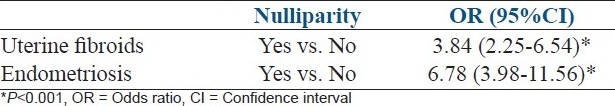
Logistic regression analysis
Since the prevalence of endometriosis and fibroids seemed to coincide, we wanted to test whether they both are independent factors associated with subfertility. We used logistic regression analysis, in which nulliparity at the time of operation was determined as subfertility [Table 4]. Data fitted the logistic regression analysis, as indicated by the Hosmer–Lemeshow goodness-of-fit test. Both endometriosis and fibroids proved to be independent factors associated with nulliparity.
Table 4.
Association for nulliparity. Logistic regression analysis revealed two independent factors, uterine fibroids and endometriosis that were significantly associated with nulliparity
DISCUSSION
Our study suggests that symptomatic endometriosis and symptomatic uterine fibroids appear together. Almost 20% of patients with symptomatic fibroids also had endometriosis. On the other hand, 26% of patients with symptomatic endometriosis also had fibroids. In the control group, none of the patients had both endometriosis and uterine fibroids. Despite the fact that the prevalence of endometriosis and fibroids seemed to coincide, they both were independent factors associated with subfertility in this data set.
Similarly to our results, Hemmings et al.[23] found that patients operated on for endometriosis had fibroids more often than those without endometriosis, and this was suggested to be due to hormone dependency and changes in intrauterine pressure during menses leading to increased retrograde menstrual flow. In a recently published study a majority of symptomatic uterine fibroid patients were also diagnosed with endometriosis.[24] There is a hypothesis that a hyperestrogenic state might have a role in the development of both fibroids and endometriosis. It seems that uterine fibroid cells significantly express aromatase, resulting in elevated tissue concentrations of estrogens in fibroid nodules compared to the surrounding myometrium.[19] Similar to uterine fibroids, endometriotic tissue has been demonstrated to express aromatase and to produce estrogen independently of the ovaries.[19] There are two case reports of rapid growth of both fibroids and endometriosis, and this has been suggested to be a result of a hyperestrogenic state.[21,22] In addition, the role of estrogens is supported by the fact that neither fibroids nor endometriosis appear before the age of onset of fertility, and during the menopause the symptoms of both diseases diminish.[7]
Women with endometriosis and uterine fibroids had fewer pregnancies and deliveries than the subjects in the control group. It is well-known that the prevalence of both diseases is increased among patients seeking infertility treatments, although it is not clear how these diseases cause infertility.[13,15,25] Because our results indicated the connection between the prevalences of endometriosis and fibroids, we wanted to evaluate whether these diseases were independently associated with subfertility or not. According to the National Institute for Health and Welfare, 90% of Finnish women in 2007 delivered their first child before the age of 35 years. Since all patients in our data set were 35 years or older, we determined subfertility as having no deliveries by the time of their operation.
Our analysis revealed that both the diagnosis of endometriosis and of uterine fibroids were independently associated with nulliparity, suggesting that the diagnosis of either one seems to be related to subfertility. The causal relationship between endometriosis and reduced fertility is undetermined, although the prevalence of endometriosis among infertile women is proven to be significantly higher.[15] Our results concerning this relationship go along with the previous results. Those patients who were nulliparous had endometriosis 6.8 times more often than those who had at least one delivery.
Women with uterine fibroids of any location in the uterus have lower rates for clinically diagnosed pregnancies, implantation, and deliveries, and their spontaneous abortion rate is higher. Especially submucosal fibroids have a relation to these rates, but intramural fibroids do as well. The size of fibroids does not seem to have a role in fertility outcomes.[13] Our results were similar. The nulliparous patients had uterine fibroids 3.8 times more often than those who had at least one delivery. Due to the lack of information, we were not able to analyze subfertility due to fibroid location and size.
The prevalence of endometriosis and uterine fibroids is very difficult to examine, because they both tend to have an asymptomatic nature. To diagnose either fibroids or endometriosis, a broader examination than a basic doctor's check-up is required. Uterine fibroids are diagnosed by a standard ultrasonographic examination[2] and endometriosis by a laparoscopic examination.[8] This means that the selection of patients for the control group in this kind of study setting is challenging.[26] Because the reliable diagnosis of endometriosis requires laparoscopy, the best available group for controls consisted of patients undergoing laparoscopy for tubal sterilization. In addition, very few women seek for tubal sterilization after the age of 45, which explains the low number of controls in our study in this age group.
Another challenge in studying endometriosis and uterine fibroids together is the age of the patients. The diagnostic ages differ from each other. The lower age limit was therefore set at 35 years, so that endometriosis would still exist and fibroids, on the other hand, would have already started to appear. There is, however, a possibility that a patient could have had endometriosis earlier and, when fibroids were diagnosed the endometriosis would have had dried out.
In conclusion, the present study showed an association between the prevalence of symptomatic endometriosis and symptomatic uterine fibroids in women aged 35 years or more. Both of these diseases seem to be related to increased subfertility independently of each other.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Okolo S. Incidence, aetiology and epidemiology of uterine fibroids. Best Pract Res Clin Obstet Gynaecol. 2008;22:571–88. doi: 10.1016/j.bpobgyn.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Parker WH. Etiology, symptomatology, and diagnosis of uterine myomas. Fertil Steril. 2007;87:725–36. doi: 10.1016/j.fertnstert.2007.01.093. [DOI] [PubMed] [Google Scholar]
- 3.Flake GP, Andersen J, Dixon D. Etiology and pathogenesis of uterine leiomyomas: A review. Environ Health Perspect. 2003;111:1037–54. doi: 10.1289/ehp.5787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart EA. Uterine fibroids. Lancet. 2001;357:293–8. doi: 10.1016/S0140-6736(00)03622-9. [DOI] [PubMed] [Google Scholar]
- 5.Farquhar CM, Steiner CA. Hysterectomy rates in the United States 1990-1997. Obstet Gynecol. 2002;99:229–34. doi: 10.1016/s0029-7844(01)01723-9. [DOI] [PubMed] [Google Scholar]
- 6.Vuorma S, Teperi J, Hurskainen R, Keskimaki I, Kujansuu E. Hysterectomy trends in finland in 1987-1995--a register based analysis. Acta Obstet Gynecol Scand. 1998;77:770–6. [PubMed] [Google Scholar]
- 7.Payson M, Leppert P, Segars J. Epidemiology of myomas. Obstet Gynecol Clin North Am. 2006;33:1–11. doi: 10.1016/j.ogc.2005.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garry R. Diagnosis of endometriosis and pelvic pain. Fertil Steril. 2006;86:1307–9. doi: 10.1016/j.fertnstert.2006.06.045. discussion 1317. [DOI] [PubMed] [Google Scholar]
- 9.Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364:1789–99. doi: 10.1016/S0140-6736(04)17403-5. [DOI] [PubMed] [Google Scholar]
- 10.Missmer SA, Cramer DW. The epidemiology of endometriosis. 2003;30:1-19. (vii).Obstet Gynecol Clin North Am. 2003;30:1–19. doi: 10.1016/s0889-8545(02)00050-5. [DOI] [PubMed] [Google Scholar]
- 11.Vigano P, Parazzini F, Somigliana E, Vercellini P. Endometriosis: Epidemiology and aetiological factors. Best Pract Res Clin Obstet Gynaecol. 2004;18:177–200. doi: 10.1016/j.bpobgyn.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Nap AW, Groothuis PG, Demir AY, Evers JL, Dunselman GA. Pathogenesis of endometriosis. Best Pract Res Clin Obstet Gynaecol. 2004;18:233–44. doi: 10.1016/j.bpobgyn.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Pritts EA, Parker WH, Olive DL. Fibroids and infertility: An updated systematic review of the evidence. Fertil Steril. 2009;91:1215–23. doi: 10.1016/j.fertnstert.2008.01.051. [DOI] [PubMed] [Google Scholar]
- 14.Klatsky PC, Tran ND, Caughey AB, Fujimoto VY. Fibroids and reproductive outcomes: A systematic literature review from conception to delivery. Am J Obstet Gynecol. 2008;198:357–66. doi: 10.1016/j.ajog.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 15.Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility. Fertil Steril. 2006;86:S156–60. doi: 10.1016/j.fertnstert.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 16.Bulun SE, Imir G, Utsunomiya H, Thung S, Gurates B, Tamura M, et al. Aromatase in endometriosis and uterine leiomyomata. J Steroid Biochem Mol Biol. 2005;95:57–62. doi: 10.1016/j.jsbmb.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 17.Hsieh YY, Chang CC, Tsai FJ, Lin CC, Tsai CH. T homozygote and allele of epidermal growth factor receptor 2073 gene polymorphism are associated with higher susceptibility to endometriosis and leiomyomas. Fertil Steril. 2005;83:796–9. doi: 10.1016/j.fertnstert.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 18.Bulun SE. Endometriosis. N Engl J Med. 2009;360:268–79. doi: 10.1056/NEJMra0804690. [DOI] [PubMed] [Google Scholar]
- 19.Bulun SE, Lin Z, Imir G, Amin S, Demura M, Yilmaz B, et al. Regulation of aromatase expression in estrogen-responsive breast and uterine disease: From bench to treatment. Pharmacol Rev. 2005;57:359–83. doi: 10.1124/pr.57.3.6. [DOI] [PubMed] [Google Scholar]
- 20.Koshiyama M, Okamoto T, Ueta M. The relationship between endometrial carcinoma and coexistent adenomyosis uteri, endometriosis externa and myoma uteri. Cancer Detect Prev. 2004;28:94–8. doi: 10.1016/j.cdp.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Kurioka H, Takahashi K, Ueda T, Ozaki T, Miyazaki K. Endometriosis and uterine leiomyomata with ovarian granulosa cell tumour. Hum Reprod. 1998;13:1357–60. doi: 10.1093/humrep/13.5.1357. [DOI] [PubMed] [Google Scholar]
- 22.Strang A, Lisson SW, Petrou SP. Ureteral endometriosis and coexistent urethral leiomyoma in a postmenopausal woman. Int Braz J Urol. 2004;30:496–8. doi: 10.1590/s1677-55382004000600008. [DOI] [PubMed] [Google Scholar]
- 23.Hemmings R, Rivard M, Olive DL, Poliquin-Fleury J, Gagné D, Hugo P, et al. Evaluation of risk factors associated with endometriosis. Fertil Steril. 2004;81:1513–21. doi: 10.1016/j.fertnstert.2003.10.038. [DOI] [PubMed] [Google Scholar]
- 24.Huang JQ, Lathi RB, Lemyre M, Rodriquez HE, Nezhat CH, Nezhat C. Coexistence of endometriosis in women with symptomatic leiomyomas. Fertil Steril. 2010;94:720–3. doi: 10.1016/j.fertnstert.2009.03.052. [DOI] [PubMed] [Google Scholar]
- 25.Khaund A, Lumsden MA. Impact of fibroids on reproductive function. Best Pract Res Clin Obstet Gynaecol. 2008;22:749–60. doi: 10.1016/j.bpobgyn.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 26.Zondervan KT, Cardon LR, Kennedy SH. What makes a good case-control study.design issues for complex traits such as endometriosis? Hum Reprod. 2002;17:1415–23. doi: 10.1093/humrep/17.6.1415. [DOI] [PubMed] [Google Scholar]


