Abstract
Objective
To assess individual urologist variability using narrow-band imaging (NBI) cystoscopy to evaluate bladder tumours.
Patients and Methods
In all, 50 patients underwent white-light and NBI cystoscopy to evaluate for recurrent bladder tumours. Endoscopic images in each patient were independently viewed by four urologists assessing presence or absence of tumour. Their findings were correlated with biopsy results.
Results
In all, 26 patients had recurrent tumour and 24 had benign histology. There were no significant differences among urologists detecting recurrent tumour or in determining final pathology.
Conclusions
There does not appear to be a learning curve' for adapting to NBI-surveillance cystoscopy in patients with bladder cancer.
Keywords: cystoscopy, narrow-band imaging, surgeon variability
Introduction
Narrow-band imaging (NBI) cystoscopy is currently being investigated as a new method to detect recurrent bladder tumours [1]. Early reports suggest NBI may enhance detection of papillary tumours and carcinoma in situ over white-light (WLI) cystoscopy [2]. NBI cystoscopy is generally performed by one surgeon in a given case, and there is a lack of information regarding how well other surgeons may detect and view lesions in the same patients. NBI, like other new imaging methods, provides a subjective visual impression of abnormal mucosal areas. The likelihood that different surgeons may view, miss or regard suspected recurrent bladder tumours differently is an important question affecting whether NBI can be readily incorporated into routine clinical practice, or whether experience (i.e. ‘learning curve’) is required. We evaluated individual surgeon variability using NBI to assess for recurrent tumours in the same patients undergoing surveillance cystoscopy.
Patients and Methods
We (H.H., M.D., G.D., J.T.) evaluated 50 patients for recurrent bladder tumours using WLI and NBI cystoscopy. H.H. performed the actual surveillance cystoscopy and took endoscopic pictures of the procedure, including any lesions showing recurrent or suspected tumours. H.H. showed the images to M.D., G.D., and J.T., who were asked to determine whether lesions seen on NBI cystoscopy were tumours. Each urologist viewed the images independently and before results of a biopsy. H.H., M.D., and G.D. are experienced urological oncologists, who are beginning to use NBI to follow patients with bladder cancer. J.T. completed a urology residency and has just begun her fellowship in urological oncology, but she had no experience with NBI cystoscopy.
NBI findings for each surgeon evaluating the same cases were correlated with the biopsy results. Correlative statistics were used to compare differences among surgeons.
Results
All 50 patients had a history of recurrent non-muscle-invasive bladder tumours and were undergoing outpatient surveillance cystoscopy, including 18 after BCG therapy. A suspected lesion or abnormal area of mucosa was seen on WLI. The bladder was then evaluated by NBI cystoscopy. Each lesion(s) was biopsied and resected for histological evaluation. In all, 26 patients had a tumour and 24 had benign histology.
Table 1 shows individual surgeon variability in NBI findings to identify recurrent bladder tumours. H.H., M.D., and G.D. detected each patient with recurrent tumour, definitely identifying lesions as malignant or suspicious enough to warrant resection. J.T. missed three cases with cancer, because she did not consider the lesions in question significant to warrant a biopsy. G.D. and M.D. assessed six cases and seven cases, respectively, having malignant disease as benign on WLI, but changed their interpretations to cancer based on NBI cystoscopy. For H.H., M.D., G.D., and J.T., respectively, the sensitivity of detecting histological tumour using NBI was 92%, 77%, 77%, 69%; the specificity was 79%, 58%, 79%, 67%; positive predictive value was 83%, 67%, 80%, 69%; and the negative predictive value was 90%, 76%, 70%, 67%. M.D. had a lower specificity because she considered more lesions positive for tumour than other urologists, leading to biopsy of benign lesions. J.T. performed ≈10% worse than the experienced urologists, but overall, there was no significant differences between expert urologists using NBI (P = 0.4), or between experienced urologists and novice (P = 0.1) by Pearson's chi-square test or analysis of variance (two-sided).
TABLE 1. Individual surgeon variability identifying bladder lesions as recurrent tumour in the same patients by NBI cystoscopy.
| NBI finding by surgeon* | No. of patients | Pathology on biopsy, n (%) | |
|---|---|---|---|
| Tumour | No tumour | ||
| H.H. | |||
| Positive | 29 | 24 (83) | 5 (17) |
| Negative | 21 | 2 (10) | 19 (90) |
| M.D. | |||
| Positive | 30 | 20 (67) | 10 (33) |
| Negative | 20 | 6 (30) | 14 (70) |
| G.D. | |||
| Positive | 25 | 20 (80) | 5 (20) |
| Negative | 25 | 6 (24) | 19 (75) |
| J.T. | |||
| Positive | 26 | 18 (69%) | 8 (31) |
| Negative | 24 | 8 (33) | 16 (67) |
Each surgeon identified a suspected recurrent bladder tumour in each patient using NBI cystoscopy and then recorded whether the lesion was positive or negative for tumour on biopsy.
Discussion
Individual variation among urologists including a novice, using NBI cystoscopy to evaluate patients for recurrent bladder tumours was minimal. H.H. was advantaged because he knew the prior history of each patient, whereas the other urologists simply evaluated the images without such knowledge. All patients had lesions detected by WLI, often more clearly seen and characterized by NBI. As the purpose of follow-up cystoscopy is to detect recurrent tumour, each surgeon fulfilled this task, often aided by NBI.
A more difficult task for the urologist is to identify and distinguish lesions that are tumours from those that are benign histology, such as after BCG therapy. Correlating NBI findings with histology, there were no significant differences among urologists, including a novice who had never seen NBI cystoscopy. Her performance was only slightly behind experienced urologists, portending that she should improve rapidly as she becomes familiar with NBI cystoscopy and more experienced following patients with bladder cancer. Figures 1 and 2 show examples of bladder lesions and the urologists' interpretation.
FIG. 1.
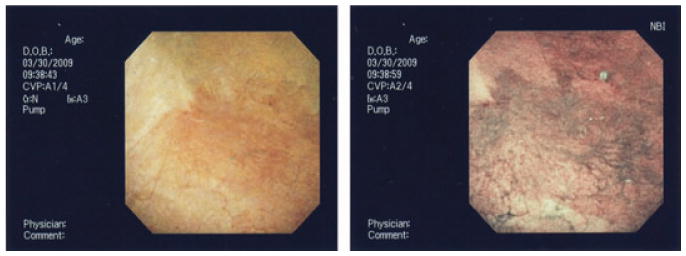
WLI (left) and NBI (right) cystoscopy of suspected bladder tumour. Based on NBI, each urologist correctly identified the lesions as carcinoma in situ.
FIG. 2.
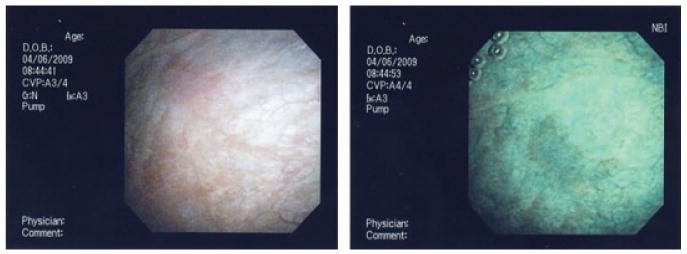
WLI (left) and NBI (right) of a lesion after BCG-therapy. Each surgeon identified the lesion on NBI. Biopsy showed inflammation only and no cancer. H.H., M.D., and G.D. correctly identified the lesion as benign, J.T. thought it was tumour.
Our methods can be criticised. Ideally, different urologists should independently evaluate the same patient at the same time with real-time WLI and NBI cystoscopy. However, as this was not practical or feasible, we elected to evaluate each patient's cystoscopic images before any biopsy became known. We recognize bias is introduced to the urologists viewing the images who are not doing the cystoscopy; however, this is more likely to exacerbate than to minimize any differences. As there were only minor disparities among the urologists including one inexperienced with NBI cystoscopy, we think our present methodology achieved the desired goals.
Experienced and a relatively inexperienced urologist adapted readily to NBI as a supplementary to WLI cystoscopy to evaluate patients with bladder cancer. Although it is unclear whether NBI cystoscopy will result in better outcomes, a long learning curve to detect and define recurrent bladder tumours does not appear necessary.
Abbreviations
- NBI
narrow-band imaging
- WLI
white-light
Footnotes
Conflict of Interest: None declared.
References
- 1.Bryan RT, Billingham LJ, Wallace DM. Narrow band imaging flexible cystoscopy in the detection of recurrent urothelial cancer of the bladder. BJU Int. 2007;101:702–6. doi: 10.1111/j.1464-410X.2007.07317.x. [DOI] [PubMed] [Google Scholar]
- 2.Herr HW, Donat SM. A comparison of white-light cystoscopy and narrow-band imaging cystoscopy to detect bladder tumour recurrences. BJU Int. 2008;102:1111–4. doi: 10.1111/j.1464-410X.2008.07846.x. [DOI] [PubMed] [Google Scholar]


