Abstract
Objective
We sought to synthesize the findings of studies evaluating interventions to improve the cultural competence of health professionals.
Design
This was a systematic literature review and analysis.
Methods
We performed electronic and hand searches from 1980 through June 2003 to identify studies that evaluated interventions designed to improve the cultural competence of health professionals. We abstracted and synthesized data from studies that had both a before- and an after-intervention evaluation or had a control group for comparison and graded the strength of the evidence as excellent, good, fair, or poor using predetermined criteria.
Main Outcome Measures
We sought evidence of the effectiveness and costs of cultural competence training of health professionals.
Results
Thirty-four studies were included in our review. There is excellent evidence that cultural competence training improves the knowledge of health professionals (17 of 19 studies demonstrated a beneficial effect), and good evidence that cultural competence training improves the attitudes and skills of health professionals (21 of 25 studies evaluating attitudes demonstrated a beneficial effect and 14 of 14 studies evaluating skills demonstrated a beneficial effect). There is good evidence that cultural competence training impacts patient satisfaction (3 of 3 studies demonstrated a beneficial effect), poor evidence that cultural competence training impacts patient adherence (although the one study designed to do this demonstrated a beneficial effect), and no studies that have evaluated patient health status outcomes. There is poor evidence to determine the costs of cultural competence training (5 studies included incomplete estimates of costs).
Conclusions
Cultural competence training shows promise as a strategy for improving the knowledge, attitudes, and skills of health professionals. However, evidence that it improves patient adherence to therapy, health outcomes, and equity of services across racial and ethnic groups is lacking. Future research should focus on these outcomes and should determine which teaching methods and content are most effective.
Keywords: race/ethnicity, health disparities, cultural competence
Racial and ethnic disparities in the quality of health care have been extensively documented,1 and it has been suggested that cultural competence on the part of health care providers and organizations may be one mechanism to reduce racial and ethnic disparities in care.2 Cultural competence has been defined as “the ability of individuals to establish effective interpersonal and working relationships that supersede cultural differences”3 by recognizing the importance of social and cultural influences on patients, considering how these factors interact, and devising interventions that take these issues into account.4
In anticipation of the promise of cultural competence training, the Office of Minority Health has put forth standards for cultural competence that include training of health care providers,5 and the Accreditation Council on Graduate Medical Education (ACGME) has required that physicians-in-training demonstrate sensitivity and responsiveness to a patient’s culture as part of its professionalism competency.6 Despite the promise of cultural competency training, there has been little systematic evaluation of its potential impact.
The purpose of this study was to conduct a systematic review of the literature of interventions designed to improve the cultural competence of health care providers. Our specific aims were to determine (1) what strategies have been shown to improve the cultural competence of healthcare providers and (2) what the costs of these strategies are.
METHODS
Study Design
We conducted a systematic review of the literature to address the broad question of which strategies to improve the quality of care for racial/ethnic minorities are effective. We chose to conduct a systematic review rather than a meta-analysis because of the anticipated heterogeneity in the literature. To that end, we used formal methods of literature identification, selection of relevant articles, data abstraction, quality assessment, and synthesis of results to review literature on the effectiveness and costs of cultural competence training for healthcare providers.
In February 2003, we searched (1) MEDLINE®, (2) the Cochrane CENTRAL Register of Controlled Trials (Issue 1, 2003), (3) EMBASE, (4) the specialized register of Effective Practice and Organization of Care Cochrane Review Group (EPOC), (5) the Research and Development Resource Base in Continuing Medical Education (RDRB/CME), and (6) the Cumulative Index of Nursing and Allied Health Literature (CINAHL®). We designed search strategies, specific to each database, to maximize sensitivity. Initially, we developed a core strategy for MEDLINE, accessed via PubMed, based on an analysis of the Medical Subject Headings (MeSH) and text words of key articles identified a priori. The PubMed strategy, which used terms such as “cultural sensitivity,” “transcultural,” “cultural diversity,” and “multicultural” as well as “cultural competency,” formed the basis for the strategies developed for the other electronic databases.7
In addition to electronic searching, we identified priority journals that had provided the most citations in the electronic searching, and we scanned their tables of contents from February 1, 2003, through June 15, 2003. We also scanned the reference lists of key review articles and all articles eligible for our report. The results of the searches were downloaded and imported into ProCite, a reference management software program. This database was used to store citations, track search results and sources, and track the abstract and article review process.
Eligibility Criteria
The following criteria were used to exclude articles from further consideration: published prior to 1980, not in English, did not include human data, contained no original data, a meeting abstract only (no full article for review), not relevant to minority health, no intervention, intervention not targeted to healthcare providers or organizations, no evaluation of the intervention, inconclusive evaluation of the intervention (intervention evaluated only with a post-test), or article did not apply to any of the study questions.
We printed the title and abstract of all citations identified through the literature search, and 2 team members independently reviewed the title and abstract for eligibility. Because reviewer agreement was anticipated to be low (calculated kappa was 0.41 on a random sample of abstracts), we designed our process such that no abstract would be excluded based on the opinion of only one reviewer. When reviewers agreed that a decision regarding eligibility could not be made because of insufficient information, the full article was retrieved for review. When reviewers disagreed on eligibility, citations were returned for adjudication by reviewers until they reached agreement. Reviewers were asked to err on the side of inclusion.
Article Review
We developed standardized review forms to (1) confirm eligibility for full article review, (2) assess study characteristics, and (3) extract the relevant data to address the study questions. The forms were developed through an iterative process that included review of forms used for previous systematic reviews, discussions among team members and experts, and pilot testing.
For each eligible study, we abstracted data regarding the targeted providers and setting, curricular content (using a previously published framework that included general cultural concepts, specific cultural content, language, racism, access issues, doctor-patient interactions, socioeconomic status and gender/sexuality),8 teaching methods, evaluation methods, and outcomes. We classified outcomes as either provider outcomes (knowledge, attitudes/beliefs, or skills/ behaviors) or patient outcomes (satisfaction, adherence, and health status). We also designed several questions to assess methodological strengths and weaknesses of studies, specifically including study design and objectivity of outcome assessment. Objective outcome assessments included written tests and standardized instruments, whereas outcome assessments that were not considered objective included open-ended interviews and learner self-assessment.
We conducted independent and serial reviews of the quality assessment forms from 10 articles to calculate the agreement between reviewers. Each quality assessment form contained 21 questions with 3–4 possible choices. We found a mean kappa (across the 21 items) of 0.81 for the independent review process and 0.87 for the serial review process. These values are similar and in the range that most experts would consider excellent agreement.9 We used a serial review process to conserve time and resources. A primary reviewer completed the quality assessment and data abstraction forms and a second reviewer, after reading the article, checked each item on the form for completeness and accuracy. Differences between primary and secondary reviewers were resolved by adjudication and, when necessary, consultation and consensus with the entire team of reviewers.
Data Synthesis
We created summary tables of evidence from these studies and then examined the relation between various intervention characteristics and outcomes across studies. In particular, we examined the outcomes of interventions according to several features of the interventions that we determined would be of interest to educators and policy makers: intervention length (for those at the extremes of ≤ 1 day and ≥ 1 week), curricular content (those that taught general concepts of culture, those that focused on specific cultures, and those that did both), and curricular method (those that used experiential learning, which was defined as either cultural immersion, clinical experience or interviewing members of another culture, and those that did not use any of those methods).
Evidence Grading
Once all articles were reviewed and data were synthesized, the strength of the evidence supporting each outcome type was graded into 4 categories (grades A through D) based on its quality, quantity, and consistency. We developed the evidence grading scheme based on proposed criteria.10 For quality, we used 2 criteria: study design and the presence of objective assessment. To meet the quality criteria for grade A, there must have been at least one randomized controlled trial and at least 75% of the studies must have used an objective assessment method. To meet grade B, there must have been at least one controlled trial (not necessarily randomized) AND at least 50% of studies must have had objective assessment. To meet grade C or D, there did not need to be any controlled trials and < 50% of studies could have had objective assessment.
For quantity of studies, there had to be at least 4 studies to meet criteria for grade A, 3 studies to meet criteria for grade B, 2 studies to meet criteria for grade C, or at least 1 study to meet criteria for grade D. For consistency, the results of the studies had to be consistent (either beneficial or harmful results in same direction across almost all studies) to meet criteria for grade A, reasonably consistent to meet criteria for grade B (most study results in the same direction), and inconsistent to meet criteria for grade C. If there were too few studies to judge the consistency of results, the strength of evidence supporting the question was given a grade of D. The grading of the evidence was discussed at team meetings (particularly to determine the consistency) and consensus was reached on each criterion. The evidence received a final “grade” that reflected the lowest rank on any of the 4 criteria (2 for quality and 1 each for quantity and consistency).
RESULTS
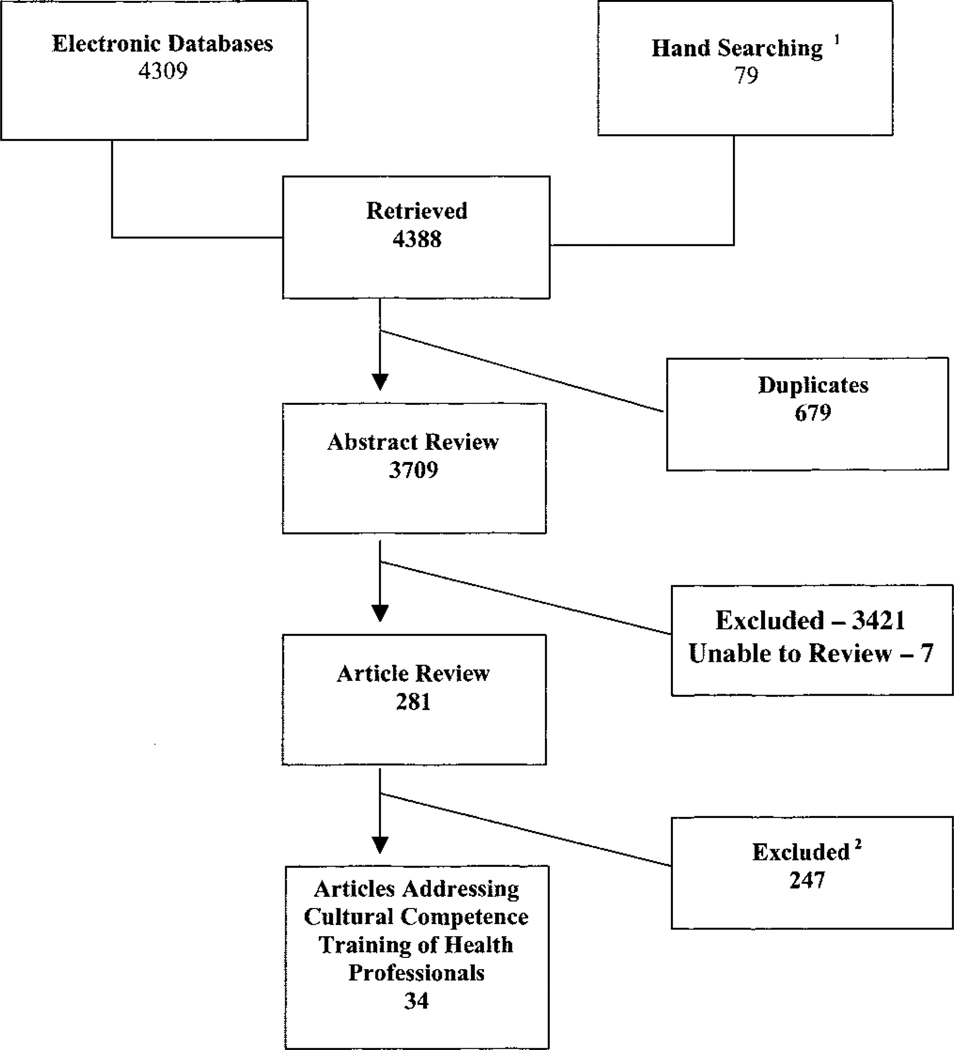
A total of 34 articles met eligibility criteria.11–44 Figure 1 describes the literature review and search process. The eligible articles are summarized in Table 1 and described in detail in Table 2. Studies on cultural competence training are increasing in frequency. Most have used a pre/post evaluation design, have occurred in the United States, and have targeted physicians and/or nurses. A variety of curricular methods and content has been evaluated, although no 2 studies have evaluated exactly the same curriculum.
FIGURE 1.
Summary of literature search and review process (number of articles). 1From reference lists of eligible and key articles as well as tables of contents of the following journals: Academic Medicine Archives of Pediatric and Adolescent Medicine Ethnicity and Disease Health Services Research Journal of the American Medical Association Journal of General Internal Medicine Journal of Health Care for the Poor and Underserved Journal of Transcultural Nursing Medical Care Milbank Quarterly New England Journal of Medicine, and Pediatrics. 2The most common reasons for exclusion at the full article review level were that the article lacked evaluation of the described intervention, the article was not relevant to minority health, or the article was not targeted to health care provider or organization. Thirty articles were excluded because the intervention was only evaluated with a postintervention evaluation.
TABLE 1.
Summary of 34 Studies Evaluating Interventions to Improve Cultural Competence Training of Health Professionals
| n | |
|---|---|
| Dates | |
| 1980–89 | 4 |
| 1990–99 | 15 |
| > 2000 | 15 |
| Study design | |
| RCT | 2 |
| Controlled | 12 |
| Pre/Post | 20 |
| Setting | |
| US | 29 |
| Non-US | 5 |
| Targeted learners* | |
| Physicians | 18 |
| Nurses | 17 |
| Learner level | |
| Preprofessional | 22 |
| Practicing professional | 11 |
| Curricular content* | |
| Specific cultures | 26 |
| General concepts | 19 |
| Language | 10 |
| Dr-pt interaction | 8 |
| Access | 3 |
| Racism | 2 |
| SES | 2 |
| Curricular methods* | |
| Lectures | 17 |
| Discussion (group) | 17 |
| Case scenarios | 12 |
| Clinical experience | 10 |
| Small group | 9 |
| Cultural immersion | 8 |
| Audio/visual | 7 |
| Interviewing other cultures | 7 |
| Role play | 5 |
| Targeted cultures (if specified)* | |
| African American | 10 |
| American Indian | 0 |
| Asian/Pacific Islander | 10 |
| Latino | 9 |
| Contact time (if specified) | |
| Less than 8 hours | 11 |
| Between 1–5 days | 5 |
| Greater than 1 week | 9 |
| Outcome type* | |
| Provider knowledge | 19 |
| Provider attitude | 25 |
| Provider skills/behaviors | 14 |
| Patient satisfaction | 3 |
| Outcome assessment | |
| Objective | 26 |
| Not objective | 8 |
Responses not mutually exclusive.
TABLE 2.
Description of 34 Studies Evaluating Interventions to Improve Cultural Competence Training of Health Professionals
| Author, Year | Study Design |
Training Level |
Curricular Content |
Specific Culture | Contact Time | Curricular Methods |
|---|---|---|---|---|---|---|
| Studies on physicians | ||||||
| Mao, 1988 | Pre/post | Pre-prof | GC, D-P, SC, |
NS | One 4-hour session held once only |
Audio/visual, discussion (group) |
| Copeman, 1989 | Pre/post | Pre-prof | R, D-P, L, SC |
Aboriginal | NS | Case scenarios, clinical experiences, discussion (group), interviewing members of another culture |
| Rubenstein, 1992 | Pre/post | Pre-prof | GC, SC | A/PI | One 4-hour session held once only |
Case scenarios, discussion (group), interviewing members of another culture, lectures |
| Nora, 1994 | pre/post (external control) |
Pre-prof | L, SC, A | H | Thirty 2-hour sessions plus 8 days full time |
Clinical experiences, culture immersion, demonstration/role modeling, discussion (group), language lessons, lectures, food shopping/planning, hospital tours, cultural and history learning |
| Culhane-Pera, 1997 | Pre/post | R/F | GC, D-P, L, SC |
H | Three 1-day sessions |
Audio/visual, clinical experiences, discussion (group), drill/practice exercise, lectures |
| Farnill, 1997 | Pre/post | Pre-prof | L | Non-English-speaking persons |
Sixteen < 2- hour sessions held over 7 months |
Discussion (group), interviewing members of another culture |
| Haq, 2000 | Pre/post | Pre-prof, R/F |
GC, SC | A/PI, AA, H | 8–10 weeks full time |
Brainstorming, case scenarios, clinical experiences, culture immersion, discussion (group), drill/practice exercise, lectures, conduction of community health activities |
| Dogra, 2001 | Pre/post | Pre-prof | GC | NS | Two 2-hour sessions in 1 week |
Brainstorming, case scenarios, drill/practice exercise, lectures |
| Godkin, 2001 | CCT | Pre-prof | GC, L, SC, SES |
A/PI, H | Thirty half-day sessions over 1 year plus 6 weeks full-time |
Culture immersion, interviewing members of another culture, language lessons, lectures, community service |
| Mazor, 2002 | Pre/post | R/F, prof | L, SC | H | 2-hour sessions held weekly for 10 weeks |
Case scenarios, language lessons |
| Tang, 2002 | Pre/post | Pre-prof | NS | NS | Sessions held over 4 years |
Case scenarios, lectures |
| Beagan, 2003 | Post only (external control) |
Pre-prof | L, SC | NS | One afternoon each week held over 2 years |
Clinical experiences, lectures |
| Crandall, 2003 | Pre/post | Pre-prof | GC, R, SC, SES |
NS | Twenty 2–3 hour sessions held over 1 year |
Audio/visual, case scenarios, demonstration/role modeling, interviewing members of another culture, lectures |
| Godkin, 2003 | CCT | Pre-prof | GC, SC | A/PI, AA, H | NS | Culture immersion |
| Studies on nurses | ||||||
| Frank-Stromborg, 1987 |
Pre/post | Prof | SC | AA | One day session held once only |
Demonstration/role modeling, discussion (group), lectures |
| Frisch, 1990 | CCT | Pre-prof | GC, SC | H | Six weeks full- time |
Culture immersion |
| Alpers, 1996 | CCT | Pre-prof | GC, SC | A/PI, AA, H | NS | Home visits |
| Williamson, 1996 | Pre/post | Pre-prof | GC | NS | Sessions held weekly |
Audio/visual, clinical experiences, culture immersion, discussion (group), interviewing members of another culture |
| Flavin, 1997 | Pre/post | Prof | D-P, SC | A/PI | < 2-hour sessions held weekly for 3 weeks |
Audio/visual, case scenarios, discussion (group) |
| St Clair, 1999 | CCT | Pre-prof | GC, D-P | AA | 2–3 weeks full time |
Culture immersion |
| Underwood, 1999 | Pre/post | Prof | SC | AA | NS | Case scenarios, demonstration/role modeling, lectures, outreach with national prevention organization |
| Jeffreys, 1999 | Pre/post | Pre-prof | GC, SC | NS | NS | Clinical experiences, discussion (group), lectures, written assignments |
| Napholz, 1999 | CCT | Pre-prof | GC, L, SC | AA | Three 2-hour sessions |
Clinical experiences |
| Inglis, 2000 | Pre/post (external control) |
Pre-prof | D-P, SC | A/PI | Three weeks full time |
Lectures, visits to local hospitals and health centers, field trip |
| Lasch, 2000 | RCT | Prof | SC | NS | One 1-day sessions held once only |
Clinical experiences, discussion (group), lectures |
| Scisney-Matlock, 2000 |
CCT | Pre-prof | GC | NS | NS | Lectures, web pages, written and verbal presentations |
| Smith, 2001 | CCT | Prof | GC, SC | NS | One session held once only |
Case scenarios, demonstration/role modeling, lectures, simulations |
|
Studies on mixed groups of healthcare providers |
||||||
| Erkel, 1995 | Pre/post | Pre-prof | SC | AA | 5 weeks full time |
Audio/visual, case scenarios, clinical experiences, culture immersion |
| Gany, 1996 | Pre/post | Prof | L, SC | A/PI, AA, H | Four sessions | Discussion (group), personal experiences |
| Gallagher Thompson, 2000 |
Pre/post | Prof | D-P, SC, A | H | One session held once only |
Audio/visual, discussion (group), lectures |
| Way, 2002 | Pre/post | Prof | GC | NS | One sessions held once only |
NS |
|
Studies on other types of healthcare providers |
||||||
| Stumphauzer, 1983 | Pre/post | Prof | GC, A | A/PI | Two hour sessions held weekly for 10 weeks |
Case scenarios, discussion (group) |
| Wade, 1991 | RCT | Prof | SC | AA | Four hours total |
Discussion (group) |
| Hansen, 2002 | Post only (external control) |
Pre-prof | GC, D-P, L, SC |
NS | Two 1-day sessions |
Discussion (group), writing cultural autobiography |
Pre-prof indicates pre-professional (student); Prof, professional; R/F, resident/fellow; L, language; SC, specific cultural content; GC, general concepts of culture; R, racism; D-P, doctor–patient interactions; G, gender; A, access; SES, socioeconomic status; NS, not specified; AA, African American; A/PI, Asian/Pacific Islander; H, Hispanic.
Effect of Cultural Competence Training on Health Care Providers
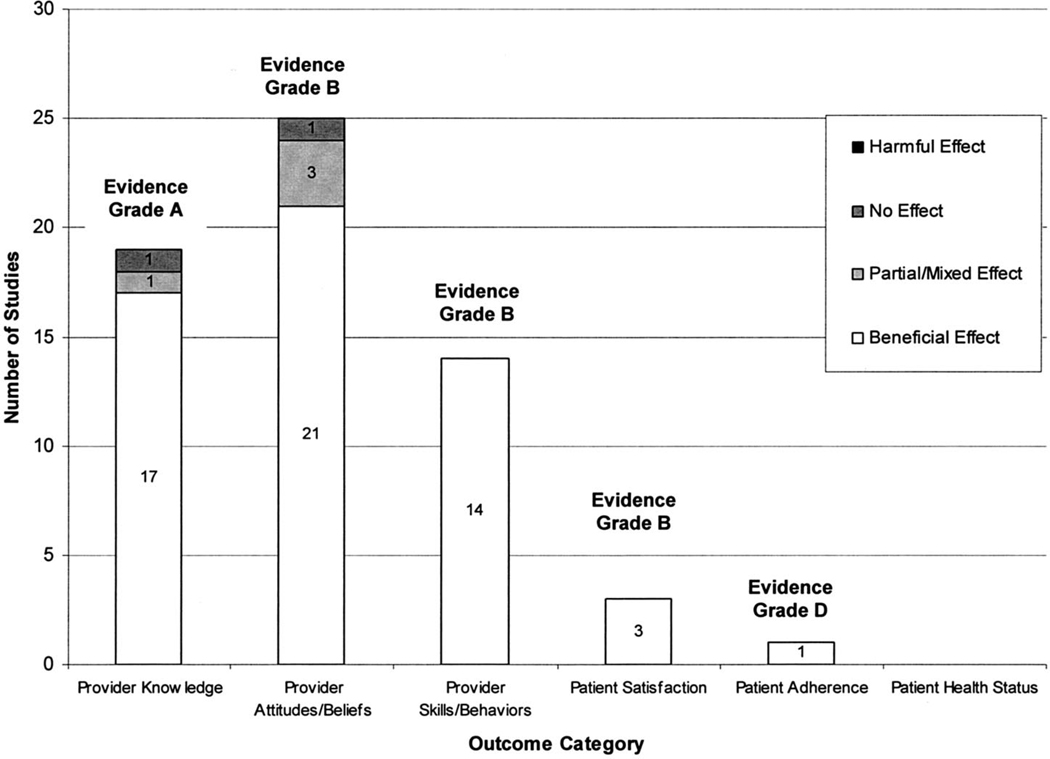
Figure 2 shows the number of studies showing beneficial, partial/mixed, harmful, or no effects by type of outcome. A summary of outcomes of these studies is provided in Table 3 and detailed in Appendix A.
FIGURE 2.
Number of studies showing beneficial, partial/mixed, harmful, or no effect reported by outcome.
TABLE 3.
Summary of Results of 34 Studies Evaluating Interventions to Improve Cultural Competence Training of Health Professionals*
| Provider Outcomes |
Patient Outcomes |
||||||
|---|---|---|---|---|---|---|---|
| Evaluation Methods |
Knowledge | Attitudes | Skills | Satisfaction | Patient Adherence |
Health Status |
|
| Physicians | |||||||
| Mao, 1988 | Ratings, self | + | + + | ||||
| Copeman, 1989 | Self, exam | ? | +/? | ||||
| Rubenstein, 1992 | Ratings, exam | + +/+ + | |||||
| Nora, 1994 | Interview, ratings, exam |
++ | + | + | |||
| Culhane-Pera, 1997 | Interview, observer, ratings, self |
++ | +/+ | + +/+ + | |||
| Farnill, 1997 | Patient, self, video/ audiotape |
+ +/+ + | |||||
| Haq, 2000 | Essays, ratings, self, open-ended questions |
+ +/+ | + + | ||||
| Dogra, 2001 | Self, exam | 0/? | |||||
| Godkin, 2001 | Self, exam | ++ | ++ | ||||
| Mazor, 2002 | Performance audits, patient, self |
+ | + +/? | + +/++/++/++ | |||
| Tang, 2002 | Self | + +/++/+ + | |||||
| Beagan, 2003 | Interviews, questionnaires |
0/0/0 | |||||
| Crandall, 2003 | Exam; MAQ | ++ | ++ | ++ | |||
| Godkin, 2003 | Self | + +/?/+ + | |||||
| Nurses | |||||||
| Frank-Stromborg, 1987 | CAI, PAS, activities survey |
+ +/+ + | |||||
| Frisch, 1990 | Exam, MER | + +/0/ + | |||||
| Alpers, 1996 | Self, CSES | +/− | |||||
| Williamson, 1996 | Interview, self, exam, CSES |
++ | ++ | ++ | |||
| Flavin, 1997 | Essays, ratings, exam | 0 | |||||
| Jeffreys, 1999 | Self, TCSET | ++ | ++ | ++ | |||
| Napholz, 1999 | Self, exam, ECSA | + | |||||
| St. Clair, 1999 | Essays, self, journal, field notes, CSES |
+ +/++/ + | |||||
| Underwood, 1999 | Ratings, self | + | +/+ | + | |||
| Inglis, 2000 | Exam | ++ | |||||
| Lasch, 2000 | Exam | ++ | ++ | ||||
| Scisney-Matlock, 2000 | Self, MLSS | + +/+ + | |||||
| Smith, 2001 | Self, exam, CSES | ++ | ++ | ||||
|
Mixed healthcare provider groups |
|||||||
| Erkel, 1995 | Ratings, self | + | +/+/+ | ||||
| Gany, 1996 | Exam | ++ | ++ | ||||
| Gallagher Thompson, 2000 |
Self, exam | + +/+ + | ++ | ||||
| Way, 2002 | Ratings, patient, self | + | +/+ + | ++ | |||
|
Other healthcare providers |
|||||||
| Strumphauzer, 1983 | Observer, ratings, exam |
++ | ++ | ||||
| Wade, 1991 | Patient, B/L RI, CES, CRF |
++ | ++ | ||||
| Hansen, 2002 | exam | + + | |||||
If cell is left blank, then outcome type is not measured for that study. Outcomes separated by “/” indicate more than one outcome in that category.
Self indicates self-assessment forms; Exam indicates written exams; Interview, individual or group interviews; Observer, observer questionnaire; Ratings, participant ratings of curriculum; Essays indicates essays; Patient, patient rating.
Specific evaluation tools: MAQ indicates Multicultural Assessment Questionnaire; CSES, Bernal and Froman Cultural Self-Efficacy Scale; CAI, Cancer Attitude Inventory; PAS, Pittsburgh Attitude Survey; MER, Measure of Epistemological Reflection; TCSET, Transcultural Self-Efficacy Tool; ECSA, Ethnic Competency Skills Assessment; MLSS, Michigan Longitudinal Study Scales; B/L RI, Barrett-Lennard Relationship Inventory; CES, Counselor Effectiveness Scale; CRF, Counselor Rating Form. “++” indicates significant beneficial effect; “+”, beneficial effect; “−,” harmful effect; “?,” partial/mixed or unclear effect; “0”, no effect.
Appendix.
Detailed Results of 34 Studies Evaluating Cultural Competence Training of Health Professionals
| Study | Outcomes |
|---|---|
| PHYSICIAN | |
| Beagan, 2003 | There were no differences in the percent of students who thought various characteristics of patients (for example appearance, English ability, social class, race, gender, culture) affected their treatments. |
| There were no differences in the percent of students who thought physicians’ social and cultural characteristics affected their medical practice. |
|
| There were no differences in the percent of students who thought their own social and cultural factors affected their medical school experience. |
|
| Copeman, 1989 | A 2-item test of knowledge showed significant improvement on one item measuring knowledge of cardiovascular disease but no improvement on the item measuring mental illness among Aboriginals. |
| After the intervention, only 20% felt “quite competent” to interview a non-English speaking patient through an interpreter and 76% thought they could “probably manage”. |
|
| After the curriculum, medical students were less likely to agree, 1) that migrants take away jobs from other Australians (P < 0.01) and 2) that restrictions should be placed on the Aboriginal to protect him from his own lack of responsibility (P < 0.05) and medical students were significantly more likely to agree 1) that the cause of Aboriginal poor health is disposition from their land (P < 0.01) and 2) that in general Aborigines are pretty much all alike (P < 0.05). |
|
| Crandall, 2003 | Statistically significant improvement of the 4 items of the skills sub-scale occurred after the course (P= 0.000). |
| Statistically significant improvement on the 6 items of the knowledge sub-scale occurred after the course (P= 0.000). |
|
| Statistically significant improvement of the 6 items of the attitudes sub-scale occurred after the course (P= 0.000). |
|
| Culhane-Pera, 1997 | Average scores on a 4-item attitudinal self-assessment improved from 3.93 to 4.1, though this change was not statistically significant. |
| Average scores on a 6-item self-assessment of skills (related to incorporating cultural issues into clinical care) improved from 3.33 to 3.96 (P = 0.000). |
|
| Residents self-assessments of their level of cultural competence significantly increased between initial and final evaluations. |
|
| Although faculty’s initial assessment of resident’s level of cultural competence did not correlate well with resident’s own assessment r = 0.092), final competence level assessment did r = 0.507, P < 0.05). |
|
| Average scores on a 6-item knowledge self-assessment of general cultural issues improved from 2.87 to 3.47 (P = 0.000). |
|
| Participants ranked the entire curriculum of 4.33/5 for importance and 4.26/5 for quality. | |
| Dogra, 2001 | There was no statistical difference in responses to case scenarios before and following training. |
| After the intervention, students had significantly different responses on 8 out of 25 attitudinal items about cultural issues (P < 0.05). |
|
| Farnill, 1997 | Students reported significantly more competence on all self-assessment dimensions (P < 0.001) related to interviewing patients of non-English speaking patients. |
| Community volunteers reported positive experiences being interviewed by the students. | |
| Blinded psychologist rating of video showed students to be significantly more competent in interviewing a non-English-speaking patient in the postintervention video over preintervention video (P < 0.01). |
|
| Godkin, 2001 | Students in the intervention group showed significant improvements in self-assessed knowledge of cultural beliefs, practices, and health needs on 8 out of 9 items. |
| Students in the intervention group showed significant improvements on 7 out of 20 cultural competence items, and had significantly better cultural competence attitudes than students who did not participate in the intervention. |
|
| Godkin, 2003 | Compared to students who did not elect to travel internationally, students who traveled were significantly more interested in an international component in career, interested in working with underserved, recognizing need to know another language and recognizing need to know a patient’s financial constraints. |
| After traveling to another country, preclinical medical students were more likely (than before they had traveled) to report (on a scale from 1 to 5) that they had an interest in an international component to their career (4.37 compared to 4.06, P < 0.001), that they had an interest in an international component to their career (3.97 compared to 3.67, P < 0.01), that there is a need to understand cultural differences (4.43 compared to 4.16, P < 0.01), that there is a need to know another language (4.51 compared to 4.15, P < 0.001), and that there was need to be an advocate for the whole community (4.14 compared to 3.91, P = 0.03). |
|
| After traveling to another country, medical students in their clinical years were more likely (than before they had traveled) to report (on a scale from 1 to 5) that there was a need to understand cultural differences (4.51 compared to 4.23, P < 0.001), that they were enthusiastic about being a physician (4.17 compared to 3.86, P = 0.03), and that they had a sense of idealism in the role of physician (3.65 compared to 3.16, P < 0.001), but were less likely to report a need to work collaboratively with other professionals (3.93 compared to 4.19, P = 0.02) and that they had awareness of their future role as physicians (4.14 compared to 4.35, P = 0.04). |
|
| Haq, 2000 | 96% would recommend international health experiences to other students. |
| Participants experienced significant positive changes in attitude towards communication and community health issues (P < 0.03) between the pre- and post-test. |
|
| 83% of participants said the experiences changed how they would practice medicine. | |
| Participants gained significant positive improvements on each of 10 self-assessed clinical skills between the pre- and post-test (P = 0.001). |
|
| Mao, 1988 | In 1986, 94% approved the use of student discussion leaders, 85% enjoyed the videotapes, and 49% found the role playing exercises helpful. |
| In 1986 and 1987, 70% of students found that the workshop achieved its objectives and 10% wanted more specific cultural information. |
|
| In 1986 and 1987 a few students commented that the workshop should explore racial and gender issues in more depth. |
|
| 1985 showed some “significant” improvement in making treatment choices in 3 case studies (paired t-tests). | |
| There was significant improvement on 3 of 9 attitudes measured. | |
| Mazor, 2002 | Families in the postintervention period were more likely to strongly agree that “the physician was concerned about my child” (OR 2.1, [CI 1.0–4.2]) than families in the preintervention period. |
| Families in the postintervention period were more likely to strongly agree that “the physician listened to what I said” (OR 2.9, [CI 1.4–5.9]) than families in the preintervention period. |
|
| Families in the postintervention were more likely to strongly agree that “the physician made me feel comfortable” (OR 2.6, [CI 1.1–4.4]) than families in the preintervention period. |
|
| Physicians used a professional interpreter less often in the postintervention period (55% versus 29%, odds ratio 0.34, [CI 0.16–0.71]). |
|
| Physicians scored higher on measures of data gathering without the use of an interpreter (17.2 pre-test versus 22.4 post-test, P = 0.01). |
|
| All but one of the physicians in the postintervention period expressed increased confidence in addressing various emergency department chief complaints in Spanish. |
|
| Families in the postintervention period were more likely to strongly agree that “the physician was respectful” (OR 3.0, [CI 1.4–6.5]) than families in the preintervention period. |
|
| Nora, 1994 | Spanish language proficiency went from 60% pre-test to 75% post-test. |
| Using the misanthropy scale (which indicates openness to those not like oneself), there were no significant differences between intervention and control post course but there was a trend towards increased acceptance of others in the intervention group. |
|
| Students reported liking the opportunity to meet Mexicans and traditional healers. | |
| Students were positive about their experience in Mexico; one reported that it exceeded their expectations. In comments 6 months later, 4 of the 8 students who went to Mexico described the experience as life- changing. |
|
| Cultural knowledge of Hispanic health in the intervention group went from 40% precourse to 58% postcourse versus the control group 46% pre and 42% post (P = 0.007). |
|
| Rubenstein, 1992 | Participants developed increased knowledge of ways physicians ignorance of patient’s health beliefs can adversely affect clinical encounter (on Likert scale out of 5 points: pre-test 3.3, post-test 4.6 (P < 0.0001)). |
| The curriculum scored a mean rating of 3.5 (0 = lowest; 4 = highest) in usefulness. | |
| Participants developed increased knowledge about available resources to learn about non-conventional health beliefs (pre-test 3.8, post-test 4.9 (P < 0.0001)). |
|
| Tang, 2002 | After the intervention, the students reported increased understanding of the importance of incorporating sociocultural factors into patient care (P < 0.01). |
| After the intervention, the students reported significantly increased understanding of the impact of sociocultural issues on the patient-physician relationship and on patients’ health (P < 0.001). |
|
| After the intervention, the students reported significantly greater understanding of the relationship among sociocultural issues, health, and medicine (P < 0.001). |
|
| NURSE | |
| Alpers, 1996 | Intervention group has a greater confidence/competence in providing care to African American and Hispanic clients. |
| Control group felt more confidence/competence in entering ethnically distinct community, and understanding Asian folk health practices than did the group who had received class content on culturalism. |
|
| Flavin, 1997 | The curriculum received good scores for design, relevancy of information, and meeting participant expectations. |
| There were no significant changes in “learning scores” regarding knowledge of practices and values of 4 targeted cultures prior to and after the curriculum. |
|
| Frank-Stromborg, 1987 | Activities survey reported increased community activities in cancer prevention and early detection. |
| Scores on the Pittsburgh Attitude Survey (PAS) self report measuring cancer attitudes improved from the pre- test (mean = 81) to the post-test (mean = 82, P < 0.08). |
|
| 94% rated simulated practice with models as excellent to above average, 98% rated the speakers as excellent to above average, and 78% rated the program as excellent. |
|
| Scores on the Cancer Attitude Inventory (CAI) improved from pre-test (mean = 132) to the post-test (mean = 139, P < 0.001). |
|
| Frisch, 1990 | 5 out of 9 students that increased their scores on the Measure of Epistemological Reflection (MER) went on exchange to Mexico. |
| Seventy-one percent of the measured cognitive improvement seen in the senior class can be attributed to the Mexico program (P = 0.018). |
|
| The Mexico exchange students were 3.5 times as likely to improve show cognitive improvement as measured by the Measure of Epistemological Reflection (MER) than were students that did not participate. |
|
| Inglis, 2000 | Students who participated in the intervention showed significant shifts on 8 out of 23 attitudinal items towards more understanding of cross-cultural issues, whereas students in the control group showed no change on any items |
| Jeffreys, 1999 | Practical (interviewing) subscale score on the Transcultural Self-Efficacy Tool increased between pre- and post-test from 16 to 55% (P < 0.001). |
| Affective subscale scores on the Transcultural Self-Efficacy Tool increased between pre- and post-test from 16 to 43% (P < 0.001). |
|
| Cognitive subscale scores on the Transcultural Self-Efficacy Tool increased between pre- and post-test from 2 to 28% (P < 0.001). |
|
| Lasch, 2000 | Nurses participating in both intervention programs (workshop only and enriched model) significantly changed pain management attitudes (P = 0.01), and maintained this change at 1 year follow-up, whereas the control group had no change. |
| Both intervention groups (workshop only and enriched model) significantly improved knowledge of cancer pain management over control group at post-test and follow-up (P < 0.0001). |
|
| Napholz, 1999 | Both groups significantly increased scores Ethnic Competency Skills Assessment (ECSA); however, the experimental group increased much higher than the control group. |
| Scisney-Matlock, 2000 | Knowledge of diversity gained through course work was not statistically significant different between experimental group and control group. |
| Intervention group showed statistically significant increase in activities devoted to understanding other racial/ ethnic groups. |
|
| Intervention group showed statistically significant increase in self-reported social interactions with peers of different race/ethnicities. |
|
| Intervention group showed statistically significant increase in satisfaction with relevance of course work to their own ethnicity. |
|
| Smith, 2001 | Questionnaire measuring knowledge of cultural diversity taken in 3 phases showed significant increases over time (P < 0.001) in the intervention group and no improvement in the control group. |
| Cultural self-efficacy scale (CSES) taken in the 3 phases, showed significant improvements in self-efficacy (P < 0.001) in the intervention group and no improvement in the control group. |
|
| St Clair, 1999 | Continual growth in cultural self-efficacy scores for students in international clinical exercises (mean score 3.7) over those who remained in the US (mean score 3.3) in the follow-up testing period (P = 0.007). |
| There was a statistically significant increase in cultural self-efficacy scores on the post-test in all students. | |
| Students developed sensitivity to being a minority through international experience. | |
| Underwood, 1999 | Since completing the program, many participants have designed and implemented a number of innovative cancer prevention programs. |
| Participants indicated more confidence in their ability to positively influence cancer prevention behaviors in practice and community. |
|
| Participants indicated that the curriculum changed their attitudes towards nurses role in cancer prevention and early detection. |
|
| Participants indicated increased knowledge of cancer prevention and early detection among African Americans. | |
| Williamson, 1996 | Attitudes about cultural patterns. Showed sustained improvements in African Americans [begin 2.77 (0.66), middle 3.31 (0.72), end 3.61 (0.65)], Hispanics [begin 2.58 (0.70), middle 3.31 (0.70), end 3.69 (0.71)], and SE Asians [begin 2.28 (0.69), middle 3.64 (0.69), end 3.35 (0.77)] (P < 0.001). |
| Students improved in transcultural skills (begin 3.29 (SD ± 0.69), middle 3.64 (SD ± 0.69), end 3.96 (SD ± 0.66) (P < 0.001)). |
|
| Participants improved their knowledge of cultural concepts (beginning 2.92 (± 0.74), middle 3.49 (± 0.70), end 3.68 (± 0.66) (P < 0.001)). |
|
| OTHER PROVIDERS/MIXED GROUPS | |
| Gallagher Thompson, 2000 | Statistically significant increased referrals of Hispanic Alzheimer patients and/or families to the appropriate specialized services about Alzheimer disease (P < 0.005). |
| Statistically significant increase in participants knowledge of Hispanic beliefs about Alzheimer disease (P < 0.05). | |
| Statistically significant increase in participants general knowledge about Alzheimer disease (P < 0.005). | |
| Gany, 1996 | There was a significant attitude shift on 12-item exam in which the mean score was 33.76 on the pre-test compared to 35.68 on the post-test (P < 0.003). |
| There was a significant knowledge shift on 21 item scale exam about immigrant health in which students scored 15.8% correct in the preintervention period compared to 18.6% correct in the postintervention period (P < 0.0001). |
|
| Erkel, 1995 | Interdisciplinary team interaction, exposure to new practice opportunities, and the community-oriented primary care project were the elements of the course that were most enjoyed by students. |
| Participants gained an increased awareness to barriers to care for rural clients. | |
| Participants gained increased knowledge of rural, transcultural, and interdisciplinary issues; principles of case- management, patient focused care, and community oriented primary care. |
|
| Course evaluations revealed that classroom and field trips met student expectations. | |
| 72% of students reported that the practicum influenced them to consider practicing in a rural setting. | |
| Participants gained an appreciation for rural lifestyle. | |
| Hansen, 2002 | Those who completed the program scored 88.3% on knowledge test, those who did not take the program (control) scored 75.3% (P < 0.001). |
| Stumphauzer, 1983 | Trainees ability to do behavioral analysis and treatment plan increased significantly (P < 0.01) from the preintervention period to the postintervention period. |
| The course was seen by all trainees as having added “a greater deal” or “a considerable amount” to their knowledge base. |
|
| There were significant increases on a 23-item test measuring knowledge of behavioral modification principles, from 38% correct on pre-test to 68% correct on post-test (P < 0.01). |
|
| Wade, 1991 | Brief culture sensitivity training produced significant differences in client perceptions of counselors and the counseling process and was more important than racial pairing. |
| Clients assigned to counselors in culture sensitivity training returned for more follow-ups (mean 2.88 versus 1.90). |
|
| Way, 2002 | After the intervention there was an increased perception among patients of seeing staff members of their ethnicity (P = 0.04) and of finding magazines/reading materials on ward that contained information of interest (P = 0.04). There was also a significant increase in patients’ reporting that staff would see them as individuals (P = 0.06). |
| There was a statistically significant increase in participants’ perception that there were pictures on walls that may remind patients of family/friends (P = 0.01), and that there were magazine/reading materials that contain information in which the patient may be interested (P = 0.0001). |
|
| 58% of participants increased interest in learning patient and family background, and 59% of participants increased sensitivity to cultural competence. |
|
| 59% of participants increased awareness of special needs of recipients who do not speak English. | |
Provider Knowledge
Most studies (17/19) demonstrated a beneficial effect on provider knowledge. Eleven of these studies tested the provider’s knowledge about general cultural concepts (such as the impact of culture on the patient–provider encounter21 or the ways in which provider ignorance can adversely impact patients13) whereas 7 evaluated culture-specific knowledge (such as knowledge of disease burdens across particular populations12,14 and traditional cultural practices24,29). One article did not specify. There was no obvious pattern regarding which type of knowledge was impacted more by cultural competence training. Overall, there is excellent evidence to suggest that cultural competence training impacts the knowledge of healthcare providers (evidence grade A).
Provider Attitudes
Of the 25 studies that evaluated the effect of cultural competence training on provider attitudes, 21 demonstrated a beneficial effect, whereas 1 study showed no effect, and 3 studies showed a partial/mixed effect. The most common attitude outcome measured was cultural self-efficacy measured using the Bernal and Freeman cultural self-efficacy scale,27,28,37 which evaluates learner confidence in knowledge and skills related to African American, Asian, Latino, and Native-American patients. Other studies measured attitudes toward community health issues17 and interest in learning about patient and family backgrounds.40 Overall, there is good evidence to suggest that cultural competence training impacts the attitudes of healthcare providers (evidence grade B). Although the quantity of evidence was sufficient and the results were consistent, the quality of the body of literature did not meet criteria for evidence grade A because less than 75% of studies used an objective assessment of learner attitudes.
Provider Skills
Of the 14 studies that evaluated the effect of cultural competence training on the provider skills, all demonstrated a beneficial effect. For example, in one study, participants were given 16 1-hour sessions in which they practiced communication skills with community volunteers and were subsequently shown to be significantly more competent in interviewing a non-English-speaking person as rated in videos by a blinded psychologist.16 Other behaviors that were observed included an increase in nurses’ involvement in community-based cancer education programs,32 an increase in learners’ self-reported social interactions with peers of different races/ethnicity,36 and an improvement in the learners’ ability to conduct a behavioral analysis and treatment plan.41 Overall, there is good evidence to suggest that cultural competence training impacts the skills/behaviors of healthcare providers (evidence grade B). Although the quantity of evidence was sufficient and the results were consistent, the quality of the body of literature did not meet criteria for evidence grade A because there was no randomized controlled trial and fewer than 75% of studies used an objective outcome assessment.
Effect of Cultural Competence Training on Patient Outcomes
Only 3 studies evaluated patient outcomes: 1 targeting physicians,20 1 targeting mental health counselors,44 and 1 targeting a mixed group of providers.40 All 3 studies reported favorable patient satisfaction measures,20,40,44 and 1 demonstrated an improvement in adherence to follow-up among patients assigned to intervention group providers.44
With regard to the methods used to bring about such improvements in patient outcomes, 1 study trained 4 mental health counselors about the attitudes that low-income African American women bring to counseling (4 hours)44 and found that, in comparison with the control group, counselors were rated more highly in the domains of expertness, trustworthiness, empathy and unconditional regard. Another study trained 9 physicians to speak the Spanish language (20 hours)20 and found, after the intervention, that patients were more likely to agree that the physician was concerned, respectful, and listened. A third study implemented a state-mandated 3-day training program focused on team training, recipient recovery principles, clinical issues and cultural competence for all staff who have contact with recipients of inpatient mental healthcare40 and found that, after the intervention, there were improvements in patients’ sense that the staff would see them as individuals. Overall, there is good evidence that cultural competence training impacts patient satisfaction (evidence grade B) and poor evidence that cultural competence training impacts patient adherence or health outcomes (evidence grade D).
Outcomes Associated with Specific Features of Cultural Competence Training
Outcomes associated with specific features of the interventions are presented in Table 4. Both shorter- and longer-duration interventions appear effective, as do both methods using experiential learning and those not using experiential learning. Interventions teaching general cultural concepts, those teaching about specific cultures, and those that teach both are all associated with positive outcomes.
TABLE 4.
Outcomes Associated With Particular Features of the Interventions
| Outcome |
|||||
|---|---|---|---|---|---|
| Intervention Feature | Provider Knowledge |
Provider Attitudes |
Provider Skills |
Patient Satisfaction |
Patient Adherence |
| Length | |||||
| ≤ 8 hours | 5 beneficial, 1 no effect |
6 beneficial, 1 mixed effect |
3 beneficial | 2 beneficial | 1 beneficial |
| > 1 week | 5 beneficial | 7 beneficial, 1 no effect |
3 beneficial | ||
| Content | |||||
| General concepts | 3 beneficial | 3 beneficial, 1 mixed effect |
3 beneficial | 1 beneficial | |
| Specific cultures | 6 beneficial, 1 no effect |
8 beneficial, 1 mixed effect 1 no effect |
5 beneficial | 2 beneficial | |
| General and specific | 8 beneficial | 10 beneficial | 5 beneficial | ||
| Method | |||||
| Experiential* | 10 beneficial, 1 mixed effect |
12 beneficial, 2 mixed effect, 1 no effect |
7 beneficial | ||
| Not Experiential | 7 beneficial, 1 no effect |
9 beneficial, 1 mixed effect |
7 beneficial | 3 beneficial | 1 beneficial |
Either clinical experiences, cultural immersion, or interviewing members of another culture.
Costs of Cultural Competence Training
Of the 34 articles, there were only 4 articles that addressed the costs of cultural competence training.14,17,19,20 Three of the 4 articles14,17,19 described the costs of interventions that involved international travel. Two programs provided US$2000 (in 200019 and in 1995–199617) for each student to travel from the United States to South America, Asia, or Africa for either 619 or 817 weeks. In each of these programs, the students provided the remaining costs. Another program estimated that an 8-day trip from the United States to Mexico cost US$1200 total in 1994, of which the students contributed 60% on average, and scholarship assistance for the remainder was available through private donations.14
There are limited data regarding the costs of classroom instruction or other types of instruction. One study estimated the cost of 20 total hours of Spanish language instruction for 9 physicians to be US$2000 in 2000, not including the opportunity costs for physician time (approximately 20 hours total for each physician).20 In another program, there were also 60 hours of classroom instruction (20 hours of Spanish language instruction and 40 hours of cultural competence training focused on Hispanic populations) provided for 19 students at an estimated local cost of US$3000 in 1994, of which each student contributed US$80.14 Finally, one program involved matching 26 students to 26 local ethnically diverse families, asked the students to visit the family 6 times, and paid each family US$400 in 1996– 2000.17 Overall, there is poor data (only one study provided comprehensive data) to determine the costs of cultural competence training (evidence grade D).
DISCUSSION
Cultural competence training is being reported with increasing frequency in the literature and is gaining the attention of health care administrators and educators. Many different curricular methods and content areas have been evaluated. There is excellent or good evidence that cultural competence training impacts intermediate outcomes such as the knowledge, attitudes, and skills of health professionals. Good evidence also exists that cultural competence training impacts patient satisfaction and insufficient evidence that training impacts patient adherence (although the one study designed to do this demonstrated a positive impact). No studies have evaluated patient health outcomes.
It has been suggested that all cultural competence interventions should target the knowledge, attitudes, and skills of health professionals, so measurement of these intermediate outcomes are appropriate, and results are encouraging.1 Intermediate outcomes might ultimately impact patient outcomes considering that health care providers who are more knowledgeable about their patients’ backgrounds, who have more positive attitudes towards their patients, and who have the skills to communicate and apply a patient-centered approach are likely to provide better care to their patients.45 The Institute of Medicine report, Unequal Treatment, suggests that the mechanism involved in the link between improved communication and improved patient health status may be through improved patient satisfaction and adherence.1 The same mechanism may be operating with improved provider cultural competence, but it is additionally possible that culturally competent health professionals may actually be more skillful in obtaining histories and therefore in making diagnoses.
Concerns have existed about whether specific cultural information taught in curricula using a knowledge-based, categorical approach might promote stereotyping of patients.1,4 Although our study found that curricula teaching about specific cultures were associated with positive outcomes in general, one of the studies in our review demonstrated that, following an intervention that taught specific cultural information, students were more likely to believe that Aboriginal people were all alike.12 Given this finding, and other evidence demonstrating that providers exhibit bias and stereotyping behavior in their interactions with ethnic minority patients,46,47 this phenomenon should be evaluated with further studies. Only 2 of the 34 studies in our review included mention of concepts of racism, bias or discrimination in their content, which, in theory, might reduce the likelihood of this effect. Another strategy to avoid stereotyping, recommended by medical educators, is a patient-centered approach that emphasizes general concepts of culture in addition to providing specific cultural information.4
Although this systematic review determined that cultural competence training impacts provider knowledge, attitudes and skills, it is difficult to conclude from the literature which types of training interventions are most effective on which types of outcomes due to the heterogeneity and intermingling of curricular content and methods. There were no 2 studies that evaluated the exact same educational experience, and there were no studies that compared different types of training methods or content. However, almost all studies reported a positive effect, suggesting that employing any intervention may be effective. In particular, our review suggests that both longer and shorter duration interventions, experiential as well as nonexperiential, and curricula focusing on general concepts of culture and specific cultural information (alone and separately) are all associated with positive outcomes. This should be of great interest to medical educators and policy makers, and suggests it might be reasonable to compare interventions of varying length and content in a randomized controlled fashion.
We found that there was little uniformity across studies in measurement of outcomes (even within outcome categories), making it difficult to determine which specific types of knowledge, attitudes, or skills are impacted by cultural competence training. For example, some studies tested students on specific cultural information whereas other studies tested students on general cultural concepts, but no 2 studies reported using the same knowledge assessment tool. Although several studies used standardized measures of cultural self-efficacy, a wide range of attitudes was measured by the studies. Finally, there was also variation in skills measured, which ranged from developing a behavioral treatment plan to socializing with peers across race/ethnicity and would likely have very different and perhaps uncertain effects on clinical care. Future studies ought to link specific provider skills (for example, communication skills to address cultural barriers to adherence) to the relevant patient outcomes of interest (for example, adherence to recommended treatments).
Organizations and providers may have limited resources to conduct educational programs to improve cultural competence. There is insufficient evidence to determine the cost of cultural competence training because only 5 articles included data on costs and because the cost information contained in these 5 articles was too limited to allow for a comprehensive estimate. However, one of the studies that was able to demonstrate an improvement in patient satisfaction also included information about cost, and so perhaps the best evidence is found in that study, where it was estimated to cost $2000 (not including the cost of physician time) to train 9 emergency department physicians in the Spanish language.20 It is also worth noting that both shorter and longer interventions were effective, suggesting that future studies should evaluate the added benefit of additional investments of time.
The limitations of the existing literature provide a template for future research on cultural competence. First, further research would be aided greatly by a uniform conceptual model for provider cultural competence and by a standardized, validated instrument to measure cultural competence. This would allow for comparisons between studies in the future. Second, given the heterogeneity of curricular interventions, it would be helpful to have studies that compare interventions varied by either curricular content or training methods (ie, those that focused on general versus specific concepts of culture, those that use experiential learning compared with classrooms, and so on). Third, and probably most important, studies should attempt to measure patient outcomes. Finally, researchers should include data about the resources and costs of training, so that those who wish to employ interventions to improve the quality of care for racial/ethnic minorities know the investment that must be made in cultural competence to achieve a given outcome.
The results of our study should be interpreted with several limitations in mind. First, we were only able to review published studies. Therefore, there is the possibility of publication bias; that is, published studies are more likely to show a positive effect of cultural competence training than unpublished work. Indeed, most studies examining knowledge, attitudes, and skills were positive studies. Second, we limited our review to articles published in English and to those articles published after 1980. However, we believed these studies would be most relevant given changes in population demographics and the paradigms of medical education. Third, we developed our own criteria to grade the strength of the evidence; however there are no previously used systems for grading evidence that are designed for educational interventions. We are explicit about the method, though, so others could apply different standards if they choose. Finally, our review focused on interventions aimed at the education of health care providers, rather than on all possible organizational strategies to provide culturally and linguistically appropriate services, as other recent reviews have focused more specifically on organizational cultural competence.48
CONCLUSION
In conclusion, cultural competence training shows promise as a strategy for improving health care professionals’ knowledge, attitudes, and skills and patients’ ratings of care. We believe that interventions that focus on the avoidance of bias, general concepts of culture, and patient-centeredness are promising strategies that should be prioritized for further study. Further research should also focus on the development of standard instruments to measure cultural competence. Studies evaluating the impact of cultural competence training should compare different methods of teaching cultural competence, use objective and standardized evaluation methods and measure patient outcomes including patient adherence, health status and equity of services across racial and ethnic groups.
ACKNOWLEDGMENTS
This article is based on research conducted by the Johns Hopkins Evidence-based Practice Center under contract to the Agency for Healthcare Research and Quality (Contract No. 290-02-0018), Rockville, MD. The authors of this article are responsible for its contents, including any clinical or treatment recommendations. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality or of the US Department of Health and Human Services.
REFERENCES
- 1.Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Care. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 2.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57 Suppl 1:181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper LA, Roter DL. Patient-provider communication: The effect of race and ethnicity on process and outcomes of healthcare. In: Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: The National Academies Press; 2002. pp. 552–593. [Google Scholar]
- 4.Betancourt JR, Green AR, Carrillo JE, et al. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office of Minority Health DoHaHS. National Standards on Culturally and Linguistically Appropriate Services (CLAS) in Health Care. Federal Register. 2002;65:247. [Google Scholar]
- 6.Accreditation Council on Graduate Medical Education. [Accessed January 19, 2005];ACGME Outcome Project. Available at: http://www.acgme.org/outcome/comp/compFull.asp.
- 7.Beach MC, Cooper LA, Robison KA, et al. Strategies for Improving Minority Healthcare Quality. Rockville, MD: Agency for Healthcare Research and Quality; 2004. Evidence Report/Technology Assessment No. 90. AHRQ Publication No. 04-E008-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peña DE, Muñoz C, Grumbach K. Cross-cultural education in U.S medical schools: development of an assessment tool. Acad Med. 2003;78:615–622. doi: 10.1097/00001888-200306000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Sackett DL, Haynes RB, Guyatt GH, et al. Clinical Epidemiology: A Basic Science for Clinical Medicine. 2nd ed. Boston/Toronto/London: Little, Brown, and Company; 1991. [Google Scholar]
- 10.West S, King V, Carey TS, et al. Systems to rate the strength of scientific evidence. Evidence Report/Technology Assessment No. 47. Rockville, MD: Agency of Health Care Policy and Research; 2002. AHRQ Publication No. 02-E016. [PMC free article] [PubMed] [Google Scholar]
- 11.Mao C, Bullock CS, Harway EC, Khalsa SK. A workshop on ethnic and cultural awareness for second-year students. J Med Educ. 1988;63:624–628. doi: 10.1097/00001888-198808000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Copeman RC. Medical students, Aborigines and migrants: evaluation of a teaching programme. Med J Aust. 1989;150:84–87. doi: 10.5694/j.1326-5377.1989.tb136369.x. [DOI] [PubMed] [Google Scholar]
- 13.Rubenstein HL, O’Connor BB, Nieman LZ, et al. Introducing students to the role of folk and popular health belief-systems in patient care. Acad Med. 1992;67:566–568. doi: 10.1097/00001888-199209000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Nora LM, Daugherty SR, Mattis-Peterson A, et al. Improving cross-cultural skills of medical students through medical school-community partnerships. West J Med. 1994;161:144–147. [PMC free article] [PubMed] [Google Scholar]
- 15.Culhane-Pera KA, Reif C, Egli E, et al. A curriculum for multicultural education in family medicine. Fam Med. 1997;29:719–723. [PubMed] [Google Scholar]
- 16.Farnill D, Todisco J, Hayes SC, et al. Videotaped interviewing of non-English speakers: training for medical students with volunteer clients. Med Educ. 1997;31:87–93. doi: 10.1111/j.1365-2923.1997.tb02464.x. [DOI] [PubMed] [Google Scholar]
- 17.Haq C, Rothenberg D, Gjerde C, et al. New world views: preparing physicians in training for global health work. Fam Med. 2000;32:566–572. [PubMed] [Google Scholar]
- 18.Dogra N. The development and evaluation of a programme to teach cultural diversity to medical undergraduate students. Med Educ. 2001;35:232–241. doi: 10.1046/j.1365-2923.2001.00734.x. [DOI] [PubMed] [Google Scholar]
- 19.Godkin MA, Savageau JA. The effect of a global multiculturalism track on cultural competence of preclinical medical students. Fam Med. 2001;33:178–186. [PubMed] [Google Scholar]
- 20.Mazor SS, Hampers LC, Chande VT, et al. Teaching Spanish to pediatric emergency physicians: effects on patient satisfaction. Arch Pediatr Adolesc Med. 2002;156:693–695. doi: 10.1001/archpedi.156.7.693. [DOI] [PubMed] [Google Scholar]
- 21.Tang TS, Fantone JC, Bozynski ME, et al. Implementation and evaluation of an undergraduate Sociocultural Medicine Program. Acad Med. 2002;77:578–585. doi: 10.1097/00001888-200206000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Beagan BL. Teaching social and cultural awareness to medical students: “it’s all very nice to talk about it in theory, but ultimately it makes no difference”. Acad Med. 2003;78:605–614. doi: 10.1097/00001888-200306000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Crandall SJ, George G, Marion GS, et al. Applying theory to the design of cultural competency training for medical students: a case study. Acad Med. 2003;78:588–594. doi: 10.1097/00001888-200306000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Godkin M, Savageau J. The effect of medical students’ international experiences on attitudes toward serving underserved multicultural populations. Fam Med. 2003;35:273–278. [PubMed] [Google Scholar]
- 25.Frank-Stromborg M, Johnson J, McCorkle R. A program model for nurses involved with cancer education of black Americans. J Cancer Educ. 1987;2:145–151. doi: 10.1080/08858198709527875. [DOI] [PubMed] [Google Scholar]
- 26.Frisch NC. An international nursing student exchange program: an educational experience that enhanced student cognitive development. J Nurs Educ. 1990;29:10–12. doi: 10.3928/0148-4834-19900101-05. [DOI] [PubMed] [Google Scholar]
- 27.Alpers RR, Zoucha R. Comparison of cultural competence and cultural confidence of senior nursing students in a private southern university. J Cult Divers. 1996;3:9–15. [PubMed] [Google Scholar]
- 28.Williamson E, Stecchi JM, Allen BB, et al. Multiethnic experiences enhance nursing students’ learning. J Community Health Nurs. 1996;13:73–81. doi: 10.1207/s15327655jchn1302_1. [DOI] [PubMed] [Google Scholar]
- 29.Flavin C. Cross-cultural training for nurses: a research-based education project. Am J Hosp Palliat Care. 1997;14:121–126. doi: 10.1177/104990919701400308. [DOI] [PubMed] [Google Scholar]
- 30.Jeffreys MR, Smodlaka I. Steps of the instrument design process. An illustrative approach for nurse educators. Nurse Educ. 1996;21:47–52. doi: 10.1097/00006223-199611000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Napholz L. A comparison of self-reported cultural competency skills among two groups of nursing students: implications for nursing education. J Nurs Educ. 1999;38:81–83. doi: 10.3928/0148-4834-19990201-09. [DOI] [PubMed] [Google Scholar]
- 32.Underwood SM. Development of a cancer prevention and early detection program for nurses working with African Americans. J Contin Educ Nurs. 1999;30:30–36. doi: 10.3928/0022-0124-19990101-07. [DOI] [PubMed] [Google Scholar]
- 33.St Clair A, McKenry L. Preparing culturally competent practitioners. J Nurs Educ. 1999;38:228–234. doi: 10.3928/0148-4834-19990501-10. [DOI] [PubMed] [Google Scholar]
- 34.Inglis A, Rolls C, Kristy S. The impact on attitudes towards cultural difference of participation in a health focused study abroad program. Contemp Nurse. 2000;9:246–255. doi: 10.5172/conu.2000.9.3-4.246. [DOI] [PubMed] [Google Scholar]
- 35.Lasch KE, Wilkes G, Lee J, Blanchard R. Is hands-on experience more effective than didactic workshops in postgraduate cancer pain education? J Cancer Educ. 2000;15:218–222. doi: 10.1080/08858190009528701. [DOI] [PubMed] [Google Scholar]
- 36.Scisney-Matlock M. Systematic methods to enhance diversity knowledge gained: a proposed path to professional richness. J Cult Divers. 2000;7:41–47. [PubMed] [Google Scholar]
- 37.Smith LS. Evaluation of an educational intervention to increase cultural competence among registered nurses. J Cult Divers. 2001;8:50–63. [PubMed] [Google Scholar]
- 38.Erkel EA, Nivens AS, Kennedy DE. Intensive immersion of nursing students in rural interdisciplinary care. J Nurs Educ. 1995;34:359–365. doi: 10.3928/0148-4834-19951101-06. [DOI] [PubMed] [Google Scholar]
- 39.Gany F, de Bocanegra HT. Maternal-child immigrant health training: changing knowledge and attitudes to improve health care delivery. Patient Educ Couns. 1996;27:23–31. doi: 10.1016/0738-3991(95)00786-5. [DOI] [PubMed] [Google Scholar]
- 40.Way BB, Stone B, Schwager M, Wagoner D, Bassman R. Effectiveness of the New York State Office of Mental Health Core Curriculum: direct care staff training. Psychiatr Rehabil J. 2002;25:398–402. doi: 10.1037/h0094997. [DOI] [PubMed] [Google Scholar]
- 41.Stumphauzer JS, Davis LC. Training community-based, Asian-American mental health personnel in behavior modification. J Community Psychol. 1983;11:253–258. doi: 10.1002/1520-6629(198307)11:3<253::aid-jcop2290110309>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 42.Hansen ND. Teaching cultural sensitivity in psychological assessment: a modular approach used in a distance education program. J Pers Assess. 2002;79:200–206. doi: 10.1207/S15327752JPA7902_03. [DOI] [PubMed] [Google Scholar]
- 43.Gallagher Thompson D, Haynie D, Takagi KA, et al. Impact of an Alzheimer’s disease education program: focus on Hispanic families. Gerontol Geriatr Med. 2000;20:25–40. [Google Scholar]
- 44.Wade P, Berstein B. Culture sensitivity training and counselor’s race: effects on black female client’s perceptions and attrition. J Couns Psychol. 1991;38:9–15. [Google Scholar]
- 45.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 46.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 47.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50:813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 48.Anderson LM, Scrimshaw SC, Fullilove MT, et al. Culturally competent healthcare systems. A systematic review. Am J Prev Med. 2003;24(3 Suppl):68–79. doi: 10.1016/s0749-3797(02)00657-8. [DOI] [PubMed] [Google Scholar]