Abstract
Background
Hashimoto’s thyroiditis (HT) is an organ –specific autoimmune disease characterized by production of antibodies such as anti-thyroperoxidase (TPO), which leads to destruction of the thyroid gland and a decrease in normal thyroid function. Thyroidectomy is not generally recommended because the dense inflammatory process that surrounds the thyroid gland can make resection more difficult. However, patients with HT are considered for surgery if they experience persistent symptoms after conservative therapy. We hypothesized that patients with HT and significant compressive and other associated symptoms may benefit from thyroidectomy for palliation.
Methods
We identified 1791 patients who underwent thyroidectomy from May 1994 to December 2009. Of those 1791 patients, 311 were diagnosed with HT. Of these 311 patients, 133 had 170 significant preoperative symptoms, and served as our sample population. Patients were subjectively evaluated for improvement or relief of symptoms postoperatively.
Results
The mean age of the group was 46 ± 1 year and 90% were female. Patients underwent lobectomy (33%), subtotal thyroidectomy (6%), or total thyroidectomy (61%). The overall rate of symptomatic improvement for HT patients was 90% after thyroidectomy. The most frequent preoperative symptom was compression, and >93% of patients experienced relief. In addition, we found high rates of improvement for HT patients with other preoperative symptoms including voice problems (77%), hormone imbalance (84%) and other (90%).
Conclusion
The overwhelming majority of HT patients with significant symptoms appear to benefit from thyroidectomy. Therefore, HT patients should consider pursing surgery for palliation if they suffer from persistent symptoms after conservative therapy.
Keywords: Hashimoto’s Thyroiditis, Thyroidectomy
Introduction
Hashimoto’s thyroiditis (HT) is an organ-specific autoimmune disease originally described in 1912 and is defined by specific characteristics. Known to occur more frequently in women, HT is the most common cause of hypothyroidism and diffuse goiter in the United States1–4. The histological appearance of the thyroid gland in HT is characterized by diffuse lymphocyte infiltration, a reduction in size of follicular cells, and fibrosis4–7. The presence of anti-thyroid antibodies, including anti-thyroglobulin (TG) and anti-thyroperoxidase (TPO), in HT patients causes destruction of the thyroid gland and can lead to a decrease in normal thyroid function4,8–10.
Many patients with HT are asymptomatic11,12 but the disease can also lead to a wide variety of clinical symptoms. For example, patients can be hypothyroid, euthyroid, hyperthyroid or fluctuate between periods of hyperthyroidism and periods of hypothyroidism, making it very difficult for patients to control hormonal levels1,7. Other symptoms include pressure, dysphagia, dyspnea, neck pain, and hoarseness1,11,13.
Treatment for patients with HT is usually conservative6,14. Thyroidectomy is not usually recommended for HT patients because the dense inflammatory process that surrounds the thyroid gland makes surgical resection more difficult11. However, there are instances in which medical treatment with levothyroxine (L-T4) is not effective and the patient continues to suffer symptoms. Generally, the indications for surgery in HT patients include suspicion of malignancy, persistent symptoms associated with the disease, or a goiter that is increasing in size1,11,13,15. While some studies identify and confirm the indications for surgery in HT patients1,12, thyroidectomy is still a controversial method of treatment. The purpose of this study was to identify HT patients with persistent preoperative symptoms despite palliative care and subjectively identify the frequency of improvement after thyroidectomy. We hypothesized that patients with HT and significant compressive and other associated symptoms may benefit from thyroidectomy for palliation.
Methods
We retrospectively reviewed data from the University of Wisconsin Thyroid Surgery Database. 1791 patients underwent thyroidectomy at the University of Wisconsin from May 1994 to December 2009. Of those 1791 patients, we identified 311 patients with HT based on histological analysis of the thyroid tissue.
In their preoperative visit, patients were subjectively evaluated for symptoms including compression, voice problems, hormone imbalance, and other. Patients were categorized according to the following: symptoms of dysphagia and/or dyspnea were categorized as compression symptoms and hoarseness was categorized as a voice problem. For patients with hyperthyroidism or fluctuations in thyroid hormone levels that lead to alternating symptoms of hyperthyroidism and hypothyroidism, they were categorized as having a hormone imbalance. Also, if patients experienced neck discomfort, pain, or pressure they were placed into the category for other symptoms. In the group of 311 patients with HT, 133 had 170 persistent preoperative symptoms, and served as our sample population. The following data were collected: age, gender, type of operation, and any postoperative complications. Patients were subjectively evaluated after thyroidectomy and the number of patients who reported improvement or relief of preoperative symptoms after surgery was documented. Patient data collection and analysis were approved through the University of Wisconsin Human Subjects and Institutional Review board.
Results
In analyzing the demographics of the patients with symptomatic HT, the mean age was 46 ± 1 years (mean ± SEM) and 90% of the patients were female. Operations performed included thyroid lobectomy (33%), subtotal thyroidectomy (6%) or total thyroidectomy (61%). Out of the 170 symptoms that were reported, compression was the most common followed by as voice problems, hormone imbalance, and others (Table 1).
Table 1.
Pre-operative symptoms in patients with HT
| Symptom | N | Frequency |
|---|---|---|
| Compression | 107 | 63% |
| Voice Problems | 22 | 13% |
| Hormone Imbalance | 19 | 11% |
| Other | 22 | 13% |
Overall, we found that 153 (90%) of the 170 symptoms improved or resolved after thyroid surgery. Specifically, we identified symptomatic improvement in the majority of the patients who experienced compression, voice problems, hormone imbalance, and other symptoms (Table 2). There were 7 patients who were lost to follow up (5 with compressive symptoms and 2 with voice problems).
Table 2.
Results after thyroidectomy in patients with HT.
| Symptom | N | Number Improved | % Improvement |
|---|---|---|---|
| Compression | 107 | 100 | 94% |
| Voice Problems | 22 | 17 | 77% |
| Hormone Imbalance | 19 | 16 | 84% |
| Other | 22 | 20 | 91% |
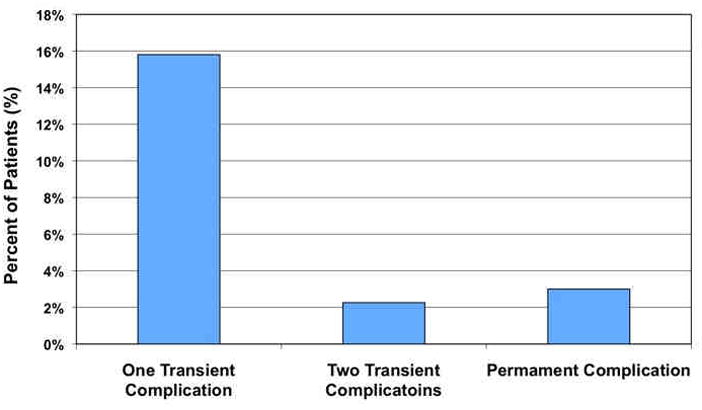
In looking at postoperative complications, we focused on the 2 most common: hypoparathyroidism or hoarseness due to recurrent laryngeal nerve injury. Of the 133 patients, 28 (21%) patients experienced postoperative complications, including 3 patients who had multiple complications. 21 patients (16%) experienced one transient complication, 3 patients (2%) experienced two transient complications, and 4 patients (3.0%) experienced one permanent complication (Figure 1). Furthermore, 2 of the patients who experienced one transient complication did not experience relief of preoperative symptoms after surgery. The other 26 patients (19 who experienced one transient complication, 3 who experienced two transient complications and all 4 patients who experienced a permanent complication) did report improvement of their preoperative symptoms after surgery.
Figure 1.
Discussion
Patients with HT are treated depending on the particular symptoms they present with. In the case of an enlarged goiter, HT patients are treated with suppressive levothyroxine in an attempt to decrease goiter size. Also, if patients present with hypothyroidism or hyperthyroidism, they are placed on hormone therapy to relieve symptoms and return to a euthyroid state1,13. However, in cases in which the patient does not respond to conservative treatment, or they fluctuate between a hyperthyroid state and a hypothyroid state and cannot consistently control their hormone levels, they must seek out other options to relieve their symptoms. Thyroidectomy is considered for patients with compressive symptoms, such as dysphagia and dyspnea, which may result from an enlarged goiter pressing on the trachea and esophagus13. For patients who fluctuate between symptoms of hypothyroidism and hyperthyroidism, thyroidectomy would be beneficial because patients would no longer move into a hyperthyroid state and would only need supplemental hormone replacement. Additionally, when other symptoms including hoarseness, pressure, neck pain and neck discomfort are present, thyroidectomy can be considered.
Thomas et al. conducted a study to determine reliable criteria for surgery in patients with HT. Out of the 260 patients who underwent thyroidectomy in their study, 11 patients were diagnosed with HT, including 4 patients with an associated diagnosis. The indications for surgery in the seven patients without an associated diagnosis included hyperthyroidism, oppressive goiter, residual mass, dominant “cold nodule,” and enlarged thyroid with a malignant neoplasm. The authors concluded indications for thyroidectomy for patients with HT including 1) dominant mass that is unresponsive to suppressive therapy; 2) enlarging goiter despite suppressive therapy; 3) findings that suggest malignancy; 4) indeterminate needle biopsy. While the authors did establish definitive criteria for thyroidectomy in patients with HT, they did not evaluate patients after thyroidectomy regarding the status of their preoperative symptoms or any complications from the surgery. Furthermore, this study was limited to a small sample size.
Shimizu, et al. performed a study in which they identified surgical indications for patients with HT and discussed subtotal thyroidectomy as the safest surgical procedure for these patients. This study included 8 patients with a diffusely enlarged goiter and a diagnosis of HT who underwent subtotal thyroidectomy. Preoperatively, patients experienced choking due to compression, unsightly appearance, dyspnea, dysphagia, hoarseness, and no malignancy. After surgery, all patients reported improvement of their preoperative symptoms. Also, none of the patients experienced complications, which the authors attributed to the safe nature of the subtotal thyroidectomy procedure. The authors concluded that patients should be considered for thyroidectomy for HT in cases in which 1) the patient experiences compression symptoms despite suppressive therapy; 2) conservative therapy is ineffective for improvement cosmetically. While this study did follow up patients postoperatively to evaluate the status of preoperative symptoms, it was limited to a very small sample size.
The purpose of this study was to identify any preoperative symptoms reported by patients with HT who underwent thyroidectomy and evaluate whether those symptoms improved postoperatively. We identified the most common symptom among HT patients to be compression, at a frequency of 63%, and >93% of those patients experienced postoperative relief. In addition, we found that the majority of patients with other symptoms also experienced relief after thyroidectomy. Although 21% of patients suffered from postoperative complications, 18% were transient complications and resolved within 6 months or less. Therefore, an overwhelming majority of symptomatic HT patients experienced benefit from thyroidectomy.
While we feel that our study reflects the benefits of thyroidectomy for HT patients with persistent symptoms, we recognize the limitations to our study. First, all symptoms were subjectively reported by the patient. Also, in some cases in which patients did not experience improvement in their symptoms after thyroidectomy, it was difficult to determine if their symptoms were a direct result of their HT disease or if there was another cause. To our knowledge, there are no validate tools to measure many of these thyroid-related symptoms. However, we are in the process of developing potential methods to objectively assess symptomatic changes after thyroidectomy.
Surgical intervention is not the most common method of treatment for patients with HT. However, thyroidectomy must be considered in specific cases. The indications for surgery in HT patients that we found in our study was consistent with other published literature1,11–13. In our patient population, a majority of patients no longer reported symptoms after thyroidectomy. Also, for 21 of the 26 patients who experienced relief of symptoms at the cost of a postoperative complication, surgery served as a long term benefit once the complication resolved. The remaining 4 patients experienced relief of symptoms but at the cost of a permanent complication. For the 2 patients who did not experience relief of preoperative symptoms and suffered from a postoperative complication, their complication was transient and resolved within 6 months.
The possibility of a complication occurring, particularly a permanent complication as with 4 patients in our study, emphasizes the necessity for surgery to be considered on a case-by-case basis. In this study, the majority of patients with HT and significant symptoms reported improvement or relief of preoperative symptoms after thyroidectomy. Therefore, HT patients should consider pursing surgery for palliation if they suffer from persistent symptoms after conservative therapy.
Acknowledgments
National Institute of Health (NIH) T32 DC009401 Training Grant
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Thomas CG, Rutledge RG. Surgical intervention in chronic (Hashimoto’s) Thyroiditis. Ann Surg. 1981;193:769–776. doi: 10.1097/00000658-198106000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Repplinger D, Bargren A, Zhang Y, Adler J, Haymart M, Chen H. Is Hashimoto’s thyroiditis a risk factor for papillary thyroid cancer? J Surg Res. 2008;150:49–52. doi: 10.1016/j.jss.2007.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma AK, Paliwal RK, Pendse AK. Hashimoto’s thyroiditis—a clinical review. J Postgrad Med. 1990;36(2):87–90. [PubMed] [Google Scholar]
- 4.Gasbarri A, Sciacchitano S, Marasco A, Papotti M, et al. Detection and molecular characterization of thyroid cancer precursor lesions in a specific subset of Hashimoto’s thyroiditis. British J of Cancer. 2004;91:1096–1104. doi: 10.1038/sj.bjc.6602097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LiVolsi VA. The pathology of autoimmune thyroid disease: a review. Thyroid. 1994;4(3):333–9. doi: 10.1089/thy.1994.4.333. [DOI] [PubMed] [Google Scholar]
- 6.Cipolla C, Sandonato L, Graceffa G. Hashimoto thyroiditis coexistent with papillary thyroid carcinoma. Am Surg. 2005;71:874–8. [PubMed] [Google Scholar]
- 7.Zaletel K. Determinants of thyroid autoantibody production in Hashimoto’s thyroiditis. Exp Rev of Clin Immunol. 2007;3(2):217–23. doi: 10.1586/1744666X.3.2.217. [DOI] [PubMed] [Google Scholar]
- 8.Beobachtungen K. Indication of operation in various forms of Hashimoto’s thyroiditis. Clinical observations. Munch Med Wochenschr. 1975;117(13):543–6. [PubMed] [Google Scholar]
- 9.Kasagi K, Kousaka T, Higuchi K, et al. Clinical significance of measurements of antithyroid antibodies in the diagnosis of Hashimoto’s thyroiditis: comparison with histological findings. Thyroid. 1996;6(5):445–50. doi: 10.1089/thy.1996.6.445. [DOI] [PubMed] [Google Scholar]
- 10.Stoll SJ, Pitt SC, Liu J, Schaefer S, Sippel RS, Chen H. Thyroid hormone replacement after thyroid lobectomy. Surgery. 2009;146(4):558–60. doi: 10.1016/j.surg.2009.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shih ML, Lee JA, Hsieh CB, et al. Thyroidectomy for Hashimoto’s thyroiditis: complications and associated cancers. Thyroid. 2008;18(7):729–34. doi: 10.1089/thy.2007.0384. [DOI] [PubMed] [Google Scholar]
- 12.Shimizu K, Nakajima Y, Kitagawa W, Akasu H, et al. Surgical therapy in Hashimoto’s thyroiditis. J Nippon Med Sch. 2003;70(1):34–9. doi: 10.1272/jnms.70.34. [DOI] [PubMed] [Google Scholar]
- 13.Tajiri J. Radioactive iodine therapy for goitrous Hashimoto’s thyroiditis. J Clin Endocrinol Metab. 2006;91(11):4497–500. doi: 10.1210/jc.2006-1163. [DOI] [PubMed] [Google Scholar]
- 14.Gyory F, Lukacs G, Juhasz F, et al. Surgically treated Hashimoto’s thyroiditis. Acta Chir Hung. 1999;38(3–4):243–7. [PubMed] [Google Scholar]
- 15.Haymart MR, Repplinger DJ, Leverson GE, Elson DF, Sippel RS, Jaume JC, Chen H. Higher Serum TSH Level in Thyroid Nodule Patients is Associated with Greater Risks of Differentiated Thyroid Cancer and Advanced Tumor Stage. Journal of Clinical Endocrinology and Metabolism. 2008;93:809–14. doi: 10.1210/jc.2007-2215. [DOI] [PMC free article] [PubMed] [Google Scholar]


