Pulmonary fibrosis is a complex and heterogeneous disease; a more detailed and integrated understanding of the cellular and molecular mechanisms influencing its pathogenesis will aid the design of new therapies.
Abstract
Pulmonary fibrosis is a highly heterogeneous and lethal pathological process with limited therapeutic options. Although research on the pathogenesis of pulmonary fibrosis has frequently focused on the mechanisms that regulate the proliferation, activation, and differentiation of collagen-secreting myofibroblasts, recent studies have identified new pathogenic mechanisms that are critically involved in the initiation and progression of fibrosis in a variety of settings. A more detailed and integrated understanding of the cellular and molecular mechanisms of pulmonary fibrosis could help pave the way for effective therapeutics for this devastating and complex disease.
Pulmonary fibrosis is a lung disease that is refractory to treatment and carries a high mortality rate. It includes a heterogeneous group of lung disorders characterized by the progressive and irreversible destruction of lung architecture caused by scar formation that ultimately leads to organ malfunction, disruption of gas exchange, and death from respiratory failure. Idiopathic pulmonary fibrosis (IPF), a particularly severe form of pulmonary fibrosis with unknown etiology has a life expectancy of 2–6 yr after diagnosis (Selman et al., 2001). Lung fibrosis can also develop after viral infections and after exposure to radiotherapy, chemotherapeutic drugs, and aerosolized environmental toxins (Denham and Hauer-Jensen, 2002; Kelly et al., 2002; Fubini and Hubbard, 2003; Chen and Stubbe, 2005). It also occurs in some bone marrow transplant recipients suffering from chronic graft versus host disease and in a subset of individuals with chronic inflammatory diseases like scleroderma and rheumatoid arthritis (Wolff et al., 2002; Young et al., 2007). Currently, the only effective treatment available for progressive lung fibrosis is lung transplantation.
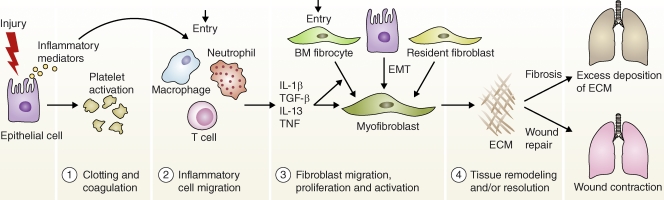
Repair of damaged tissues is a fundamental biological mechanism that allows the ordered replacement of dead or damaged cells after injury, a process critically important for survival (Wynn, 2007). However, if this process becomes dysregulated, it can lead to the development of a permanent fibrotic “scar,” which is characterized by the excess accumulation of extracellular matrix (ECM) components (e.g., hyaluronic acid, fibronectin, proteoglycans, and interstitial collagens) at the site of tissue injury. Consequently, fibrogenesis is often defined as an out of control wound healing response. Wound repair has four distinct stages that include a clotting/coagulation phase, an inflammatory phase, a fibroblast migration/proliferation phase, and a final remodeling phase where normal tissue architecture is restored (Fig. 1). In the earliest stages after tissue damage, epithelial cells and/or endothelial cells release inflammatory mediators that initiate an antifibrinolytic-coagulation cascade that triggers clotting and development of a provisional ECM. Platelet aggregation and subsequent degranulation in turn promotes blood vessel dilation and increased permeability, allowing efficient recruitment of inflammatory cells (e.g., neutrophils, macrophages, lymphocytes, and eosinophils) to the site of injury. Neutrophils are the most abundant inflammatory cell at the earliest stages of wound healing, but are quickly replaced by macrophages after neutrophil degranulation. During this initial leukocyte migration phase, activated macrophages and neutrophils debride the wound and eliminate any invading organisms. They also produce a variety of cytokines and chemokines that amplify the inflammatory response and trigger fibroblast proliferation and recruitment. Myofibroblasts are recruited from a variety of sources including local mesenchymal cells, bone marrow progenitors (called fibrocytes), and via a process called epithelial–mesenchymal transition (EMT), wherein epithelial cells transdifferentiate into fibroblast-like cells. The overall importance of each fibroblast population, however, remains unclear. Once fibroblasts become activated, they transform into α-smooth muscle actin–expressing myofibroblasts that secrete ECM components. Finally, in the wound maturation/remodeling phase, myofibroblasts promote wound contraction, a process where the edges of the wound migrate toward the center and epithelial/endothelial cells divide and migrate over the temporary matrix to regenerate the damaged tissue. Fibrosis develops when the wound is severe, the tissue-damaging irritant persists, or when the repair process becomes dysregulated. Thus, many stages in the wound repair process can go awry and contribute to scar formation, likely explaining the complex nature of pulmonary fibrosis.
Figure 1.
Disruptions in normal wound healing contribute to the development of pulmonary fibrosis. Wound healing has four distinct stages: a clotting/coagulation phase (1), an inflammatory cell migration phase (2), a fibroblast migration/proliferation/activation phase (3), and a tissue remodeling and resolution phase (4). After lung injury, epithelial cells release inflammatory mediators that initiate an antifibrinolytic coagulation cascade, which triggers platelet activation and blood clot formation. This is followed by entry of leukocytes (e.g., neutrophils, macrophages, and T cells). The recruited leukocytes secrete profibrotic cytokines such as IL-1β, TNF, IL-13, and TGF-β. The activated macrophages and neutrophils also remove dead cells and eliminate any invading organisms. In the subsequent phase, fibrocytes from the bone marrow and resident fibroblasts proliferate and differentiate into myofibroblasts, which release ECM components. Fibroblasts and myofibroblasts may also be derived from epithelial cells undergoing EMT. In the final remodeling and resolution phase, activated myofibroblasts can promote wound repair, leading to wound contraction and restoration of blood vessels. However, fibrosis often develops if any stage in the tissue repair program is dysregulated or when the lung-damaging stimulus persists.
Although the relative importance of inflammation in the progression of pulmonary fibrosis has been debated, many forms of the disease are believed to be induced, at least initially, by a strong inflammatory response (Crystal et al., 2002). Although some types of pulmonary fibrosis maintain a significant inflammatory component throughout the course of the disease, other forms like IPF are often characterized as exhibiting highly progressive fibrotic disease in the absence of detectable inflammation (Thannickal et al., 2004). In this case, it has been hypothesized that intrinsic defects in the wound healing response involving lung epithelial cells and fibroblasts contribute to the progression of fibrosis. The fact that an active inflammatory response is not a strict prerequisite likely explains why standard antiinflammatory therapies, including corticosteroids and cytotoxic agents have shown little efficacy in IPF (Demedts et al., 2005). An improved clinical, radiographical, and histopathologic classification of the various forms and stages of pulmonary fibrosis and a more detailed understanding of the molecular mechanisms of fibrogenesis is needed so that therapies can be better tailored to specifically attack the underlying causes of the disease.
Although many forms of pulmonary fibrosis can be effectively modeled and studied in rodents including drug (e.g., bleomycin), particulate-matter (e.g., asbestos and silica), radiation, bronchiolitis obliterans, and chronic graft-versus-host–induced pulmonary fibrosis, it remains unclear whether any of the experimental models truly duplicate the idiopathic form of the disease that is commonly seen in humans (Moore and Hogaboam, 2008). Nevertheless, many important advances have been generated from rodent models, which have been dominated by transgenic and knockout mice that display either enhanced or decreased susceptibility to pulmonary fibrosis. These important studies have greatly expanded our understanding of the mechanisms of pulmonary fibrosis and are a major focus of this review.
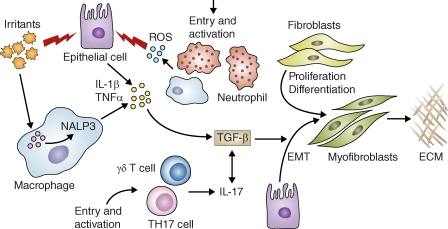
Whereas nearly two decades of research have suggested that TGF-β plays a central role in the pathogenesis of pulmonary fibrosis by promoting the activation, proliferation, and differentiation of epithelial cells and collagen-producing myofibroblasts (Border and Noble, 1994), little progress has been made in moving TGF-β pathway inhibitors from the bench to the bedside (Kisseleva and Brenner, 2008). In fact, there are still currently no approved drugs that specifically target any proposed mechanism of pulmonary fibrosis. Over the past few years several novel antifibrotic strategies have been described that do not involve targeting the TGF-β signaling pathway directly (Fig. 2). This review will highlight some of these exciting discoveries and illustrate how these unique targets and approaches might be exploited to treat this highly heterogeneous and complex disease. It also emphasizes that although many important advances have been made over the past few years, a great deal of work is needed before we can fully integrate all of the pathways and mechanisms that regulate the pathogenesis of pulmonary fibrosis.
Figure 2.
Proinflammatory and profibrotic mediators in the initiation and maintenance of fibrosis. Irritants like silica, asbestos, and bleomycin (uric acid) can injure lung epithelial cells and can be detected by the Nalp3 inflammasome in macrophages. These irritants stimulate the production of ROS, chemokines, and cytokines. These inflammatory mediators enhance the recruitment and activation of leukocytes at the site of tissue injury. For example, IL-1β induces the activation of ROS-expressing neutrophils, which can further damage epithelial cells. IL-1β also promotes production of TGF-β1, an important profibrotic cytokine that triggers fibroblast proliferation and activation. TGF-β also targets epithelial cells, inducing EMT and the formation of ECM-producing myofibroblasts. TGF-β1 further exacerbates the inflammatory response by stimulating the differentiation of Th17 cells. Interactive PPT slides for this figure are available online.
A role for proinflammatory mediators in pulmonary fibrosis
It seems clear that inflammatory mediators play a role in both the initiation and progression of some forms of pulmonary fibrosis (Bringardner et al., 2008). Surgical biopsies and serum samples from patients with idiopathic or systemic sclerosis-associated pulmonary fibrosis display elevated levels of TNF and mice that overexpress the cytokine in the lung develop progressive pulmonary fibrosis (Piguet et al., 1993; Miyazaki et al., 1995; Hasegawa et al., 1997). Macrophages and many other cell types produce TNF in the lung after exposure to silica, asbestos, and bleomycin (Piguet et al., 1990; Piguet and Vesin, 1994; Zhang et al., 1993). Clinical trials were recently initiated to investigate if TNF pathway inhibitors like Etanercept might be beneficial in the treatment of IPF (Raghu et al., 2008). However, although inhibitors of TNF have shown efficacy in some pulmonary fibrosis models, because TNF can inhibit collagen synthesis in myofibroblasts, TNF antagonists might have the undesired effect of worsening the disease (Siwik et al., 2000). Indeed, TNF blockade exacerbated pulmonary fibrosis in rheumatoid arthritis patients taking methotrexate (Thavarajah et al., 2009). Therefore, it remains unclear if TNF blockade will ultimately prove beneficial in IPF or other forms of pulmonary fibrosis.
Like TNF, IL-1β can induce acute lung injury and may contribute to the progression of pulmonary fibrosis (Kolb et al., 2001). Interestingly, IL-1β–induced fibrosis is associated with increased expression of TNF, suggesting that IL-1β– and TNF–triggered fibrosis might be linked mechanistically. The neutrophil attracting CXC chemokines CXCL1 (KC) and CXCL2 (MIP-2) are also increased by IL-1β, as are the profibrotic cytokines platelet-derived growth factor (PDGF) and TGF-β1, illustrating how acute lung injury initiated by proinflammatory cytokines and neutrophils can quickly evolve to a progressive fibrotic response (Kolb et al., 2001; Lappalainen et al., 2005). The IL-1 receptor antagonist dampens the profibrotic effects of IL-1β (Ortiz et al., 2007), and studies with IL-1R1−/−, MyD88−/−, ASC−/−, Caspase-1−/−, and Nalp3−/− mice have suggested that uric acid (induced by bleomycin), asbestos, and silica are detected by the Nalp3 inflammasome in macrophages, leading to IL-1R1/MyD88 signaling that is critical in the pathogenesis of particulate matter and bleomycin-driven fibrosis (Gasse et al., 2007, 2009; Cassel et al., 2008; Dostert et al., 2008).
IL-17A has also been implicated in the pathogenesis of pulmonary fibrosis (Langrish et al., 2005; Bettelli et al., 2006; Simonian et al., 2009; Wilson et al., 2010). IL-17A is increased in the bronchoalveolar lavage (BAL) fluid of patients with IPF (Wilson et al., 2010). IL-17A expression is associated with the persistent neutrophilia observed in a variety of lung disorders, including bacterial pneumonia and cystic fibrosis (Ye et al., 2001; Decraene et al., 2010; Brodlie et al., 2011; Hsu et al., 2011). Notably, recruitment of neutrophils to the BAL is an important predictor of early mortality in IPF patients (Kinder et al., 2008). IL-17A– and IL-17RA–dependent signaling are also important for the development of pulmonary fibrosis after exposure to bleomycin or Saccharopolyspora rectivirgula, a bacterium that causes hypersensitivity pneumonitis in rodent models (Simonian et al., 2009; Wilson et al., 2010). Detailed mechanistic studies in mice with bleomycin-induced fibrosis suggested that IL-23 and possibly IL-12 are important inducers of IL-17A–dependent fibrosis. Although γδ T cells are an important source of IL-17A, CD4+ T cells were identified as the dominant producer of IL-17A after bleomycin exposure. Interestingly, IL-22 produced by γδ T cells protected mouse lungs from Bacillus subtilis–induced fibrosis, perhaps suggesting opposing roles for CD4+ Th17 cells and IL-22–expressing γδ T cells in the development of pulmonary fibrosis (Simonian et al., 2010). Bleomycin-induced IL-17A production is also highly dependent on TGF-β1 signaling, and recombinant IL-17A–driven fibrosis is dependent on the downstream profibrotic activity of TGF-β1, suggesting codependent roles for IL-17A and TGF-β1 in the development of pulmonary fibrosis (Wilson et al., 2010).
Oxidative stress also perpetuates profibrotic inflammatory responses. Indeed, activation of the Nalp3 inflammasome and IL-1β secretion are largely driven by reactive oxygen species (ROS) derived by ROS-generating mitochondria (Naik and Dixit, 2011; Zhou et al., 2011) and NADPH oxidase (NOX) family members expressed in macrophages and neutrophils (Cassel et al., 2008; Dostert et al., 2008). NOX4 activity is induced in the lungs of mice after particle phagocytosis and promotes fibrogenesis in two distinct models of lung injury (Hecker et al., 2009). NOX4 is also increased in cases of human IPF. Mechanistically, NOX4 is required for TGF-β1–induced myofibroblast differentiation, ECM synthesis, and fibroblast contractility.
In addition to directly promoting fibroblast activation, ROS, IL-1β, and TNF can also promote fibrosis by increasing expression of plasminogen activator inhibitor 1, which functions as a physiological inhibitor of the ECM degrading plasmin/plasminogen activator system that protects mouse lungs from fibrosis (Liu, 2008). The plasmin/plasminogen activation system also increases production of prostaglandin E2 and COX-2, which exhibit potent antifibrotic activity in the lung (Park and Christman, 2006; Bauman et al., 2010). The antifibrotic mediator prostaglandin E2 is also induced in the lungs of mice deficient in cytosolic phospholipase A(2), suggesting that antagonists of cytosolic phospholipase A(2) might represent an additional strategy to treat fibrotic lung disease (Nagase et al., 2002; Peters-Golden et al., 2002; Wilborn et al., 1996). It is important to note, however, that not all prostaglandins exhibit antifibrotic activity, as prostaglandin F-2 α, found in the BAL fluid of subjects with IPF, was shown to stimulate collagen production in fibroblasts through a TGF-β1–independent/PG(F) receptor–dependent mechanism (Oga et al., 2009). Nevertheless, these observations illustrate an important role for various mediators in inflammation-driven pulmonary fibrosis (Fig. 2).
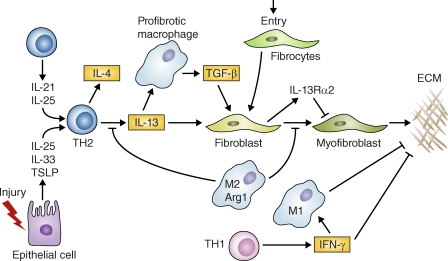
Regulation by Th2 responses and IL-13
There is a great deal of evidence that CD4+ Th1 and Th2 cells play important roles during the inflammatory/maintenance phase of pulmonary fibrosis (Wynn, 2004). Indeed, cytokines associated with CD4+ Th1 and Th2 cells have exhibited contrasting activity in fibrogenesis (Wynn et al., 1995; Fig. 3). IFN-γ inhibits fibrosis, whereas the Th2-associated cytokines IL-4, IL-5, and IL-13 have been causally linked to the development of fibrosis in a variety of chronic inflammatory diseases (Wynn, 2004). Transgenic mice that specifically overexpress IL-4 or IL-13 in the lung confirmed that both cytokines function as profibrotic mediators by both directly and indirectly influencing the activation of myofibroblasts (Rankin et al., 1996; Zhu et al., 1999). IL-5 can also promote fibrosis in the lung by recruiting eosinophils that produce TGF-β1, PDGF, and IL-13 (Huaux et al., 2003b; Cho et al., 2004; Fulkerson et al., 2006; Reiman et al., 2006). Nevertheless, detailed mechanistic studies conducted with IL-4 and IL-13 inhibitors and il-4−/−, il13−/−, il-4ra−/−, and il13ra1−/− mice suggest that the IL-13 signaling pathway likely serves as the dominant inducer of Th2-dependent fibrosis in several chronic lung diseases (Chiaramonte et al., 1999b; Kumar et al., 2002; Huaux et al., 2003a; Kolodsick et al., 2004; Yang et al., 2004; Lama et al., 2006; Keane et al., 2007; Ramalingam et al., 2008). IL-13 is detected in the BAL fluid of IPF patients, IPF fibroblasts are hyperresponsive to IL-13, and expression of both IL-13 and IL-13Rα1 correlate with the severity of the disease (Murray et al., 2008; Park et al., 2009).
Figure 3.
Specialized subsets of T helper cells and macrophages play distinct roles in pulmonary fibrosis. After injury, epithelial cells release IL-25, IL-33, and TSLP, which can facilitate the development of profibrotic Th2 responses. T cells also release IL-21 and IL-25, which promote Th2 differentiation. Th2 cells release IL-4 and IL-13, which promote the development of a profibrotic macrophage subpopulation that secretes TGF-β1 among other mediators. IL-13 can also directly activate fibroblasts independently of TGF-β1. Th2 cytokines also trigger specific chemokines that promote the recruitment of collagen-secreting fibrocytes from the bone marrow, which amplify fibrotic responses. The resulting myofibroblasts release ECM components. However, Th2 cytokines can also trigger antifibrotic feedback mechanisms. For example, Th2 cytokines activate arginase-1 activity in M2 macrophages, which inhibit further IL-13 production and myofibroblast differentiation. IL-13 can also up-regulate the IL-13 decoy receptor in fibroblasts, which antagonizes ECM production via a negative feedback loop. In addition, IFN-γ, produced by Th1 cells, exhibits potent antifibrotic activity by suppressing collagen synthesis in fibroblasts and by promoting the activation of inflammatory M1 macrophages that favor ECM degradation. Interactive PPT slides for this figure are available online.
Consequently, recent studies have focused on elucidating mechanisms that regulate IL-13 effector function. In addition to expressing an IL-13 signaling receptor, a heterodimer composed of the IL-4Rα and IL-13Rα1 subunits, fibroblasts also express a decoy receptor for IL-13, IL-13Rα2 (Chiaramonte et al., 2003). The latter exhibits four orders of magnitude increased affinity for IL-13 (Lupardus et al., 2010) and suppresses IL-13-IL-13Rα1–induced responses, including pulmonary fibrosis (Wilson et al., 2007; Ramalingam et al., 2008; Zheng et al., 2008). IL-21 produced by T cells, IL-33, and thymic stromal lymphopoietin (TSLP) released from damaged epithelial cells, as well as IL-25 produced by both T cells and epithelial cells, also represent potential targets for antifibrotic therapy, as each of these cytokines has been reported to play a major role in the induction and/or amplification of type 2 immunity (Fort et al., 2001; Schmitz et al., 2005; Zhou et al., 2005; Pesce et al., 2006). Nevertheless, although IL-21 regulates liver fibrosis during S. mansoni infection (Pesce et al., 2006) and IL-33 is a major inducer of IL-13–dependent cutaneous fibrosis (Rankin et al., 2010), few studies have examined whether these “Th2-initiating cytokines” participate in the development of pulmonary fibrosis (Ramalingam et al., 2009). In addition to focusing on upstream mediators that regulate IL-13 production, several groups have also been elucidating the downstream mechanisms that are targeted by IL-13. IL-1 (Ingram et al., 2004), TGF-β1 (Lee et al., 2001), adenosine (Blackburn et al., 2003), chitinase family members (Zhu et al., 2004; Lee et al., 2009), chemokines (Belperio et al., 2002a; Zhu et al., 2002; Ma et al., 2004), matrix metalloproteinases (Lanone et al., 2002; Madala et al., 2010) and various fibroblast subsets (Chiaramonte et al., 1999a; Murray et al., 2008; Shao et al., 2008) are emerging as important targets of profibrotic IL-13. Together, these studies support recent efforts investigating the therapeutic potential of IL-13 antagonists in IPF and other chronic lung diseases (Hariyawasam et al., 2009).
Chemokines recruit leukocytes and fibroblasts to the lung
Chemokines are a large family of chemoattractants that recruit leukocytes, fibroblast precursors, and other key effector cells to sites of tissue injury and therefore represent potential targets for antifibrotic therapy (Strieter et al., 2007). Serum levels of CCL18 correlate negatively with declining pulmonary function in patients with pulmonary fibrosis of various causes, suggesting that CCL18 might be developed as a serum biomarker of progressive pulmonary fibrosis (Prasse et al., 2006; Prasse et al., 2009).
Blocking or genetically deleting CCL2 (monocyte-chemoattractant protein-1), CCL6 (C10), or CCR1 provides significant protection from bleomycin-induced pulmonary fibrosis, albeit through mechanisms that remain undefined (Smith et al., 1994; Moore et al., 2001; Tokuda et al., 2000; Belperio et al., 2002a). CXCL12, CCL12, and CCR2 also play important roles in FITC- and bleomycin-induced pulmonary fibrosis by facilitating the recruitment of bone marrow–derived collagen–secreting fibrocytes to the lung (Phillips et al., 2004; Moore et al., 2005, 2006). Signals through the chemokine receptors CCR2, CXCR3, and CXCR2 also regulate fibrosis associated with bronchiolitis obliterans syndrome, by regulating vascular remodeling and recruitment of mononuclear phagocytes and neutrophils (Belperio et al., 2001, 2002b, Belperio et al., b2005). The lysophosphatidic acid receptor 1 also controls the recruitment of fibroblasts in mice with bleomycin-induced fibrosis and levels of lysophosphatidic acid are increased in the BAL fluid of people with IPF (Tager et al., 2008).
Interestingly, however, not all chemoattractants promote pulmonary fibrosis. CXCL10, CXCL11, and CXCR3 inhibit bleomycin-induced fibrosis by preventing fibroblast recruitment, decreasing angiogenesis in the lung, and by promoting the production of the antifibrotic cytokine IFN-γ, respectively (Jiang et al., 2004, 2010; Burdick et al., 2005). Thus, disrupting and/or augmenting specific chemokine signaling pathways could have a significant impact on the progression of pulmonary fibrosis. Given the well-known redundancy in chemokine–chemokine receptor signaling, it will be important to determine which forms and stages of pulmonary fibrosis might benefit from targeting these pathways.
Factors influencing epithelial cell and fibroblast differentiation and proliferation
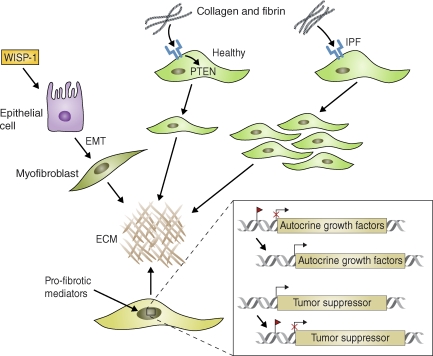
Aberrant activation of developmental and wound-healing pathways also contributes to the pathogenesis of pulmonary fibrosis, particularly in IPF, where ongoing inflammation is believed to play less of a role. For example, the Wnt–β-catenin signaling pathway, which regulates homeostatic self-renewal in several adult tissues, is constitutively active in ATII cells in both a mouse model of pulmonary fibrosis and in patients diagnosed with IPF (Chilosi et al., 2003; Königshoff et al., 2008, 2009). Treatment with WNT1-inducible signaling protein-1 (WISP-1) promotes proliferation and EMT of mouse ATII cells and synthesis of ECM components by mouse and human lung fibroblasts. Development of pulmonary fibrosis in bleomycin-treated mice is reduced when the WNT1 pathway is blocked with WISP1-neutralizing antibodies (Königshoff et al., 2009). Thus, as an inducer of EMT, WISP1 is a potential therapeutic target in IPF (Fig. 4; Thiery and Sleeman, 2006). The integrin α3β1, expressed on epithelial cells, is another important inducer of EMT. Therefore, the α3β1 and Wnt–β-catenin pathways both appear to be involved in the development of pulmonary fibrosis (Kim et al., 2009a).
Figure 4.
Intrinsic changes in the activation status of epithelial cells and fibroblasts can promote growth factor–independent pulmonary fibrosis. Wnt–β-catenin signaling activated (for example) by WISP-1, is constitutively active in some ATII epithelial cells in IPF patients and in mice with bleomycin-induced pulmonary fibrosis. This signaling triggers EMT and synthesis of ECM components by fibroblasts. In healthy fibroblasts, collagen-mediated stimulation of β1 integrin (blue) up-regulates PTEN activity and inhibits proliferation. IPF fibroblasts, however, display a pathological pattern of β1 integrin expression and signaling that can lead to decreased PTEN expression, aberrant activation of PI3 kinase, and excessive proliferation. Profibrotic mediators also promote epigenetic changes in fibroblasts that contribute to the pathogenesis of fibrosis. For example, the promoter regions of various genes encoding autocrine growth and/or differentiation factors can be demethylated, leading to their sustained and heritable activation. In addition, tumor suppressor genes can become methylated (red flag) and therefore inactivated, leading to the sustained activation of oncogenes that promote growth factor–independent proliferation of fibroblasts. miRNAs (e.g., miR-21) may operate in a similar fashion by blocking the translation or promoting the degradation of tumor suppressor genes in fibroblasts.
Fibroblasts isolated from IPF patients also display constitutive changes in their proliferative ability (Ramos et al., 2001), fail to invade the ECM, and display altered expression of genes in matrix production and degradation (Lovgren et al., 2011), suggesting that intrinsic defects in the activation status of fibroblasts might contribute to the pathogenesis of pulmonary fibrosis. β1 integrin inhibits fibroblast proliferation when bound to polymerized type 1 collagen by facilitating the activation of the tumor suppressor phosphatase and tensin homologue (PTEN), which normally suppresses the PI3K–Akt–S6K1 signaling pathway (Xia et al., 2008). IPF fibroblasts evade this inhibitory mechanism by displaying a pathological pattern of β1 integrin expression that leads to low PTEN activity and uncontrolled activation of the PI3K–AKT–S6K1 pathway (Fig. 4). In support of this theory, mice deficient in PTEN display a prolonged fibroproliferative response after tissue injury (Xia et al., 2008). Loss of either β-arrestin1 or β-arrestin2 was shown to block fibroblast invasion into the ECM and to protect mice from bleomycin-induced fibrosis (Lovgren et al., 2011). In contrast, mice deficient in the cationic amino acid transporter Slc7a2 exhibit heightened fibroproliferative responses and increased Th2-cytokine–associated fibrosis (Thompson et al., 2008). Thus, intrinsic defects in fibroblast proliferative pathways can have a significant impact on the progression of pulmonary fibrosis.
Epigenetic changes in fibroblasts have also been hypothesized to contribute to the pathogenesis of fibrosis by preventing proliferating fibroblasts from returning to their resting state. A recent genome-wide methylation scan of fibroblasts revealed several DNA methylation modifications that were unique to collagen-secreting myofibroblasts obtained from fibrotic kidneys (Bechtel et al., 2010). One of these modifications led to the epigenetic silencing of Rasal1, a suppressor of the Ras protooncogene, which led to increased Ras activity and growth factor–independent proliferation of fibroblasts. This study was important because it provided a novel molecular explanation for the sustained and heritable activation of fibroblasts that is often observed when fibrosis becomes advanced (Fig. 4). The targeted repression of known antifibrotic genes by hypermethylation may also contribute to the development of pulmonary fibrosis (Coward et al., 2010). Interestingly, DNA methyltransferase inhibitors reversed epigenetic modifications and protected mice from pulmonary fibrosis (Sanders et al., 2008). Therefore, because epigenetic modifications are potentially reversible, they may represent attractive targets for novel antifibrotic therapies.
Additional potential therapeutic targets and strategies
Peroxisome proliferator-activated receptors (PPARs) α, β/δ, and γ are ligand-activated transcription factors that belong to the nuclear hormone receptor family and important regulators of metabolic and inflammatory processes (Kostadinova et al., 2005). The receptors are found on a wide variety of tissues in the lung, including airway epithelial cells and smooth muscle cells, and PPAR signaling has been implicated in the pathogenesis of a wide variety of inflammatory diseases of the lung (Huang et al., 2005). Agonists of the three receptors suppress inflammation by inhibiting the production of proinflammatory cytokines, including IL-1β and TNF, and by reducing the influx of neutrophils into the lung. Some PPAR ligands also reduce the expression of Th2 cytokines, adhesion molecules, and chemokines that function as major drivers of pulmonary fibrosis (Sime, 2008). PPARα agonists reduce the development of bleomycin-induced pulmonary fibrosis, and mice deficient in PPARα develop exacerbated lung fibrosis associated with increased production of IL-1β and TNF (Genovese et al., 2005b). PPARβ/δ agonists also inhibit lung fibroblast proliferation and enhance the antifibrotic properties of PPARγ agonists. PPARγ agonists display similar protective activity and inhibit TGF-β1–driven myofibroblast differentiation in vitro and the profibrotic activity of TGF-β1 in vivo (Burgess et al., 2005; Genovese et al., 2005a; Milam et al., 2008). Thus, in cases where pulmonary fibrosis is associated with a persistent proinflammatory response, PPAR ligands may prove beneficial.
MicroRNAs (miRNAs) are small, evolutionarily conserved, noncoding RNAs ∼22 nt in length that play important roles in a variety of pathophysiologic processes by blocking the translation or promoting the degradation of specific target mRNAs. Unique miRNA expression patterns have been identified in a variety of lung disorders including COPD, emphysema, cystic fibrosis, asthma, lung cancer, and IPF, suggesting that distinct subsets of genes are targeted by microRNAs in each disease (Nana-Sinkam et al., 2009). Recently, miR-21 was identified in the lungs of patients with IPF and in mice with bleomycin-induced pulmonary fibrosis (Liu et al., 2010). In agreement with related studies (Thum et al., 2008; Kim et al., 2009b), miR-21 production was primarily localized to myofibroblasts and expression was tightly controlled by the profibrotic cytokine TGF-β1 (Liu et al., 2010). Administration of miR-21 antisense probes decreased the severity of bleomycin-induced fibrosis in mice and attenuated the profibrotic activity of TGF-β1 in fibroblasts, confirming a critical role for miR-21 in lung fibrogenesis. Interestingly, miR-21 targets several tumor suppressor genes and promotes tumor growth and invasion (Fig. 4), suggesting it can function as an oncogene (Meng et al., 2007; Zhu et al., 2007, 2008; Asangani et al., 2008). miR-21 also operates as antiapoptotic factor in tumor cells (Chan et al., 2005). Thus, aberrant expression of miR-21 in fibroblasts could promote their survival and differentiation into pathogenic collagen-secreting myofibroblasts. Therefore, small-molecule inhibitors of miR-21 might be developed to treat IPF. Identifying specific miRNAs that block profibrotic genes or promote lung regeneration could also prove highly beneficial in the treatment of pulmonary fibrosis (Pandit et al., 2010).
Disease stage-specific roles of macrophages
Macrophages are integrated into all stages of the fibrotic process, perhaps because they serve as key regulators of fibroblast recruitment, proliferation, and activation (Wynn and Barron, 2010). They promote fibrosis by secreting chemokines and specific matrix metalloproteinases that degrade ECM components, thus facilitating the recruitment of inflammatory cells to sites of tissue injury (Zuo et al., 2002; Jiang et al., 2005). They also produce several profibrotic mediators, including TGF-β1 and PDGF that induce the proliferation and activation of collagen-secreting myofibroblasts (Song et al., 2000). Alveolar macrophages isolated from fibrotic lung tissues are also capable of producing profibrotic cytokines (Hancock et al., 1998; Ingram et al., 2004; Cassel et al., 2008; Wilson et al., 2010).
Nevertheless, although some macrophages clearly promote tissue fibrogenesis, other macrophage subpopulations may facilitate the resolution and/or reversal of fibrosis (Iredale, 2007; Wynn and Barron, 2010). Studies conducted with CD11b-DTR mice showed that if macrophages were depleted during the early inflammatory/maintenance phase of a fibrotic response, scarring was reduced and myofibroblasts were decreased (Fig. 1). In contrast, if macrophages were depleted during the late remodeling/recovery phase, fibrosis persisted (Duffield et al., 2005). This important study confirmed that macrophages could play distinct roles in the inflammatory and remodeling phases of wound healing and fibrosis. Macrophages inhibit fibrosis by secreting mediators that induce myofibroblast apoptosis, removing cellular debris that can drive inflammation, digesting and engulfing ECM components, and stimulating the production of collagen-degrading MMPs in a variety of cell types, including myofibroblasts and neutrophils (Atabai et al., 2009; Wynn and Barron, 2010). Th2 cytokine-stimulated macrophages that express the enzyme arginase-1 also exhibit potent antifibrotic activity (Pesce et al., 2009). An important goal of future research will be to determine if the pro- and antifibrotic activities of macrophages are performed by distinct subpopulations or whether the same macrophage can adjust its phenotype over time in coordination with new stimuli found in the local environment. Harnessing the protective activity of antifibrotic macrophages may be key to ameliorating established and progressive fibrosis, as restoration of normal tissue architecture can proceed only if the existing collagen matrix is successfully removed.
Conclusions and future perspectives
A variety of experimental models have been generated to study the mechanisms of pulmonary fibrosis (Moore and Hogaboam, 2008). However, the mouse bleomycin model has garnered the most attention, perhaps because it is a well-characterized and clinically relevant model of pulmonary fibrosis. Nevertheless, although it successfully models the early proinflammatory stages of the disease, because of the transient nature of the bleomycin response and the reversibility of the fibrosis, it is unclear whether this model can truly replicate the chronic and progressive forms of the disease seen in humans. Epithelial damage, inflammation, EMT, myofibroblast activation, and repetitive cycles of tissue injury are certainly important initiators of fibrosis. However, if we are to develop effective therapeutics for pulmonary fibrosis, a more detailed understanding of the complex environmental, cellular, genetic, and epigenetic changes that synergize to promote the progression of chronic pulmonary fibrosis is needed. Inflammatory and profibrotic mediators likely serve as the trigger for the epigenetic modifications that are observed in epithelial cells, endothelial cells, and fibroblasts. Therefore, a more integrated approach that targets key inflammatory cytokines, profibrotic mediators, and epigenetic modifications simultaneously will likely emerge as the most successful strategy to treat this highly complex and devastating disease. As there are numerous causes, forms, and stages of pulmonary fibrosis, the heterogeneous nature of the disease must be considered when evaluating the results from individual mouse models, and, most importantly, when designing and implementing novel treatment strategies.
Acknowledgments
I would like to sincerely thank the past and present members of my laboratory for their guidance and support. The Wynn laboratory is supported by the intramural research program of the National Institute of Allergy and Infectious Disease/National Institutes of Health.
Footnotes
Abbreviations used:
- BAL
- bronchoalveolar lavage
- ECM
- extracellular matrix
- EMT
- epithelial–mesenchymal transition
- IPF
- idiopathic pulmonary fibrosis
- miRNA
- micro RNA
- PDGF
- platelet-derived growth factor
- PPAR
- peroxisome proliferator-activated receptor
- PTEN
- phosphatase and tensin homologue
- ROS
- reactive oxygen species
- TSLP
- thymic stromal lymphopoietin
- WISP-1
- WNT1-inducible signaling protein-1
References
- Asangani I.A., Rasheed S.A., Nikolova D.A., Leupold J.H., Colburn N.H., Post S., Allgayer H. 2008. MicroRNA-21 (miR-21) post-transcriptionally downregulates tumor suppressor Pdcd4 and stimulates invasion, intravasation and metastasis in colorectal cancer. Oncogene. 27:2128–2136 10.1038/sj.onc.1210856 [DOI] [PubMed] [Google Scholar]
- Atabai K., Jame S., Azhar N., Kuo A., Lam M., McKleroy W., Dehart G., Rahman S., Xia D.D., Melton A.C., et al. 2009. Mfge8 diminishes the severity of tissue fibrosis in mice by binding and targeting collagen for uptake by macrophages. J. Clin. Invest. 119:3713–3722 10.1172/JCI40053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman K.A., Wettlaufer S.H., Okunishi K., Vannella K.M., Stoolman J.S., Huang S.K., Courey A.J., White E.S., Hogaboam C.M., Simon R.H., et al. 2010. The antifibrotic effects of plasminogen activation occur via prostaglandin E2 synthesis in humans and mice. J. Clin. Invest. 120:1950–1960 10.1172/JCI38369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechtel W., McGoohan S., Zeisberg E.M., Müller G.A., Kalbacher H., Salant D.J., Müller C.A., Kalluri R., Zeisberg M. 2010. Methylation determines fibroblast activation and fibrogenesis in the kidney. Nat. Med. 16:544–550 10.1038/nm.2135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belperio J.A., Keane M.P., Burdick M.D., Lynch J.P., III, Xue Y.Y., Berlin A., Ross D.J., Kunkel S.L., Charo I.F., Strieter R.M. 2001. Critical role for the chemokine MCP-1/CCR2 in the pathogenesis of bronchiolitis obliterans syndrome. J. Clin. Invest. 108:547–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belperio J.A., Dy M., Burdick M.D., Xue Y.Y., Li K., Elias J.A., Keane M.P. 2002a. Interaction of IL-13 and C10 in the pathogenesis of bleomycin-induced pulmonary fibrosis. Am. J. Respir. Cell Mol. Biol. 27:419–427 [DOI] [PubMed] [Google Scholar]
- Belperio J.A., Keane M.P., Burdick M.D., Lynch J.P., III, Xue Y.Y., Li K., Ross D.J., Strieter R.M. 2002b. Critical role for CXCR3 chemokine biology in the pathogenesis of bronchiolitis obliterans syndrome. J. Immunol. 169:1037–1049 [DOI] [PubMed] [Google Scholar]
- Belperio J.A., Keane M.P., Burdick M.D., Gomperts B., Xue Y.Y., Hong K., Mestas J., Ardehali A., Mehrad B., Saggar R., et al. 2005. Role of CXCR2/CXCR2 ligands in vascular remodeling during bronchiolitis obliterans syndrome. J. Clin. Invest. 115:1150–1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bettelli E., Carrier Y., Gao W., Korn T., Strom T.B., Oukka M., Weiner H.L., Kuchroo V.K. 2006. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 441:235–238 10.1038/nature04753 [DOI] [PubMed] [Google Scholar]
- Blackburn M.R., Lee C.G., Young H.W., Zhu Z., Chunn J.L., Kang M.J., Banerjee S.K., Elias J.A. 2003. Adenosine mediates IL-13-induced inflammation and remodeling in the lung and interacts in an IL-13-adenosine amplification pathway. J. Clin. Invest. 112:332–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Border W.A., Noble N.A. 1994. Transforming growth factor beta in tissue fibrosis. N. Engl. J. Med. 331:1286–1292 10.1056/NEJM199411103311907 [DOI] [PubMed] [Google Scholar]
- Bringardner B.D., Baran C.P., Eubank T.D., Marsh C.B. 2008. The role of inflammation in the pathogenesis of idiopathic pulmonary fibrosis. Antioxid. Redox Signal. 10:287–301 10.1089/ars.2007.1897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodlie M., McKean M.C., Johnson G.E., Anderson A.E., Hilkens C.M., Fisher A.J., Corris P.A., Lordan J.L., Ward C. 2011. Raised interleukin-17 is immunolocalised to neutrophils in cystic fibrosis lung disease. Eur. Respir. J. 37:1378–1385 10.1183/09031936.00067110 [DOI] [PubMed] [Google Scholar]
- Burdick M.D., Murray L.A., Keane M.P., Xue Y.Y., Zisman D.A., Belperio J.A., Strieter R.M. 2005. CXCL11 attenuates bleomycin-induced pulmonary fibrosis via inhibition of vascular remodeling. Am. J. Respir. Crit. Care Med. 171:261–268 10.1164/rccm.200409-1164OC [DOI] [PubMed] [Google Scholar]
- Burgess H.A., Daugherty L.E., Thatcher T.H., Lakatos H.F., Ray D.M., Redonnet M., Phipps R.P., Sime P.J. 2005. PPARgamma agonists inhibit TGF-beta induced pulmonary myofibroblast differentiation and collagen production: implications for therapy of lung fibrosis. Am. J. Physiol. Lung Cell. Mol. Physiol. 288:L1146–L1153 10.1152/ajplung.00383.2004 [DOI] [PubMed] [Google Scholar]
- Cassel S.L., Eisenbarth S.C., Iyer S.S., Sadler J.J., Colegio O.R., Tephly L.A., Carter A.B., Rothman P.B., Flavell R.A., Sutterwala F.S. 2008. The Nalp3 inflammasome is essential for the development of silicosis. Proc. Natl. Acad. Sci. USA. 105:9035–9040 10.1073/pnas.0803933105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.A., Krichevsky A.M., Kosik K.S. 2005. MicroRNA-21 is an antiapoptotic factor in human glioblastoma cells. Cancer Res. 65:6029–6033 10.1158/0008-5472.CAN-05-0137 [DOI] [PubMed] [Google Scholar]
- Chen J., Stubbe J. 2005. Bleomycins: towards better therapeutics. Nat. Rev. Cancer. 5:102–112 10.1038/nrc1547 [DOI] [PubMed] [Google Scholar]
- Chiaramonte M.G., Donaldson D.D., Cheever A.W., Wynn T.A. 1999a. An IL-13 inhibitor blocks the development of hepatic fibrosis during a T-helper type 2-dominated inflammatory response. J. Clin. Invest. 104:777–785 10.1172/JCI7325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiaramonte M.G., Schopf L.R., Neben T.Y., Cheever A.W., Donaldson D.D., Wynn T.A. 1999b. IL-13 is a key regulatory cytokine for Th2 cell-mediated pulmonary granuloma formation and IgE responses induced by Schistosoma mansoni eggs. J. Immunol. 162:920–930 [PubMed] [Google Scholar]
- Chiaramonte M.G., Mentink-Kane M., Jacobson B.A., Cheever A.W., Whitters M.J., Goad M.E., Wong A., Collins M., Donaldson D.D., Grusby M.J., Wynn T.A. 2003. Regulation and function of the interleukin 13 receptor α2 during a T helper cell type 2-dominant immune response. J. Exp. Med. 197:687–701 10.1084/jem.20020903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilosi M., Poletti V., Zamò A., Lestani M., Montagna L., Piccoli P., Pedron S., Bertaso M., Scarpa A., Murer B., et al. 2003. Aberrant Wnt/beta-catenin pathway activation in idiopathic pulmonary fibrosis. Am. J. Pathol. 162:1495–1502 10.1016/S0002-9440(10)64282-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho J.Y., Miller M., Baek K.J., Han J.W., Nayar J., Lee S.Y., McElwain K., McElwain S., Friedman S., Broide D.H. 2004. Inhibition of airway remodeling in IL-5-deficient mice. J. Clin. Invest. 113:551–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coward W.R., Watts K., Feghali-Bostwick C.A., Jenkins G., Pang L. 2010. Repression of IP-10 by interactions between histone deacetylation and hypermethylation in idiopathic pulmonary fibrosis. Mol. Cell. Biol. 30:2874–2886 10.1128/MCB.01527-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crystal R.G., Bitterman P.B., Mossman B., Schwarz M.I., Sheppard D., Almasy L., Chapman H.A., Friedman S.L., King T.E., Jr, Leinwand L.A., et al. 2002. Future research directions in idiopathic pulmonary fibrosis: summary of a National Heart, Lung, and Blood Institute working group. Am. J. Respir. Crit. Care Med. 166:236–246 10.1164/rccm.2201069 [DOI] [PubMed] [Google Scholar]
- Decraene A., Willems-Widyastuti A., Kasran A., De Boeck K., Bullens D.M., Dupont L.J. 2010. Elevated expression of both mRNA and protein levels of IL-17A in sputum of stable cystic fibrosis patients. Respir. Res. 11:177 10.1186/1465-9921-11-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demedts M., Behr J., Buhl R., Costabel U., Dekhuijzen R., Jansen H.M., MacNee W., Thomeer M., Wallaert B., Laurent F., et al. ; IFIGENIA Study Group 2005. High-dose acetylcysteine in idiopathic pulmonary fibrosis. N. Engl. J. Med. 353:2229–2242 10.1056/NEJMoa042976 [DOI] [PubMed] [Google Scholar]
- Denham J.W., Hauer-Jensen M. 2002. The radiotherapeutic injury—a complex ‘wound’. Radiother. Oncol. 63:129–145 10.1016/S0167-8140(02)00060-9 [DOI] [PubMed] [Google Scholar]
- Dostert C., Pétrilli V., Van Bruggen R., Steele C., Mossman B.T., Tschopp J. 2008. Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica. Science. 320:674–677 10.1126/science.1156995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffield J.S., Forbes S.J., Constandinou C.M., Clay S., Partolina M., Vuthoori S., Wu S., Lang R., Iredale J.P. 2005. Selective depletion of macrophages reveals distinct, opposing roles during liver injury and repair. J. Clin. Invest. 115:56–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fort M.M., Cheung J., Yen D., Li J., Zurawski S.M., Lo S., Menon S., Clifford T., Hunte B., Lesley R., et al. 2001. IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo. Immunity. 15:985–995 10.1016/S1074-7613(01)00243-6 [DOI] [PubMed] [Google Scholar]
- Fubini B., Hubbard A. 2003. Reactive oxygen species (ROS) and reactive nitrogen species (RNS) generation by silica in inflammation and fibrosis. Free Radic. Biol. Med. 34:1507–1516 10.1016/S0891-5849(03)00149-7 [DOI] [PubMed] [Google Scholar]
- Fulkerson P.C., Fischetti C.A., Rothenberg M.E. 2006. Eosinophils and CCR3 regulate interleukin-13 transgene-induced pulmonary remodeling. Am. J. Pathol. 169:2117–2126 10.2353/ajpath.2006.060617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasse P., Mary C., Guenon I., Noulin N., Charron S., Schnyder-Candrian S., Schnyder B., Akira S., Quesniaux V.F., Lagente V., et al. 2007. IL-1R1/MyD88 signaling and the inflammasome are essential in pulmonary inflammation and fibrosis in mice. J. Clin. Invest. 117:3786–3799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasse P., Riteau N., Charron S., Girre S., Fick L., Pétrilli V., Tschopp J., Lagente V., Quesniaux V.F., Ryffel B., Couillin I. 2009. Uric acid is a danger signal activating NALP3 inflammasome in lung injury inflammation and fibrosis. Am. J. Respir. Crit. Care Med. 179:903–913 10.1164/rccm.200808-1274OC [DOI] [PubMed] [Google Scholar]
- Genovese T., Cuzzocrea S., Di Paola R., Mazzon E., Mastruzzo C., Catalano P., Sortino M., Crimi N., Caputi A.P., Thiemermann C., Vancheri C. 2005a. Effect of rosiglitazone and 15-deoxy-Delta12,14-prostaglandin J2 on bleomycin-induced lung injury. Eur. Respir. J. 25:225–234 10.1183/09031936.05.00049704 [DOI] [PubMed] [Google Scholar]
- Genovese T., Mazzon E., Di Paola R., Muia C., Crisafulli C., Caputi A.P., Cuzzocrea S. 2005b. Role of endogenous and exogenous ligands for the peroxisome proliferator-activated receptor alpha in the development of bleomycin-induced lung injury. Shock. 24:547–555 10.1097/01.shk.0000190825.28783.a4 [DOI] [PubMed] [Google Scholar]
- Hancock A., Armstrong L., Gama R., Millar A. 1998. Production of interleukin 13 by alveolar macrophages from normal and fibrotic lung. Am. J. Respir. Cell Mol. Biol. 18:60–65 [DOI] [PubMed] [Google Scholar]
- Hariyawasam H.H., Nicholson G.C., Tan A.J., Syngal N., Quinn D., Boulton C., Walker C., Rodman D., Westwick J., Kon O.M., et al. 2009. Effects of Anti-IL-13 (Novartis QAX576) on Inflammatory Responses Following Nasal Allergen Challenge (NAC). Am. J. Respir. Crit. Care Med. 179:A3642 [Google Scholar]
- Hasegawa M., Fujimoto M., Kikuchi K., Takehara K. 1997. Elevated serum tumor necrosis factor-alpha levels in patients with systemic sclerosis: association with pulmonary fibrosis. J. Rheumatol. 24:663–665 [PubMed] [Google Scholar]
- Hecker L., Vittal R., Jones T., Jagirdar R., Luckhardt T.R., Horowitz J.C., Pennathur S., Martinez F.J., Thannickal V.J. 2009. NADPH oxidase-4 mediates myofibroblast activation and fibrogenic responses to lung injury. Nat. Med. 15:1077–1081 10.1038/nm.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu E., Shi H., Jordan R.M., Lyons-Weiler J., Pilewski J.M., Feghali-Bostwick C.A. 2011. Lung tissues in patients with systemic sclerosis have gene expression patterns unique to pulmonary fibrosis and pulmonary hypertension. Arthritis Rheum. 63:783–794 10.1002/art.30159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang T.H., Razmovski-Naumovski V., Kota B.P., Lin D.S., Roufogalis B.D. 2005. The pathophysiological function of peroxisome proliferator-activated receptor-gamma in lung-related diseases. Respir. Res. 6:102 10.1186/1465-9921-6-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huaux F., Liu T., McGarry B., Ullenbruch M., Phan S.H. 2003a. Dual roles of IL-4 in lung injury and fibrosis. J. Immunol. 170:2083–2092 [DOI] [PubMed] [Google Scholar]
- Huaux F., Liu T., McGarry B., Ullenbruch M., Xing Z., Phan S.H. 2003b. Eosinophils and T lymphocytes possess distinct roles in bleomycin-induced lung injury and fibrosis. J. Immunol. 171:5470–5481 [DOI] [PubMed] [Google Scholar]
- Ingram J.L., Rice A.B., Geisenhoffer K., Madtes D.K., Bonner J.C. 2004. IL-13 and IL-1beta promote lung fibroblast growth through coordinated up-regulation of PDGF-AA and PDGF-Ralpha. FASEB J. 18:1132–1134 [DOI] [PubMed] [Google Scholar]
- Iredale J.P. 2007. Models of liver fibrosis: exploring the dynamic nature of inflammation and repair in a solid organ. J. Clin. Invest. 117:539–548 10.1172/JCI30542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang D., Liang J., Hodge J., Lu B., Zhu Z., Yu S., Fan J., Gao Y., Yin Z., Homer R., et al. 2004. Regulation of pulmonary fibrosis by chemokine receptor CXCR3. J. Clin. Invest. 114:291–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang D., Liang J., Fan J., Yu S., Chen S., Luo Y., Prestwich G.D., Mascarenhas M.M., Garg H.G., Quinn D.A., et al. 2005. Regulation of lung injury and repair by Toll-like receptors and hyaluronan. Nat. Med. 11:1173–1179 10.1038/nm1315 [DOI] [PubMed] [Google Scholar]
- Jiang D., Liang J., Campanella G.S., Guo R., Yu S., Xie T., Liu N., Jung Y., Homer R., Meltzer E.B., et al. 2010. Inhibition of pulmonary fibrosis in mice by CXCL10 requires glycosaminoglycan binding and syndecan-4. J. Clin. Invest. 120:2049–2057 10.1172/JCI38644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane M.P., Gomperts B.N., Weigt S., Xue Y.Y., Burdick M.D., Nakamura H., Zisman D.A., Ardehali A., Saggar R., Lynch J.P., III, et al. 2007. IL-13 is pivotal in the fibro-obliterative process of bronchiolitis obliterans syndrome. J. Immunol. 178:511–519 [DOI] [PubMed] [Google Scholar]
- Kelly B.G., Lok S.S., Hasleton P.S., Egan J.J., Stewart J.P. 2002. A rearranged form of Epstein-Barr virus DNA is associated with idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 166:510–513 10.1164/rccm.2103058 [DOI] [PubMed] [Google Scholar]
- Kim K.K., Wei Y., Szekeres C., Kugler M.C., Wolters P.J., Hill M.L., Frank J.A., Brumwell A.N., Wheeler S.E., Kreidberg J.A., Chapman H.A. 2009a. Epithelial cell alpha3beta1 integrin links beta-catenin and Smad signaling to promote myofibroblast formation and pulmonary fibrosis. J. Clin. Invest. 119:213–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y.J., Hwang S.J., Bae Y.C., Jung J.S. 2009b. MiR-21 regulates adipogenic differentiation through the modulation of TGF-beta signaling in mesenchymal stem cells derived from human adipose tissue. Stem Cells. 27:3093–3102 [DOI] [PubMed] [Google Scholar]
- Kinder B.W., Brown K.K., Schwarz M.I., Ix J.H., Kervitsky A., King T.E., Jr 2008. Baseline BAL neutrophilia predicts early mortality in idiopathic pulmonary fibrosis. Chest. 133:226–232 10.1378/chest.07-1948 [DOI] [PubMed] [Google Scholar]
- Kisseleva T., Brenner D.A. 2008. Mechanisms of fibrogenesis. Exp. Biol. Med. (Maywood). 233:109–122 10.3181/0707-MR-190 [DOI] [PubMed] [Google Scholar]
- Kolb M., Margetts P.J., Anthony D.C., Pitossi F., Gauldie J. 2001. Transient expression of IL-1beta induces acute lung injury and chronic repair leading to pulmonary fibrosis. J. Clin. Invest. 107:1529–1536 10.1172/JCI12568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolodsick J.E., Toews G.B., Jakubzick C., Hogaboam C., Moore T.A., McKenzie A., Wilke C.A., Chrisman C.J., Moore B.B. 2004. Protection from fluorescein isothiocyanate-induced fibrosis in IL-13-deficient, but not IL-4-deficient, mice results from impaired collagen synthesis by fibroblasts. J. Immunol. 172:4068–4076 [DOI] [PubMed] [Google Scholar]
- Königshoff M., Balsara N., Pfaff E.M., Kramer M., Chrobak I., Seeger W., Eickelberg O. 2008. Functional Wnt signaling is increased in idiopathic pulmonary fibrosis. PLoS ONE. 3:e2142 10.1371/journal.pone.0002142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Königshoff M., Kramer M., Balsara N., Wilhelm J., Amarie O.V., Jahn A., Rose F., Fink L., Seeger W., Schaefer L., et al. 2009. WNT1-inducible signaling protein-1 mediates pulmonary fibrosis in mice and is upregulated in humans with idiopathic pulmonary fibrosis. J. Clin. Invest. 119:772–787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostadinova R., Wahli W., Michalik L. 2005. PPARs in diseases: control mechanisms of inflammation. Curr. Med. Chem. 12:2995–3009 10.2174/092986705774462905 [DOI] [PubMed] [Google Scholar]
- Kumar R.K., Herbert C., Yang M., Koskinen A.M., McKenzie A.N., Foster P.S. 2002. Role of interleukin-13 in eosinophil accumulation and airway remodelling in a mouse model of chronic asthma. Clin. Exp. Allergy. 32:1104–1111 10.1046/j.1365-2222.2002.01420.x [DOI] [PubMed] [Google Scholar]
- Lama V.N., Harada H., Badri L.N., Flint A., Hogaboam C.M., McKenzie A., Martinez F.J., Toews G.B., Moore B.B., Pinsky D.J. 2006. Obligatory role for interleukin-13 in obstructive lesion development in airway allografts. Am. J. Pathol. 169:47–60 10.2353/ajpath.2006.050975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langrish C.L., Chen Y., Blumenschein W.M., Mattson J., Basham B., Sedgwick J.D., McClanahan T., Kastelein R.A., Cua D.J. 2005. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J. Exp. Med. 201:233–240 10.1084/jem.20041257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanone S., Zheng T., Zhu Z., Liu W., Lee C.G., Ma B., Chen Q., Homer R.J., Wang J., Rabach L.A., et al. 2002. Overlapping and enzyme-specific contributions of matrix metalloproteinases-9 and -12 in IL-13-induced inflammation and remodeling. J. Clin. Invest. 110:463–474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lappalainen U., Whitsett J.A., Wert S.E., Tichelaar J.W., Bry K. 2005. Interleukin-1beta causes pulmonary inflammation, emphysema, and airway remodeling in the adult murine lung. Am. J. Respir. Cell Mol. Biol. 32:311–318 10.1165/rcmb.2004-0309OC [DOI] [PubMed] [Google Scholar]
- Lee C.G., Homer R.J., Zhu Z., Lanone S., Wang X., Koteliansky V., Shipley J.M., Gotwals P., Noble P., Chen Q., et al. 2001. Interleukin-13 induces tissue fibrosis by selectively stimulating and activating transforming growth factor beta(1). J. Exp. Med. 194:809–821 10.1084/jem.194.6.809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.G., Hartl D., Lee G.R., Koller B., Matsuura H., Da Silva C.A., Sohn M.H., Cohn L., Homer R.J., Kozhich A.A., et al. 2009. Role of breast regression protein 39 (BRP-39)/chitinase 3-like-1 in Th2 and IL-13-induced tissue responses and apoptosis. J. Exp. Med. 206:1149–1166 10.1084/jem.20081271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R.M. 2008. Oxidative stress, plasminogen activator inhibitor 1, and lung fibrosis. Antioxid. Redox Signal. 10:303–319 10.1089/ars.2007.1903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu G., Friggeri A., Yang Y., Milosevic J., Ding Q., Thannickal V.J., Kaminski N., Abraham E. 2010. miR-21 mediates fibrogenic activation of pulmonary fibroblasts and lung fibrosis. J. Exp. Med. 207:1589–1597 10.1084/jem.20100035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovgren A.K., Kovacs J.J., Xie T., Potts E.N., Li Y., Foster W.M., Liang J., Meltzer E.B., Jiang D., Lefkowitz R.J., Noble P.W. 2011. beta-arrestin deficiency protects against pulmonary fibrosis in mice and prevents fibroblast invasion of extracellular matrix. Sci. Transl. Med. 3:74ra23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupardus P.J., Birnbaum M.E., Garcia K.C. 2010. Molecular basis for shared cytokine recognition revealed in the structure of an unusually high affinity complex between IL-13 and IL-13Ralpha2. Structure. 18:332–342 10.1016/j.str.2010.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma B., Zhu Z., Homer R.J., Gerard C., Strieter R., Elias J.A. 2004. The C10/CCL6 chemokine and CCR1 play critical roles in the pathogenesis of IL-13-induced inflammation and remodeling. J. Immunol. 172:1872–1881 [DOI] [PubMed] [Google Scholar]
- Madala S.K., Pesce J.T., Ramalingam T.R., Wilson M.S., Minnicozzi S., Cheever A.W., Thompson R.W., Mentink-Kane M.M., Wynn T.A. 2010. MMP12-deficiency augments extracellular matrix degrading metalloproteinases and attenuates IL-13-dependent fibrosis. J. Immunol. 184:3955–3963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng F., Henson R., Wehbe-Janek H., Ghoshal K., Jacob S.T., Patel T. 2007. MicroRNA-21 regulates expression of the PTEN tumor suppressor gene in human hepatocellular cancer. Gastroenterology. 133:647–658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milam J.E., Keshamouni V.G., Phan S.H., Hu B., Gangireddy S.R., Hogaboam C.M., Standiford T.J., Thannickal V.J., Reddy R.C. 2008. PPAR-gamma agonists inhibit profibrotic phenotypes in human lung fibroblasts and bleomycin-induced pulmonary fibrosis. Am. J. Physiol. Lung Cell. Mol. Physiol. 294:L891–L901 10.1152/ajplung.00333.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyazaki Y., Araki K., Vesin C., Garcia I., Kapanci Y., Whitsett J.A., Piguet P.F., Vassalli P. 1995. Expression of a tumor necrosis factor-alpha transgene in murine lung causes lymphocytic and fibrosing alveolitis. A mouse model of progressive pulmonary fibrosis. J. Clin. Invest. 96:250–259 10.1172/JCI118029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore B.B., Hogaboam C.M. 2008. Murine models of pulmonary fibrosis. Am. J. Physiol. Lung Cell. Mol. Physiol. 294:L152–L160 10.1152/ajplung.00313.2007 [DOI] [PubMed] [Google Scholar]
- Moore B.B., Paine R., III, Christensen P.J., Moore T.A., Sitterding S., Ngan R., Wilke C.A., Kuziel W.A., Toews G.B. 2001. Protection from pulmonary fibrosis in the absence of CCR2 signaling. J. Immunol. 167:4368–4377 [DOI] [PubMed] [Google Scholar]
- Moore B.B., Kolodsick J.E., Thannickal V.J., Cooke K., Moore T.A., Hogaboam C., Wilke C.A., Toews G.B. 2005. CCR2-mediated recruitment of fibrocytes to the alveolar space after fibrotic injury. Am. J. Pathol. 166:675–684 10.1016/S0002-9440(10)62289-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore B.B., Murray L., Das A., Wilke C.A., Herrygers A.B., Toews G.B. 2006. The role of CCL12 in the recruitment of fibrocytes and lung fibrosis. Am. J. Respir. Cell Mol. Biol. 35:175–181 10.1165/rcmb.2005-0239OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L.A., Argentieri R.L., Farrell F.X., Bracht M., Sheng H., Whitaker B., Beck H., Tsui P., Cochlin K., Evanoff H.L., et al. 2008. Hyper-responsiveness of IPF/UIP fibroblasts: interplay between TGFbeta1, IL-13 and CCL2. Int. J. Biochem. Cell Biol. 40:2174–2182 10.1016/j.biocel.2008.02.016 [DOI] [PubMed] [Google Scholar]
- Nagase T., Uozumi N., Ishii S., Kita Y., Yamamoto H., Ohga E., Ouchi Y., Shimizu T. 2002. A pivotal role of cytosolic phospholipase A(2) in bleomycin-induced pulmonary fibrosis. Nat. Med. 8:480–484 10.1038/nm0502-480 [DOI] [PubMed] [Google Scholar]
- Naik E., Dixit V.M. 2011. Mitochondrial reactive oxygen species drive proinflammatory cytokine production. J. Exp. Med. 208:417–420 10.1084/jem.20110367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nana-Sinkam S.P., Hunter M.G., Nuovo G.J., Schmittgen T.D., Gelinas R., Galas D., Marsh C.B. 2009. Integrating the MicroRNome into the study of lung disease. Am. J. Respir. Crit. Care Med. 179:4–10 10.1164/rccm.200807-1042PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oga T., Matsuoka T., Yao C., Nonomura K., Kitaoka S., Sakata D., Kita Y., Tanizawa K., Taguchi Y., Chin K., et al. 2009. Prostaglandin F(2alpha) receptor signaling facilitates bleomycin-induced pulmonary fibrosis independently of transforming growth factor-beta. Nat. Med. 15:1426–1430 10.1038/nm.2066 [DOI] [PubMed] [Google Scholar]
- Ortiz L.A., Dutreil M., Fattman C., Pandey A.C., Torres G., Go K., Phinney D.G. 2007. Interleukin 1 receptor antagonist mediates the antiinflammatory and antifibrotic effect of mesenchymal stem cells during lung injury. Proc. Natl. Acad. Sci. USA. 104:11002–11007 10.1073/pnas.0704421104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandit K.V., Corcoran D., Yousef H., Yarlagadda M., Tzouvelekis A., Gibson K.F., Konishi K., Yousem S.A., Singh M., Handley D., et al. 2010. Inhibition and role of let-7d in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 182:220–229 10.1164/rccm.200911-1698OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park G.Y., Christman J.W. 2006. Involvement of cyclooxygenase-2 and prostaglandins in the molecular pathogenesis of inflammatory lung diseases. Am. J. Physiol. Lung Cell. Mol. Physiol. 290:L797–L805 10.1152/ajplung.00513.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S.W., Ahn M.H., Jang H.K., Jang A.S., Kim D.J., Koh E.S., Park J.S., Uh S.T., Kim Y.H., Park J.S., et al. 2009. Interleukin-13 and its receptors in idiopathic interstitial pneumonia: clinical implications for lung function. J. Korean Med. Sci. 24:614–620 10.3346/jkms.2009.24.4.614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesce J., Kaviratne M., Ramalingam T.R., Thompson R.W., Urban J.F., Jr, Cheever A.W., Young D.A., Collins M., Grusby M.J., Wynn T.A. 2006. The IL-21 receptor augments Th2 effector function and alternative macrophage activation. J. Clin. Invest. 116:2044–2055 10.1172/JCI27727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesce J.T., Ramalingam T.R., Mentink-Kane M.M., Wilson M.S., El Kasmi K.C., Smith A.M., Thompson R.W., Cheever A.W., Murray P.J., Wynn T.A. 2009. Arginase-1-expressing macrophages suppress Th2 cytokine-driven inflammation and fibrosis. PLoS Pathog. 5:e1000371 10.1371/journal.ppat.1000371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters-Golden M., Bailie M., Marshall T., Wilke C., Phan S.H., Toews G.B., Moore B.B. 2002. Protection from pulmonary fibrosis in leukotriene-deficient mice. Am. J. Respir. Crit. Care Med. 165:229–235 [DOI] [PubMed] [Google Scholar]
- Phillips R.J., Burdick M.D., Hong K., Lutz M.A., Murray L.A., Xue Y.Y., Belperio J.A., Keane M.P., Strieter R.M. 2004. Circulating fibrocytes traffic to the lungs in response to CXCL12 and mediate fibrosis. J. Clin. Invest. 114:438–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piguet P.F., Vesin C. 1994. Treatment by human recombinant soluble TNF receptor of pulmonary fibrosis induced by bleomycin or silica in mice. Eur. Respir. J. 7:515–518 10.1183/09031936.94.07030515 [DOI] [PubMed] [Google Scholar]
- Piguet P.F., Collart M.A., Grau G.E., Sappino A.P., Vassalli P. 1990. Requirement of tumour necrosis factor for development of silica-induced pulmonary fibrosis. Nature. 344:245–247 10.1038/344245a0 [DOI] [PubMed] [Google Scholar]
- Piguet P.F., Ribaux C., Karpuz V., Grau G.E., Kapanci Y. 1993. Expression and localization of tumor necrosis factor-alpha and its mRNA in idiopathic pulmonary fibrosis. Am. J. Pathol. 143:651–655 [PMC free article] [PubMed] [Google Scholar]
- Prasse A., Pechkovsky D.V., Toews G.B., Jungraithmayr W., Kollert F., Goldmann T., Vollmer E., Müller-Quernheim J., Zissel G. 2006. A vicious circle of alveolar macrophages and fibroblasts perpetuates pulmonary fibrosis via CCL18. Am. J. Respir. Crit. Care Med. 173:781–792 10.1164/rccm.200509-1518OC [DOI] [PubMed] [Google Scholar]
- Prasse A., Probst C., Bargagli E., Zissel G., Toews G.B., Flaherty K.R., Olschewski M., Rottoli P., Müller-Quernheim J. 2009. Serum CC-chemokine ligand 18 concentration predicts outcome in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 179:717–723 10.1164/rccm.200808-1201OC [DOI] [PubMed] [Google Scholar]
- Raghu G., Brown K.K., Costabel U., Cottin V., du Bois R.M., Lasky J.A., Thomeer M., Utz J.P., Khandker R.K., McDermott L., Fatenejad S. 2008. Treatment of idiopathic pulmonary fibrosis with etanercept: an exploratory, placebo-controlled trial. Am. J. Respir. Crit. Care Med. 178:948–955 10.1164/rccm.200709-1446OC [DOI] [PubMed] [Google Scholar]
- Ramalingam T.R., Pesce J.T., Sheikh F., Cheever A.W., Mentink-Kane M.M., Wilson M.S., Stevens S., Valenzuela D.M., Murphy A.J., Yancopoulos G.D., et al. 2008. Unique functions of the type II interleukin 4 receptor identified in mice lacking the interleukin 13 receptor alpha1 chain. Nat. Immunol. 9:25–33 10.1038/ni1544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramalingam T.R., Pesce J.T., Mentink-Kane M.M., Madala S., Cheever A.W., Comeau M.R., Ziegler S.F., Wynn T.A. 2009. Regulation of helminth-induced Th2 responses by thymic stromal lymphopoietin. J. Immunol. 182:6452–6459 10.4049/jimmunol.0900181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos C., Montaño M., García-Alvarez J., Ruiz V., Uhal B.D., Selman M., Pardo A. 2001. Fibroblasts from idiopathic pulmonary fibrosis and normal lungs differ in growth rate, apoptosis, and tissue inhibitor of metalloproteinases expression. Am. J. Respir. Cell Mol. Biol. 24:591–598 [DOI] [PubMed] [Google Scholar]
- Rankin J.A., Picarella D.E., Geba G.P., Temann U.A., Prasad B., DiCosmo B., Tarallo A., Stripp B., Whitsett J., Flavell R.A. 1996. Phenotypic and physiologic characterization of transgenic mice expressing interleukin 4 in the lung: lymphocytic and eosinophilic inflammation without airway hyperreactivity. Proc. Natl. Acad. Sci. USA. 93:7821–7825 10.1073/pnas.93.15.7821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rankin A.L., Mumm J.B., Murphy E., Turner S., Yu N., McClanahan T.K., Bourne P.A., Pierce R.H., Kastelein R., Pflanz S. 2010. IL-33 induces IL-13-dependent cutaneous fibrosis. J. Immunol. 184:1526–1535 10.4049/jimmunol.0903306 [DOI] [PubMed] [Google Scholar]
- Reiman R.M., Thompson R.W., Feng C.G., Hari D., Knight R., Cheever A.W., Rosenberg H.F., Wynn T.A. 2006. Interleukin-5 (IL-5) augments the progression of liver fibrosis by regulating IL-13 activity. Infect. Immun. 74:1471–1479 10.1128/IAI.74.3.1471-1479.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders Y.Y., Pardo A., Selman M., Nuovo G.J., Tollefsbol T.O., Siegal G.P., Hagood J.S. 2008. Thy-1 promoter hypermethylation: a novel epigenetic pathogenic mechanism in pulmonary fibrosis. Am. J. Respir. Cell Mol. Biol. 39:610–618 10.1165/rcmb.2007-0322OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz J., Owyang A., Oldham E., Song Y., Murphy E., McClanahan T.K., Zurawski G., Moshrefi M., Qin J., Li X., et al. 2005. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 23:479–490 10.1016/j.immuni.2005.09.015 [DOI] [PubMed] [Google Scholar]
- Selman M., King T.E., Pardo A.; American Thoracic Society; European Respiratory Society; American College of Chest Physicians 2001. Idiopathic pulmonary fibrosis: prevailing and evolving hypotheses about its pathogenesis and implications for therapy. Ann. Intern. Med. 134:136–151 [DOI] [PubMed] [Google Scholar]
- Shao D.D., Suresh R., Vakil V., Gomer R.H., Pilling D. 2008. Pivotal Advance: Th-1 cytokines inhibit, and Th-2 cytokines promote fibrocyte differentiation. J. Leukoc. Biol. 83:1323–1333 10.1189/jlb.1107782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sime P.J. 2008. The antifibrogenic potential of PPARgamma ligands in pulmonary fibrosis. J. Investig. Med. 56:534–538 [DOI] [PubMed] [Google Scholar]
- Simonian P.L., Roark C.L., Wehrmann F., Lanham A.K., Diaz del Valle F., Born W.K., O’Brien R.L., Fontenot A.P. 2009. Th17-polarized immune response in a murine model of hypersensitivity pneumonitis and lung fibrosis. J. Immunol. 182:657–665 10.4049/jimmunol.0900013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonian P.L., Wehrmann F., Roark C.L., Born W.K., O’Brien R.L., Fontenot A.P. 2010. γδ T cells protect against lung fibrosis via IL-22. J. Exp. Med. 207:2239–2253 10.1084/jem.20100061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siwik D.A., Chang D.L., Colucci W.S. 2000. Interleukin-1beta and tumor necrosis factor-alpha decrease collagen synthesis and increase matrix metalloproteinase activity in cardiac fibroblasts in vitro. Circ. Res. 86:1259–1265 [DOI] [PubMed] [Google Scholar]
- Smith R.E., Strieter R.M., Phan S.H., Lukacs N.W., Huffnagle G.B., Wilke C.A., Burdick M.D., Lincoln P., Evanoff H., Kunkel S.L. 1994. Production and function of murine macrophage inflammatory protein-1 alpha in bleomycin-induced lung injury. J. Immunol. 153:4704–4712 [PubMed] [Google Scholar]
- Song E., Ouyang N., Hörbelt M., Antus B., Wang M., Exton M.S. 2000. Influence of alternatively and classically activated macrophages on fibrogenic activities of human fibroblasts. Cell. Immunol. 204:19–28 10.1006/cimm.2000.1687 [DOI] [PubMed] [Google Scholar]
- Strieter R.M., Gomperts B.N., Keane M.P. 2007. The role of CXC chemokines in pulmonary fibrosis. J. Clin. Invest. 117:549–556 10.1172/JCI30562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tager A.M., LaCamera P., Shea B.S., Campanella G.S., Selman M., Zhao Z., Polosukhin V., Wain J., Karimi-Shah B.A., Kim N.D., et al. 2008. The lysophosphatidic acid receptor LPA1 links pulmonary fibrosis to lung injury by mediating fibroblast recruitment and vascular leak. Nat. Med. 14:45–54 10.1038/nm1685 [DOI] [PubMed] [Google Scholar]
- Thannickal V.J., Toews G.B., White E.S., Lynch J.P., III, Martinez F.J. 2004. Mechanisms of pulmonary fibrosis. Annu. Rev. Med. 55:395–417 10.1146/annurev.med.55.091902.103810 [DOI] [PubMed] [Google Scholar]
- Thavarajah K., Wu P., Rhew E.J., Yeldandi A.K., Kamp D.W. 2009. Pulmonary complications of tumor necrosis factor-targeted therapy. Respir. Med. 103:661–669 10.1016/j.rmed.2009.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiery J.P., Sleeman J.P. 2006. Complex networks orchestrate epithelial-mesenchymal transitions. Nat. Rev. Mol. Cell Biol. 7:131–142 10.1038/nrm1835 [DOI] [PubMed] [Google Scholar]
- Thompson R.W., Pesce J.T., Ramalingam T., Wilson M.S., White S., Cheever A.W., Ricklefs S.M., Porcella S.F., Li L., Ellies L.G., Wynn T.A. 2008. Cationic amino acid transporter-2 regulates immunity by modulating arginase activity. PLoS Pathog. 4:e1000023 10.1371/journal.ppat.1000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thum T., Gross C., Fiedler J., Fischer T., Kissler S., Bussen M., Galuppo P., Just S., Rottbauer W., Frantz S., et al. 2008. MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature. 456:980–984 10.1038/nature07511 [DOI] [PubMed] [Google Scholar]
- Tokuda A., Itakura M., Onai N., Kimura H., Kuriyama T., Matsushima K. 2000. Pivotal role of CCR1-positive leukocytes in bleomycin-induced lung fibrosis in mice. J. Immunol. 164:2745–2751 [DOI] [PubMed] [Google Scholar]
- Wilborn J., Bailie M., Coffey M., Burdick M., Strieter R., Peters-Golden M. 1996. Constitutive activation of 5-lipoxygenase in the lungs of patients with idiopathic pulmonary fibrosis. J. Clin. Invest. 97:1827–1836 10.1172/JCI118612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson M.S., Elnekave E., Mentink-Kane M.M., Hodges M.G., Pesce J.T., Ramalingam T.R., Thompson R.W., Kamanaka M., Flavell R.A., Keane-Myers A., et al. 2007. IL-13Ralpha2 and IL-10 coordinately suppress airway inflammation, airway-hyperreactivity, and fibrosis in mice. J. Clin. Invest. 117:2941–2951 10.1172/JCI31546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson M.S., Madala S.K., Ramalingam T.R., Gochuico B.R., Rosas I.O., Cheever A.W., Wynn T.A. 2010. Bleomycin and IL-1β–mediated pulmonary fibrosis is IL-17A dependent. J. Exp. Med. 207:535–552 10.1084/jem.20092121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff D., Reichenberger F., Steiner B., Kahl C., Leithäuser M., Skibbe T., Friedrich T., Terpe H., Helbig W., Freund M. 2002. Progressive interstitial fibrosis of the lung in sclerodermoid chronic graft-versus-host disease. Bone Marrow Transplant. 29:357–360 10.1038/sj.bmt.1703386 [DOI] [PubMed] [Google Scholar]
- Wynn T.A. 2004. Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat. Rev. Immunol. 4:583–594 10.1038/nri1412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wynn T.A. 2007. Common and unique mechanisms regulate fibrosis in various fibroproliferative diseases. J. Clin. Invest. 117:524–529 10.1172/JCI31487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wynn T.A., Barron L. 2010. Macrophages: master regulators of inflammation and fibrosis. Semin. Liver Dis. 30:245–257 10.1055/s-0030-1255354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wynn T.A., Cheever A.W., Jankovic D., Poindexter R.W., Caspar P., Lewis F.A., Sher A. 1995. An IL-12-based vaccination method for preventing fibrosis induced by schistosome infection. Nature. 376:594–596 10.1038/376594a0 [DOI] [PubMed] [Google Scholar]
- Xia H., Diebold D., Nho R., Perlman D., Kleidon J., Kahm J., Avdulov S., Peterson M., Nerva J., Bitterman P., Henke C. 2008. Pathological integrin signaling enhances proliferation of primary lung fibroblasts from patients with idiopathic pulmonary fibrosis. J. Exp. Med. 205:1659–1672 10.1084/jem.20080001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang G., Volk A., Petley T., Emmell E., Giles-Komar J., Shang X., Li J., Das A.M., Shealy D., Griswold D.E., Li L. 2004. Anti-IL-13 monoclonal antibody inhibits airway hyperresponsiveness, inflammation and airway remodeling. Cytokine. 28:224–232 10.1016/j.cyto.2004.08.007 [DOI] [PubMed] [Google Scholar]
- Ye P., Rodriguez F.H., Kanaly S., Stocking K.L., Schurr J., Schwarzenberger P., Oliver P., Huang W., Zhang P., Zhang J., et al. 2001. Requirement of interleukin 17 receptor signaling for lung CXC chemokine and granulocyte colony-stimulating factor expression, neutrophil recruitment, and host defense. J. Exp. Med. 194:519–527 10.1084/jem.194.4.519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A., Koduri G., Batley M., Kulinskaya E., Gough A., Norton S., Dixey J.; Early Rheumatoid Arthritis Study (ERAS) group 2007. Mortality in rheumatoid arthritis. Increased in the early course of disease, in ischaemic heart disease and in pulmonary fibrosis. Rheumatology (Oxford). 46:350–357 10.1093/rheumatology/kel253 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Lee T.C., Guillemin B., Yu M.C., Rom W.N. 1993. Enhanced IL-1 beta and tumor necrosis factor-alpha release and messenger RNA expression in macrophages from idiopathic pulmonary fibrosis or after asbestos exposure. J. Immunol. 150:4188–4196 [PubMed] [Google Scholar]
- Zheng T., Liu W., Oh S.Y., Zhu Z., Hu B., Homer R.J., Cohn L., Grusby M.J., Elias J.A. 2008. IL-13 receptor alpha2 selectively inhibits IL-13-induced responses in the murine lung. J. Immunol. 180:522–529 [DOI] [PubMed] [Google Scholar]
- Zhou B., Comeau M.R., De Smedt T., Liggitt H.D., Dahl M.E., Lewis D.B., Gyarmati D., Aye T., Campbell D.J., Ziegler S.F. 2005. Thymic stromal lymphopoietin as a key initiator of allergic airway inflammation in mice. Nat. Immunol. 6:1047–1053 10.1038/ni1247 [DOI] [PubMed] [Google Scholar]
- Zhou R., Yazdi A.S., Menu P., Tschopp J. 2011. A role for mitochondria in NLRP3 inflammasome activation. Nature. 469:221–225 10.1038/nature09663 [DOI] [PubMed] [Google Scholar]
- Zhu Z., Homer R.J., Wang Z., Chen Q., Geba G.P., Wang J., Zhang Y., Elias J.A. 1999. Pulmonary expression of interleukin-13 causes inflammation, mucus hypersecretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. J. Clin. Invest. 103:779–788 10.1172/JCI5909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z., Ma B., Zheng T., Homer R.J., Lee C.G., Charo I.F., Noble P., Elias J.A. 2002. IL-13-induced chemokine responses in the lung: role of CCR2 in the pathogenesis of IL-13-induced inflammation and remodeling. J. Immunol. 168:2953–2962 [DOI] [PubMed] [Google Scholar]
- Zhu Z., Zheng T., Homer R.J., Kim Y.K., Chen N.Y., Cohn L., Hamid Q., Elias J.A. 2004. Acidic mammalian chitinase in asthmatic Th2 inflammation and IL-13 pathway activation. Science. 304:1678–1682 10.1126/science.1095336 [DOI] [PubMed] [Google Scholar]
- Zhu S., Si M.L., Wu H., Mo Y.Y. 2007. MicroRNA-21 targets the tumor suppressor gene tropomyosin 1 (TPM1). J. Biol. Chem. 282:14328–14336 10.1074/jbc.M611393200 [DOI] [PubMed] [Google Scholar]
- Zhu S., Wu H., Wu F., Nie D., Sheng S., Mo Y.Y. 2008. MicroRNA-21 targets tumor suppressor genes in invasion and metastasis. Cell Res. 18:350–359 10.1038/cr.2008.24 [DOI] [PubMed] [Google Scholar]
- Zuo F., Kaminski N., Eugui E., Allard J., Yakhini Z., Ben-Dor A., Lollini L., Morris D., Kim Y., DeLustro B., et al. 2002. Gene expression analysis reveals matrilysin as a key regulator of pulmonary fibrosis in mice and humans. Proc. Natl. Acad. Sci. USA. 99:6292–6297 10.1073/pnas.092134099 [DOI] [PMC free article] [PubMed] [Google Scholar]