Abstract
Microfilariae in bone marrow aspirates have been reported occasionally, but until now no case has been reported in association with acute leukaemia. This is a unique finding, not mentioned in literature. Microfilariae are seen mainly in peripheral blood smears (PBS) and rarely in bone marrow aspirate, but this surprisingly did not show any parasite in PBS. Meticulous examination of bone marrow smears revealed acute lymphoblastic leukaemia and a few interspersed microfilariae. This rare combination, reported for the first time, definitely needs a space in literature.
Introduction
Filariasis is a health problem of tropical countries, including Indian subcontinent, particularly rural areas of India. It presents as lymphatic obstruction, fever, tropical pulmonary eosinophilia and asymptomatic microfilaremia. Microfilaria has been reported in association with bone aspirate of a few diseases, but in bone marrow of leukaemic patient it is the first report, as concluded after searching extensively in literature.
Case Report
A 21 year old female presented with weakness, anaemia, lassitude for 1 month, and fever, cervical lymphadenopathy for 15 days. Lymph nodes were multiple, small, bilateral and mostly of ≤1 cm. Bilateral small, vesicular, painful lesions were present at the angle of mouth, which were considered as herpetic on seeing a dermatologist and could have been simply reactivation of a previous infection due to diminishing immunity. On examination patient was anaemic, had mild hepatosplenomegaly and perioral lesions. On investigation platelet count was significantly reduced, peripheral and bone marrow smears showed >40% blasts. Blasts were MPO negative and PAS positive suggesting, its lymphoid lineage. Marrow smears showed a few microfilariae also interspersed in between marrow cells. These microfilaria were confirmed as Waucheria bancrofti because of the presence of a hyaline sheath, length of cephalic space and presence of somatic cells (nuclei). The somatic cells appeared as granules and the tail tip was free from nuclei (Fig. 1a, b).
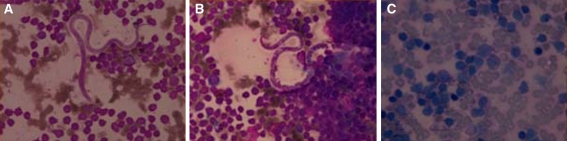
Fig. 1.
a and b Microfilaria of W. bancrofti showing cephalic space, rounded anterior end, hyaline sheath remarkably free from kinks and somatic nuclei. c PAS positivity of blasts indicating its lymphoid lineage
Discussion
Filariasis is a global problem affecting mainly tropics and subtropics of Africa, Asia, western pacific and parts of America affecting over 120 million people in 80 countries [1]. There are at least eight species of filarial parasite that are specific to man [2], of these only three nematode worms—W. bancrofti, Brugia malayi and Brugia timori are found in India and cause lymphatic filariasis. W. bancrofti is the most widespread of filarial nematode infecting human. Human are exclusive host. Vectors are culex mosquitoes in most urban and anopheles in rural areas [3].
Laboratory diagnosis of microfilariae is conventionally made by demonstration in peripheral blood smear. Adult worm reside in lymphatic vessels and the larval form (microfilariae) may circulate in the peripheral blood [3], however in literature it has been described in aspirates from thyroid, soft tissue, lung, epididymis, bone marrow, bronchoalveolar fluid, hydrocele fluid, breast, gastric brushing and subcutaneous swelling. It has also been reported in bone marrow of a case of aplastic anemia. Their presence in bone marrow may indicate the ability of microfilariae to cross vessel wall [4].
This case is unique, as here microfilariae have been reported in the bone marrow, which was primarily aspirated to rule out leukaemia and microfilariae was a coincidental finding, this peculiar presentation has not been described in literature until now.
Conclusion
Whether microfilaria is a simple bystander or acute leukaemic patients are more susceptible to parasitic infections because of their immunocompromised status needs to be studied further. Careful evaluation of smears not only reveals the primary pathology but also associated/coincidental pathologies.
References
- 1.WHO (1998) World Health Report 1998, life in the 21st century, a vision for all, Report of the Director General WHO
- 2.Dissanalike AS. Bull WHO. 1979;57(3):349. [PMC free article] [PubMed] [Google Scholar]
- 3.Garbyal GS, Arundhati, Anshu B, kissonwttee BH. An unusual presentation of filariasis. Acta Cytol. 2008;52:204–206. doi: 10.1159/000325481. [DOI] [PubMed] [Google Scholar]
- 4.Pradhan S, Lahiri Vl, Elehence BR, Singh KN. Am J Trop Med Hyg. 1976;25(25):199–200. doi: 10.4269/ajtmh.1976.25.199. [DOI] [PubMed] [Google Scholar]