There are no therapeutic guidelines regarding ambulation for older adults hospitalized for acute illness.1 The importance of early ambulation to recovery in other patient populations is well established.2,3 For example, time to ambulation after hip fracture surgery is a predictor of complications such as prolonged length of stay (LOS).4 In the present study, we examined the association between ambulation and LOS in geriatric patients admitted for acute illnesses. We hypothesized that increase in ambulation within the 48 hours after admission would predict LOS after adjusting for risk factors.
Methods
Patients 65 years or older admitted to an Acute Care for Elders unit were studied. A Step Activity Monitor (SAM) was placed on patients at admission, and participants were instructed to walk as usual. Data were collected over 4 months in 2009. Patients with an orthopedic surgical diagnosis or a contraindication to wearing the SAM (eg, bilateral leg infection or severe edema) were excluded. Patients (N=162) who spent 2 or more days in hospital were included in the analysis. Institutional review board approval was obtained.
The SAM is a pager-sized accelerometer attached at the ankle. It will not record leg movements in bed and has been shown to be 98% accurate in clinical populations.5–7 Steps were recorded in 1-minute intervals synchronized to a 24-hour clock, resulting in a temporal series of 1440 observations per day.
Total steps were summed for each 24-hour day. A step change score was calculated using the difference in step totals between the first and second day. Mean daily steps were calculated using the number of complete days the SAM was worn. Demographic and clinical characteristics were obtained from medical records.
Generalized estimating equation models were used to examine the association between step change score and LOS with and without adjustment for covariates. The best fitting model was the one in which LOS was discontinuous with a large drop at 600 steps or more. We used χ2 and t tests to examine differences between patients who increased their walking by 600 steps or more from the first to second day vs those who did not. Statistical analyses were performed using SAS version 9.2 software (SAS Institute Inc, Cary, North Carolina). Testing was 2-sided, and P<.05 was considered significant.
Results
Mean (SD) age was 77.4 (7.7) years; 55.7% were women; mean (SD) body mass index was 26.5 (6.5) (calculated as weight in kilograms divided by height in meters squared); and 21.4% reported a fall in the past year. Reasons for admission included cardiopulmonary (30.8%), infections (25.2%), and gastrointestinal (16.4%), neurologic (6.2%), and other (21.4%) complications. The all patient refined diagnosis related group severity of illness classification8 was minor (10.6%), moderate (43.8%), major (36.2%), and extreme (9.4%). Mean (SD) LOS was 6.1 (2.9) days (range, 4–26 days).
Prior to admission, 52.8% were independent ambulators, 35.2% used a cane or walker, and 12.0% required help from another person. Ambulation was restricted at admission by tubing and/or monitoring equipment in 28.9% of patients. Physician activity orders at admission were “as tolerated” (53.0%), “ambulate with assist” (16.6%), and “bed rest” (29.6%).
Patients averaged 662.1 (SD, 784.9) steps per day. Mean (SD) number of steps for the first complete day was 540.6 (812.9) and 737.0 (904.1) for the second day. Mean (SD) step change score between the first and second day was 196.5 steps (669.3) (range, −1546.0 to 2378.0).
Only sex (β=269.4 [SE, 112.8]; P=.02) was significantly associated with the step change score; men increased their step count significantly more than women.
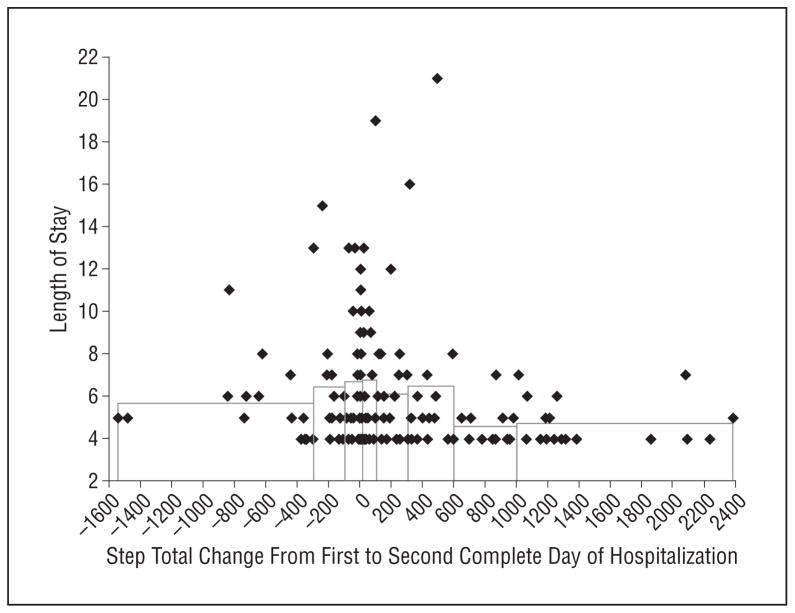
The Figure shows the unadjusted step total change scores and step change score deciles by LOS. Patients with low or negative change scores had longer LOS. The unadjusted mean difference in LOS between those who increased their step total by 600 steps or more and those who did not was 1.73 days (95% confidence interval, 0.60–2.85). After adjusting for demographic and clinical characteristics, the difference between groups was 2.13 days (95% confidence interval, 1.05–3.97).
Figure.
Unadjusted step total change scores and step change score deciles by length of stay. Bars are mean length of stay for change score deciles: −300 steps or less; −300 to −100 steps; −100 to 0 steps; 0 to 99 steps; 100 to 299 steps; 300 to 599 steps; 600 to 1000 steps; and more than 1000 steps. Adjacent deciles in the range −100 to 100 steps were combined. The unadjusted mean difference in length of stay between those who increased their step total by 600 steps or more from the first to second complete day of hospitalization and those who did not was 1.73 days (95% confidence interval, 0.60 to 2.85 days); after adjusting for demographic and clinical characteristics (see “Methods” section), the difference was 2.13 days (95% confidence interval, 1.02 to 3.93 days).
We compared the 32 patients who increased their walking by 600 steps or more with all other patients. No significant differences existed by age, diagnosis, presence of tubing and/or monitoring equipment, fall history, number of comorbid conditions, or illness severity. They were more likely to be men (P=.02) and independent ambulators (P<.01) and have an admitting order of “ambulate with assist” (P=.03).
Comment
Patients who increased their walking by at least 600 steps from the first to second 24-hour day were discharged approximately 2 days earlier than those who did not. Results suggest accelerometers may be useful in creating clinical thresholds for ambulation in hospitalized persons. These thresholds may not be excessively high; 600 steps correspond to approximately 12 minutes of slow walking.9
A limitation of the study is the possibility of reverse causation. Patients who increased their step count may have been less ill. This possibility should be explored in future studies. In conclusion, level of ambulation during the first 48 hours after admission was linked to LOS in geriatric patients. These results may inform future research investigating ambulation as an intermediate measure to health outcomes like functional status, service use, and LOS.
Acknowledgments
Funding/Support: This work was funded in part by grants R01 AG031178, P30 AG017231-03, and K12 HD055929 from the National Institutes of Health.
Role of the Sponsor: The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Financial Disclosure: None reported.
Author Contributions: Dr Fisher had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Fisher, Kuo, and Graham. Acquisition of data: Fisher and Ostir. Analysis and interpretation of data: Fisher, Kuo, and Ottenbacher. Drafting of the manuscript: Fisher and Ostir. Critical revision of the manuscript for important intellectual content: Fisher, Kuo, Graham, Ottenbacher, and Ostir. Statistical analysis: Fisher and Kuo. Obtained funding: Ottenbacher and Ostir. Study supervision: Ostir.
References
- 1.Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52(8):1263–1270. doi: 10.1111/j.1532-5415.2004.52354.x. [DOI] [PubMed] [Google Scholar]
- 2.Mundy LM, Leet TL, Darst K, Schnitzler MA, Dunagan WC. Early mobilization of patients hospitalized with community-acquired pneumonia. Chest. 2003;124(3):883–889. doi: 10.1378/chest.124.3.883. [DOI] [PubMed] [Google Scholar]
- 3.Harpur JE, Conner WT, Hamilton M, et al. Controlled trial of early mobilisation and discharge from hospital in uncomplicated myocardial infarction. Lancet. 1971;2(7738):1331–1334. doi: 10.1016/s0140-6736(71)92357-9. [DOI] [PubMed] [Google Scholar]
- 4.Kamel HK, Iqbal MA, Mogallapu R, Maas D, Hoffmann RG. Time to ambulation after hip fracture surgery: relation to hospitalization outcomes. J Gerontol A Biol Sci Med Sci. 2003;58(11):1042–1045. doi: 10.1093/gerona/58.11.m1042. [DOI] [PubMed] [Google Scholar]
- 5.Storti KL, Pettee KK, Brach JS, Talkowski JB, Richardson CR, Kriska AM. Gait speed and step-count monitor accuracy in community-dwelling older adults. Med Sci Sports Exerc. 2008;40(1):59–64. doi: 10.1249/mss.0b013e318158b504. [DOI] [PubMed] [Google Scholar]
- 6.Cavanaugh JT, Coleman KL, Gaines JM, Laing L, Morey MC. Using step activity monitoring to characterize ambulatory activity in community-dwelling older adults. J Am Geriatr Soc. 2007;55(1):120–124. doi: 10.1111/j.1532-5415.2006.00997.x. [DOI] [PubMed] [Google Scholar]
- 7.Foster RC, Lanningham-Foster LM, Manohar C, et al. Precision and accuracy of an ankle-worn accelerometer-based pedometer in step counting and energy expenditure. Prev Med. 2005;41(3–4):778–783. doi: 10.1016/j.ypmed.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Averill RF, Goldfield NI, Muldoon J, Steinbeck BA, Grant TM. A closer look at all-patient refined DRGs. J AHIMA. 2002;73(1):46–50. [PubMed] [Google Scholar]
- 9.Perry J. Gait Analysis. Thorofare, NJ: SLACK Inc; 1992. [Google Scholar]