Abstract
This study examined the classification accuracy of the UPPS Impulsive Behavior Scale (UPPS) in discriminating several attention deficit/hyperactivity disorder (ADHD) subtypes, including predominantly inattentive type (ADHD/I), combined type (ADHD/C), and combined type with behavioral problems (ADHD/ODD), between each other and a non-ADHD control group using logistic regression analyses. The sample consisted of 88 children ranging in age from 9.0 years to 12.8 years, with a mean of 10.9 years. Children were predominantly male (74%) and Caucasian (86%) and in grades 3–7. Results indicated that the UPPS performed well in classifying ADHD subtypes relative to traditional diagnostic measures. In addition, analyses indicated that differences in symptoms between subtypes can be explained by specific pathways to impulsivity. Implications for the assessment of ADHD and conceptual issues are discussed.
Keywords: ADHD, Impulsivity, UPPS, ADHD subtypes
Attention-deficit/hyperactivity disorder (ADHD) is a common childhood disorder that is currently thought to have three primary symptoms: inattention, hyperactivity, and impulsivity. ADHD subtypes were first identified in DSM-III, and have since become the focus of considerable research examining the epidemiology, pathology, and symptomatology of these subtypes. According to the DSM-IV (American Psychiatric Association 2000), ADHD combined type (ADHD/C) is characterized both by 6 or more symptoms of hyperactivity/impulsivity, and 6 or more symptoms of inattention. In contrast, ADHD primarily inattentive type (ADHD/I) is characterized by symptoms of inattention, and ADHD primarily hyperactive/impulsive type (ADHD/HI) ADHD/HI is thought to be somewhat rare and is generally conceptualized as a pre-cursor to ADHD/C (Lahey et al. 2005). Because the criteria for ADHD/I reflect a subset of those for ADHD/C, it is often treated as a related, but less severe variant of ADHD/C, although others have argued that the inattentive subtype is a distinct and unrelated disorder (Milich et al. 2001).
One area of ADHD subtype research that is gaining considerable attention is subtype relations to impulsivity (Adams et al. 2008; Derefinko et al. 2008; Fillmore et al. 2009). Because impulsive and hyperactive behaviors characterize ADHD/C, significant effort over the past twenty years has focused on describing the specific nature of inhibitory deficits associated with the combined type (Barkley 1997; Pennington and Ozonoff 1996; Quay 1997). At this point, behavioral inhibitory deficits are among the most robust and reliable findings in the ADHD/C literature (Nigg 2005). However, given the theoretical differences between the impulsive nature of ADHD/C and the inattentive characterization of ADHD/ I, recent research has begun to investigate various aspects of inhibitory functioning between these subtype groups as a potentially fruitful domain through which to differentiate the subtypes (Derefinko et al. 2008; Nigg et al. 2002; Pasini et al. 2007). Thus, in order to determine whether ADHD/I is better characterized as a less severe variant or, instead, as a distinct diagnostic entity from ADHD/C, researchers are focused on comparing how the groups perform on measures and tasks purported to measure behavioral inhibition, as deficits in this area are regarded as central to ADHD/C.
ADHD and Impulsivity
The core symptoms of ADHD all have associations with a number of developmental problems, including poor social functioning, poor adjustment, internalizing disorders, and externalizing disorders (Barkley 1990; Gaub and Carlson 1997; Miller et al. 2007), as well as to problematic outcomes in adolescence and adulthood, including substance use (Flory et al. 2003), risky sexual behaviors (Flory et al. 2006), and criminal conduct (Babinski et al. 1999). In fact, there is evidence that ADHD and comorbid conduct problems interact, leading to a higher risk for substance abuse (Flory and Lynam 2003), including marijuana dependence and hard drug use and dependence (Flory et al. 2003). With respect to externalizing and antisocial behavior, Lynam (1996) documented the considerable overlap between hyperactivity-impulsivity-inattention (HIA) and conduct problems, suggesting that individuals with these symptoms are at greatest risk for chronic criminal offending. However, when specific symptoms and subtypes are examined, differences emerge, particularly with respect to impulsivity and comorbid psychopathology.
DSM-IV criteria stipulate that ADHD/C is characterized by not only inattention, but also impulsivity and it is these impulsivity characteristics that perhaps have led some to see ADHD/C as having more in common with conduct disorder than with ADHD/I (Milich et al. 2001). Indeed, relations among ADHD/C, impulsivity, and conduct disorder have been well established (see Colledge and Blair 2001; Faraone et al. 1998; Mathias et al. 2007). In fact, in a recent molecular genetics study, Caspi et al. (2008) provided further evidence for the heterogeneity of ADHD and asserted that meaningful divisions can be made based on the presence of antisocial behavior. Thus, measuring traits such as impulsivity that are associated with antisocial behavior may also prove important in distinguishing between ADHD subtypes.
Further, Nigg and colleagues have documented differences between ADHD subtypes in terms of cognitive and personality measures and have suggested that meaningful contributions can be made by personality measures of inhibition in understanding the mechanisms underlying ADHD (see Nigg et al. 2007). Specifically, attention problems were linked to low conscientiousness and resiliency, hyperactivity-impulsivity was linked to low reactive control, conduct-impulsivity was linked to low agreeableness, oppositional defiant symptoms were linked to high negative emotionality, and total ADHD symptoms were linked to low agreeableness and conscientiousness and high neuroticism (Martel and Nigg 2006; Nigg et al. 2002). Many of these scales represent aspects of disinhibition (impulsivity) and demonstrate not only the importance of impulsivity in ADHD, but also the presence of meaningful differences in impulsivity between the ADHD subtypes.
Using the UPPS to Explore ADHD Impulsivity
With the recognition that impulsivity is a multifaceted construct, Whiteside and Lynam (2001) developed the UPPS Impulsive Behavior Scale (UPPS) via factor-analytic methods. The scale measures four distinct pathways to impulsivity: Urgency (URG), (lack of) Premeditation (loPRE), (lack of) Perseverance (loPSV), and Sensation Seeking (SS). Urgency refers to the tendency to act impulsively when experiencing negative affect. Lack of Premeditation refers to a failure to reflect on the consequences of an act before engaging in that act. Lack of Perseverance refers to an inability to focus or follow through on difficult or boring tasks. Sensation Seeking, as it is assessed on the UPPS, refers to “a tendency to enjoy and pursue activities that are exciting and an openness to trying new experiences that may be dangerous” (Whiteside et al. 2005, p. 561).
Although there is consensus that impulsivity is central to ADHD, the extent to which it plays a role across subtypes remains unclear (Baeyens et al. 2006). There is mounting evidence that there are not only marked differences between subtypes, but also that ADHD/I and ADHD/C are separable disorders with different underlying pathology (Derefinko et al. 2008; Diamond 2005; Milich et al. 2001). Diamond (2005) posits that ADHD/I may reflect boredom susceptibility more than distractibility. In fact, “distractible” (in addition to “disinhibited” and “hyperactive”) has been described as one of the relevant symptoms of ADHD/C (Milich et al. 2001). Despite the evidence supporting ADHD subtypes as different disorders, research is still emerging. The multifaceted nature of the UPPS provides a unique opportunity to further flesh out subtype differences and perhaps improve classification. (Lack of) Premeditation and (lack of) Perseverance are not unlike reactive control and resiliency, which have been mapped onto ADHD/I and ADHD/C, respectively (Martel and Nigg 2006), and may be particularly useful in assessing these subtypes.
The UPPS also provides information about disorders comorbid with ADHD, such as conduct disorder. Indeed, impulsivity was found to be the core feature most common to ADHD and conduct disorder (Colledge and Blair 2001; Mathias et al. 2007; Moeller et al. 2001). Furthermore, when combined with oppositional defiant disorder and/or conduct disorder, ADHD/C relates more strongly with externalizing problems (e.g., acts of violence; Guang-Wen et al. 2005). Given the UPPS's impulsivity and conduct disorder-relevant content, it may improve the classification of ADHD subtypes, as well as inform us about important underlying differences among the subtypes.
Current Study
The current study examines the ability of the UPPS to differentiate the inattentive and combined ADHD subtypes, as well as the group composed of both ADHD combined type and comorbid conduct problems. That is, using logistic regression we examine the incremental diagnostic utility of the UPPS scales and attempt to provide clarity to the understanding of specific aspects or features thought to be central to ADHD subtypes and ADHD/ODD. To the extent that differences in impulsivity across ADHD subtypes are meaningful, we expect the UPPS to provide good diagnostic classification accuracy. Additionally, we expect the ADHD subtypes to differ in their relations to UPPS impulsivity scales. Thus, as a further test, we conducted analyses to determine which aspects of impulsivity via the UPPS account for differences in ADHD symptomatology between the ADHD subtypes and ADHD/ODD. Specifically, we believe ADHD/I will be best characterized by UPPS (lack of) Perseverance, and ADHD/C and ADHD/ODD will be best characterized by UPPS (lack of) Premeditation.
Method
Participants
A sample of 60 children with ADHD and 21 comparison children participated in this study. The children in each diagnostic group were between the ages of 9 and 12 years (M = 10.86 years, SD = 1.09). Approximately 85% of the children were Caucasian, 11% were African American and 4% identified themselves as other. The children with ADHD were recruited from the Hyperactive Children's Clinic in the School of Medicine at the University of Kentucky. The children were carefully selected to fulfill the DSM-IV criteria for ADHD inattentive, ADHD combined, or ADHD combined with comorbid behavioral problems and to be free of confounding factors (i.e., low IQ, neurological problems). Diagnoses were based on a convergence of evidence from multiple informants and multiple measures.
Chart Review and Screening
Children were first required to have received the appropriate DSM-IV ADHD diagnosis (i.e., inattentive or combined) based on a comprehensive psychiatric clinic evaluation at the Hyperactive Children's Clinic. This evaluation utilizes multiple assessment procedures designed to identify psychiatric and neurological factors that may influence or better account for ADHD symptoms, such as mood disorders, developmental disorders, epilepsy or neurological disorders, or mental retardation. In addition, the medical charts of all the children were reviewed in detail to gather specific information about ADHD diagnoses and medical history, including reason for clinic referral, age at onset of symptoms, classroom behavior via teacher ratings, evidence of impairment, parent ratings of behavior, IQ, medical history, and comorbid diagnoses. Children were excluded from the study if their medical charts provided evidence of IQ scores lower than 80, presence of sensory impairments, diagnoses of epilepsy or other neurological disorders, or prescribed medication that could not be temporarily discontinued during study participation. Further, children who were diagnosed by the Hyperactive Children's Clinic with ADHD primarily hyperactive/impulsive subtype were excluded from the study.
If the above criteria were met, then a parent of the child with ADHD was contacted. A semi-structured interview, similar to the P-ChIPS (Weller et al. 2000), but only consisting of verbatim DSM-IV criteria for ADHD and ODD, was conducted with the parent to confirm the child's diagnostic status. The interviews were conducted by trained graduate students in clinical psychology. In the interview, the parent was asked whether each diagnostic criterion was true of his/her child. If a criterion was endorsed, the parent was asked a) to give behavioral examples, b) to provide information regarding whether that behavior seemed inappropriate for the child's age, and c) whether it impaired the child's functioning academically and/or socially. A diagnostic criterion was considered to be endorsed only if the parent indicated the behavior was age inappropriate and impairing. This interview procedure has been used successfully by our research group in previous studies, with interrater reliabilities for the number of ADHD symptoms endorsed by the parent above 95% (e.g., Lorch et al. 1999). The data for children whose parental interviews supported an ADHD diagnosis were retained for analysis in this study. In addition to the DSM-IV semi-structured interview, parents completed the Conners (1997) Parent Rating Scales (CPRS-R:S), the Child Behavior Checklist (Achenbach 1991), a parent-report version of the UPPS (Whiteside and Lynam 2001), and the Childhood Psychopathy Scale (Lynam 1997).
Diagnostic Subgroups
Children with ADHD were assigned to one of the three subgroups under investigation (ADHD/I; ADHD/C; ADHD/ODD) based upon the semi-structured DSM-IV interview, CPRS-R:S, and CBCL scores.
To be placed in the ADHD/I group, children were required to meet criteria for attention problems on the DSM-IV interview, have T scores above 60 on the Conners Cognitive Problems/Inattention scale, have three or fewer symptoms of hyperactivity/impulsivity on the DSM-IV interview, have T scores less than 60 on the Conners Hyperactivity scale, and have T scores below 60 on the CBCL Aggression and Delinquency scales.
To be placed in the ADHD/C group, children were required to meet criteria for attention problems and hyperactivity/impulsivity on the DSM-IV interview, have T scores above 60 on the Conners Hyperactivity and ADHD scales, and have T scores below 60 on the CBCL Aggression and Delinquency scales.
To be placed in the ADHD/ODD group, children were required to meet criteria for attention problems and hyperactivity/impulsivity on the DSM-IV interview, have T scores above 60 on the Conners Hyperactivity and ADHD scales, and have a CBCL Aggression or Delinquency T score above 60.
Seventeen children were placed in the ADHD/I group, 22 were placed in the ADHD/C group, and 21 were placed in the ADHD/ODD group. Consistent with the exclusion criteria utilized at the first stage of recruitment, no children with ADHD hyperactive/impulsive subtype were identified. Table 1 summarizes the mean scores on these diagnostic measures for ADHD children. Groups differed significantly on the relevant diagnostic indicators.
Table 1.
Descriptive variables: means and standard deviations by group
| Comparison |
ADHD/I |
ADHD/C |
ADHD/ODD |
|||||
|---|---|---|---|---|---|---|---|---|
| (N=21) |
(N=17) |
(N=22) |
(N =21) |
|||||
| M | SD | M | SD | M | SD | M | SD | |
| Age (months) | 131.19 | 11.31 | 125.12 | 13.63 | 132.73 | 12.53 | 130.81 | 15.63 |
| Gender | .333 | .483 | .353 | .493 | .182 | .395 | .143 | .359 |
| Father's Education | 16.0 | 2.03 | 16.0 | 3.30 | 14.23 | 3.61 | 14.47 | 3.32 |
| Mother's Education | 16.38 | 1.75 | 15.29 | 1.99 | 15.55 | 2.11 | 15.69 | 3.01 |
| DSM ATT | .520 | 1.12 | 6.18 | 2.60 | 6.68 | 2.03 | 7.90 | 1.51 |
| DSM HYP | .380 | .669 | 1.47 | 1.46 | 4.82 | 1.68 | 6.14 | 2.78 |
| DSM OPP | .190 | .402 | 1.06 | 1.30 | 2.05 | 1.46 | 4.67 | 2.08 |
| Connors ATT | 45.05 | 3.78 | 71.53 | 9.26 | 71.82 | 7.73 | 74.05 | 9.45 |
| Connors HYP | 47.76 | 5.14 | 53.06 | 11.56 | 74.23 | 8.85 | 79.76 | 11.16 |
| Connors OPP | 42.76 | 3.91 | 50.41 | 8.28 | 54.68 | 10.09 | 68.71 | 9.36 |
| UPPS URG | 21.91 | 6.84 | 30.29 | 6.16 | 30.91 | 4.84 | 38.57 | 5.32 |
| UPPS loPRE | 22.14 | 4.96 | 28.00 | 5.98 | 31.24 | 4.46 | 36.33 | 4.62 |
| UPPS loPSV | 19.10 | 4.83 | 30.77 | 5.29 | 29.81 | 4.14 | 32.91 | 3.69 |
| UPPS SS | 30.14 | 8.97 | 25.75 | 9.88 | 27.77 | 9.61 | 34.81 | 7.39 |
a ADHD/I ADHD primarily inattentive type; b ADHD/C ADHD combined type; c ADHD/ODD ADHD with comorbid conduct problems; d UPPS URG UPPS urgency; e UPPS loPRE UPPS (lack of) premeditation; f UPPS loPSV UPPS (lack of) perseverance; g UPPS SS UPPS sensation seeking; h Males were coded as 0 and females were coded as 1 for Gender; i DSM scores based on semi-structured interview
The comparison group of children without ADHD was recruited through newspaper advertisements, posted advertisements in the community, and by word-of-mouth. They were screened during a recruitment phone call in which the parents were asked if their child had ever been referred for any behavioral or learning problems. The comparison children were not required to be symptom free, but had to have two or fewer symptoms in a diagnostic category. These children were significantly less symptomatic than the children with ADHD in terms of the DSM-IV criteria for inattentive symptoms and hyperactivity symptoms, and moreover did not meet diagnostic criteria for any subtype of ADHD. In addition, the children in the comparison group had to have T scores below 60 on all of the relevant rating scales. As indicated in Table 1, the diagnostic interview and rating scale data successfully differentiated between the comparison children and the three ADHD groups.
All children received two small toys and $30.00 for their participation in the study. Groups were not significantly different on the basis of age, gender, racial composition, grade level, maternal education, or paternal education, or KBIT composite scores.
Procedure
The study took place at the Neurocognition Research Laboratory in the Department of Psychology at the University of Kentucky. All children were tested individually. Testing occurred on a non-school day between the hours of 9 am and 5 pm. Upon arrival at the lab the child and parent were greeted by two experimenters who described the general details of the study and the basic testing procedures. Written consent was then obtained from the parent and verbal assent was obtained from the child. After obtaining consent, one of the experimenters accompanied the parent to an interview room to complete the semi-structured interview and questionnaires. The other experimenter accompanied the child to a nearby testing room to complete part of a larger test battery that contained neuropsychological tests and other measures of cognitive functioning. At the conclusion of the session, the child and parent were debriefed and paid for their participation.
Measures
Conners’ Parent Rating Scale—Revised: Short Form (CPRS-R:S)
The Conners’ Parent Rating Scale–Revised: Short Form (CPRS–R:S; Conners 1997) is a 27-item screening instrument that assesses all of the 12 criteria that are listed in the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text revision [DSM–IV–TR]; American Psychiatric Association 2000) for attention deficit hyperactivity disorder (ADHD). The child's parent is asked to rate how much each of the symptoms has been problematic for the child during the last month using a 4-point scale ranging from 0 (not true at all) to 3 (very much true). The CPRS–R:S is used with children between the ages of 3 and 17. Parent ratings are summed to yield Oppositional, Cognitive Problems/Inattention, and Hyperactivity scales (Conners 1997).
Child Behavior Checklist (CBCL)
The parent-version of the CBCL (Achenbach 1991) is one of the most widely used assessments of parent's perceptions of behavioral and social problems of their children. The CBCL consists of 118 behavioral and emotional items used to form eight empirically derived scales: withdrawn, somatic complaints, anxious/depressed, social problems, thought problems, attention problems, aggressive behavior and delinquent behavior. Several studies have supported the psychometric properties of the CBCL, showing good reliability and validity in both clinical and non-clinical populations.
UPPS Impulsivity Scale—Parent Report Version (UPPS)
The UPPS (Whiteside and Lynam 2001) is a 45-item parent-completed inventory designed to measure four personality pathways to impulsive behavior. The UPPS consists of 4 subscales, including (lack of) Premeditation (loPRE; 11 items), Urgency (URG; 12 items), Sensation Seeking (SS; 12 items), and (lack of) Perseverance (loPSV; 10 items). Whiteside and Lynam (2001) found that the UPPS demonstrates excellent internal consistency and convergent validity, and later studies have indicated that the subscales of the UPPS make unique contributions to different disorders, suggesting that these subscales represent important aspects of impulsivity not assessed in other impulsivity measures (Whiteside et al. 2005). Coefficient alphas in the current study for loPRE, URG, SS, and loPSV were .89, .91, .93, and .90, respectively.
Results
Profile Construction and Differences between ADHD Subtypes
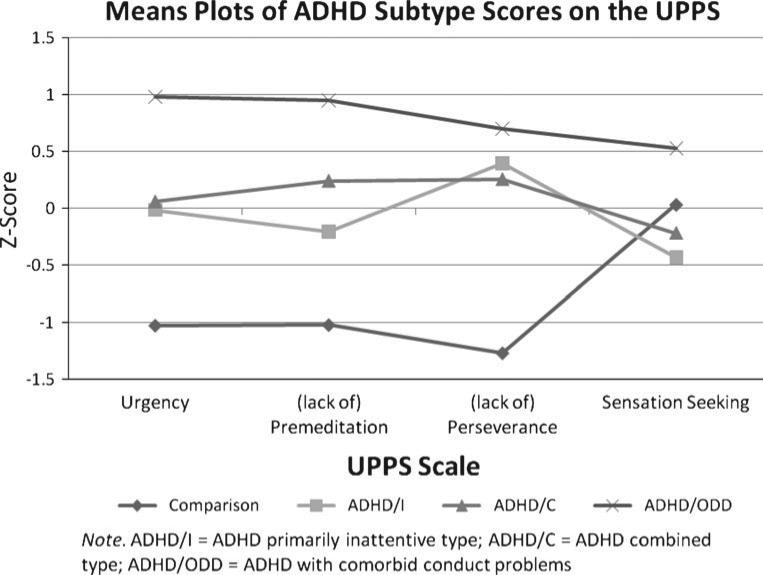
One-way ANOVAs were used to detect whether ADHD subtype means were significantly different on the UPPS scales (see Fig. 1). Results indicated significant differences between subtypes on UPPS URG (F (3, 77) = 28.86, p<.001), loPRE (F (3, 76) = 29.76, p<.001), loPSV (F (3, 76) = 39.28, p<.001), and SS (F (3, 76) = 3.66, p<.05). Post-hoc Tukey HSDs were used to determine the nature of significant differences. Results indicated that children with an ADHD/ODD diagnosis scored significantly higher than all other subtypes on UPPS URG (all ps < .001), and loPRE (all ps < .05). The children with any ADHD subtype diagnosis scored significantly higher than the non-ADHD comparison group on UPPS URG (all ps < .001), loPRE (all ps < .01), and loPSV (all ps < .001). Children with an ADHD/I diagnosis did not differ significantly from those with an ADHD/C diagnosis on the UPPS scales.
Fig. 1.
Means plots of ADHD subtypes on the UPPS
ANCOVAs were conducted to determine whether differences between subtypes in ADHD symptoms could be accounted for by pathways to impulsivity (see Table 2). That is, we examined which aspects of impulsivity could explain the symptom differences thought to be the distinguishing features of the subtypes (e.g. hyperactivity and ADHD/C). ADHD symptom variables were computed by summing standardized DSM-IV interview and CPRS-R: S symptom counts. The ADHD subtype groups obtained significantly higher symptom counts on inattention, hyperactivity, and oppositional symptoms compared to non-ADHD comparison group. UPPS loPSV was able to account for differences in inattention and hyperactivity symptoms between the non-ADHD comparison and ADHD/I groups. In addition, although none of the UPPS scales were significant covariates in accounting for ADHD/I and ADHD/C subtype differences in hyperactivity symptoms, UPPS URG was a significant covariate in accounting for differences in oppositional symptoms between the ADHD/C and ADHD/ODD groups.
Table 2.
ANCOVA results for UPPS scales predicting inattention and oppositional symptoms
| Model | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| ATT Model 1 | 109.74 | 1 | 109.74 | 245.35 | .000 |
| Intercept | 19.17 | 1 | 19.17 | 42.85 | .000 |
| Group | 109.74 | 1 | 109.74 | 245.35 | .000 |
| Error | 16.10 | 36 | .447 | ||
| ATT Model 2 | 115.22 | 3 | 38.41 | 122.92 | .000 |
| Intercept | 9.65 | 1 | 9.65 | 30.87 | .000 |
| Group | .46 | 1 | .46 | 1.46 | .24 |
| PSV | 4.84 | 1 | 4.84 | 15.48 | .000 |
| Group × PSV | .72 | 1 | .72 | 2.29 | .14 |
| Error | 10.62 | 34 | .31 | ||
| OPP Model 1 | 59.41 | 1 | 59.41 | 28.27 | .000 |
| Intercept | 76.33 | 1 | 76.33 | 36.32 | .000 |
| Group | 59.41 | 1 | 59.41 | 28.27 | .000 |
| Error | 86.17 | 41 | 2.10 | ||
| OPP Model 2 | 86.87 | 3 | 28.96 | 19.24 | .000 |
| Intercept | 13.96 | 1 | 13.96 | 9.27 | .004 |
| Group | 3.28 | 1 | 3.28 | 2.18 | .15 |
| URG | 26.58 | 1 | 26.58 | 17.66 | .000 |
| Group × URG | 1.68 | 1 | 1.68 | 1.12 | .30 |
| Error | 58.70 | 39 | 1.51 |
a ATT Inattention Symptoms; b OPP Oppositional Symptoms
UPPS Prediction and Classification Accuracy
To determine which UPPS scales were the best predictors of ADHD subtypes, we conducted a multinomial logistic stepwise regression analysis using forward entry (entry probability = .05; removal probability = .10). Urgency (URG), (lack of) Premeditation (loPRE), and (lack of) Perseverance (loPSV) were the only predictors left in the model and all three significantly improved the χ2 value (p<.001; see Table 3). Next, odds ratios (ORs) were calculated for each unique predictor (see Table 4).
Table 3.
Prediction and classification accuracy for UPPS
| Variables | –2 Log Likelihood | df | p | Classification Accuracy (Final Model) |
|---|---|---|---|---|
| Intercept Only | 215.36 | 9 | .000 | Comparison: 90.5% |
| URG | 106.04 | ADHD/I: 56.2% | ||
| loPRE | ADHD/C: 65.0% | |||
| loPSV | ADHD/ODD: 81.0% | |||
| Model χ2 | 109.31 | Overall %: 74.4 |
a ADHD/I ADHD primarily inattentive type; b ADHD/C ADHD combined type; c ADHD/ODD ADHD with comorbid conduct problems; d URG UPPS urgency; e loPRE UPPS (lack of) premeditation; f loPSV UPPS (lack of) perseverance
Table 4.
UPPS prediction subtype comparisons
| Comparison | Distinguishing Factor (Odds Ratio) |
|---|---|
| ADHD/I vs. Comparison | loPSV (1.69**) |
| ADHD/ODD vs. Comparison | URG (1.61***), loPRE (1.56*), loPSV (1.51*) |
| ADHD/C vs. ADHD/I | loPRE (1.30*), loPSV (.80*) |
| ADHD/ODD vs. ADHD/C | URG (1.37*), loPRE (1.31*) |
| ADHD/I vs. ADHD/ODD | URG (.69**), loPRE (.59***) |
a ADHD/I ADHD primarily inattentive type; b ADHD/C ADHD combined type; c ADHD/ODD ADHD with comorbid conduct problems; d URG UPPS urgency; e loPRE UPPS (lack of) premeditation; f loPSV UPPS (lack of) perseverance; g Only significant relations reported
p < .001.
p < .01.
p < .05
ADHD Subtypes vs. Comparison Group
UPPS loPSV uniquely distinguished ADHD/I from the non-ADHD comparison group (see Table 3). Specifically, the odds of having a diagnosis of ADHD/I increase by 69% for a one unit increase in loPSV. Additionally, UPPS URG, loPRE, and loPSV uniquely distinguished ADHD/ODD from the non-ADHD comparison group. URG and loPSV did not uniquely distinguish ADHD/C from the non-ADHD comparison group, but odds-ratios approached significance (p<.08).
Comparison Among ADHD Subtypes
UPPS loPRE and loPSV uniquely distinguished ADHD/C from ADHD/I. Specifically, the odds of having a diagnosis of ADHD/C increase by 30% for a one unit increase in loPRE and decrease by 20% for a one unit increase in loPSV. Additionally, UPPS URG and loPRE uniquely distinguished ADHD/ODD from ADHD/C. Specifically, the odds of having a diagnosis of ADHD/ODD increase by 37% and 31% for a one unit increase in URG and loPRE, respectively. Lastly, UPPS URG and loPRE uniquely distinguished ADHD/I from ADHD/ODD. Specifically, the odds of having a diagnosis of ADHD/I decrease by 31% and 41% for a one unit increase in URG and loPRE, respectively.
Classification Accuracy
Multinomial logistic regression was used to determine the classification accuracy of the best predictors from the UPPS (see Table 3). Classification accuracy is a measure of the number of cases correctly classified and is equal to the sum of true positives and true negatives, divided by the total number of cases. The UPPS classified ADHD with an overall accuracy of 74.4% and was most accurate in classifying the comparison group.
Discussion
The current study examined the utility of a multidimensional measure of impulsivity, the UPPS, to differentiate between ADHD subtypes. Consistent with previous evidence (Caspi et al. 2008, Faraone et al. 1998; Lynam 1996), children with ADHD/ODD were characterized by the highest levels of impulsivity, followed by children with ADHD/C and ADHD/I. That is, as the number of ADHD symptoms and comorbid disorders increased, so too did the number of symptoms related to impulsivity. Because impulsivity is the trait most common to ADHD and conduct disorder (Mathias et al. 2007) it is not surprising that specific impulsivity traits played a significant role in explaining differences between ADHD/C and ADHD/ODD subtypes. However, contrary to our expectations, UPPS loPRE did not account for their mean difference in oppositional symptoms. Rather, UPPS URG accounted for differences between these subtypes, which is consistent with previous studies finding significant relations between negative emotionality and oppositional defiant disorder symptoms and not inattention or hyperactivity-impulsivity symptoms (Martel and Nigg 2006) as well as developmental theories emphasizing the interaction between Control (impulsivity) and Negative Emotionality in the development of psychopathology (Eisenberg et al. 1996). Thus, in terms of impulsivity, developing oppositional symptoms may be less about an increased failure to anticipate or consider consequences and more about an increased failure to regulate one's actions and impulses when experiencing negative affect. As Martel and Nigg (2006) suggest, relations between oppositional symptoms negative emotionality in ADHD may result from comorbid antisocial traits. Nevertheless, this provides further evidence for UPPS URG as a useful trait in understanding how ADHD/C and ADHD/ODD differ.
With respect to ADHD/I, our hypothesis that it would be best characterized by UPPS loPSV was only partially supported. That is, ADHD/I was made up of UPPS loPSV, but also levels of UPPS URG and SS comparable to ADHD/C. Despite ADHD/I being predominantly characterized by symptoms of inattention, our results parallel descriptions of the ADHD/I subtype as somewhat heterogeneous (Carlson and Mann 2002). Indeed, previous research has found these children to have some impulsive characteristics (e.g. poor executive response inhibition and effortful control; Nigg et al. 2007). That is, the difference between hyperactivity symptoms in ADHD/I and ADHD/C could not be accounted for by any one UPPS scale, but the mean difference became nonsignificant when all UPPS scales were in the model. Thus, the comparison of hyperactivity symptom differences between the ADHD/I and ADHD/C subtypes supported the existence of several impulsive traits. The fact that not one, but all UPPS scales accounted for ADHD/I and ADHD/C subtype differences is important because it demonstrates that both subtypes are made up of several impulsive traits, but also that they differ little in them.
Although the ADHD/C group generally had higher levels of impulsivity than ADHD/I, this was not true across all facets of impulsivity. Interestingly, the exception occurred on UPPS loPSV, as children with ADHD/I appeared to struggle following through on tasks more so than those with ADHD/C. Further, UPPS loPSV appeared to be particularly salient when comparing the non-ADHD comparison group and the ADHD/I group by accounting for differences in both inattention and hyperactivity symptoms. Thus, ADHD/I children are also more impulsive than children without ADHD, but this impulsivity is characterized by an inability to finish tasks when feeling fatigued or bored. Thus, we believe that the increased hyperactivity/impulsivity ratings seen in ADHD/I children compared to those without ADHD can be largely explained by UPPS loPSV. Unfortunately, it remains unclear if children with ADHD/I leave tasks unfinished because they are unmotivated and choose to give up (e.g. cognitive-sluggishness) or because they have trouble focusing on one thing for a sustained period of time and tend to move from activity to activity frequently (e.g. distractibility or boredom-susceptibility). Due to the ADHD/I group's relative low level of UPPS SS, we believe the former is more probable. Although differences were small, these results are nonetheless interesting due to the fact that few have considered children with ADHD/I to be impulsive. Thus, it may be that ADHD subtypes cannot be classified as simply “impulsive” and “not impulsive.” Rather, it may involve how children look on several facets of impulsivity.
Clinical Implications
Accurate classification has also been shown to be have practical applications in terms of behavioral problem trajectories (Loeber and Stouthamer-Loeber 1998; Lynam 1996; Moffitt 1993; Waschbusch 2002), comorbid psychopathology, school and social functioning, academic achievement (Faraone et al. 1998; Milich et al. 2001), and treatment response/outcome (Barkley et al. 1991; Faraone et al. 1998). For example, children with ADHD/C are more likely to have comorbid externalizing disorders (e.g. conduct disorder; Faraone et al. 1998) and children with both ADHD/C and conduct disorder are more likely to engage in externalizing behaviors (Guang-Wen et al. 2005) and develop substance use and dependence symptoms (Molina et al. 1999; Flory et al. 2003).
To this end, the UPPS appears to represent a measure relevant to both ADHD subtype classification and behavioral problem trajectories. The UPPS demonstrated good predictive validity and classification accuracy for ADHD subtypes and ADHD/ODD. Specifically, Urgency (URG), (lack of) Premeditation (loPRE), and (lack of) Perseverance (loPSV) appeared to be the pathways to impulsivity most salient in ADHD. These three subscales demonstrated an overall classification accuracy similar to the BASC parent rating scale and better than the BASC teacher rating scale and CBCL (Vaughn et al. 1997). While previous research has subtyped ADHD with behavioral problem trajectories (i.e., antisocial behavior; Caspi et al. 2008), it is interesting that subtypes emerge similarly at the trait level using impulsivity. That is, while diagnostic criteria for ADHD subtypes are almost entirely based on behaviors, they are also inextricably linked to underlying traits (e.g., impulsivity, negative emotionality). Thus, the use of the UPPS in identifying subtypes demonstrates the importance of impulsivity in understanding children's behavior in multiple areas and may inform treatment interventions.
Limitations and Future Directions
The small sample size may also have impaired our ability to detect significant differences between ADHD/I and ADHD/C. With the current sample size, we have a 6% chance of detecting a significant mean difference. In order to increase our power to .80, we would need to increase the sample size by 545 children.
Given the importance of impulsivity in understanding ADHD and its subtypes, future research would do well to attempt to tease apart the salience of different types of impulsivity across subtypes, age, and gender. In the same way that age and gender have been shown to inform the diagnosis of ADHD subtypes (Nolan et al. 1999), impulsivity may also inform diagnosis and/or interact with age and gender.
Acknowledgements
This research was supported by grants DA021027 and DA005312 from the National Institute on Drug Abuse.
Contributor Information
Drew J. Miller, Department of Psychological Sciences, Purdue University, West Lafayette, IN 47907, USA
Karen J. Derefinko, Department of Psychology, University of Kentucky, Lexington, KY, USA
Donald R. Lynam, Department of Psychological Sciences, Purdue University, West Lafayette, IN 47907, USA
Richard Milich, Department of Psychology, University of Kentucky, Lexington, KY, USA.
Mark T. Fillmore, Department of Psychology, University of Kentucky, Lexington, KY, USA
References
- Achenbach TM. Manual for the child behavior checklist/4–18 and 1991 profile. University of Vermont Department of Psychiatry; Burlingon: 1991. [Google Scholar]
- Adams ZW, Derefinko KJ, Milich R, Fillmore MT. Inhibitory functioning across ADHD subtypes: recent findings, clinical implications, and future directions. Developmental Disabilities Research Reviews. 2008;14:268–275. doi: 10.1002/ddrr.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders-text revision. 4th ed. Author; Washington, DC: 2000. [Google Scholar]
- Babinski LM, Hartsough CS, Lambert NM. Childhood conduct problems, hyperactivity-impulsivity, and inattention as predictors of adult criminal activity. Journal of Child Psychology and Psychiatry. 1999;40:347–355. [PubMed] [Google Scholar]
- Baeyens D, Roeyers H, Walle JV. Subtypes of Attention-Deficit/Hyperactivity Disorder (ADHD): distinct or related disorders across measurement levels? Child Psychiatry and Human Development. 2006;36:403–417. doi: 10.1007/s10578-006-0011-z. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment. Guilford; New York: 1990. [Google Scholar]
- Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Barkley RA, DuPaul GJ, McMurray MB. Attention deficit disorder with and without hyperactivity: clinical response to three dose levels of methylphenidate. Pediatrics. 1991;87:519–531. [PubMed] [Google Scholar]
- Carlson CL, Mann M. Sluggish cognitive tempo predicts more severe impairment in the ADHD, predominantly inattentive type. Journal of Clinical Child and Adolescent Psychology. 2002;31:123–129. doi: 10.1207/S15374424JCCP3101_14. [DOI] [PubMed] [Google Scholar]
- Caspi A, Langley K, Milne B, Moffitt TE, O'Donovan M, Owen MJ, et al. A replicated molecular genetic basis for subtyping antisocial behavior in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2008;65:203–210. doi: 10.1001/archgenpsychiatry.2007.24. [DOI] [PubMed] [Google Scholar]
- Colledge E, Blair RJR. The relationship in children between inattention and impulsivity components of attention deficit and hyperactivity disorder and psychopathic tendencies. Personality and Individual Differences. 2001;30:1175–1187. [Google Scholar]
- Conners CK. Conners'rating scales–revised: Technical manual. Multi-Health Systems; North Tonawanda: 1997. [Google Scholar]
- Derefinko KJ, Adams ZW, Milich R, Fillmore MT, Lorch EP, Lynam DR. Response style differences in the inattentive and combined subtypes of attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2008;36:745–758. doi: 10.1007/s10802-007-9207-3. [DOI] [PubMed] [Google Scholar]
- Diamond A. Attention-deficit disorder (attention-deficit/hyperactivity disorder without hyperactivity): a neurobiologically and behaviorally distinct disorder from attention deficit/hyperactivity (with hyperactivity). Development and Psychopathology. 2005;17:807–825. doi: 10.1017/S0954579405050388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Guthrie IK, Murphy BC, Maszk P, Holmgren R, et al. The relations of regulation and emotionality to problem behavior in elementary school children. Development and Psychopathology. 1996;8:141–162. [Google Scholar]
- Faraone SV, Biederman J, Weber W, Russell RW. Psychiatric, neuropsychological, and psychosocial features of DSM-IV subtypes of attention-deficit/hyperactivity disorder: results from a clinically referred sample. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:185–193. doi: 10.1097/00004583-199802000-00011. [DOI] [PubMed] [Google Scholar]
- Fillmore MT, Milich R, Lorch EP. Inhibitory deficits in children with Attention-Deficit/Hyperactivity Disorder: Intentional versus automatic mechanisms of attention. Development and Psychopathology. 2009 doi: 10.1017/S0954579409000297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flory K, Lynam DR. The relation between attention deficit hyperactivity disorder and substance abuse: what role does conduct disorder play? Clinical Child and Family Psychology Review. 2003;6:1–16. doi: 10.1023/a:1022260221570. [DOI] [PubMed] [Google Scholar]
- Flory K, Milich R, Lynam DR, Leukefeld C, Clayton R. Relation between childhood disruptive behavior disorders and substance use and dependence symptoms in young adulthood: individuals with symptoms of attention-deficit/hyperactivity disorder are uniquely at risk. Psychology of Addictive Behaviors. 2003;17:151–158. doi: 10.1037/0893-164x.17.2.151. [DOI] [PubMed] [Google Scholar]
- Flory K, Molina BS, Pelham WE, Jr., Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology. 2006;35:571–577. doi: 10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- Gaub M, Carlson CL. Behavioral characteristics of DSM-IV ADHD subtypes in a school-based population. Journal of Abnormal Child Psychology. 1997;25:103–111. doi: 10.1023/a:1025775311259. [DOI] [PubMed] [Google Scholar]
- Guang-Wen H, Lin-Yan S, Ying R. Behavior characters of ODD children with ADHD symptoms. Chinese Mental Health Journal. 2005;19:259–261. [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV Subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Loeber R, Stouthamer-Loeber M. Development of juvenile aggression and violence: some common misconceptions and controversies. American Psychologist. 1998;53:242–259. doi: 10.1037//0003-066x.53.2.242. [DOI] [PubMed] [Google Scholar]
- Lorch EP, Sanchez RP, van den Broek P, Milich R, Murphy EL, Lorch RF, Jr., et al. The relation of story structure properties to recall of television stories in young children with attention-deficit hyperactivity disorder and nonreferred peers. Journal of Abnormal Child Psychology. 1999;27:293–309. doi: 10.1023/a:1022658625678. [DOI] [PubMed] [Google Scholar]
- Lynam DR. Early identification of chronic offenders: who is the fledgling psychopath? Psychological Bulletin. 1996;120:209–234. doi: 10.1037/0033-2909.120.2.209. [DOI] [PubMed] [Google Scholar]
- Lynam DR. Pursuing the psychopath: capturing the fledgling psychopath in a nomological net. Journal of Abnormal Psychology. 1997;106:425–438. doi: 10.1037//0021-843x.106.3.425. [DOI] [PubMed] [Google Scholar]
- Martel M, Nigg JT. Control, resiliency, negative emotionality, and ADHD in children. Journal of Child Psychology and Psychiatry. 2006;47:1175–1183. doi: 10.1111/j.1469-7610.2006.01629.x. [DOI] [PubMed] [Google Scholar]
- Mathias CW, Furr RM, Daniel SS, Marsh DM, Shannon EE, Dougherty DM. The relationship of inattentiveness, hyperactivity, and psychopathy among adolescents. Personality and Individual Differences. 2007;43:1333–1343. [Google Scholar]
- Milich R, Balentine AC, Lynam DR. ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clinical Psychology: Research and Practice. 2001;8:463–488. [Google Scholar]
- Miller TW, Nigg JT, Faraone SV. Axis I and II comorbidity in adults with ADHD. Journal of Abnormal Psychology. 2007;116:519–528. doi: 10.1037/0021-843X.116.3.519. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. American Journal of Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychology Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Molina BSG, Smith BH, Pelham WE. Interactive effects of attention deficit hyperactivity disorder and conduct disorder on early adolescent substance use. Psychology of Addictive Behaviors. 1999;13:348–358. [Google Scholar]
- Nigg JT. Neuropsychologic theory and findings in Attention-Deficit/Hyperactivity Disorder: the state of the field and salient challenges for the coming decade. Biological Psychiatry. 2005;57:1424–1435. doi: 10.1016/j.biopsych.2004.11.011. [DOI] [PubMed] [Google Scholar]
- Nigg JT, John OP, Blaskey LG, Huang-Pollock CL, Willicut EG, Hinshaw SP, et al. Big Five dimensions and ADHD symptoms: links between personality traits and clinical symptoms. Journal of Personality and Social Psychology. 2002;83:451–469. doi: 10.1037/0022-3514.83.2.451. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Carr L, Martel M, Henderson JM. Concepts of inhibition and developmental psychopathology. In: Gorfein D, MacCleod C, editors. Inhibition in cognition. American Psychological Association Press; Washington DC: 2007. pp. 259–277. [Google Scholar]
- Nolan EE, Volpe RJ, Gadow KD, Sprafkin J. Developmental, gender, and comorbidity differences in clinically referred children with ADHD. Journal of Emotional and Behavioral Disorders. 1999;7:11–21. [Google Scholar]
- Pasini A, Paloscia C, Alessandrelli R, Porfirio MC, Curatolo P. Attention and executive functions profile in drug naive ADHD subtypes. Brain and Development. 2007;29:400–408. doi: 10.1016/j.braindev.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Pennington BF, Ozonoff S. Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry. 1996;37:51–87. doi: 10.1111/j.1469-7610.1996.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Quay HC. Inhibition and attention deficit hyperactivity disorder. Journal of Abnormal Child Psychology. 1997;25:7–13. doi: 10.1023/a:1025799122529. [DOI] [PubMed] [Google Scholar]
- Vaughn ML, Riccio CA, Hynd GW, Hall J. Diagnosing ADHD (predominantly inattentive and combined type subtypes): discriminant validity of the behavior assessment system for children and the achenbach parent and teacher rating scales. Journal of Clinical Child Psychology. 1997;26:249–357. doi: 10.1207/s15374424jccp2604_3. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin. 2002;128:118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Weller EB, Weller RA, Fristad MA, Rooney MT, Checter J. Children's interview for psychiatric disorders (ChIPS). Journal of the American Academy of Child and Adolescent Psychiatry. 2000;31:76–84. doi: 10.1097/00004583-200001000-00019. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS impulsive behavior scale: a four-factor model of impulsivity. European Journal of Personality. 2005;19:559–574. [Google Scholar]