Abstract
Endoscopy plays an important role in the diagnosis and treatment of digestive diseases. The benefits are maximized when procedures are performed at an optimal level of quality. Technical failures and adverse events are more likely to occur when procedures are performed by inexperienced endoscopists. Professional organizations and manufacturing industry which support and represent endoscopy, and their leaders, have increasingly embraced the quality improvement paradigm that is advancing through medicine. We all need to agree on the metrics of endoscopic performance, to develop the infrastructure to collect and analyze the data, and to use the resulting knowledge to stimulate improvements in practice and benefit the patients.
Key words: quality performance, endoscopy, endoscopists, endoscopy unit
Introduction
Endoscopy has become enormously popular throughout the world because of its proven value in the diagnosis and treatment of digestive diseases. One problem is that the benefits are maximized only when procedures are performed at an optimal level of quality, which is not always the case. Technical failures and adverse events can occur even in the best of hands, but are more likely when procedures are performed by endoscopists with inadequate training and experience. Practitioners, patients and payers should all be interested in enhancing the quality of endoscopy, and documenting it.
The professional organizations which support and represent endoscopy, and their leaders, have increasingly embraced the quality improvement paradigm that is advancing through medicine, as it has through manufacturing industry. Amongst others, the American Society for Gastrointestinal Endoscopy (ASGE), the American College of Gastroenterology (ACG) and the World organization (OMED) have produced helpful reports and guidelines (1–6). Britain and Australia have taken a step further in setting up authorities which represent all of the stakeholders, i.e. the Joint Advisory Group (JAG) (7) in Britain, and the Conjoint Committee in Australia (8). Unfortunately, most of the thoughtful conclusions and well meaning documents from these and other authorities have had little impact so far in the real world. Quality is discussed, but not measured to any extent, and certainly not mandated. Hospital privileging bodies seldom follow published guidelines for credentialing.
We all need to agree on the metrics of endoscopic performance, to develop the infrastructure to collect and analyze the data, and to use the resulting knowledge to stimulate improvements in practice. Patients will benefit.
What is quality endoscopy?
Society (ie the informed patient) expects that diagnostic and therapeutic procedures will be appropriate (ie indicated), and that they will be performed expeditiously, skillfully, successfully, safely and comfortably. These expectations can be expanded to make a list of desirable characteristics for all types of endoscopic procedures.
Correct indications - adherence to published guidelines
Appropriate environment, support team and behavior
Well prepared and informed patients
Strategies to minimize risk, including patient preparation and monitoring.
Appropriate use of medications, including sedation/analgesia when used.
Correct selection of equipment
Comfortable intubation
Complete survey of the target organ(s)
Recognition of all abnormalities (and photo documentation)
Appropriate tissue sampling (adherence to published guidelines)
Application of indicated therapy
Avoiding, recognizing, and managing, adverse events
Reasonable duration
Smooth recovery, explanation and discharge
Detailed and clear recommendations and follow-up plans
Integrated pathology results and communications
Complete documentation (and billing)
Positive feedback from patients
Many organizations and groups have explored these quality issues and their metrics and guidelines for credentialing physicians and granting privileges to perform endoscopy. These proposals have mainly focused on the activities of the endoscopist, and focusing mainly on colonoscopy (9), but all of the elements of the process are important. We will discuss quality issues for endoscopy units after those pertaining to individual endoscopists.
How to recognize, predict and measure excellence of endoscopists?
There are some features of an endoscopist that make a good experience more likely. Formal endoscopic training and extensive experience do not guarantee quality practice, but they certainly make it more likely. Thus, documentation of these and related elements should be a part of any assessment of endoscopic performance. Appropriate metrics could include
Specialty training and certification (place and dates)
Training and maintenance of competence in life support and sedation
Evidence for continuing education in endoscopy
For each procedure (eg ERCP) - lifetime numbers, total last year, and spectrum of practice
The proof of quality comes from documentation of performance. There is no substitute for collecting relevant data (10). Trainees in most countries are now expected to maintain logbooks of their procedural activity during training, and many authorities have recommended that endoscopists should continue to collect data prospectively on their endoscopic practice and performance. This translates into “endoscopy report cards” (11).
New complexity scales for endoscopic procedures
When trying to determine and document quality in endoscopy, it is important to recognize that some procedures are more difficult than others. Any case may prove to be technically challenging (colonoscopy with multiple loops, or ERCP with the papilla inside a diverticulum), but some situations are predictably challenging (e.g. ERCP after surgical biliary diversion, or treating a patient with active hematemesis). Schutz and Abbot addressed this issue many years ago by proposing a scale for “degree of difficulty” for ERCP. Their initial 5 level scale was reduced to 3, and has been widely used (5). Grade 1 procedures are the common biliary interventions that anyone offering ERCP services should be able to achieve to a reasonable level of competence, whereas grade 3 cases are those usually referred to tertiary centers. This allows endoscopists to understand their comfort level for cases, and could be used also to help patients and payers to make good choices. The “Schutz scale” for ERCP is now outdated by subsequent developments, and an ASGE working group recently proposed complexity scales for all of the common procedures (12). All now have 4 levels, and those proposed for colonoscopy are shown in Figure 1.
Figure 1.
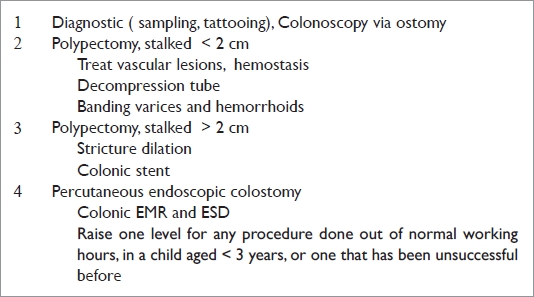
Proposed complexity levels for colonoscopy
Endoscopists report cards and benchmarking performance
Endoscopists cannot be expected to report on all of the data elements that have been listed in various well-meaning publications (and listed above). Items should be selected based on ease of data collection, and by assumed relative importance (5,13). Some items are easily recorded, and already appear in most procedure reports (e.g. indication, anatomical extent, duration, diagnosis, and any immediate adverse events). Other items are more subjective (e.g. lesion interpretation), or more difficult to record (e.g. delayed adverse events, endoscopist-specific patient satisfaction). Some items would appear to be more important markers of quality than others. For colonoscopy, cecal intubation rates, withdrawal times, and adenoma detection rates appear to be particularly relevant (9). For ERCP, success rates for selective cannulation and for removal of bile duct stones, are obvious key parameters (14).
Keeping track of one's own performance data is important, but more meaningful when it can be compared with others, i.e. benchmarking. This requires an organization as well as motivation.
Further details are discussed in the context of ERCP, which is the most challenging (and risky) of the commonly performed procedures.
The ERCP quality network
With the support of Olympus America, we set up a pilot project to test the practicality and acceptability of collecting and comparing data on the practice and quality of ERCP procedures by individual endoscopists (15). Baseline information included the experience and practice environment of the endoscopists. Data on each procedure are loaded onto a secure website, prospectively, either directly or via a single paper data sheet. The data points include the indications, complexity grade, ASA grade, sedation/anesthesia, admission policy, scope and fluoroscopy times, and success rates for individual technical procedures such as deep biliary cannulation, sphincterotomy, stenting, etc. Immediate and delayed adverse events are noted. Patients and endoscopists are not individually identified. The data are analysed automatically, and the results are posted immediately on the web site. Contributors can view a summary of their own performance (report card), and compare it with that of all other contributors to the system (benchmarking), none being identified by name. More than 120 endoscopists from several countries have entered data on over 20,000 ERCPs. Figure 2 shows the biliary cannulation rates of doctors who have entered more than 50 cases. More detailed analyses are easily done, such as comparing practice patterns and performance by the level of experience. The project has been criticized for the fact that the data are self-reported, and not validated by independent audit. While the overall reported success rates are high, and adverse event rates are low, some endoscopists have indeed reported poor results. Since the system does not identify the individual endoscopists (except to themselves), there is little incentive to consider selective reporting. This criticism will become moot when the quality data are retrieved automatically from the computer systems generating the clinical reports.
This pilot study has demonstrated that certain physicians are prepared, even enthusiastic, to share their data, and to compare their performance with peers. The plan is to expand the number and variety of participants in the network and to include other quality parameters. This will allow more meaningful comparisons across the spectrum of ERCP practice. Hopefully this project will facilitate the development of a viable national system for quality reporting.
What performance level is good enough? Who decides?
The ERCP quality project has confirmed the obvious fact that endoscopists vary in their levels of performance, even amongst those comfortable enough to share their data. Not all patients can be managed by the super-experts. The issue then is how to determine who decides what constitutes acceptable performance, and what that should be. Professional organizations initially guessed (far too low) at the “numbers” needed to achieve competence, but have recently concentrated on what might be acceptable performance, ie the skill level that would justify independent practice (completion of formal training). The latest ASGE report on ERCP quality (14) paints a broad canvas “Successful cannulation rates at or above 95% are consistently achieved by experienced endoscopists, and rates at or above 80% are a goal of training programs….Thus, although >90% is an overall appropriate target for successful cannulation, rates of >85% should be achievable for most endoscopists”. It goes on to say that “Technical success for common (biliary) procedures should be achievable in >85% of cases”.
Who is going to do YOUR ERCP?
Would you let your recent trainee loose on your family? Would you yourself submit to an 80–85% ERCPist? This level of performance would be acceptable, maybe life-saving, in an urgent and remote situation, but certainly not for an elective procedure when experts are available nearby. I would suggest that 95% is an appropriate target, at least for the basic common biliary procedures. How can patients make an informed judgment since they have no way of telling the difference between an 85% and a 95% performer. Those of us in health care have ways of knowing who is “good” and who is not, but most of our customers do not. They rely on advice from their primary care givers (and friends), and the honesty and communication skills (sometimes inadequate) of their proposed endoscopists. I believe that we need to do better, and there are only 2 ways forward. One is for professional societies (and the payers) to set the bar higher, and to press for a certificate or diploma, to be granted only after a formal examination. This would be resource intensive, and not without controversy, but exams are the recognized method for assuring a reasonable level of knowledge and performance in many other fields. The diploma would be based on data from report cards, an examination of core knowledge, observation of a few cases, and, possibly, some work on simulators. This exercise would require agreement on how to “score” the more subjective elements of a procedure. The second method - and a step towards the first - is to encourage or mandate report cards, and to educate the public to ask for them.
Benchmarking in Colonoscopy
Pike in Virginia, USA, has been running an important voluntary benchmarking project focusing on the quality of colonoscopy procedures (16). This has the same main goal as the ERCP study, to allow individuals to benchmark their performance against colleagues and guidelines, but differs in that there were many more data points, entry was on paper, delayed data were required (pathology reports), and that the analyses were not done on-line, and reported only intermittently.
These projects, and the rising tide of professional opinion, led the ASGE and ACG to initiate a joint national system for benchmarking, called GIQuIC (17). This opened for enrollment in July 2010, and will focus initially on colonoscopy. ERCP will be incorporated along with other procedures eventually, and the ERCP Quality Network will likely cease at that point. In the meantime, it remains available as a viable resource for personal quality assessment and improvement.
Quality of endoscopy units and the endoscopy process
Patients hope and usually assume that their procedures will be “done well”, and are often more concerned about their safety, comfort and dignity, and the efficiency of the process. Indeed, patients are much better able to assess these elements than the technical aspects performed while they are sedated. Whilst endoscopists have responsibility for these elements, and can influence the way the rest of the team functions, there are important quality elements of the endoscopy unit and staff that can be considered separately. Endoscopists (however talented) cannot work without good facilities, equipment, and a team of well-trained and motivated staff. Whilst most healthcare facilities pay some attention to “quality improvement”, the extent to which this percolates down to the endoscopy unit is variable. There has been no national quality improvement program specific for endoscopy units in the United States, and the agencies which accredit them do not have comprehensive guidelines.
Metrics of quality in endoscopy units
It is not difficult to list features of endoscopy units which may affect the quality of the procedures being performed in them.
Years unit existed
Nature; hospital, freestanding endoscopy clinic, or office
Accreditation agency (and most recent rating)
Name of medical director
Name of nurse manager
Volumes last calendar year (uppers, colons, ERCP, EUS)
Number of procedure rooms and patient bays.
Total number of nursing staff (and training levels)
-
Written policies and systems for
sedation and monitoring
cleaning and disinfection
risk reduction
patient recall for surveillance
tracking pathology results
quality improvement
-
Safety data
Infection rates
Unplanned intubations
Unplanned admissions
-
Communications and feed-back
No-show rates
Patient satisfaction data
Staff satisfaction data
An “Endoscopy Unit Report Card” could be developed by picking a selection of these criteria (1).
Projects to assess and promote the quality of endoscopy units
As part of the Endoscopy Modernization process in Britain, a “Global Rating Scale” for endoscopy units was developed by Dr Roland Valori (18). The system is supported by a comprehensive knowledge base, and useful improvement tools. Sequential measurements in almost all the British endoscopy units over 4 years have shown gratifying and progressive improvement in the results.
In USA, the ASGE has initiated a system for “recognizing units” (3). To obtain recognition, a representative from the unit (doctor or senior nurse) must attend a 2 day seminar on key quality topics, and agree (in writing) to comply with the comprehensive ASGE guidelines in this context. The majority of endoscopists in each unit must be ASGE members. This program has been popular and many hundreds of units are now officially recognized. Emphasis is placed on quality improvement projects and processes.
Conclusion
No one involved in endoscopy doubts the importance of ensuring the highest possible quality of our processes and procedures. Many patients assume that any doctor offering a procedure is competent to do it, and that all facilities are equally safe (although some may look less appealing). The very simplicity of endoscopy as a “walk-in, walk-out” procedure can lull patients and practitioners alike into a sense of false security. Bad things can and do happen. Our profession must work harder to encourage the collection and dissemination of performance data. The fact that some endoscopists will be reluctant to document and advertise their performance should not stop us from doing the right thing. We should wear our data plainly and proudly as badges of quality. It will pay huge dividends eventually.
Figure 2.
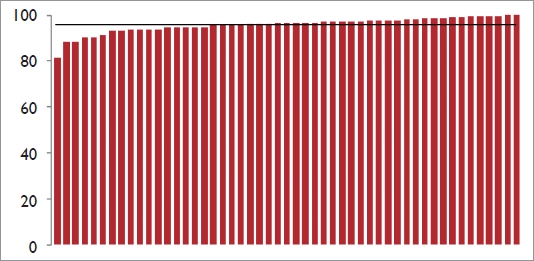
Biliary cannulation rates reported by participants in the ERCP Quality Network
Abbreviations
- ASGE
American Society for Gastrointestinal Endoscopy
- ACG
American College of Gastroenterology
- OMED
World Organization of Digestive Endoscopy
- JAG
Joint Advisory Group
- ERCP
Endoscopic Retrograde Cholangiopancreatography
- EMR
Endoscopic mucosal resection
- ESD
Endoscopic submucosal dissection
- ASA
American Society of Anesthesiology
- GIQuIC
GI Quality Improvement Consortium
- EUS
Endoscopic Ultrasonography
Biography
PETER B COTTON, MD., FRCP., FRCS
Peter Cotton was born in Herefordshire, England, where his father was a country physician. He was educated at Cambridge University and at St. Thomas Hospital Medical School (London), and graduated in 1963. He became interested in endoscopy in the late 1960's with the introduction of flexible fiberscopes, and developed endoscopy units at St. Thomas' Hospital and at the Middlesex Hospital, which pioneered and evaluated many diagnostic and therapeutic procedures, particularly ERCP. He attracted postgraduates from many countries, held numerous teaching courses, and introduced live CCTV workshops. In 1986 he became Professor of Medicine and Chief of Endoscopy at Duke University in North Carolina, USA. He developed a state of the art endoscopy center. He maintained his interests in teaching, evaluation of new techniques, and their impact on clinical outcome. He moved to Charleston, South Carolina in 1994 create a Digestive Disease Center dedicated to multi-disciplinary patient care, research and education.
He has been active in many National and International organizations, and has given invited lectures and demonstrations in more than 50 countries. He helped form the British Society for Digestive Endoscopy, became its president; and served the British Society of Gastroenterology as its vice president and treasurer. He was secretary of the European Society for Gastrointestinal Endoscopy, and president of the Pancreatic Society of Great Britain. He was elected Fellow of the Royal College of Physicians (London) in 1978, and Fellow of the Royal College of Surgeons (London) in 2002. Dr Cotton was awarded the Rudolph Schindler award of the American Society for Gastrointestinal Endoscopy in 2004.
Dr Cotton's clinical activities have focused on patients with known or suspected biliary and pancreatic problems, and their management by ERCP. He retired from clinical work in May 2011, but will continue in teaching and research, notably as principal investigator of an NIH-funded multi-center randomized shamcontrolled study of sphincterotomy in sphincter of Oddi dysfunction. In recent years Dr Cotton has also become more involved in quality issues in endoscopy, including objective assessment of performance and benchmarking.
“The tunnel at the end of light: my endoscopic journey in six decades”
His bibliography includes over 850 publications, with more than 250 original contributions in peer reviewed journals, and 8 books. “Practical Gastrointestinal Endoscopy” (co-authored by Christopher Williams) is the standard teaching text. Dr Cotton recently completed and published his memoirs, entitled “The tunnel at the end of the light: my endoscopic journey in six decades” (www.peterbcotton.com).
He is blessed with a wonderful wife and family, including 8 grandchildren, and one great-grandchild.
Footnotes
Presented at the 25th International Workshop on Therapeutic Endoscopy held at the Prince of Wales Hospital, Hong Kong on December 7th–9th 2010.
Previously published online: www.landesbioscience.com/journals/jig
References
- 1.Johanson JF, Schmitt CM, Deas TM, Jr, Eisen GM, Freeman M, Goldstein JL, et al. Quality and outcomes assessment in Gastrointestinal Endoscopy. Gastrointest Endosc. 2000;52:827–830. [PubMed] [Google Scholar]
- 2.Johanson JF. Continuous quality improvement in the ambulatory endoscopy center. Gastrointest Endosc Clin N Am. 2002;12:351–365. doi: 10.1016/s1052-5157(01)00015-0. [DOI] [PubMed] [Google Scholar]
- 3. www.asge.org.
- 4. www.acg.org.
- 5.Cotton PB, Hawes RH, Barkun A, Ginsberg GG, Amman S, Cohen J, et al. Excellence in endoscopy: toward practical metrics. Gastrointest Endosc. 2006;63:286–291. doi: 10.1016/j.gie.2005.04.048. [DOI] [PubMed] [Google Scholar]
- 6.Faigel DO, Cotton PB World Organization of Digestive Endoscopy, author. The London OMED position statement for credentialing and quality assurance in digestive endoscopy. Endoscopy. 2009;41:1069–1074. doi: 10.1055/s-0029-1215279. [DOI] [PubMed] [Google Scholar]
- 7. www.thejag.org.uk.
- 8. www.conjoint.org.au.
- 9.Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002;97:1296–1308. doi: 10.1111/j.1572-0241.2002.05812.x. [DOI] [PubMed] [Google Scholar]
- 10.Nelson EC, Splaine ME, Batalden PB, Plume SK. Building measurement and data collection into medical practice. Ann Intern Med. 1998;128:460–466. doi: 10.7326/0003-4819-128-6-199803150-00007. [DOI] [PubMed] [Google Scholar]
- 11.Cotton PB. How many times have you done this procedure, doctor? Am J Gastroenterol. 2002;97:522–523. doi: 10.1111/j.1572-0241.2002.05526.x. [DOI] [PubMed] [Google Scholar]
- 12.Cotton PB, Eisen G, Romagnuolo J, Vargo J, Baron T, Tarnasky P, et al. Grading the complexity of endoscopic procedures; results of an ASGE working party. Gastrointest Endosc. 2011;73:868–874. doi: 10.1016/j.gie.2010.12.036. [DOI] [PubMed] [Google Scholar]
- 13.Faigel DO, Pike IM, Baron TH, Chak A, Cohen J, Deal SE, et al. Quality indicators for gastrointestinal endoscopic procedures: an introduction. Am J Gastroenterol. 2006;101:866–872. doi: 10.1111/j.1572-0241.2006.00677.x. [DOI] [PubMed] [Google Scholar]
- 14.Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, Deal SE, et al. Quality indicators for endoscopic retrograde holangiopancreatography. Am J Gastroenterol. 2006;101:892–897. doi: 10.1111/j.1572-0241.2006.00675.x. [DOI] [PubMed] [Google Scholar]
- 15.Garrow D, Romagnuolo J, Cotton PB. Comparing ERCP practice and outcomes by level of experience. Gastrointest Endosc. 2009;69:AB231. [Google Scholar]
- 16.Pike IM, Vicari J. Incorporating quality measurement and improvement into a gastroenterology practice. Am J Gastroenterol. 2010;105:252–254. doi: 10.1038/ajg.2009.475. [DOI] [PubMed] [Google Scholar]
- 17. www.giquic.org.
- 18. www.grs.org.


