Abstract
Background
The water method is easy-to-learn and improves colonoscopy outcomes. Dye-spray chromoendoscopy enhances ADR but has not been widely accepted for routine application in screening or surveillance colonoscopy.
Hypothesis
With dye added to the water used in the water method, ADR can be enhanced compared with the water or air method alone.
Objective
To compare ADR determined by the air method, water method alone, and water method with indigo carmine (0.008%) added.
Design
Review of prospectively collected data in a performance improvement program.
Setting
VA endoscopy unit.
Patient
Screening or surveillance colonoscopy.
Methods
Patients (n=50/group) underwent colonoscopy with each of the three methods. Water method involved warm water infusion in lieu of air insufflation coupled with removal of residual air by suction and residual feces by water exchange. ADR and procedural data were collected prospectively to monitor performance.
Main Outcome Measurements
ADR.
Results
ADR in the air method, water method alone and water method with indigo carmine were 36%, 40% and 62%, respectively. Water method with indigo carmine produced significantly higher ADR than the air or water method alone (p<0.05).
Limitations
Non-randomized data, single VA site, retrospective comparison. Absence of significant difference between air and water methods could be a type II error due to small number of patients
Conclusions
The approach with indigo carmine added to the water used in the water method yielded significantly higher ADR than the water or the air method alone. The data suggest that a prospective RCT to compare the different methods is warranted.
Key words: colorectal cancer screening, optical colonoscopy, water method, chromoendoscopy, polyp, adenoma, indigo carmine
Introduction
Conventional colonoscopy involves air insufflation (air method) to distend the colonic lumen during insertion. The water method has recently been reported to be superior to air method1–9, produces less sedation medication requirement in the sedated veterans1–3, and minimizes discomfort and enhances cecal intubation in the unsedated veterans4–6. Retrospective review of data in sedated veterans showed that the water method increased adenoma detection rate (ADR).7 The pooled data of two RCT in predominantly unsedated veterans showed that the water method increased proximal diminutive adenoma detection.8 Chromoendoscopy with pan colonic or targeted dye sprays has been shown to improve detection of colonic lesions.10–12 Chromoendoscopy may be important also in the detection of non-polypoid colorectal neoplasms.13 Despite these encouraging features chromoendoscopy for screening and surveillance has not been performed routinely by endoscopists in the United States (US).10,14–16 Because the water method is easy-to-use consideration for combining it with chromoendoscopy to increase ADR may have merit. The objective of this current retrospective non-randomized review is to compare ADR in colonoscopy performed using the air method, water method alone, and water method with indigo carmine added. We test the hypothesis that with dye added to the water used in the water method, ADR can be enhanced.
Methods
Since the water method1–9 and use of chromoendoscopy10–14 were reported to have beneficial impacts, a performance improvement project evaluating their utility was carried out at the Sacramento VA Medical Center in Mather, California. Data were collected prospectively to monitor performance and analyzed retrospectively. Approval was granted by the local IRB to report the observations. Informed consent waiver was granted since the data were deidentified.
Patients received usual bowel preparation, a low-residue diet for 2 days before and 2 tablets of bisacodyl plus 1 gallon of Colyte (polyethylene glycol-electrolyte) on the day before colonoscopy.1–3 Premedication included a combination of Fentanyl, Midazolam, and Diphenhydramine for sedation.1–3 High resolution Olympus colonoscopes were used.
Air method: Air insufflation, shortening maneuvers, abdominal compression and change of patient position were used. Contact with residual feces which would smear the lens and impair the view was avoided. Cecal intubation was defined as passage of the colonoscope tip to a point proximal to the ileocecal valve so that the entire cecal caput, including the medial wall of the cecum between the ileocecal valve and appendix orifice were visible.
Water method: Further improvement to the water method was made since it was first described.1 In addition to water infusion in lieu of air insufflation to distend the colon to facilitate scope insertion, suction removal of residual air to reduce looping formation and angulations at all flexures to minimize discomfort, and removal of residual feces that obscure luminal view by water exchange were implemented. For the water method, the air pump on the light source generator (CLV 180; Olympus, Tokyo, Japan) was turned off prior to insertion of the colonoscope. Warm water (at 37 °C) was infused using a peristaltic pump (Endolav EL-100C, Cooper Surgical, Trumbull, CT, USA) with a blunt needle adaptor inserted through the biopsy channel of the colonoscope. Removal of angulations by suction of residual air collapsed the colon around the colonoscope, increasing the chance that the tip would point in the “future” lumen direction. The tip of the colonoscope was oriented towards and abutted the “slit-like lumen” ahead. The infused water opened the lumen if the orientation was correct. Incorrect orientation did not lead to opening of the lumen ahead, and water infusion was stopped. The tip of the colonoscope was pulled back away from the mucosa and redirected against the possible lumen. The colonoscope was advanced by a series of to and fro, back and forth, or repeated insertion and withdrawal motions of the shaft of the colonoscope with a torque in the direction of the expected lumen, with intermittent water infusion. Since air was not used to find the lumen, suspended residual feces obscuring the view had to be suctioned and replaced by clean water until the colonic lumen was visualized again. To minimize suction of the mucosa into the endoscope channel the water infusion was started first followed by application of suction.
The volume of water needed to clear the view (200 to 2000 ml) was kept to a minimum, but not restricted. The collapsed colonic lumen allowed the water to more adequately soak the colonic surfaces and remove the adherent stool from the colonic mucosa. The turbulence set up by the sequential infusion and suction of water in the collapsed lumen dislodged the residual feces from the surrounding mucosa in close proximity to the tip of the colonoscope. This maneuver made removal of the residual feces “easier” than washing with a single water jet in a dilated air filled colon. Most of the infused water was aspirated into the suction bottle instead of being left in the colon, and over-distension was obviated. If advancement failed, the assistant provided abdominal compression followed by changing the patient position if necessary. If the advancement was uninterrupted, no abdominal pressure or change in patient position was used. For the combined chromoendosocopy and water method, residual stool in the proximal colon (especially in patients with inadequate bowel preparation) changed the indigo carmine solution to a greenish color. Additional suction and water exchange was performed until the color of the water remained blue to “stain” the mucosa. If the appendix opening was seen under water or when the cecum was thought to be reached, the air feature was turned on to confirm the location. If the cecum had not been reached, failed intubation was recorded based on intent-to-treat (ITT) but colonoscopy was continued. Cecal intubation was defined as described above. Any residual water was suctioned on scope withdrawal to facilitate examination.
Both methods during withdrawal: Intermittent air insufflation (air pump set at high) was used to distend the colon for inspection, biopsy and polypectomy. Washing of any residual stool covered mucosa was performed by water or in the chromoendoscopy cases with diluted indigo carmine irrigation and inspection of the mucosa including examination behind folds was performed systematically as needed. After turn around in the rectum, residual air in the colon was removed by suction.
In an in vitro preparation the tip of the colonoscope was held at a distance of 1 cm from a measuring scale placed at the bottom of a beaker. Indigo carmine in water at concentrations of 0.8%, 0.08% and 0.008% was placed in the beaker. The ability to see through the blue water was recorded. The results showed that water colored by indigo carmine could be seen through using usual endoscopic light setting when the indigo carmine concentration was 0.008%. This concentration of indigo carmine was used in the combined chromoendoscopy and water method. As part of the performance improvement project, we incorporated chromoendoscopy with indigo carmine in patients undergoing water colonoscopy for colorectal cancer screening or surveillance. The combined chromoendoscopy and water method was accomplished by adding 10 ml of 0.8% indigo carmine to a liter bottle of water used with the water method without having to perform dye spray separately as previously described.10–12 A representative description of pan- and selective dye spray11 is included for comparison. For pan-chromoscopy a chromoscopy diffusion catheter was used to apply a maximum of 150 ml of 0.5% indigo carmine to the entire mucosa during withdrawal from the cecum. Chromoscopy was performed in 10 cm segments which were then re-inspected following aspiration of any excess indigo carmine forming pools in the colon.11 Selective chromoscopy (2–5 ml of indigo carmine flushed down the side port of the colonoscope followed by a 20 ml air “push”) delineated suspected mucosal lesions which had been identified by observing the mucosal signs (presence of erythema, focal pallor, hemorrhagic spots, absence of vascular network pattern, discrete mucosal unevenness, or deformity) without the prior use of chromoscopy. A minimum diagnostic extubation time from the cecum to the anus (excluding that required for interventional procedures) was set at eight minutes for all patients.11 The strict adherence to water infusion in lieu of air insufflation and meticulous removal of all residual air inside the colon permits the infused water to bathe all mucosal surfaces. The contact of feces adherent to the mucosal surface with water in the collapsed lumen facilitated suspension of residual feces for removal by suction to clear the colonic lumen. The ‘soaking’ effect of the water also permitted the dye to contact all of the mucosal surfaces. With adequate exchange of water, the surface mucosal irregularities such as polyps (including adenomas) could be highlighted by the diluted indigo carmine solution. This was in contrary to the staining of lesions when a much higher concentration of indigo carmine was used with the dye spraying technique.
The ADR (proportion of subjects with at least one adenoma) in the study group (combined chromoendoscopy and water method) was compared with two historical control groups of screening or surveillance patients, one examined with the usual air method, and another with the water method alone. The tabulated data were analyzed using chi-squared analysis or unpaired t-test A p value of <0.05 was considered to be significant.
Results
The comparison of patient age, colonoscopy indication (screening vs. surveillance), ADR and total procedure time for each of the three methods are shown in Table 1. There was no difference in the mean age. The ADR provided by the chromoendoscopy with indigo carmine combined with the water method (62%) was significantly higher than either the air (36%) or water method applied alone (40%). The procedure time was also significantly longer when the water combined with indigo carmine method was used. The characteristic features of the adenomas (size and location) are shown in Table 2A and 2B, respectively. There were more adenomas detected in the colon at or proximal to the splenic flexure in the water method groups, particularly diminutive one that were <10 mm in size (Figures 1A, 1B, 2 and 3).
Table 1.
Comparison of adenoma detection rates between three different methods for screening and surveillance colonoscopy
| Historical Cohorts | |||
| Air Method (n=50) | Water Method (n=50) | Water with indigo carmine (n=50) | |
| Male sex, % | 100 | 98 | 98 |
| Mean Age | 58 (7) | 61 (8) | 61 (7) |
| Screening | 39 | 37 | 34 |
| Surveillance | 11 | 13 | 16 |
| Body mass index | 30 (6) | 30 (6) | 29 (5) |
| Overall ADR (proportion of patient with at least 1 adenoma) | 36% | 40% | 62%a,b |
| Total procedure time (min) | 24 (9) | 28 (13) | 32 (7)a,b |
Data as mean (SD); avs. water bvs. air; p<0.05, Chi square or ANOVA with contrasts.
Table 2A.
Size of adenomas
| Historical Cohorts | |||||||||
| Air Method (n=50) | Water Method (n=50) | Water with indigo carmine (n=50) | |||||||
| Adenoma | Proximal | Distal | Total | Proximal | Distal | Total | Proximal | Distal | Total |
| <6mm | 15 | 11 | 26 | 25 | 7 | 32 | 25 | 13 | 38 |
| 6–9mm | 2 | 3 | 5 | 5 | 0 | 5 | 6 | 6 | 12 |
| ≥10mm | 3 | 5 | 8 | 4 | 4 | 8 | 10 | 7 | 17 |
| Total | 20 | 19 | 39 | 34 | 11 | 45 | 41 | 26 | 67 |
Data are number of adenoma of the size category tabulated. Proximal = at or proximal to the splenic flexure. Distal = distal to the splenic flexure.
Table 2B.
Location of adenomas
| Historical Cohorts | |||
| Number of adenoma in the following locations | Air Method (n=50) | Water Method (n=50) | Water with indigo carmine (n=50) |
| Cecum | 1 | 4 | 8 |
| Ascending | 6 | 14 | 20 |
| Transverse | 13 | 16 | 13 |
| Descending | 12 | 6 | 14 |
| Sigmoid | 2 | 3 | 7 |
| Rectum | 5 | 2 | 5 |
Figure 1.
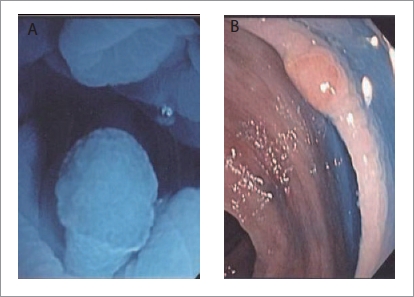
A: Small adenoma in ascending colon seen under blue water. B: same polyp seen after suction removal of water and air insufflation.
Figure 2.

Large flat polyp (tubular adenoma) in proximal colon (outline of polyp is highlighted by the blue dye)
Figure 3.
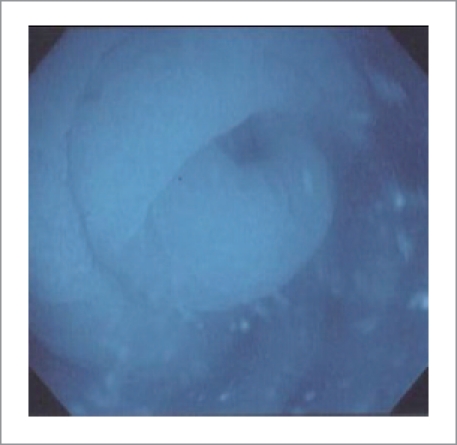
Appendix opening seen under blue water
Discussions
Case-control reports indicated that colonoscopy failed to reduce incident cancers and cancer mortality in the right colon17–19. Adenoma detection rate (ADR), but not cecal intubation rate was an independent predictor of the risk of interval colorectal cancer after screening colonoscopy.20 The impact of recent development in technology and techniques on ADR has been highly variable and inconclusive. These include colonoscopy performed with high- definition, wide-angle endoscope15,21–25; narrow band imaging26–28; transparent hood attached to the tip of the colonoscope26,29,30 withdrawal time >6 min31,32 or modified (e.g. split-dose) bowel preparation33,34. An optimal “colonoscopist-controlled” technique to enhance ADR and minimize “missed” right-sided lesions is desirable.
A major limitation of the conventional dye-spray chromoendoscopy method is poor bowel preparation. Proportion of patient excluded varied from 4%35, 5%36, 8%37 to 9%15. Intent-to-treat analysis would have dictated an adjustment of the ADR reported in each of these studies by the proportion of patients excluded due to poor bowel preparation (see values in [ ] in Table 3). The results of the current report indicate chromoendoscopy added to the water method is feasible showing an ADR of 62%. The salvage cleansing effect of the water exchange, which is an integral part of the water method4,8 obviated the need to exclude any patients because of poor bowel preparation even when indigo carmine was added to the water. The water with indigo carmine could provide cleansing of the colon with suboptimal bowel preparation. Coupled with dye-staining, an enhanced detection of adenomas was quite evident even with intent-to-treat analysis.
Table 3.
Comparison of ADR in the current study and those reported in the literature
| Overall ADR air method | 36% | Current report |
| Overall ADR water method | 40% | |
| Overall ADR water with indigo carmine method (intent-to-treat without poor bowel prep exclusion) | 62% | |
| Representative published overall ADR | ADR | Literature Reference |
| Narrow band imaging | 23% | 27 |
| High definition colonoscopes | 24.7% | 23 |
| Withdrawal time >6 min | 28.3% | 32 |
| High definition colonoscopes | 28.8% | 22 |
| Chromoendoscopy and standard colonoscope (after excluding 4% with poor bowel preparation) | 33.6% [29.6%] | 35 |
| Chromoendoscopy and standard colonoscope (after excluding 5% with poor bowel preparation) | 35.4% [30.4%] | 36 |
| High resolution colonoscope | 42 | 13 |
| White light and high definition colonoscope | 41–57% | 15 |
| Narrow band imaging | 51% | 24 |
| Chromoendoscopy and high definition colonoscope (after excluding 9% with poor bowel preparation) | 55.5% [46.5%] | 15 |
| Narrow band imaging | 57.3% | 28 |
| White light | 58.3% | 28 |
| High definition colonoscope | 60.4% | 21 |
| Chromoendoscopy (after excluding 8% with poor bowel preparation) | 66.2% [58.2%] | 37 |
Values in [ ] indicate results based on intent-to-treat analysis without excluding the patients with suboptimal bowel preparation.
Recent published rates of adenoma and cancer detection are summarized in Tables 3. The ADR of 62% using the water with indigo carmine method was higher than those derived from studies using other modalities, even those obtained with high definition colonoscopes15,21–23, narrow band imaging (NBI)24,27,28 or dye spray chromoendoscopy35–37.
Conventional targeted dye-spray chromoendoscopy has been reported to require up to an average of 33 minutes in total procedure time13, 26 minutes in withdrawal time10, or a median withdrawal time of 25 minutes (range 8 – 153 min)37. The total procedure time of the water combined with indigo carmine method offers comparable procedure time [32 (7) min, mean (SD)]. The presence of residual stool required additional water irrigation and suction to maintain the blue color of the indigo carmine solution. Additional time was in fact taken up by performing biopsies of the lesions found. The water with indigo carmine method did not appear to complicate the simple and easy approach of the water method. The diluted solution of indigo carmine did not interfere with examination under water and the dye enhanced the surface irregularities and highlighted the outline of small mucosal lesions including polyps. This combined method is compatible with conventional colonoscope (not requiring high definition or NBI) and minimizes set up cost.
Prevention of colorectal cancer by detection and removal of adenomas has been the recommended practice in the US for almost 20 years.38 National guideline has recommended that endoscopists performing screening colonoscopy should detect adenomas in at least 25% of men and 15% of women age 50 years or older.39 Variability exists in the detection of adenomas by endoscopists (Table 3).
Various methods have been proposed to improve detection of neoplastic lesions including taking adequate time for examination on scope withdrawal.32 However, adherence to mandated withdrawal time of >7 min did not increase ADR.31 The use of chromoendoscopy with dye-spraying has been shown to improve ADR. Soetikno et al.13 reported a neoplastic polyp detection rate of 42% using a targeted dye-spray technique with traditional air insufflation colonoscopy. Chromoendoscopy may be particularly useful in the detection of non-polypoid colorectal adenomas.13
Targeted or pan-colonic dye staining during colonoscopy requires the use of spray catheters14 or injection of the dye and air into the working channel of endoscope to apply a uniform mist of the staining agent onto the mucosa14. In addition, the delivery of dyes via capsule and enemas has been described.40,41 Implementation of chromoendoscopy, however, has not been adopted for routine use in screening and surveillance colonoscopy.14,16 The combination of chromoendoscopy with the water method appears to be feasible based on the observation in the current study. The limitations of the current study include non-randomized data, single VA site, retrospective comparison, and absence of significant difference between air (36%) and water (40%) methods could be affected by type II error due to small number of patients. Another study limitation is the small case number to permit analysis of the impact on detection of advanced adenoma. It is not clear whether the lesions identified with indigo carmine might have been missed with the other methods. Adenomas were detected in 31 of 50 patients (62%), a detection rate much higher than with the air or water method alone. Whether the potential benefits of a higher ADR provided by combining chromoendoscopy with the water method will offset the added cost of longer procedure times deserves to be evaluated in future studies.
Acknowledgement
The study is support by the C.W. Law Research Fund and the Research and Medical Services of the VANCHCS and VAGLAHS; and in part by the ACG and ASGE Clinical Research Awards.
Abbreviations
- ADR
adenoma detection rate
- NBI
narrow band imaging
- SD
standard deviations
- US
United States
- VA
Veterans Affairs
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
References
- 1.Leung JW, Mann S, Leung FW. Options for screening colonoscopy without sedation: a pilot study in United States veterans. Aliment Pharmacol Ther. 2007;26:627–631. doi: 10.1111/j.1365-2036.2007.03404.x. [DOI] [PubMed] [Google Scholar]
- 2.Leung JW, Salera R, Toomsen L, Mann S, Leung FW. Pilot feasibility study of the method of water infusion without air insufflation in sedated colonoscopy. Dig Dis Sci. 2009;54:1997–2001. doi: 10.1007/s10620-008-0576-4. [DOI] [PubMed] [Google Scholar]
- 3.Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim B, Cabrera H, et al. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009;70:505–510. doi: 10.1016/j.gie.2008.12.253. [DOI] [PubMed] [Google Scholar]
- 4.Leung FW, Aharonian HS, Leung JW, Guth PH, Jackson G. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. 2009;69:546–550. doi: 10.1016/j.gie.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, et al. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 6.Leung J, Mann S, Siao-Salera R, Ransibrahmanakul K, Lim B, Canete W, et al. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103–110. doi: 10.1016/j.gie.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 7.Leung JW, Do L, Siao-Salera RM, Parikh DA, Mann SK, Leung FW. Retrospective data showing the water method increased adenoma detection rate - a hypothesis generating observation. J Interv Gastroenterol. 2011;1:3–7. doi: 10.4161/jig.1.1.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leung FW, Leung JW, Siao-Salera RM, Mann SK. The water method significantly enhances proximal diminutive adenoma detection rate in unsedated patients. J Interv Gastroenterol. 2011;1:8–13. doi: 10.4161/jig.1.1.14587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung FW. Is there a place for sedationless colonoscopy? J Interv Gastroenterol. 2011;1:19–22. doi: 10.4161/jig.1.1.14592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Le Rhun M, Coron E, Parlier D, Nguyen JM, Canard JM, Alamdari A, et al. High resolution colonoscopy with chromoscopy versus standard colonoscopy for the detection of colonic neoplasia: a randomized study. Clin Gastroenterol Hepatol. 2006;4:349–354. doi: 10.1016/j.cgh.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Hurlstone DP, Cross SS, Slater R, Sanders DS, Brown S. Detecting diminutive colorectal lesions at colonoscopy: a randomised controlled trial of pan-colonic versus targeted chromoscopy. Gut. 2004;53:376–380. doi: 10.1136/gut.2003.029868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brooker °C, Saunders BP, Shah SG, Thapar CJ, Thomas HJ, Atkin WS, et al. Total colonic dye-spray increases the detection of diminutive adenomas during routine colonoscopy: a randomized controlled trial. Gastrointest Endosc. 2002;56:333–338. doi: 10.1016/s0016-5107(02)70034-5. [DOI] [PubMed] [Google Scholar]
- 13.Soetikno RM, Kaltenbach T, Rouse RV, Park W, Maheshwari A, Sato T, et al. Prevalence of nonpolypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults. JAMA. 2008;299:1027–1035. doi: 10.1001/jama.299.9.1027. [DOI] [PubMed] [Google Scholar]
- 14.ASGE Technology Committee, author. Wong Kee Song LM, Adler DG, Chand B, Conway JD, Croffie JM, et al. Chromoendoscopy. Gastrointest Endosc. 2007;66:639–649. doi: 10.1016/j.gie.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 15.Kahi CJ, Anderson JC, Waxman I, Kessler WR, Imperiale TF, Li X, et al. High-definition chromocolonoscopy vs. high-definition white light colonoscopy for average-risk colorectal cancer screening. Am J Gastroenterol. 2010;105:1301–1307. doi: 10.1038/ajg.2010.51. [DOI] [PubMed] [Google Scholar]
- 16.Rex DK. Maximizing detection of adenomas and cancers during colonoscopy. Am J Gastroenterol. 2006;101:2866–2877. doi: 10.1111/j.1572-0241.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- 17.Bressler B, Paszat LF, Vinden C, Li C, He J, Rabeneck L. Colonoscopic miss rates for right-sided colon cancer: a population-based analysis. Gastroenterology. 2004;127:452–456. doi: 10.1053/j.gastro.2004.05.032. [DOI] [PubMed] [Google Scholar]
- 18.Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1–8. doi: 10.7326/0003-4819-150-1-200901060-00306. [DOI] [PubMed] [Google Scholar]
- 19.Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Altenhofen L, Haug U. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010;102:89–95. doi: 10.1093/jnci/djp436. [DOI] [PubMed] [Google Scholar]
- 20.Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010;362:1795–1803. doi: 10.1056/NEJMoa0907667. [DOI] [PubMed] [Google Scholar]
- 21.Beduya D, Oliner C, Lee Y. Adenoma detection rate using high-definition white-light colonoscopy versus standard colonoscopy; Gastrointestinal Cancers Symposium; 2010. Abstract No:318. [Google Scholar]
- 22.Buchner AM, Shahid MW, Heckman MG, McNeil RB, Cleveland P, Gill KR, et al. High-definition colonoscopy detects colorectal polyps at a higher rate than standard white-light colonoscopy. Clin Gastroenterol Hepatol. 2010;8:364–370. doi: 10.1016/j.cgh.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 23.Burke CA, Choure AG, Sanaka MR, Lopez R. A comparison of high-definition versus conventional colonoscopes for polyp detection. Dig Dis Sci. 2010;55:1716–1720. doi: 10.1007/s10620-009-0941-y. [DOI] [PubMed] [Google Scholar]
- 24.Inoue T, Murano M, Murano N, Kuramoto T, Kawakami K, Abe Y, et al. Comparative study of conventional colonoscopy and pan-colonic narrow-band imaging system in the detection of neoplastic colonic polyps: a randomized, controlled trial. J Gastroenterol. 2008;43:45–50. doi: 10.1007/s00535-007-2125-x. [DOI] [PubMed] [Google Scholar]
- 25.Pellisé M, Fernández-Esparrach G, Cárdenas A, Sendino O, Ricart E, Vaquero E, et al. Impact of wide-angle, high-definition endoscopy in the diagnosis of colorectal neoplasia: a randomized controlled trial. Gastroenterology. 2008;135:1062–1068. doi: 10.1053/j.gastro.2008.06.090. [DOI] [PubMed] [Google Scholar]
- 26.Horiuchi A, Nakayama Y, Kato N, Ichise Y, Kajiyama M, Tanaka N. Hood-assisted colonoscopy is more effective in detection of colorectal adenomas than narrow-band imaging. Clin Gastroenterol Hepatol. 2010;8:379–383. doi: 10.1016/j.cgh.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 27.Adler A, Aschenbeck J, Yenerim T, Mayr M, Aminalai A, Drossel R, et al. Narrow-band versus white-light high definition television endoscopic imaging for screening colonoscopy: a prospective randomized trial. Gastroenterology. 2009;136:410–416. doi: 10.1053/j.gastro.2008.10.022. e1 quiz 715. [DOI] [PubMed] [Google Scholar]
- 28.Paggi S, Radaelli F, Amato A, Meucci G, Mandelli G, Imperiali G, et al. The impact of narrow band imaging in screening colonoscopy: a randomized controlled trial. Clin Gastroenterol Hepatol. 2009;7:1049–1054. doi: 10.1016/j.cgh.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 29.Harada Y, Hirasawa D, Fujita N, Noda Y, Kobayashi G, Ishida K, et al. Impact of a transparent hood on the performance of total colonoscopy: a randomized controlled trial. Gastrointest Endosc. 2009;69:637–644. doi: 10.1016/j.gie.2008.08.029. [DOI] [PubMed] [Google Scholar]
- 30.Lee YT, Lai LH, Hui AJ, Wong VW, Ching JY, Wong GL, et al. Efficacy of cap-assisted colonoscopy in comparison with regular colonoscopy: a randomized controlled trial. Am J Gastroenterol. 2009;104:41–46. doi: 10.1038/ajg.2008.56. [DOI] [PubMed] [Google Scholar]
- 31.Sawhney MS, Cury MS, Neeman N, Ngo LH, Lewis JM, Chuttani R, et al. Effect of institution-wide policy of colonoscopy withdrawal time > or = 7 minutes on polyp detection. Gastroenterology. 2008;135:1892–1898. doi: 10.1053/j.gastro.2008.08.024. [DOI] [PubMed] [Google Scholar]
- 32.Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006;355:2533–2541. doi: 10.1056/NEJMoa055498. [DOI] [PubMed] [Google Scholar]
- 33.Matro R, Shnitser A, Spodik M, Daskalakis C, Katz L, Murtha A, et al. Efficacy of morning-only compared with split-dose polyethylene glycol electrolyte solution for afternoon colonoscopy: a randomized controlled single-blind study. Am J Gastroenterol. 2010;105:1954–1961. doi: 10.1038/ajg.2010.160. [DOI] [PubMed] [Google Scholar]
- 34.Parra-Blanco A, Nicolas-Perez D, Gimeno-Garcia A, Grosso B, Jimenez A, Ortega J, et al. The timing of bowel preparation before colonoscopy determines the quality of cleansing, and is a significant factor contributing to the detection of flat lesions: a randomized study. World J Gastroenterol. 2006;12:6161–6166. doi: 10.3748/wjg.v12.i38.6161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park SY, Lee SK, Kim BC, Han J, Kim JH, Cheon JH, et al. Efficacy of chromoendoscopy with indigocarmine for the detection of ascending colon and cecum lesions. Scand J Gastroenterol. 2008;43:878–885. doi: 10.1080/00365520801935442. [DOI] [PubMed] [Google Scholar]
- 36.Pohl J, Lotterer E, Balzer C, Sackmann M, Schmidt KD, Gossner L, et al. Computed virtual chromoendoscopy versus standard colonoscopy with targeted indigocarmine chromoscopy: a randomised multicentre trial. Gut. 2009;58:73–78. doi: 10.1136/gut.2008.153601. [DOI] [PubMed] [Google Scholar]
- 37.Bustamante-Balén M, Bernet L, Cano R, Pertejo V, Ponce J. Prevalence of nonpolypoid colorectal neoplasms in symptomatic patients scheduled for colonoscopy: a study with total colonic chromoscopy. J Clin Gastroenterol. 2010;44:280–285. doi: 10.1097/MCG.0b013e3181aed327. [DOI] [PubMed] [Google Scholar]
- 38.Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, Sternberg SS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 39.Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002;97:1296–1308. doi: 10.1111/j.1572-0241.2002.05812.x. [DOI] [PubMed] [Google Scholar]
- 40.Mitooka H, Fujimori T, Maeda S, Nagasako K. Minute flat depressed neoplastic lesions of the colon detected by contrast chromoscopy using an indigo carmine capsule. Gastrointest Endosc. 1995;41:453–459. doi: 10.1016/s0016-5107(05)80003-3. [DOI] [PubMed] [Google Scholar]
- 41.Carroll RE. Colon preparation for magnification endoscopy: a rapid novel approach. Endoscopy. 2004;36:609–611. doi: 10.1055/s-2004-814516. [DOI] [PubMed] [Google Scholar]


