Abstract
Pain limits the success of cecal intubation in unsedated patient. Carbon dioxide infusion instead of air insufflation and water infusion as an adjunction to air insufflation have both been investigated as modalities to minimize pain associated with colonoscopy. Multiple RCT support an effect of carbon dioxide in reducing pain after colonoscopy. A modern method of water infusion as the sole modality for aiding colonoscope insertion has been shown to reduce pain during and after colonoscopy. Favorable effects in reducing discomfort have been documented in both sedated and unsedated patients. Because of the need to perform water exchange in the patients with suboptimal bowel perparation, a serendipitous consequence of salvage cleansing is evident with application of the water method. The associated increase in adenoma detection especially in the proximal colon is most intriguing. The hypothesis that the water method during insertion combined with carbon dioxide insufflation during withdrawal will optimally decrease colonoscopy pain should be evaluated. The implications of increased adenoma detection by the water method also deserve to be studied.
Key words: adenoma detection, colonoscopy, colonoscopy discomfort, on demand sedation, screening, unsedated, water method
I want to thank the DDW organizing committee for the invitation. I plan to focus on colonoscopy pain and detection of lesions. Four decades ago diagnostic colonoscopy was developed as an unsedated procedure. Air insufflation, a convenient modality to distend the lumen for viewing, lengthens the colon and accentuates angulations at flexures. The need to push through angulated loops during insertion results in pain. Over distension or the spasms precipitated by the distention are also painful.1 When sedation is unavailable, pain limits cecal intubation; or patients may be coerced into putting up with “excessive discomfort”.2,3 Where it is available, conscious sedation has become standard, and even adopted for screening cases. Deep sedation enhances efficiency, but also markedly increases cost.4 Not surprisingly, sedation with its inherent escort and time off requirement has been recognized as a significant barrier to screening.5 New challenges have also emerged and reviewed in recent reports of impact of the water method on adenoma detection.6,7 Post screening colonoscopy interval cancers are likely due to missed lesions. Proximal colon cancer mortality is not reduced by screening colonoscopy or is reduced at best by only ∼50% (in contrast to 80% to 90% in the distal colon). The suspicion is strong that missed lesions during screening colonoscopy may be playing a role.
A considerable number of RCT in unsedated or sedated patients summarized in a review of methods of reducing discomfort during colonoscopy1 and in more recent reports8–10 showed that CO2 instead of air insufflations decreases pain scores and increases the proportion of patients with no pain after colonoscopy. The mechanism is based on ‘rapid’ absorption of CO2 from the lumen, decreasing distention and associated pain. The presentation by Amato et al.11 this afternoon is the most current confirmation of the efficacy of CO2 insufflation. The investigators show that CO2 insufflation is associated with a decrease in the proportion of patients requesting on-demand sedation as compared to air insufflation and improves patient tolerance and decreases colonoscopy related pain.11
In a review of water infusion as an adjunct to air insufflation water infusion has been well-documented to facilitate insertion through difficult segments affected by diverticulosis, speed insertion to the cecum and decrease pain.12 The need to complete examination to the cecum using the unconventional option of unsedated colonoscopy in the US led to the recognition that air insufflation, which lengthens the colon, is the major contributor limiting success13–15, an experience probably very similar to those of the early colonoscopists who resorted to sedation. Incremental steps were taken to confirm that cecal intubation could be accomplished using water in lieu of air during insertion in the fully sedated patients16, in patients given half the usual doses of sedation medications16, in patients given minimal sedation17,18, in patient offered the option of sedation on-demand19,20, in sedated patients examined by supervised trainees18,21,22, in patients who underwent scheduled unsedated colonoscopy23,24, and in patients examined by an experienced colonoscopist who chose self-education and documented the learning curve of the water method25,26.
I shall describe the most up-to-date version of the water method as the sole modality for facilitating insertion.27 Air is used only during withdrawal. To avoid elongation of the colon by insufflated air, the air pump is turned off. To minimize angulations of the flexures, all residual air in the colon is removed by suction. Water is infused to identify the lumen. To clear the view, water exchange is used. Unlimited water is supplied by the water pump. The residual feces are removed simultaneously by suction to keep the lumen from being excessively distended. The still images in Figure 1 illustrate the technical details.28 Upon entering an air filled rectum all the residual air is removed by suction. The tip of the endoscope is pushed against the point where the folds converge. Water is infused to confirm that the lumen lies ahead. Water exchange is used to remove residual feces. With simultaneous infusion of water and suction of residual feces, the turbulence in the vicinity of the tip of the colonoscope dislodges feces from the adjacent mucosa. Eventually, the lumen clears. Most of the infused water is suctioned out during insertion to obviate excessive distention of the lumen. Examples of the appendix opening under water are shown here. Sometimes, red suction marks indicate arrival in the cecum. The middle panels reveal one caveat. If air insufflation instead of water exchange is used when difficulty (poor view) is encountered, identification of the lumen can be made easier. However, the potential drawback is the leaving behind of the ”dirty fecal water” which may continue to impair the view, during withdrawal. Water exchange is the preferred approach to deal with a suboptimal bowel preparation in the water method. A suboptimal bowel preparation can be salvaged by the water exchange (Fig. 2). The withdrawal phase is done with air insufflation similar to the traditional air method.
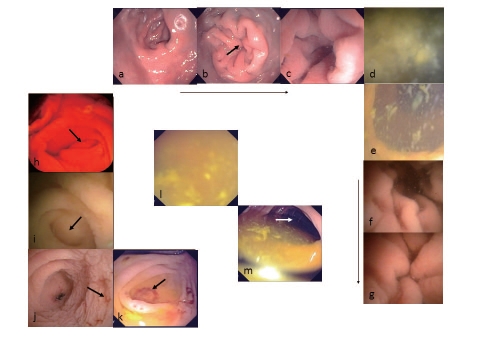
Figure 1.
Still images illustrating the technical details of the water method: a. air filled rectum; b. air removal collapses rectal lumen; c. infused water opens lumen; d. residual feces removed by suction; e. simultaneous water infusion and suction produce turbulence at the tip of the colonoscope to dislodge adherent feces from nearby mucosa; f & g. suction of luminal water minimizes distention; h & i. appendix opening; j & k. suction marks near appendix opening; l. difficult view due to excessive residual feces; m. insufflated air in the presence of excessive residual feces can produce air/fluid compartments to facilitate viewing of the lumen, but the preferred maneuver with the water method is water exchange to clear the view.
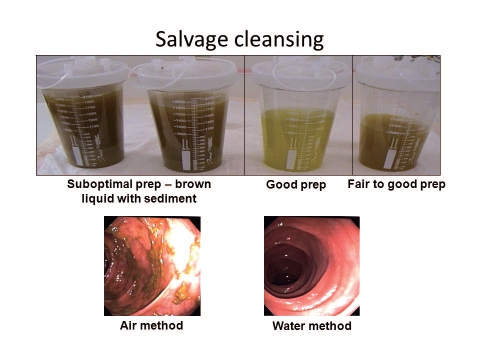
Figure 2.
Most of the dirty water is in the suction bottle during insertion. Water exchange provides salvage cleansing of the colon.
In a RCT comparing air vs. water in unsedated patients24, the median maximum pain score (0 = none; 10 = most severe) during colonoscopy was significantly lower in the water group (3 vs. 6). The median overall pain score (0 = none; 10 = most severe) after colonoscopy (2 vs. 3) was lower in the water group and the difference approached significance. The proportion with severe overall pain score of ≥5 after colonoscopy was significantly lower in the water group (12% vs. 33%). The cecal intubation rate (98% vs. 78%) and willingness to repeat unsedated colonoscopy (93% vs. 78%) were both significantly higher in the water group (Fig. 3). In another RCT, combined with the option of sedation on-demand (Fig. 4), the water method permitted a significantly higher proportion of patients to complete unsedated colonoscopy (78% vs. 54%). The median maximum pain score during colonoscopy was significantly lower in the water group. The water group spent significantly less time in recovery on site and at home. In the water group, the dose of fentanyl was significantly lower and the lower dose of midazolam approached significance.20
Figure 3.
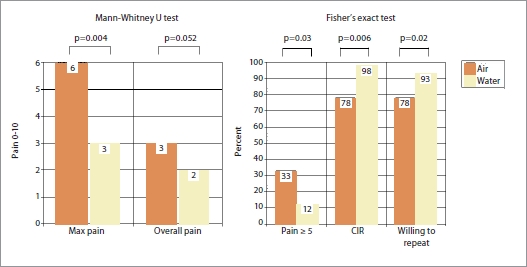
Outcome of randomized controlled trial in scheduled unsedated patients. N, Air = 40; water = 42. Pain (0 = none, 10 = most severe); median scores. CIR, cecal intubation rate.
Figure 4.
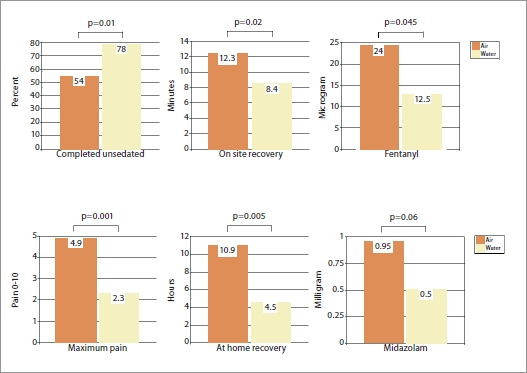
Outcome of randomized controlled trial in patients examined with the option of on-demand sedation. N, air = 50; water = 50. Pain (0 = none, 10 = most severe) and recovery times are median scores. Sedation medications are means. Significant difference based on Fisher's exact test, Mann-Whitney U test and unpaired t test.
The findings in the above two RCT are being confirmed by several presentations at this meeting. One RCT from India29 shows that water infusion significantly reduced the proportion of unsedated patients with pain score ≥2 (5 was most severe) compared with the air method (p<0.05). Another RCT from Italy11 shows that warm water infusion is associated with a decrease in the proportion of patients requesting on-demand sedation as compared to air insufflation and improves patient tolerance and decreases colonoscopy related pain. Another RCT from Germany30 comparing water infusion vs. air insufflation for aiding colonoscopy insertion in unsedated patients at screening colonoscopy shows that water infusion permits cecal intubation in 78% and 60% with the water and air method, respectively (p<0.05).
When the databases of the two US RCT described above were combined31, the <10 mm adenoma detection rate (ADR) in the proximal colon in the screening cases were 6% and 20%. The <10 mm hyperplastic polyps in the proximal colon in the screening cases were 0% and 6%. The combined <10 mm lesions in the proximal colon in the screening cases were 6% and 31%, a significant difference in favor of the water method (Fig. 5). The performance improvement study32 reported earlier this afternoon, and again next Tuesday during the session of the Best of Digestive Disease Week 2011, shows that with a larger sample size, the overall ADR for the entire colon, the proximal colon ADR and proximal colon <10 mm ADR were all significantly higher in the water group (Fig. 6). A third observational study during this meeting33 suggests that application of the water method in community settings in the US is feasible with significantly lower sedation requirement and higher ADR.
Figure 5.
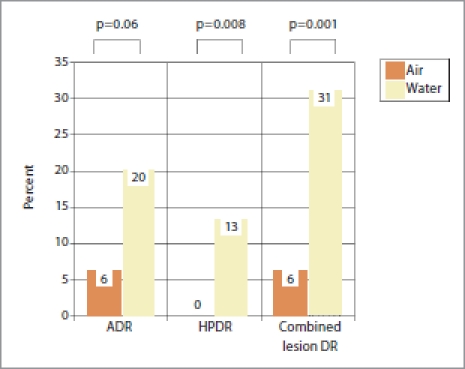
Detection rate of <10 mm lesions in the proximal colon in screening cases. N, air = 52; water = 45. HP = hyperplastic polyp. DR, detection rate. Significant difference based on Fisher's exact test.
Figure 6.
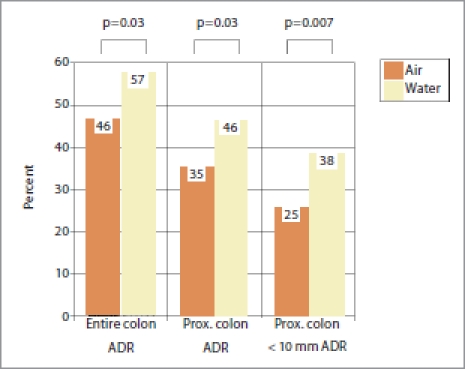
Head-to-head comparison of adenoma detection rate between water and air methods. N, air = 191; water = 177. Significant difference based on Fisher's exact test.
The take home messages are quite clear. Carbon dioxide insufflation decreases pain after colonoscopy. The water method as the sole modality to aid insertion decreases pain during and after colonoscopy; increases overall ADR; and increases proximal <10 mm lesion detection rate. To put the new knowledge presented this afternoon into planning the next study, I propose the following. The study method is a combination of the water method (without air or CO2 insufflation) for insertion and CO2 insufflation for withdrawal. Polypectomy can be performed during insertion and/or withdrawal at the discretion of the colonoscopist, and recorded. The study method will be compared with any traditional techniques or new methods. Data will include pain during and after colonoscopy; and lesion yield (both adenomas and sessile serrated polyps).
If the data discussed this afternoon can be reproduced, the combination will decrease pain, provide salvage cleansing and increase proximal lesion yield. My speculations are as follows (Fig. 7). This combination may lead to the possibility of decreased sedation, less assistant help, improved bowel preparation and decreased missed lesions. Decreased sedation may result in less time spent in recovery, less need for escort if scheduled unsedated colonoscopy is progressively more successful. Overall patient burden (escort requirement and recovery time spent on site and for home recovery) can be minimized. Decreased colonoscopy pain may reduce post colonoscopy pain-related emergency department visits and hospitalizations. Salvage cleansing may permit a bowel preparation schedule less burdensome to the patients. Reduced sedation and reduced abdominal pressure may result in decreased need for assistant and nursing support, decreased cost of screening, and perhaps increased screening with fixed resources. Increased lesion yield (especially in the proximal colon) may lead to decrease in interval cancers and decrease in mortality of proximal colon cancers, and eventually reduction in cancer care costs. These hypotheses deserve to be evaluated in future screening colonoscopy studies.
Figure 7.
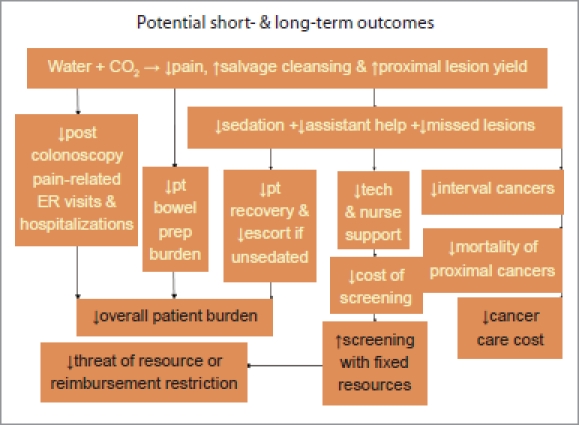
Potential short- and long-term outcomes (abbreviations: ER, emergency room; prep, preparation; pt, patient; tech, technician)
Acknowledgement
The review is support in part by VA Medical Research Funds (FWL) and in part by ASGE Career Development Award (FWL 1985), ASGE and ACG Clinical Research Funds (JWL & FWL) .
Abbreviations
- ACC
Ambulatory Care Center
- ACG
American College of Gastroenterology
- ASGE
American Society for Gastrointestinal Endoscopy
- OS
observational study
- RCT
randomized controlled trial
- SD
standard deviation
- US
United States
- VA
Veterans Affairs, VAMC, Veterans Affairs Medical Center
Biography
Felix W. Leung, MD, FACG
Felix W. Leung, MD was a native of Hong Kong. He began his post high school education in the United States in 1970. He received his Doctor of Medicine degree in 1978 from Yale Medical School, New Haven, Connecticut. He did his medicine training at the UCLA-Wadsworth VAMC, and continued with the UCLA-Wadsworth GI Fellowship and post-doctoral research programs. He is currently affiliated with the Section of Gastroenterology, Sepulveda Ambulatory Care Center and Nursing Home and the West Los Angeles VAMC, VA Greater Los Angeles Healthcare System and is Professor of Medicine at the David Geffen School of Medicine at UCLA.
Dr. Leung has a broad range of interests - experimental and endoscopic assessment of GI blood flow, management of fecal incontinence and most recently methods to minimize discomfort during unsedated colonoscopy. Over the years, he has received research support from Department of Veterans Affairs, California Tobacco-Related Diseases Research Program, Smokeless Tobacco Research Council, Inc., American Society for Gastrointestinal Endoscopy, American Gastroenterological Association, American Digestive Health Foundation, American College of Gastroenterology, National Institute of Health and several pharmaceutical companies and industry sources. At times, his insistence on focusing attention on the patients' needs - his late entry into the unsedated colonoscopy research arena - is at odds with mainstream physician-centered practice. Nevertheless, he constantly reminds his audience that none who considers helping him seriously in this venture has regretted participation. Serendipity smiles on his research team with the discovery that the water method not only significantly diminishes colonoscopy discomfort, also appears to improve adenoma detection, particularly in the proximal colon. Colleagues have begun to recognize his contributions by inviting him to give the State-of-the-Art Lecture on Unsedated Colonoscopy at the 8th Pan Arab Gastroenterology Meeting in Riyadh, Saudi Arabia in Feb 2011, and the State-of-the-Art Lecture at the Cutting Edge Colonoscopy Technique session at the 2011 Digestive Disease Week Meeting in Chicago, United States. Since his appointment as Associate Editor of the Journal of Interventional Gastroenterology last year, he has made unprecedented contributions to shape the image and content of the inaugural issue, resulting in his rapid promotion to Senior Associate Editor in a short span of 6 months. “This has been my best year” he reminisces as he volunteers to publish the 2011 DDW State-of-the-Art Lecture in the Journal, “and the halo effect will nurture the continued growth and development of the Journal at its infant stage.” And more recently, he added “The excitement over the new developments are definitely warranted because even GI & Hepatology News (the official newspaper of the American Gastroenterological Association Institute) plans to feature a front page article about the water method, carbon dioxide, patient comfort and adenoma detection rate in an upcoming issue in 2011.”
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
References
- 1.Leung FW. Methods of reducing discomfort during colonoscopy. Dig Dis Sci. 2008;53:1462–1467. doi: 10.1007/s10620-007-0025-9. [DOI] [PubMed] [Google Scholar]
- 2.Leung FW, Aljebreen AM, Brocchi E, Chang EB, Liao WC, Mizukami T, et al. Sedation risk-free colonoscopy for minimizing the burden of colorectal cancer screening. World J Gastrointest Endosc. 2010;2:81–89. doi: 10.4253/wjge.v2.i3.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leung FW. Is there a place for sedationless colonoscopy? J Interv Gastroenterol. 2011;1:19–22. doi: 10.4161/jig.1.1.14592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leung FW. The case of unsedated screening colonoscopy in the United States. Gastrointest Endosc. 2009;69:1354–1356. doi: 10.1016/j.gie.2008.12.234. [DOI] [PubMed] [Google Scholar]
- 5.Denberg TD, Melhado TV, Coombes JM, Beaty BL, Berman K, Byers TE, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med. 2005;20:989–995. doi: 10.1111/j.1525-1497.2005.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leung JW, Do L, Siao-Salera RM, Parikh DA, Mann SK, Leung FW. Retrospective data showing the water method increased adenoma detection rate - a hypothesis generating observation. J Interv Gastroenterol. 2011;1:3–7. doi: 10.4161/jig.1.1.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung FW, Leung JW, Siao-Salera RM, Mann SK. The water method significantly enhances proximal diminutive adenoma detection rate in unsedated patients. J Interv Gastroenterol. 2011;1:8–13. doi: 10.4161/jig.1.1.14587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uraoka T, Kato J, Kuriyama M, Hori K, Ishikawa S, Harada K, et al. CO2 insufflation for potentially difficult colonoscopies: efficacy when used by less experienced colonoscopists. World J Gastroenterol. 2009;15:5186–5192. doi: 10.3748/wjg.15.5186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riss S, Akan B, Mikola B, Rieder E, Karner-Hanusch J, Dirlea D, et al. CO2 insufflation during colonoscopy decreases post-interventional pain in deeply sedated patients: a randomized controlled trial. Wien Klin Wochenschr. 2009;121:464–468. doi: 10.1007/s00508-009-1202-y. [DOI] [PubMed] [Google Scholar]
- 10.Wong JC, Yau KK, Cheung HY, Wong DC, Chung CC, Li MK. Towards painless colonoscopy: a randomized controlled trial on carbon dioxide-insufflating colonoscopy. ANZ J Surg. 2008;78:871–874. doi: 10.1111/j.1445-2197.2008.04683.x. [DOI] [PubMed] [Google Scholar]
- 11.Amato A, Radaelli F, Paggi S, Spinzi G, Terruzzi V. Carbon dioxide insufflation (CO2) and warm water infusion (WWI) versus standard air insufflation (AI): preliminary results of a randomized controlled trial in unsedated colonoscopy. DDW 2011 abstract 602, program p. 301.
- 12.Leung FW. Water-related method for performance of colonoscopy. Dig Dis Sci. 2008;53:2847–2850. doi: 10.1007/s10620-008-0259-1. [DOI] [PubMed] [Google Scholar]
- 13.Leung FW, Aharonian HS, Guth PH, Chu SK, Nguyen BD, Simpson P. Involvement of trainees in routine unsedated colonoscopy: review of a pilot experience. Gastrointest Endosc. 2008;67:718–722. doi: 10.1016/j.gie.2007.11.040. [DOI] [PubMed] [Google Scholar]
- 14.Leung FW. Unsedated colonoscopy introduced to ensure access is acceptable to a subgroup of veterans. Dig Dis Sci. 2008;53:2719–2722. doi: 10.1007/s10620-007-0192-8. [DOI] [PubMed] [Google Scholar]
- 15.Leung FW. Promoting informed choice of unsedated colonoscopy: patient-centered care for a subgroup of US Veterans. Dig Dis Sci. 2008;53:2955–2959. doi: 10.1007/s10620-008-0253-7. [DOI] [PubMed] [Google Scholar]
- 16.Leung JW, Salera R, Toomsen L, Mann S, Leung FW. Pilot feasibility study of the method of water infusion without air insufflation in sedated colonoscopy. Dig Dis Sci. 2009;54:1997–2001. doi: 10.1007/s10620-008-0576-4. [DOI] [PubMed] [Google Scholar]
- 17.Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim B, Cabrera H, et al. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009;70:505–510. doi: 10.1016/j.gie.2008.12.253. [DOI] [PubMed] [Google Scholar]
- 18.Leung CW, Kaltenbach T, Soetikno R, Wu KK, Leung FW, Friedland S. Water immersion versus standard colonoscopy insertion technique: randomized trial shows promise for minimal sedation. Endoscopy. 2010;42:557–563. doi: 10.1055/s-0029-1244231. [DOI] [PubMed] [Google Scholar]
- 19.Leung JW, Mann S, Leung FW. Options for screening colonoscopy without sedation: a pilot study in United States veterans. Aliment Pharmacol Ther. 2007;26:627–631. doi: 10.1111/j.1365-2036.2007.03404.x. [DOI] [PubMed] [Google Scholar]
- 20.Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim BS, Canete W, et al. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103–110. doi: 10.1016/j.gie.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 21.Ransibrahmanakul K, Leung JW, Mann SK, Siao-Salera R, Lim BS, Hasyagar C, et al. Comparative effectiveness of water vs. air methods in minimal sedation colonoscopy performed by supervised trainees in the US - randomized controlled trial. Am J Clin Med. 2010;7:113–118. [Google Scholar]
- 22.Friedland S, Leung FW. Learning and teaching the water method. J Interv Gastroenterol. 2011 doi: 10.4161/jig.1.3.18511. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leung FW, Aharonian HS, Leung JW, Guth PH, Jackson G. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. 2009;69:546–550. doi: 10.1016/j.gie.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 24.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, et al. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 25.Ramirez FC, Leung FW. Adopting the water method: lessons, tips and pitfalls learned. Am J Clin Med. 2010;7:121–123. [Google Scholar]
- 26.Ramirez FC, Leung FW. J Interv Gastroenterol. 2011. The water method for aiding colonoscope insertion: the learning curve of an experienced colonoscopist. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leung FW, Leung JW, Mann SK, Friedland S, Ramirez FC. Endoscopy. 2011. Innovation Forum - The water method significantly enhances the outcome of colonoscopy in sedated and unsedated patient. in press. [DOI] [PubMed] [Google Scholar]
- 28.Leung FW. Inaugural issue cover page illustrations. J Interv Gastroenterol. 2011;1(1) cover. [Google Scholar]
- 29.Sawant PD, Samarth A, Vashishtha C, Patel J, Agasti A. Water infusion vs. air insufflation colonoscopy in unsedated patients - impact on patient discomfort. DDW 2011 Poster Tu1434, program p. 873.
- 30.Pohl JP, Pech O, Manner H, May A, Ell C. A RCT comparing water infusion vs. air insufflation for aiding colonoscopy insertion in unsedated patients at screening colonoscopy. DDW 2011 Colon Potpourri session: Monday presentation 673, program p. 321.
- 31.Leung FW, Leung JW, Siao-Salera RM, Mann SK, Guy Jackson G. The water method significantly enhances detection of diminutive lesions (adenoma and hyperplastic polyp combined) in the proximal colon in screening colonoscopy - data derived from two RCT in US veterans. J Interv Gastroenterol. 2011;1:48–52. doi: 10.4161/jig.1.2.16826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramirez FC, Leung FW. The water method is associated with higher adenoma detection rate (ADR) - a head-to-head comparative study. DDW 2011 abstract 601 and 601r, program p. 301 and p. 435.
- 33.Portocarrero DJ, Che K, Olafsson S, Walter MH, Sahba B, Jackson CS, et al. Application of the water method to aid colonoscope insertion in community settings in the United States is feasible: sedation requirement can be minimized without compromising patientcentered and procedure-related outcomes. DDW 2011 Poster Tu1430, program p. 873.