Abstract
Background
Health-related quality of life instruments (HRQoL) are widely used to produce measures that summarize population health and to inform decision-making and health policy. Although the literature about the relationship between health and race in the United States is quite extensive, there is a lack of studies that comprehensively examine the relationship between race and preference-based HRQoL. Given the widespread use of these measures, it becomes important to understand the extent of the race differences in HRQoL scores and factors associated with any such differences.
Methods
We examined the differences in HRQoL, between blacks and whites and associated factors, using the summary scores of the SF-6D, EQ-5D, QWB-SA, HUI2, HUI3, administered by telephone to a nationally representative sample of 3,578 black and white US adults between the ages of 35 and 89 in the National Health Measurement Study (NHMS).
Results
Black women had substantially lower HRQoL than white women. The difference was largely explained by sociodemographic and socioeconomic variables. Black men did not differ significantly from white men, except for the EQ-5D. HRQoL among black men was higher at higher income levels, while the HRQoL of black women was especially low compared to other groups at high income levels.
Keywords: NHMS, Race, HRQoL, SF-6D, EQ-5D, QWB, HUI2, HUI3
Introduction
Race differences in health have been extensively documented in the literature, and for the most part, studies show that African Americans or blacks have worse health outcomes than whites in the United States [1–3]. The majority of studies that explored the relationship between race and health used outcomes such as self-rated health, mortality or morbidity, and disability [1]. A smaller portion of the literature on race and health utilized Health-Related Quality of Life (HRQoL) measures. Among such studies, there is variation in which HRQoL measures and groups or subgroups were investigated. For example, blacks were shown to have lower HRQoL with cystic fibrosis on a disease-specific measure [4] and much lower generic HRQoL scores with coronary heart disease [5]. Fewer studies investigated population level race differences in generic preference-based HRQoL indexes and their domains [6–8]. The evidence from such studies is mixed, and results depend on what control variables were included. Without adjustments, blacks had higher HRQoL scores than whites in some studies [7] and lower in others [6, 8].
Generic preference-based HRQoL indexes differ from other health measures by summarizing multiple dimensions or domains of health into a single score by using preference weights derived from evaluations of health states by community samples. These measures are further used to compute quality adjusted life years (QALYs) that incorporate both quality of life and longevity to inform economic evaluation, such as cost-utility analyses of health interventions. Among the most commonly used such measures are the EuroQol EQ-5D (EQ-5D) [9, 10], Health Utilities Index Mark 2 (HUI2) [11] and Mark 3 (HUI3) [12], Quality of Well-Being Scale (QWB-SA) [13] and SF-6D, which is computed from the SF-36v2™ [14] or the SF-12v2™ [15]. Although these instruments aim to measure the same construct, there are important differences in how this is accomplished, and it has been widely shown that different indexes can yield widely different assessments [16].
Research has shown that once differences in socioeconomic status (SES) are taken into account, the disparities between blacks and whites tend to be reduced and in some cases, disappear [2]. Nevertheless, there is still evidence that SES differences may not explain all the health disparities that exist between race groups in the United States [1, 17].
This paper has two goals. First, as an addition to the existing literature on racial health disparities, we assess whether there are significant population level race differences in HRQoL as measured by the above five preference-based indexes, self-reported health and number of self-reported diagnosed chronic conditions. In this context, we also examine the influence of gender and socioeconomic factor on race difference in HRQoL. Second, we assess whether there is agreement in the results informed by different measures. Identifying, understanding, and eliminating health disparities is a major national goal, and it can be expected that preference-based indexes will play a major role in assessing disparities and in evaluating efforts to reduce them.
Methods
Data and sample information
The analyses are based on data from the National Health Measurement Study—NHMS [18]. The NHMS is a random-digit-dialed telephone survey conducted in 2005/2006 of a nationally representative sample of 3,844 non-institutionalized US adults in the 48 contiguous states. Individuals aged 35–89 were included. The estimated response rate was 56%. Telephone exchanges with high percentages of African Americans were over-sampled, as were individuals older than 65. Our analyses include individuals who reported their race as white or black. Those reporting their race as Asian, Native American, American Indian, Alaskan Native, Native Hawaiian, Pacific Islander, other or not reporting their race were excluded. An additional 70 white or black individuals reporting themselves to be Hispanic or Latino were similarly excluded. This resulted in 3,578 individuals from NHMS being eligible for inclusion. The diversity among the 266 excluded individuals did not allow assessment of the relationship of their ethnicity or race with HRQoL.
As previously described [18], analytic survey weights are available for the NHMS based on sampling design and post-stratification by age, gender, and race. Due to the importance of socioeconomic level to the present investigation, these weights were further post-stratified to reflect the distribution of educational levels shown in Table 1 within race, gender, and age groups in the US population in 2005 (http://www.census.gov/population/www/socdemo/education/cps2005.html), while preserving the race, gender, and age distribution generated by the original weights. Weighted results of our analyses are generalizable to the non-Hispanic US non-institutionalized adult population aged 35–89 in the 48 contiguous states, self-reporting their race as white or black.
Table 1.
Characteristics of sample and underlying population
| White men | Black men | White women | Black women | |||||
|---|---|---|---|---|---|---|---|---|
| Sample | Pop.%a | Sample | Pop.%a | Sample | Pop.%a | Sample | Pop.%a | |
| N | 1,149 | 370 | 1,366 | 693 | ||||
| Age | ||||||||
| 35–44 | 163 | 27.0 | 78 | 38.0 | 209 | 31.0 | 126 | 43.0 |
| 45–64 | 465 | 43.8 | 154 | 44.3 | 511 | 45.7 | 281 | 38.1 |
| 65–89 | 521 | 29.2 | 138 | 17.7 | 646 | 23.2 | 286 | 19.0 |
| Marital status | ||||||||
| Single | 87 | 6.1 | 49 | 14.1 | 93 | 4.8 | 127 | 22.2 |
| Married/Partner | 841 | 80.2 | 218 | 61.6 | 629 | 73.0 | 145 | 38.6 |
| Div/sep/Widowed | 219 | 13.7 | 103 | 24.3 | 643 | 22.2 | 421 | 39.2 |
| Missing | 2 | 1 | ||||||
| Education | ||||||||
| <HS | 82 | 11.5 | 53 | 21.9 | 131 | 9.8 | 142 | 20.3 |
| HS | 315 | 32.2 | 120 | 39.3 | 437 | 34.3 | 220 | 34.9 |
| Some college | 225 | 24.1 | 83 | 23.0 | 323 | 28.1 | 167 | 26.2 |
| ≥College | 518 | 32.2 | 112 | 15.8 | 470 | 27.8 | 163 | 18.6 |
| Missing | 9 | 3 | 5 | 1 | ||||
| Income | ||||||||
| <$20 K | 107 | 10.9 | 96 | 26.9 | 247 | 12.0 | 263 | 41.1 |
| $20 ≤ $35 K | 179 | 14.9 | 69 | 24.2 | 268 | 17.6 | 132 | 15.9 |
| $35 ≤ $75 K | 435 | 40.1 | 121 | 35.1 | 404 | 35.0 | 151 | 26.3 |
| >$75 K | 368 | 34.1 | 63 | 13.8 | 304 | 35.4 | 73 | 16.7 |
| Missing | 60 | 21 | 143 | 74 | ||||
Weighted to US population age 35 within each group with missing values imputed
Variables
Dependent variables
The NHMS interview first asked the respondent to rate their health on the ordinal Excellent, Very Good, Good, Fair, Poor scale. Results presented here group this variable into Fair/Poor versus Good or better. Four HRQoL questionnaires were then administered in random order to each individual: EQ-5D, SF-36v2, HUI, and QWB-SA. Five indexes were computed from these according to the developers’ guidelines: SF-6D [15], EQ-5D [10], QWB-SA [13], HUI2 [11], and HUI3 [12]. These are preference-based generic HRQoL measures anchored on a cardinal scale by 0 (dead) and 1 (full health). The EQ-5D, HUI2 and HUI3 allow health states with utilities less than zero (worse than dead). The SF-6D index refers to health in the “past 4 weeks” and covers six health domains (physical function, role limitation, social function, pain, mental health, and vitality). The SF-6D index produces single summary utility scores ranging from 0.35 to 1.0. In this study, the SF-12v2™ version of SF-6D is used [15].
The EuroQoL EQ-5D refers to health “today” and incorporates five domains of health (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). This index produces summary utility scores that range from −0.11 to 1 [18]. US scoring is used in this study [10].
The HUI2 and HUI3 indexes refer to health “in the past week.” HUI2 has six domains (sensation, mobility, emotion, cognition, self-care, pain), and HUI3 has eight domains (vision, hearing, speech, ambulation, dexterity, emotion, cognition, pain) for which data are collected using the proprietary Health Utilities Index questionnaire [11, 12]. Summary utility scores range from −0.03 to 1.0 for HUI2 and from −0.36 to 1.0 for HUI3.
In addition to the 5 individual preference scores, we present results for a summary score obtained by first taking the mean of HUI2 and HUI3 scores, and then averaging this mean together with scores from the SF-6D, EQ-5D and QWB-SA.
The NHMS survey also inquired about chronic conditions. Questions were formulated as “Has a doctor or other health professional ever told you that you had…” with follow-up questions. The 11 conditions used in the present analysis were coronary heart disease, myocardial infarction, diabetes, arthritis, eye disease, sleep disorder, chronic respiratory, clinical depression or anxiety, ulcer, thyroid disorder, and back pain due to slipped disk. Results are presented grouping these conditions into greater than one (i.e. multiple conditions) versus one or zero.
Explanatory variables
Socioeconomic level is generally recognized to differ between blacks and whites, and also to be strongly related to health. We selected sociodemographic variables that were shown to be important in several previous publications using the National Health and Measurement Study [19, 20].
Demographics
Individuals self-reported race (black/white), gender (male/female), marital status and age in years. Age was classified into categories (35–44; 45–64; 65–89). Marital status was recoded into 3 categories: (a) single, or never married, (b) married or living with a partner, (c) divorced, widowed, or separated.
SES measures
Household income was reported in 8 categories, which were combined into less than $20,000, $20,000–$34,999, $35,000–$74,999, and $75,000 and above. Education was reported in years and categorized as less than high school, high school graduate, some college, college degree or higher.
Analytic strategy
Analyses were conducted using SAS/STAT 9.1, Copyright© 2002–2003 (SAS Institute Inc., Cary, NC).
As racial differences were dissimilar for men and women, all analyses focused on the four races by gender groups. There were missing values on marital status, education, and income as indicated in Table 1. In addition, there were individuals with missing scores on the HRQoL instruments: 95 for the SF-6D, 28 for EQ-5D, 159 for HUI2 and 149 for HUI3, and 2 individuals with missing self-reported health. We generated ten datasets, each with 3,578 complete cases, through multiple imputation, using SAS PROC MI separately for each race/gender group and including all analytic and design variables. The survey-weighted estimates and their robust standard errors were combined across the ten data sets following standard procedures [21]. Means and percentages, as appropriate, with corresponding confidence intervals are presented for race by gender subgroups, and means and percentages for race by gender by age subgroups. Differences and odds ratios between black and white men and between black and white women were estimated within each imputed data set by survey-weighted multiple and logistic regression unadjusted, adjusted for age group and adjusted for age group and all other sociodemographic variables.
In addition to the above analyses based on the multiple imputed data sets, overall effects and interaction effects of race/gender with age, marital status, education, and income categories were tested by weighted F-tests based on the first imputed data set. Guided by these tests, graphs are presented for the means (across imputations) of summary HRQoL, proportion reporting better than fair health and proportion reporting zero or one health condition by income and race/gender groups.
Finally, discrepancies between indexes in the estimated differences between race and gender groups were tested by a weighted robust F-test of the interaction between index indicators and the race by gender indicators in a joint age-adjusted regression model taking into account correlation between indexes within survey respondent.
Hypothesis test results were considered statistically significant when P < 0.05. Difference estimates were considered clinically significant at 0.033 or greater [22–25].
Results
Table 1 presents sample characteristics and those of the underlying population by race and gender subgroups. It is clear that both black men and black women are younger and have lower education levels and income than their white counterparts. Blacks are also less likely to be married or living with a partner, as are women within both races.
Table 2 presents mean HRQoL, and self-reported health and chronic conditions by gender and race. Black men have lower HRQoL than white men, and black women have lower mean scores than white women across all indexes. All indexes, except HUI2, as well as the percent reporting fair or poor health differ significantly between race/gender groups overall. It is clear, however, that racial differences in HRQoL are much larger among women than among men. On the other hand, self-reported health differs substantially between whites and blacks among both men and women. Although the percentage reporting more than one chronic condition do not differ significantly between groups, black men have the lowest percentage.
Table 2.
HRQoL and self-reported health status by race and gender, mean or percent with 95% confidence interval
| White men | Black men | White women | Black women | |
|---|---|---|---|---|
| SF-6D*** | 0.793 (0.781,0.805) | 0.773 (0.743,0.803) | 0.785 (0.774,0.79) | 0.722 (0.697,0.747) |
| EQ-5D*** | 0.871 (0.857,0.886) | 0.834 (0.798,0.870) | 0.867 (0.855,0.878) | 0.795 (0.768,0.823) |
| QWB-SA** | 0.666 (0.652,0.680) | 0.655 (0.617,0.692) | 0.647 (0.633,0.662) | 0.614 (0.589,0.639) |
| HUI2 | 0.849 (0.833,0.864) | 0.807 (0.763,0.851) | 0.833 (0.820,0.847) | 0.763 (0.698,0.827) |
| HUI3* | 0.797 (0.774,0.819) | 0.755 (0.701,0.810) | 0.800 (0.780,0.819) | 0.682 (0.603,0.762) |
| Summary HRQoL*** | 0.777 (0.765, 0.789) | 0.754 (0.722, 0.785) | 0.766 (0.756, 0.776) | 0.710 (0.688, 0.733) |
| % self-reporting Fair/poor health*** | 15.0 (11.8,18.3) | 22.5 (15.7,29.3) | 15.1 (12.2,18.1) | 30.7 (24.6,37.0) |
| % reporting >1 chronic condition | 43.0 (38.5,47.5) | 38.9 (30.4,47.3) | 41.3 (36.8,45.8) | 48.0 (41.0,55.0) |
P < 0.05 for difference between groups;
P < 0.01 for difference between groups;
P < 0.001 for difference between groups
Table 3 further displays mean HRQoL scores by race, gender, and age groups. Differences between groups, adjusted for age, remain statistically significant for all measures except HUI2. With few exceptions, blacks have lower scores than whites across all indexes and age groups, and have worse self-reported health. Differences between blacks and whites appear more pronounced within older age groups, but interaction effects between age and race/gender groups were statistically significant only for the SF-6D (P = 0.03) and QWB-SA (P = 0.005). Black women have the lowest HRQoL mean scores across all indexes and age groups, with few exceptions. Blacks also have the largest percentage reporting more than 1 chronic condition, except for black men age 65–89.
Table 3.
HRQoL and self-reported health status by race, gender and age, mean or percent
| Age | White men | Black men | White women | Black women | |
|---|---|---|---|---|---|
| SF-6D*** | 35–44a | 0.80 | 0.81 | 0.81 | 0.77 |
| 45–64 | 0.80 | 0.76 | 0.78 | 0.67 | |
| 65–89 | 0.78 | 0.72 | 0.75 | 0.70 | |
| EQ-5D*** | 35–44 | 0.90 | 0.89 | 0.90 | 0.85 |
| 45–64 | 0.87 | 0.81 | 0.86 | 0.75 | |
| 65–89 | 0.86 | 0.77 | 0.83 | 0.77 | |
| QWB-SA*** | 35–44b | 0.72 | 0.70 | 0.68 | 0.65 |
| 45–64 | 0.67 | 0.64 | 0.64 | 0.57 | |
| 65–89 | 0.61 | 0.59 | 0.61 | 0.62 | |
| HUI2 | 35–44 | 0.87 | 0.85 | 0.86 | 0.79 |
| 45–64 | 0.84 | 0.79 | 0.83 | 0.71 | |
| 65–89 | 0.84 | 0.78 | 0.81 | 0.82 | |
| HUI3* | 35–44 | 0.83 | 0.82 | 0.84 | 0.71 |
| 45–64 | 0.80 | 0.73 | 0.80 | 0.62 | |
| 65–89 | 0.76 | 0.68 | 0.75 | 0.75 | |
| Summary HRQoL*** | 35–44 | 0.81 | 0.80 | 0.80 | 0.76 |
| 45–64 | 0.78 | 0.74 | 0.76 | 0.66 | |
| 65–89 | 0.75 | 0.69 | 0.73 | 0.70 | |
| % self-reporting fair/poor health*** | 35–44 | 2.8 | 6.0 | 3.6 | 18 |
| 45–64 | 16 | 31 | 16 | 38 | |
| 65–89 | 24 | 37 | 28 | 45 | |
| % reporting >1 chronic condition* | 35–44 | 19 | 22 | 22 | 29 |
| 45–64 | 38 | 44 | 40 | 56 | |
| 65–89 | 73 | 63 | 69 | 74 |
P 0.05 for difference between groups adjusted for age;
P < 0.001
P < 0.05 for interaction between age and race/sex groups
P < 0.001 for interaction between age and race/sex groups
Although the indexes differ greatly in mean value (P < 0.0001), an overall test between the HRQoL indexes in how they capture race/gender differences was not statistically significant (P = 0.46).
Regression analyses focused on the difference between HRQoL, self-reported health and chronic conditions between blacks and whites among men and women. Table 4 shows these differences unadjusted, age adjusted and adjusted for marital status, education and income. After adjustment by age, the race differences increased for all indexes due to the younger age distribution of blacks in this sample. Although the estimated differences among men are of a magnitude indicating clinical significance for the HUI2, HUI3, and EQ-5D, they do not reach statistical significance, except for the EQ-5D with age adjustment. Black women differ from white women on all indexes with and without age adjustment.
Table 4.
Unadjusted and adjusted differences in mean HRQoL or odds ratio for fair/poor health or >1 reported health condition for black versus white men and black versus white women
| Group | Unadjusted | Adj. for age | Adj. for age and sociodemographics |
|
|---|---|---|---|---|
| SF-6 Da | Black versus white men | −0.020 (−0.052, 0.012) | −0.025 (−0.057,0.006) | 0.010 (−0.019, 0.039) |
| Black versus white women | −0.063 (−0.090, − 0.036) | −0.067 (−0.093, − 0.041) | −0.022 (−0.049, 0.006) | |
| EQ-5 Da | Black versus white men | −0.038 (−0.076, 0.001) | −0.045 (−0.082, − 0.007) | −0.007 (−0.044, 0.030) |
| Black versus white women | −0.071 (−0.100, −0.042) | −0.077 (−0.106, −0.048) | −0.028 (−0.062, 0.005) | |
| QWB-SAa | Black versus white men | −0.011 (−0.052, 0.029) | −0.021 (−0.060, 0.018) | 0.011 (−0.026, 0.049) |
| Black versus white women | −0.033 (−0.062, −0.004) | −0.041 (−0.069, −0.012) | −0.002 (−0.031, 0.028) | |
| HUI2a | Black versus white men | −0.042 (−0.088, 0.005) | −0.046 (−0.093,0.000) | −0.017 (−0.083, 0.049) |
| Black versus white women | −0.071 (−0.136, −0.005) | −0.076 (−0.142, −0.009) | −0.028 (−0.098, 0.041) | |
| HUI3a | Black versus white men | −0.041 (−0.100, 0.018) | −0.050 (−0.108, 0.008) | 0.018 (−0.039, 0.074) |
| Black versus white women | −0.117 (−0.199, − .035) | −0.124 (−0.207, − 0.041) | −0.039 (−0.125, 0.046) | |
| Summary HRQoLa | Black versus white men | −0.023 (−0.057, 0.010) | −0.030 (−0.063, 0.002) | 0.005 (−0.026, 0.035) |
| Black versus white women | −0.056 (−0.081, −0.031) | −0.061 (−0.086, −0.037) | −0.017 (−0.044, 0.009) | |
| Fair/poor healthb | Black versus white men | 1.64 (1.03, 2.62) | 2.11 (1.32, 3.38) | 1.09 (0.64,1.86) |
| Black versus white women | 2.49 (1.71,3.60) | 3.29 (2.25, 4.82) | 1.68 (1.07, 2.63) | |
| >1 chronic conditionb | Black versus white men | 0.84 (0.56,1.26) | 1.07 (0.69,1.66) | 0.71 (0.45,1.13) |
| Black versus white women | 1.31 (0.94, 1.83) | 1.63 (1.12, 2.38) | 1.04 (0.68,1.59) |
Differences that are significantly different from 0 and odds ratios that are significantly different from 1 at p < 0.05 are bolded
Difference in mean with 95% confidence interval
Odds ratio with 95% confidence interval
In contrast, self-reported health status differs significantly between blacks and whites for both men and women, with and without age adjustment, while multiple chronic conditions are significantly more common only among black women.
Further adjusted results including marital status, education, and income are shown in the last column. Except for marital status, these adjustment variables were all statistically significantly predictive of at least one index, with income being the most significant (P < 0.0001) for all HRQoL indexes. The results indicate that these sociodemographic factors account for most of the racial differences. None remains statistically significant, and only the difference on HUI3 remains of a clinically significant magnitude, although several of the confidence intervals still reach into the clinically important range.
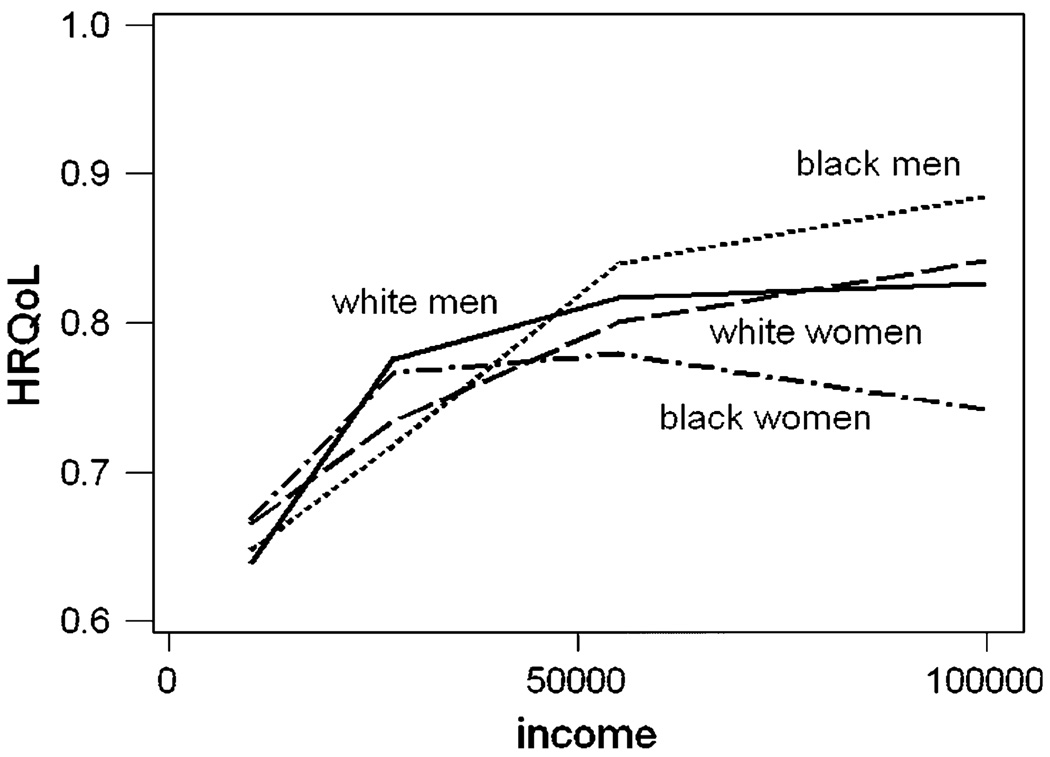
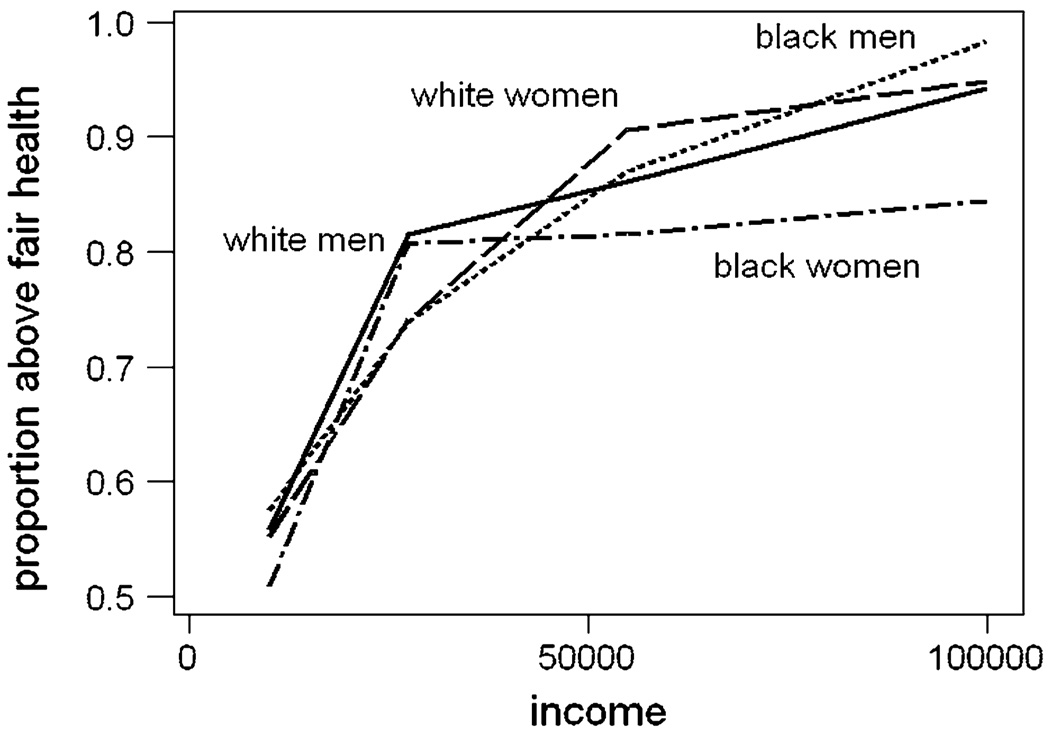
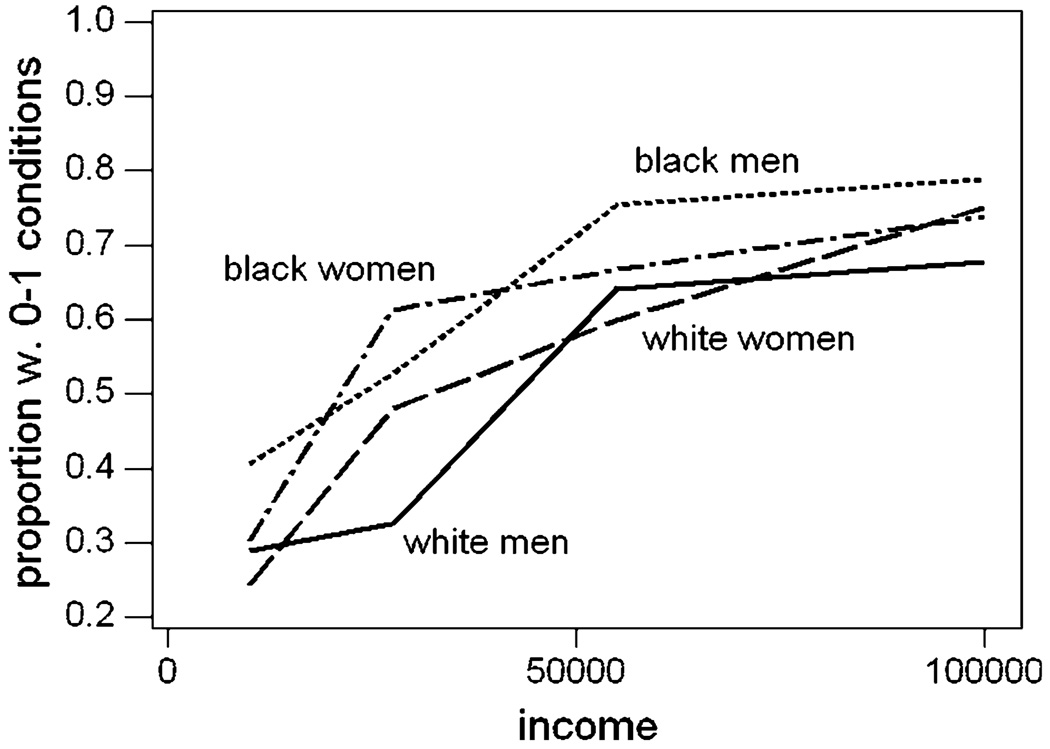
In further analyses of the summary HRQoL score in the fully adjusted model, we found interaction effects between race/gender groups and age (P = 0.038) and race/gender groups and income (P = 0.0083). There were no significant interaction effects in the logistic models for self-reported health or presence of multiple chronic conditions. Inspection of the model indicates that the age interaction largely arises from the age trend among black women seen in Table 3, with a dip in HRQoL in the middle age group. Further insight into the interaction with income is provided in Figs. 1, 2, 3. It is seen that black men at the highest income levels have high HRQoL, while black women have very low HRQoL. This does not coincide well with the pattern for self-reported health, where the relationship of HRQoL to income is more similar within race/gender groups, or with the pattern for no or a single chronic condition. In the latter case, we see that while all groups have a similar pattern with income, both black men and women tend to have fewer physician diagnosed conditions at all income levels.
Fig. 1.
Mean summary HRQoL by income level for white and black men and women
Fig. 2.
Proportion reporting better than fair health by income level for white and black men and women
Fig. 3.
Proportion reporting no or a single chronic health problem from a list of 11 common conditions
Discussion
We found that black women in the US report health states associated with lower preference-scored HRQoL. Black women had substantially lower HRQoL than white men and women on all measures. HRQoL differed less between black and white men. This result is somewhat surprising in light of morbidity and mortality data for black men, but not inconsistent with some previous findings on HRQoL and race [7]. Our further analyses demonstrated that black men do have worse self-reported health than white men, but possibly have fewer doctor diagnosed chronic conditions. Adjusting for household income, education, and marital status practically eliminated the difference in HRQoL between blacks and whites both among women and men. In addition, we found that black women did not demonstrate benefit on HRQoL of high income as did other groups, while black men demonstrated more benefit than other groups. Black men tended to report lower HRQoL at the lowest income level than did white men, but much higher HRQoL at the highest income level. Based on our results, the age and income brackets targeted may strongly influence findings and explain some discrepancies between studies.
The NHMS is unique in being recent and in simultaneously administering five different HRQoL measures. Most of our findings were remarkably similar for all the indexes.
Other research addressing the EQ-5D, HUI2, and HUI3 has observed that blacks scored slightly lower, but after adjustments for SES, both black women and black men had slightly higher scores than other non-Hispanics with the largest difference being for men with the HUI3 at 0.03 [8]. Similar to these results, our fully adjusted models showed non-significant positive coefficients for black versus white men on the SF-6D, QWB-SA, and HUI3, with the largest positive coefficient, 0.018, occurring for the HUI3. Black women remained slightly lower than white women on all measures even after adjusting for the sociodemographic factors.
Black men in the United States have the lowest life expectancy, estimated in 2005 to be 8 years below the national average [26]. Furthermore, they are disproportionately burdened by health problems such as hypertension, diabetes, HIV/AIDS heart disease, and violence [27]. Such excess morbidity did not emerge from our questions on physician diagnosed conditions, possibly because many existing conditions may not have been diagnosed. The lower level of self-reported health among black than white men is consistent with such a possibility, and black men tend to seek less routine medical intervention [27].
HRQoL scores differ fundamentally from these measures as they are based on self-report of specific health states and community valuation of these states. Valuation studies have indicated that blacks tend to assign higher preference than whites to compromised health states [28]. A similar phenomenon may lead them to report a more positive health state than a white person with similar limitations, even when reporting worse overall self-rated health.
Black males may also interpret questions differently. It is not well known if questions on HRQoL instruments are similarly understood by all race and gender groups. The potential for differential interpretation is referred to as differential item functioning (DIF). A few studies have attempted to investigate DIF in relation to race in HRQoL instruments. A study found several consistent patterns of DIF including by race, using two national datasets with different population characteristics [29]. In this study of MOS SF-36, the effect of DIF rarely transferred to the SF-36 scale level [29]. Index scores also depend on the mode of administration and greater personal contact, such as telephone interview, may yield higher scores [30]. It is not known whether mode effects differ by race or gender.
According to our assessments using these data, there are relatively few individuals who fall in the extreme, more easily identifiable categories “unable to dress oneself” or “confined to bed”. Rather, black men may have interpreted more subtle problems such as “moderate pain” differently than other groups. Despite the fact that the literature [28] points to black men and women providing similar valuations of health states presented as vignettes, they may differ in awareness and valuation of their own health. It does not seem unreasonable that black men in many respects report their health more similarly to white men and that perhaps a lower health level coupled with a tendency to choose better health states cancels any differences. Future research may address which health states may be affected by race and gender-based differences in reporting.
Nevertheless, it is necessary to seek alternative explanations for the finding that HRQoL among black men was comparable to that of white men. The NHMS oversampled telephone exchanges with a high percentage of blacks to compensate for the fact that the black male is a relative numerical minority in the United States [27]. In spite of this, black men make up the smallest group, with 370 participants. Besides relatively small sample size, selection bias may be an issue even with the weights post-stratified to the education distribution of each race/gender and age group. The recalibration of weights appears to have calibrated also the income distribution. For example, estimated the percentage (13.8%) of black men in the NHMS population in the greater or equal than US$ 75,000 income bracket is similar to the 14.3% in the Current Population Survey, panel of 2004 [31]. Attempts to further adjust for bias by introducing the differential between a participant’s socioeconomic level and that of their neighborhood minimally affected the result.
Clearly, the possibility of participation bias associated directly with the outcome remains. For example, biases could result from survival effects and African–American overrepresentation in institutional settings. Hence, community-based surveys are likely to under-represent African Americans with some types of health-related issues, most notably mental illnesses [32]. A more subtle influence is the fact that blacks in general may be more suspicious or afraid to reveal how they really feel to others, especially to whites [33]. This may play a role in black men’s participation in health surveys and in the way they respond [34]. For instance, distrust of the health source has been historically based on evidence of racial discrimination and the fear of becoming exploited in medical experiments, such as the Tuskegee Syphilis Experiment [35, 36].
Although the possibilities for bias enumerated here are plausible, they are not consistent with the fact that black men had much higher HRQoL than white men in the highest income category, where these biases would be expected to be least likely. However, the general difficulties of obtaining participation, combined with the issues discussed above that are particular to participation and sharing of information among blacks, may imply that telephone survey is not the optimal method for extracting reliable HRQoL information from this population.
The finding of much lower HRQoL among black women, and especially among black women in the highest household income bracket stands on sharp contrast to the finding among black men. The results are consistent with what has been previously found regarding a variety of health outcomes [37, 38]. Similar to our results, a study of older adults in Chicago found especially low HRQoL among black women, and that the race difference was greater at older age [39]. Evidence from the literature indicates that older black women tend to report more negative health assessments and have worse health beliefs than their white counterparts [40].
Furthermore, it is known that African–American women occupy a disadvantaged position in American society in comparison with whites and black men. Such disadvantage influences how they see themselves but also shapes the perceptions, responses and expectations of others toward them. It is well documented in the literature that neither African American men, with whom they share a racial identity, nor women of other racial or ethnic groups encounter similar struggles of having both race and gender-based threats combine to impact their mental well-being [39, 41, 42]. Their gender and race status also impacts SES attainment and black women have lower educational achievement than their white counterparts. Nevertheless, they have higher levels of education than black men, which has implications for their mental health, given that the female/male gap in education may affect the availability of eligible mates, relationships, family dynamics and marital stability [42], and this could possibly have implications for their overall health-related quality of life, especially among those at the highest income level brackets.
Conclusions and future directions for research
Black women have dramatically lower HRQoL than white men, white women and black men. Surprisingly, the difference is the largest at the highest household income levels. Nonetheless, sociodemographic factors explain a large part of the lower HRQoL among black women. The findings of relatively high HRQoL among black men need to be further evaluated in terms of DIF and with methods of data collection other than telephone or in person survey. Results of different HRQoL indexes paint a very consistent picture of racial differences.
Acknowledgments
Claudia Pereira was funded through a CAPES/Fulbright fellowship. Data collection (The National Health Measurement Study) was funded through grant P01 AG020679 from the National Institute of Aging as was Mari Palta’s effort on the paper.
Contributor Information
Claudia C. A. Pereira, Email: pereirac.claudia@gmail.com, Fundação Oswaldo Cruz, Escola Nacional de Saúde Pública Sergio Arouca, Departamento de Administração e Planejamento em Saúde, Rua Leopoldo Bulhões 1480, sala 724 Manguinhos, Rio de Janeiro, RJ 21041-210, Brazil.
Mari Palta, Email: mpalta@wisc.edu, Population Health Sciences, and Biostatistics and Medical Informatics, School of Medicine and Public Health, University of Wisconsin, 689 Warf Office Building, 610 Walnut St, Madison, WI 53726, USA.
John Mullahy, Email: jmullahy@wisc.edu, Population Health Sciences, School of Medicine and Public Health, University of Wisconsin, 787 Warf Office Building, 610 Walnut St, Madison, WI 53726, USA.
Dennis G. Fryback, Email: dfryback@wisc.edu, Population Health Sciences, School of Medicine and Public Health, University of Wisconsin, 16451 Harbour Ln., Huntington Beach, CA 92649, USA.
References
- 1.Williams D, Mohammed S. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barr DA. Health disparities in the United States : Social class, race, ethnicity, and health. Baltimore: Johns Hopkins University Press; 2008. [Google Scholar]
- 3.Williams DR, Yan Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socioeconomic status, stress and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 4.Quittner AL, Schechter MS, Rasouliyan L, Haselkorn T, Pasta DJ, Wagener JS. Impact of socioeconomic status, race, and ethnicity on quality of life in patients with cystic fibrosis in the United States. Chest. 2010;137(3):642–650. doi: 10.1378/chest.09-0345. [DOI] [PubMed] [Google Scholar]
- 5.Xie J, Wu E, Zheng Z, Sullivan P, Zhan L, Labarthe D. Patient-reported health status in coronary heart disease in the United States: Age, sex, racial, and ethnic differences. Circulation. 2008;118:491–497. doi: 10.1161/CIRCULATIONAHA.107.752006. [DOI] [PubMed] [Google Scholar]
- 6.Gaskin D, Frick K. Race and ethnic disparities in valuing health. Medical Decision Making. 2008;28:12–20. doi: 10.1177/0272989X07309641. [DOI] [PubMed] [Google Scholar]
- 7.Luo N, Johnson J, Shaw J, Feeny D, Coons S. Self-reported health status of the general adult U.S. population as assessed by the EQ-5D and health utilities index. Medical Care. 2005;43:1078–1086. doi: 10.1097/01.mlr.0000182493.57090.c1. [DOI] [PubMed] [Google Scholar]
- 8.Lubetkin E, Jia H, Franks P, Gold M. Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: Examining the EQ-5D in the U.S. general population. Quality of Life Research. 2005;14:2187–2196. doi: 10.1007/s11136-005-8028-5. [DOI] [PubMed] [Google Scholar]
- 9.Brooks R, Rabin R, de Charro F. The measurement and valuation of health status using EQ-5D: A European perspective. Dordrecht, Netherlands: Kluwer Academic Publishers; 2003. [Google Scholar]
- 10.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: Development and testing of the DI valuation model. Medical Care. 2005;43(3):203–220. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Torrance WG, Feeny DH, Furlong WJ, Barr RD, Zhang Y, Wang Q. Multiattribute utility function for a comprehensive health status classification system: Health utilities index mark 2. Medical Care. 1996;34(7):702–722. doi: 10.1097/00005650-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, et al. Multiattribute and singleattribute utility functions for the health utilities index mark 3 system. Medical Care. 2002;40:113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Andresen EM, Rothenberg BM, Kaplan RM. Performance of a self-administered mailed version of the quality of well-being (QWB-SA) questionnaire among older adults. Medical Care. 1998;36:1349–1360. doi: 10.1097/00005650-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. Journal of Health Economics. 2002;21:271–292. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 15.Brazier J, Roberts J. The estimation of a preference-based measure of health from the SF-12. Medical Care. 2004;42:851–859. doi: 10.1097/01.mlr.0000135827.18610.0d. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan P, Lawrence W, Ghushchyan V. A national catalog of preference-based scores for chronic conditions in the United States. Medical Care. 2005;43:736–749. doi: 10.1097/01.mlr.0000172050.67085.4f. [DOI] [PubMed] [Google Scholar]
- 17.House J, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Hofrichter R, editor. Health and social justice: A reader on the politics, ideology, and inequity in the distribution of disease. San Francisco: Jossey-Bass; 2003. pp. 89–131. [Google Scholar]
- 18.Fryback D, Dunham N, Palta M, Hanmer J, Buechner J, Cherepanov D, et al. US norms for six generic health-related quality-of-life indexes from the national health measurement study. Medical Care. 2007;45:1162–1170. doi: 10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cherepanov D, Palta M, Fryback DG, Robert SA. Gender differences in health-related quality-of-life are partly explained by sociodemographic and socioeconomic variation between adult men and women in the US: Evidence from four US nationally representative data sets. Quality of Life Research. 2010 doi: 10.1007/s11136-010-9673-x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robert SA, Cherepanov D, Palta M, Dunham NC, Feeny D, Fryback DG. Socioeconomic status and age variations in health-related quality of life: Results from the national health measurement study. Journal of Gerontology: Social Science. 2009;64B:378–389. doi: 10.1093/geronb/gbp012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schafer JL. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997. [Google Scholar]
- 22.Kaplan RM. The minimally clinically important difference in generic utility-based measures. COPD. 2005;21:91–97. doi: 10.1081/copd-200052090. [DOI] [PubMed] [Google Scholar]
- 23.Walters SJ, Brazier JE. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health and Quality of Life Outcomes. 2003;11:1–4. doi: 10.1186/1477-7525-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Health and Quality of Life Outcomes. 2005;146:1523–1532. doi: 10.1007/s11136-004-7713-0. [DOI] [PubMed] [Google Scholar]
- 25.Coons S, Shaw J. Generic adult health status measures. In: Hayers P, Hays R, editors. Assessing quality of life in clinical trials. New York: Oxford University Press; 2005. p. 467. [Google Scholar]
- 26.National Center for Health Statistics. In Health, United States, 2007. Hyattsville, MD: 2007. Chartbook on trends in the health of Americans; p. 551. [PubMed] [Google Scholar]
- 27.Ware D, Livingston I. The life expectancy of the black male: Pressing issues from the cradle to the grave. In: Livingston IL, editor. Praeger handbook of Black American health: Policies, issues behind disparities in health. Westport, CT: Praeger; 2004. [Google Scholar]
- 28.Shaw J, Johnson J, Chen S, Levin J, Coons S. Racial/ethnic differences in preferences for the EQ-5D health states: Results from the U.S. valuation study. Journal of Clinical Epidemiology. 2007;60:479–490. doi: 10.1016/j.jclinepi.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Perkins A, Stump T, Monahan P, McHorney C. Assessment of differential item functioning for demographic comparisons in the MOS SF-36 health survey. Quality of Life Research. 2006;15:331–348. doi: 10.1007/s11136-005-1551-6. [DOI] [PubMed] [Google Scholar]
- 30.Hanmer J, Hays RD, Fryback DG, et al. Mode of administration is important in US national estimates of health-related quality of life. Medical Care. 2007;45:1171–1179. doi: 10.1097/MLR.0b013e3181354828. [DOI] [PubMed] [Google Scholar]
- 31.United States Census Bureau. Current population survey, 2004 panel. Washington, DC: 2009. [Google Scholar]
- 32.Department of Health, Human Services. Mental health: Culture, race, and ethnicity—a supplement to mental health: A report of the surgeon general. Rockville, MD: Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2001. [PubMed] [Google Scholar]
- 33.McHorney C, Ware J, Lu J, Sherbourne C. The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Shavers-Hornaday V, Lynch C, Burmeister L, Torner J. Why are African Americans under-represented in medical research studies? Impediments to participation. Ethnicity and Health. 1997;2:31–45. doi: 10.1080/13557858.1997.9961813. [DOI] [PubMed] [Google Scholar]
- 35.Katz R, Green B, Kressin N, Kegeles S, Wang M, James S, et al. The legacy of the Tuskegee syphilis study: Assessing its impact on willingness to participate in biomedical studies. Journal of Health Care for the Poor and Underserved. 2008;19:1168–1180. doi: 10.1353/hpu.0.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thomas S, Quinn S. The Tuskegee syphilis study, 1932 to 1972: Implications for HIV education and AIDS risk education programs in the black community. American Journal of Public Health. 1991;81:1498–1505. doi: 10.2105/ajph.81.11.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thorpe RJ, Weiss C, Xue Q, Fried L. Transitions among disability levels or death in African American and white older women. Journal of Gerontology Series A Biological Sciences Medical Sciences. 2009;64:670–674. doi: 10.1093/gerona/glp010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Skarupski KA, Mendes de Leon CF, Bienas JL, Scherr PA, Zack MM, Moriarty DG, et al. Black-white differences in health-related quality of life among older adulta. Quality of Life Research. 2007;16:287–296. doi: 10.1007/s11136-006-9115-y. [DOI] [PubMed] [Google Scholar]
- 39.Bratter J, Eschbach K. Race/ethnic differences in nonspecific psychological distress: Evidence from the national health interview survey. Race/ethnic differences in nonspecific psychological distress: Evidence from the national health interview survey. Social Science Quarterly. 2005;86:620–644. [Google Scholar]
- 40.Ferraro K. Are black older adults health-pessimistic? Journal of Health and Social Behavior. 1993;34:201–214. [PubMed] [Google Scholar]
- 41.Kessler R, Neighbors H. A new perspective on the relationships among race, social class, and psychological distress. Journal of Health and Social Behavior. 1986;27:107–115. [PubMed] [Google Scholar]
- 42.Brown D. A conceptual model of mental well-being for African American women. In: Brown D, Keith V, editors. In and out of our right minds: The mental health of African American women. Vol. xv. New York: Columbia University Press; 2003. p. 301. [Google Scholar]