Abstract
Objective
Cardiovascular risk factors increase risk for stroke recurrence. Secondary prevention of stroke may be affected not only by established risk factors, but also socioeconomic status. This study evaluates relationships between socioeconomic status and cardiovascular and behavioral factors.
Design
Cross-section study.
Setting
Public Health and Education Institute, Peking University.
Participants
Outpatients (n = 2354) with a past diagnosis of stroke or transient ischemic attack.
Intervention(s)
The investigation consisted of a questionnaire regarding patients' socioeconomic and living status, and a clinical examination at the research center.
Main outcome measure(s)
Control rates of risk factors for cardiovascular disease.
Results
With regard to hypertension patients, 67.0% were aware of having hypertension, 63.6% were treated and 53.9% had controlled hypertension; for patients with hypercholesterolemia, 46.7% were aware of having hypercholesterolemia, 38.6% were treated and 3.8% had controlled hypercholesterolemia; for patients with diabetes mellitus, 28.0% were aware of having diabetes mellitus, 25.7% were treated and 3.5% had controlled diabetes mellitus. After multivariate analysis, education was the strongest associated factor for controls of hypertension and diabetes mellitus. After adjustment for sex and age, strong and graduated relationships were noted between the level of education and control of risk factors, with the odds ratios increasing at every increment.
Conclusion
Education exerts the most important effect on the control of established cardiovascular risk factors; Successful intervention to reduce these risk factors will have to be addressed, not just with regard to specific risk factors, but also with the societal conditions that lead to the adoption and maintenance of high-risk behaviors.
Keywords: socioeconomic status, secondary prevention, stroke
Introduction
Stroke is the third leading cause of morbidity and mortality in both men and women after heart disease and cancer [1]; with an estimated 1 million cases per year in Europe, 1.2 million in North America and 10 million in the rest of the world, the burden of stroke is enormous. A quarter of all stroke patients have a history of a symptomatic coronary event [2]; these patients are prone to recurrent stroke and coronary heart disease (CHD) events. In the perindopril protection against recurrent stroke study trial, in the subset of patients with recent stroke and a history of CHD, the risk of a new CHD event was as high as the risk of a new stroke [3]. After a stroke/transient ischemic attack, patients are at high risk of short-term non-fatal stroke and of long-term fatal coronary heart disease [4]. The incidence of stroke is likely to increase despite the understanding of underlying risk factors, extensive well-tolerated drug therapy options and the availability of published practice guidelines for the prevention of stroke. Some data suggest that ‘traditional risk factors’ such as cigarette smoking, hypertension, unfavorable lipid profile, obesity and diabetes would explain as much as 85% of the world's experience of atherosclerosis [5]. Optimal management of risk factors, especially the modifiable ones and appropriately targeted pharmacotherapy, have been shown to play a significant role in improving the outcomes and quality-of-life as secondary prevention in patients who have a history of stroke.
There are large differences in health outcomes by socioeconomic status (SES) that cannot be explained fully by traditional arguments, such as access to care or poor health behaviors. We consider a different explanation—better self-management of disease by the more educated. We examine differences with respect to education in awareness of risk factors and treatment adherence among patients with diagnosed stroke, and then assess the impact of SES on health status. We believe that patient's perception level holds the key to enhancing the compliance for secondary prevention of stroke.
Method
Study process
The public health and education institute of Peking University was the general coordinator and the cross-section study was approved by the Medical Ethics Committee of Peking University (Beijing, China). Questionnaires used in the study were developed from the INTERHEART study [6].
Participating centers and sampling methods
A total of 16 hospitals in Beijing, Tianjin and Hebei province were recruited to establish the collaborating network, and data collection was carried out between June 2008 and October 2009. Eligible patients were registered with the use of uniform questionnaires, and core data from each center were reported to the Data Center in Peking University according to a common protocol.
Patient identification and data abstraction
Cases were recruited from the community of those who were discharged from collaborating hospitals. Any stroke patients who had suffered a stroke within the past 5 years were eligible to participate in the study. All patients had medical records with diagnosis by brain computed tomography/magnetic resonance imaging. Patients with ischemic stroke, cerebral hemorrhage, subarachnoid hemorrhage or transient ischemic attacks were included. Uniform questionnaires were filled out according to their medical record and face-to-face interview. Informed consent was obtained from the patients at enrollment. Patients who refused to participate in the study or had difficulties with going to the index hospitals, were thereby excluded from study consideration at the sites where active case ascertainment was to be carried out.
Information collection was undertaken on patient demographic characteristics, medical history, biochemical examinations, medications, lifestyle and SES. Standardized definitions for patient-related variables and clinical diagnoses were applied following the manual of INTERHEART project [6].
Measurements
Lifestyle
Lifestyle items included in this analysis were current and past smoking habits, weight control and exercise habits. Current smokers were defined as those who smoked any tobacco in the previous 12 months. Former smokers were defined as those who had quit more than a year ago. The rate of smoking cessation was calculated as numbers of former smokers divided by numbers of former and current smokers. Individuals were considered physically active if they were regularly involved in moderate or strenuous exercise for ≥4 h per week.
Vascular risk factors
Non-fasting blood samples (20 ml) were drawn from every individual after admission and analyzed for total cholesterol and glucose at recruited hospitals. The analytical laboratories in the research sites had closely coordinated, standardized and calibrated their techniques with the quality control center of Peking University in Beijing.
The following definitions were used. Diabetes—fasting glucose >126 ml/dl, non-fasting glucose >200 ml/dl or self-reported use of diabetes medications; high cholesterol—total cholesterol >240 ml/dl; hypertension—systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg (average of two blood pressure measurements), or self-reported use of hypertension medications; obesity—categorized as normal (body mass index <25 kg/m2) or overweight (25 kg/m2 < body mass index <30 kg/m2)/obese (body mass index ≥30 kg/m2).
Sociodemographic factors
Information on education, occupation and household income as indicators of SES was obtained during the clinic interview. Outpatients were asked about their formal education, the number of years of each type of education and whether their education had been completed. From this information, the level of education was classified into three categories: low (education ≤6 years), medium (6 years < education ≤ 12 years), and high (education > 12 years). The other sociodemographic factors (i.e. ‘having a partner’ and health insurance status) were assessed during the same interview with a questionnaire. On the basis of the question regarding partnership, subjects were categorized into two groups: those currently with a partner and those without a partner, including widowed and divorced persons. Health insurance was dichotomized into those with health insurance (including medical insurance and commercial insurance) and those without insurance (self-paid treatment). Current occupation was collected as a open-ended variable and classified into three groups: professionals/clerks, business owners/merchant and unskilled workers/homemakers. Individuals were judged to have routine exercise if they were regularly involved in moderate (walking, cycling or gardening) or strenuous exercise (jogging, football and vigorous swimming) for 4 h or more a week.
On the basis of patients' awareness, treatment status and control of risk factors, patients were classified into three subgroups: controlled, treated and awareness. Awareness of hypertension was defined as a self-report of any prior diagnosis of hypertension by a health-care professional. Treatment of hypertension was defined as self-reported current use of pharmacological medication to manage high blood pressure. Control of hypertension was defined as having an average systolic blood pressure of <140 mmHg and an average diastolic blood pressure of <90 mmHg in the context of pharmacological treatment of hypertension.
Awareness of high total cholesterol was defined as a self-report of any prior diagnosis of hypercholesterolemia by a health-care professional. Treatment of high cholesterol was defined as self-reported current use of cholesterol-lowering medication. Controlled cholesterol was defined as total cholesterol concentration of <240 mg/dl in the context of pharmacological treatment.
Awareness of diabetes was defined as a self-report of any prior diagnosis of diabetes by a health-care professional. Treatment of diabetes mellitus was defined as self-reported current use of insulin or antidiabetic pills and diabetes control was defined as a fasting glucose <120 ml/dl.
Data analysis
All analyses were performed with SPSS 13.0 and focused on five modifiable risk factors (hypertension, hypercholesterolemia, diabetes mellitus, current smoking and absence of exercise). Demographic and socioeconomic characteristics (age, gender, education, income, occupation and living status) and the prevalence of stroke risk factors were calculated for patients according to laboratory tests in research centers. Next, we calculated the proportion of stroke survivors with hypertension who (i) were aware of their diagnosis of hypertension, (ii) were treated with pharmacological anti-hypertensive medication and (iii) had achieved blood pressure control. Analogous calculations were performed for those with high cholesterol or with diabetes mellitus.
Differences in the prevalence of any risk factor, in reports of awareness of individual stroke risk factor, and in control rates of risk factors among people with impaired SES were assessed using χ2 statistics. Logistic regression models were used to determine univariate and multivariate relationships between control rates of those risk factors and SES. Adjusted odd ratios with 95% confidence intervals were estimated. For multivariable analyses, all the tests used in this study were double sided and considered significant at α < 0.05.
Results
Distribution of stroke risk factors, socioeconomic characters, health behaviors and living statuses of patients appears in Table 1 with probability values for differences by sex. The sample of 2354 had a mean age of 64.9 years (standard deviation 10.4); 68.6% were male; 75.5% lived with partners; the prevalence of hypertension, hypercholesterolemia and diabetes mellitus were 90.8%, 87.1% and 78.4%, respectively. The rates of higher educational level, having health insurance and current smoking were higher in males than that in females (23.1% and 10.1%; 75.3% and 61.5%; 16.5% and 4.2% respectively, P < 0.05), whereas women had higher rates of obesity (5.5%) than men (3.5%). Men tended to have more professional/clerical occupations (51.9%) and routine exercise (62.0%) than women (28.2% and 52.0%) and had higher monthly income (ren min bi (RMB) 1269.85 ± 879.12).
Table 1.
Demographic and socioeconomic character of patients with diagnosed stroke history
| Male (n = 1614) | Female (n = 740) | Overall (n = 2354) | |
|---|---|---|---|
| Age (years) | 64.34 ± 10.71 | 66.32 ± 9.64** | 64.96 ± 10.43 |
| Body mass index (kg/m2) | 24.27 ± 3.22 | 24.48 ± 3.43 | 24.33 ± 3.29 |
| Monthly income (RMB) | 1269.85 ± 879.12 | 1048.12 ± 741.19** | 1201.62 ± 845.15 |
| Obesity (%) | 3.5 | 5.5* | 4.2 |
| Overweight (%) | 38.9 | 40.3 | 39.4 |
| Hypertension (%) | 90.5 | 91.5 | 90.8 |
| Diabetes (%) | 78.0 | 79.3 | 78.4 |
| Dislipidemia (%) | 87.1 | 87.2 | 87.1 |
| Current smoker (%) | 16.5 | 4.2* | 12.7 |
| Former smoker (%) | 55.9 | 12.7** | |
| Education (%) | |||
| ≤6 years | 22.6 | 47.4 | 30.4 |
| 6–12 years | 54.3 | 42.4 | 50.6 |
| >12 years | 23.1 | 10.1%** | 19.0 |
| Occupation (%) | |||
| Professionals/clerks | 51.9 | 28.2** | 44.4 |
| Business owners/merchants | 12.2 | 14.5 | 12.9 |
| Unskilled workers/homemakers | 35.9 | 57.3 | 42.7 |
| Medical insurance (%) | 75.3 | 61.5** | 70.9 |
| Routine exercise (%) | 62.0 | 52.0** | 58.9 |
| Lived with partner (%) | 76.3 | 74.5 | 75.5 |
*P < 0.05; **P < 0.01.
Prevalence, awareness, treatment and control of risk factors
Table 2 shows levels of awareness, treatment and control of hypertension, hypercholesterolemia and diabetes mellitus among stroke patients. No significant difference of the aforementioned risk factors can be observed among different groups (age, sex, education level, income and occupation). Subjects older than 65 had high prevalence of hypercholesterolemia and diabetes mellitus (88.4% and 79.8%) than younger people (85.7% and 76.9%), and men tended to have higher treatment rates than women. In general, rates of awareness, treatment and control rateof risk factors increased with levels of education; the control rate of hypertension, rates of awareness and treatment of hypercholesterolemia were associated with household income. With regard to hypertension, 67.0% of hypertensive patients were aware of having hypertension, 63.6% were treated and 53.9% had controlled hypertension; for patients with hypercholesterolemia, 46.7% were aware of having hypercholesterolemia, 38.6% were treated and 3.8% had controlled hypercholesterolemia; for patients with diabetes mellitus, 28.0% were aware of having diabetes mellitus, 25.7% were treated and 3.5% had controlled diabetes mellitus.
Table 2.
Prevalence, awareness, treatment and control of cardiovascular risk factors according to SES
| Hypertension |
Hypercholesterolemia |
Diabetes mellitus |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence | Awareness | Treatment | Control | Prevalence | Awareness | Treatment | Control | Prevalence | Awareness | Treatment | Control | |
| Sex | ||||||||||||
| Male | 90.5 | 66.4 | 63.0 | 54.3 | 87.1 | 46.4 | 38.0 | 3.8 | 78.0 | 27.0 | 24.2 | 3.2 |
| Female | 91.5 | 68.4 | 64.9 | 53.2 | 87.2 | 47.2 | 40.0 | 3.9 | 79.3 | 30.3 | 28.8* | 4.3 |
| Age | ||||||||||||
| <65 years | 90.9 | 67.5 | 64.3 | 52.8 | 85.7 | 47.5 | 38.7 | 4.0 | 76.9 | 26.5 | 23.5 | 2.9 |
| ≥65 years | 90.8 | 66.6 | 63.0 | 54.9% | 88.4* | 46.0 | 38.5 | 3.7 | 79.8* | 29.4 | 27.6 | 4.0 |
| Education | ||||||||||||
| <6 years | 90.5 | 66.9 | 62.3 | 46.5 | 84.5* | 44.1 | 37.2 | 3.5 | 78.1 | 25.5 | 23.6 | 1.7 |
| 6–9 years | 90.5 | 66.3 | 63.1 | 55.8 | 87.7 | 46.9 | 38.1 | 3.9 | 78.6 | 27.4 | 24.4 | 2.7 |
| >10 years | 92.2 | 69.1 | 67.2 | 60.8** | 89.7 | 50.0 | 42.1 | 3.8 | 78.4 | 30.7 | 29.3 | 6.1** |
| Income | ||||||||||||
| Lowest | 89.9 | 66.1 | 60.6 | 48.2 | 86.1 | 41.9 | 35.0 | 4.0 | 76.5 | 25.9 | 23.8 | 3.0 |
| Middle | 90.6 | 66.9 | 64.3 | 55.9 | 88.3 | 45.8 | 36.9 | 3.1 | 78.9 | 26.9 | 23.8 | 3.1 |
| Highest | 91.9 | 66.5 | 64.0 | 58.2** | 88.2 | 51.1* | 43.0* | 4.7 | 79.3 | 30.9 | 29.1 | 3.7 |
| Occupation | ||||||||||||
| A | 91.9 | 65.8 | 63.7 | 59.5 | 88.3 | 46.3 | 39.2 | 3.4 | 78.3 | 27.9 | 24.9 | 3.1 |
| B | 88.8 | 67.4 | 64.3 | 53.7 | 87.2 | 54.4 | 43.9 | 3.8 | 80.3 | 24.0 | 22.7 | 2.9 |
| C | 90.3 | 68.2 | 63.4 | 48.1** | 85.9 | 44.7* | 36.3 | 4.3 | 78.0 | 29.4 | 27.5 | 4.2 |
| Overall | 90.8 | 67.0 | 63.6 | 53.9 | 87.1 | 46.7 | 38.6 | 3.8 | 78.4 | 28.0 | 25.7 | 3.5 |
A, professionals/clerks; B, business owners/merchants; C, unskilled workers/homemakers.
*P < 0.05; **P < 0.01.
Differences by socioeconomic factors
Table 3 shows the age, and sex-adjusted odds ratios for risk factors and for being aware, treated and controlled according to several sociodemographic factors. Hypercholesterolemia was slightly more frequent among the more educated patients, awareness and treatment of hypercholesterolemia were associated with household income, the control of hypertension was related to education, household income and occupation; treatment and control of diabetes mellitus were related to household income and education, respectively. Multivariate analysis showed that education was the strongest associated factor for control of hypertension and diabetes mellitus.
Table 3.
Odds ratio of prevalence, awareness, treatment and control of risk factors with SES in patients with history of stroke or transient ischemic attack
| Prevalence | Awareness | Treatment | Control | |
|---|---|---|---|---|
| Hypertension | ||||
| Educationa | ||||
| 2 versus 1 | 0.669 (0.438, 1.022) | 0.996 (0.804, 1.235) | 1.062 (0.859, 1.312) | 1.519 (1.240, 1.862) |
| 3 versus 1 | 0.806 (0.587, 1.108) | 1.140 (0.865, 1.501) | 1.286 (0.980, 1.689) | 1.877 (1.447, 2.436) |
| Incomeb | ||||
| 2 versus 1 | 1.087 (0.760, 1.555) | 1.066 (0.842, 1.351) | 1.203 (0.953, 1.519) | 1.359 (1.087, 1.700) |
| 3 versus 1 | 1.286 (0.885, 1.868) | 1.053 (0.831, 1.334) | 1.194 (0.945, 1.508) | 1.482 (1.183, 1.856) |
| Occupationc | ||||
| 2 versus 1 | 0.669 (0.438, 1.022) | 1.061 (0.792, 1.421) | 1.004 (0.751, 1.341) | 0.800 (0.607, 1.054) |
| 3 versus 1 | 0.806 (0.587, 1.108) | 1.102 (0.901, 1.348) | 0.965 (0.791, 1.177) | 0.630 (0.520, 0.762) |
| Hypercholesterolemia | ||||
| Educationa | ||||
| 2 versus 1 | 1.380 (1.048, 1.818) | 1.105 (0.882, 1.385) | 1.045 (0.828, 1.318) | 1.009 (0.590, 1.725) |
| 3 versus 1 | 1.710 (1.172, 2.494) | 1.276 (0.961, 1.695) | 1.255 (0.938, 1.678) | 0.890 (0.443, 1.787) |
| Incomeb | ||||
| 2 versus 1 | 1.204 (0.878, 1.651) | 1.173 (0.915, 1.503) | 1.102 (0.853, 1.424) | 0.805 (0.436, 1.486) |
| 3 versus 1 | 1.210 (0.880, 1.664) | 1.464 (1.141, 1.879) | 1.422 (1.101, 1.837) | 1.239 (0.705, 2.177) |
| Occupationc | ||||
| 2 versus 1 | 0.873 (0.592, 1.287) | 1.372 (1.014, 1.856) | 1.185 (0.873, 1.610) | 1.155 (0.556, 2.397) |
| 3 versus 1 | 0.795 (0.608, 1.040) | 0.939 (0.760, 1.159) | 0.880 (0.708, 1.094) | 1.281 (0.774, 2.119) |
| Diabetes mellitus | ||||
| Educationa | ||||
| 2 versus 1 | 1.052 (0.833, 1.328) | 1.088 (0.820, 1.444) | 1.023 (0.764, 1.371) | 1.580 (0.642, 3.890) |
| 3 versus 1 | 1.031 (0.767, 1.386) | 1.261 (0.923, 1.721) | 1.275 (0.926, 1.755) | 3.620 (1.478, 8.865) |
| Incomeb | ||||
| 2 versus 1 | 1.175 (0.911, 1.516) | 1.039 (0.796, 1.357) | 0.979 (0.742, 1.291) | 1.234 (0.636, 2.395) |
| 3 versus 1 | 1.150 (0.890, 1.485) | 1.291 (0.985, 1.693) | 1.324 (1.002, 1.750) | 1.300 (0.660, 2.562) |
| Occupationc | ||||
| 2 versus 1 | 1.117 (0.809, 1.543) | 0.784 (0.559, 1.100) | 0.846 (0.598, 1.198) | 0.934 (0.397, 2.198) |
| 3 versus 1 | 0.981 (0.790, 1.220) | 1.066 (0.849, 1.338) | 1.124 (0.889, 1.422) | 1.400 (0.806, 2.432) |
All odds ratio were adjusted by sex and age.
aEducation: 1, ≤6 years; 2, 6–12; 3, >12 years.
bIncome: 1, lowest trisection; 2, middle trisection; 3, highest trisection.
cOccupation: 1, professionals/clerks; 2, business owners/merchants; 3, unskilled workers/homemakers.
Effect of education on control of risk factors and health behaviors
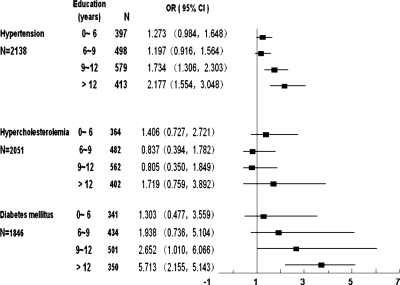
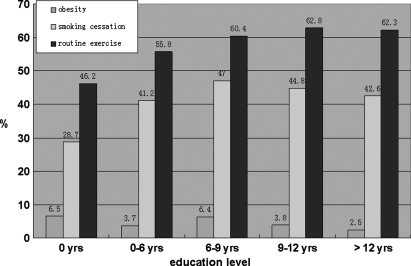
After being adjusted for sex and age, strong and graduated relationship were noted between level of education and control of risk factors, with the odds ratios increasing at every increment, so that individuals educated for more than 12 years had an odds ratio of 2.177 (95% CI 1.554–3.048) for control of hypertension and 5.713 (95% CI 2.155–5.143) for control of diabetes mellitus (Fig. 1). No statistical relationship can be observed between education and control of hypercholesterolemia. Figure 2 shows that the prevalence of obesity, smoking cessation and routine exercise increased with education levels (P < 0.05); people educated more than 6 years had a higher rate of smoking cessation than less educated people although the current smoking rate showed no significant difference among groups with diverse education level.
Figure 1.
Association of education levels with control of risk factors after adjustment for age and sex.
Figure 2.
Prevalence of obesity, smoking cessation and routine exercise by education level.
Discussion
Despite recent declines in mortality, cardiovascular diseases (including stroke) are the leading cause of death in many areas today. Although many of the major risk factors for stroke/ischemic attack have been identified, other different modifiable factors that may influence cardiovascular diseases still remain to be explored. SES may provide a new focus. There is a considerable body of evidence for a relationship between socioeconomic factors and all causes of mortality [7]. These findings have been replicated repeatedly over 80 years across measures of socioeconomic level and in geographically diverse populations [8], Cardiovascular disease studies have shown that lower levels of education are associated with hypertension [9], cigarette smoking [10] and high cholesterol [9], as well as with cardiovascular morbidity and mortality [11].
This study provides data on the prevalence, treatment, awareness and control of cardiovascular risk factors among stroke patients. Furthermore, data are given on sociodemographic differences in the prevalence, treatment, and control of risk factors. In the study of 2354 outpatients with a stroke history from 16 practices in primary care, we found low rates of control of stroke risk factors: only 3.2% of men and 4.3% of women had fasting glucose less than 126 mg/dl, 3.8% of men and 3.9% of women had normal serum cholesterol (less than 240 mg/dl) and 54.3% of men and 53.2% of women had normal blood pressure. Control rates of hypertension and diabetes mellitus increased with education level; Insignificant effect of education on the control rate of hypercholesterolemia, possibly due to insufficient public health education on cholesterol management [12].
On the basis of our findings, education may be the most important SES measure for use in secondary prevention of stroke. Control rates of hypertension and diabetes increased gradually with the educational level. Several different mechanisms through which education may positively influence health have been proposed [13]. Some have suggested that higher education may improve health by conferring economic advantages, but in this study we cannot find any significant association between education and income or between income and risk factor control, and so we can draw the same conclusion as that of Winkleby et al. [13] that higher education, rather than income or occupation, may be the strongest and most consistent predictor of good health.
One hypothesis we find most plausible is that education may protect against disease by influencing lifestyle behaviors, problem-solving abilities and values [14, 15]. Moreover, education may facilitate the acquisition of positive social, psychological, and economic skills and assets, and may provide insulation from adverse influences [16]. Such skills and assets that may accompany higher educational attainment include positive attitudes about health, access to preventive health services [17–19], membership in peer groups that promote the adoption or continuation of positive health behaviors, and higher self-esteem and self-efficacy [20, 21]. In our study, health behaviors are indicated by rates of smoking cessation and routine exercise, which increased with the education level, whereas the rate of obesity was inversely associated with education level. Moreover, this study also demonstrated a beneficial effect of awareness and control in people who had occupations that were professional or clerical. Our finding that household income affects the treatment and control of hypertension and hypercholesterolemia can be partially explained by the insufficiency of medical supplies currently in China; about 30% patients had no insurance for medicine.
Among stroke patients in our study, only 53.9% of hypertensive, 3.8% of those with hypercholesterolemia and 3.5% of those with diabetes have controlled their risk factors. To achieve better control of these risk factors and further reduction of the recurrence of stroke, more attention should be given to the detection and subsequent treatment and control of these established cardiovascular risk factors.
Our current findings have important public health implications, which have been noted by Goldman et al [22]. If medical science continues to bring forth effective but complicated drug regimens, this may exacerbate health outcome disparities across patients with different levels of education unless we recognize that not all patients are equally adept at adherence. Research aimed at encouraging patients with low education level to better adhere to currently available treatments might be effective in improving the health of the millions of people with chronic disease. Since education does not usually change (as occupation or income might) after young adulthood, the successful intervention to reduce the increased cardiovascular disease risk will have to ensure that the targeted audience is involved in developing and implementing the education program, and explore new and appropriate techniques and methods to deliver more effective messages.
Findings in the current study must be considered within the context of the study's limitations. First, the prevalence of CVD may be underestimated because the study sample focused on stroke survivors and did not include patients who died within 1 year of the stroke attack. Secondly, as all research centers were located in urban areas of northern China, more comprehensive research needs to be achieved to reflect the general status of secondary prevention of stroke in China.
In conclusion, the prevalence rates of hypertension, hypercholesterolemia and diabetes mellitus were higher among stroke patients. A substantial proportion of hypertensive persons are aware of and are successfully treated for hypertension. However, a still considerable proportion of persons with hypercholesterolemia and diabetes mellitus do not have their targeted disease well controlled. Education exerts the most important effect on the control of these factors; successful intervention to reduce established risk factors will have to be broad based, addressing not just specific cardiovascular risk factors but also the societal conditions that lead to the adoption and maintenance of high-risk behaviors. These stroke patients require more appropriate techniques and methods for the delivery of more effective messages by medical practitioners to reduce the burden of cardiovascular diseases.
Funding
Funding to pay the Open Access publication charges for this article was provided by Beijing Shijingshan Hospital.
References
- 1.Writing Group Members; Rosamond W, Flegal K, Furie K, et al. Committee ftAHAS, Stroke Statistics Subcommittee. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 2.Touboul P-J, Elbaz A, Koller C, et al. Investigators ftG. Common carotid artery intima-media thickness and brain infarction: the etude du profil genetique de l'infarctus cerebral (genic) case-control study. Circulation. 2000;102:313–8. doi: 10.1161/01.cir.102.3.313. [DOI] [PubMed] [Google Scholar]
- 3.Arima H, Tzourio C, Butcher K, et al. for the PROGRESS Collaborative Group. Prior events predict cerebrovascular and coronary outcomes in the progress trial. Stroke. 2006;37:1497–502. doi: 10.1161/01.STR.0000221212.36860.c9. [DOI] [PubMed] [Google Scholar]
- 4.Touze E, Varenne O, Chatellier G, et al. Risk of myocardial infarction and vascular death after transient ischemic attack and ischemic stroke: a systematic review and meta-analysis. Stroke. 2005;36:2748–55. doi: 10.1161/01.STR.0000190118.02275.33. [DOI] [PubMed] [Google Scholar]
- 5.Beaglehole R, Magnus P. The search for new risk factors for coronary heart disease: occupational therapy for epidemiologists? Int J Epidemiol. 2002;31:1117–22. doi: 10.1093/ije/31.6.1117. [DOI] [PubMed] [Google Scholar]
- 6.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART Study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 7.Raine R, Wong W, Ambler G, et al. Sociodemographic variations in the contribution of secondary drug prevention to stroke survival at middle and older ages: Cohort study. BMJ. 2009;338:b1279. doi: 10.1136/bmj.b1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaplan G, Keil J. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–98. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 9.Matthews KA, Kelsey SF, Meilahn EN, et al. Educational attainment and behavioral and biologic risk factors for coronary heart disease in middle-aged women. Am J Epidemiol. 1989;129:1132–44. doi: 10.1093/oxfordjournals.aje.a115235. [DOI] [PubMed] [Google Scholar]
- 10.Wagenknecht L, Perkins L, Cutter G, et al. Cigarette smoking behavior is strongly related to educational status: the CARDIA Study. Prev Med. 1990;19:158–69. doi: 10.1016/0091-7435(90)90017-e. [DOI] [PubMed] [Google Scholar]
- 11.Jacobsen BK, Thelle DS. Risk factors for coronary heart disease and level of education: The Tromso Heart Study. Am J Epidemiol. 1988;127:923–32. doi: 10.1093/oxfordjournals.aje.a114895. [DOI] [PubMed] [Google Scholar]
- 12.Goldman RE, Parker DR, Eaton CB, et al. Patients' perceptions of cholesterol, cardiovascular disease risk, and risk communication strategies. Ann Fam Med. 2006;4:205–12. doi: 10.1370/afm.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winkleby MA, Jatulis DE, Frank E, et al. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82:816–20. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Connor M, Bower J, Cho H, et al. To assess, to control, to exclude: effects of biobehavioral factors on circulating inflammatory markers. Brain Behav Immun. 2009;23:887–97. doi: 10.1016/j.bbi.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barakat K, Stevenson S, Wilkinson P, et al. Socioeconomic differentials in recurrent ischaemia and mortality after acute myocardial infarction. Heart. 2001;85:390–4. doi: 10.1136/heart.85.4.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Winkleby M, Fortmann S, Barrett D. Social class disparities in risk factors for disease: eight-year prevalence patterns by level of education. Prev Med. 1990;19:1–12. doi: 10.1016/0091-7435(90)90001-z. [DOI] [PubMed] [Google Scholar]
- 17.Metcalf PA, Scragg RR, Schaaf D, et al. Comparison of different markers of socioeconomic status with cardiovascular disease and diabetes risk factors in the diabetes, heart and health survey. N Z Med J. 2008;121:45–56. [PubMed] [Google Scholar]
- 18.Kanjilal S, Gregg EW, Cheng YJ, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch Intern Med. 2006;166:2348–55. doi: 10.1001/archinte.166.21.2348. [DOI] [PubMed] [Google Scholar]
- 19.Sodjinou R, Agueh V, Fayomi B, et al. Obesity and cardio-metabolic risk factors in urban adults of Benin: relationship with socio-economic status, urbanisation, and lifestyle patterns. BMC Public Health. 2008;8:84. doi: 10.1186/1471-2458-8-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clark AM, DesMeules M, Luo W, et al. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6:712–22. doi: 10.1038/nrcardio.2009.163. [DOI] [PubMed] [Google Scholar]
- 21.Zeljko H, Skaric-Juric T, Narancic NS, et al. Traditional CVD risk factors and socio-economic deprivation in Roma minority population of Croatia. Coll Antropol. 2008;32:667–76. [PubMed] [Google Scholar]
- 22.Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? PNAS. 2002;99:10929–34. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]