Abstract
Purpose
Patient-centeredness has been advocated to reduce racial/ethnic disparities in health care quality, but no empirical data support such a connection. The authors' purpose was to determine whether students with patient-centered attitudes have better performance and are less likely to demonstrate disparities with African American compared with white standardized patients (SPs).
Method
Third-year medical students were assessed by SPs at the Clinical Educational Center of the Johns Hopkins University School of Medicine in 2002. One African American and one white actor were trained as SPs for each of four case scenarios; students were randomly assigned to interact with either SP for each case. Before the exam, students were surveyed about their attitudes towards patient-centered medicine. Students with and without patient-centered attitudes were compared with regard to their performance with African American and white SPs. Outcome measures were student exam scores in interpersonal skill, history taking, physical exam, and counseling.
Results
All 177 of eligible students participated in all four case scenarios. With white SPs, students with patient-centered attitudes performed similarly to students without patient-centered attitudes in all four areas. However, with African American SPs, students with patient-centered attitudes performed significantly better than students without patient-centered attitudes in interpersonal skills (71.4 versus 69.4, P = .010), history taking (63.8 versus 61.1, P = .003), and counseling (92.1 versus 88.7, P = .002) and not significantly different in physical exam performance (73.6 versus 68.6, P = .311).
Conclusions
Patient-centered attitudes may be more important in improving physician behaviors with African American patients than with white patients and may, therefore, play a role in reducing disparities.
The Institute of Medicine has concluded that racial and ethnic minorities receive lower-quality health care and have poorer health outcomes than their white counterparts in the United States.1 In addition to well-documented disparities in the technical quality of care, studies have shown that disparities exist in the quality of patient–provider communication2,3 and in the attitudes that physicians harbor towards racial/ethnic minority patients.4 As a result, health care providers have been called upon to become more patient-centered in the care they deliver and to develop cultural competence.1,5–10
Patient-centered care is considered fundamental to cultural competence and theoretically has the potential to reduce racial/ethnic disparities in health care quality, because it directly addresses many of the hypothesized mechanisms by which a patient's race/ethnicity may affect clinician behaviors.11 First, physicians have been shown to exhibit stereotyping towards patients on the basis of the patient's race/ethnicity.4,11 Although stereotyping is often unconscious, patient-centered care may reduce the occurrence of stereotyping by embracing the notion that each person should be viewed as “a unique human being.”12 Second, physicians have been found to make differential clinical decisions based on patient race.11,13 Because patient-centered care has the goal of equalizing power between patients and doctors, disparities in clinical decisions may be reduced by increasing patient involvement. Finally, physicians have shown differential interpersonal behavior, characterized by more affective distance (less warmth and empathy), when interacting with racial/ethnic minorities.3,14 Here, too, patient-centeredness places emphasis on improving these qualities of patient–physician interactions.
Despite the theoretical promise of patient-centeredness to improve the quality of interpersonal relations between minority patients and their physicians,5,8 there have been no empirical studies demonstrating that a patient-centered approach reduces disparities. We have previously demonstrated that students performed more poorly during exams with African American standardized patients (SPs) than in exams with white SPs.15 The purpose of this study was to determine whether medical students who have patient-centered attitudes perform better and are less likely to demonstrate disparities in quality of care than students without patient-centered attitudes during exams with white and African American SPs.
Method
Study purpose and design
We used a brief cohort study design. We surveyed students immediately before their SP exams to determine their attitudes towards patient-centered medicine, and then examined the association of students' attitudes with their subsequent performance on exams with white and African American SPs. The study took place in 2002 and was reviewed and approved by the institutional review board of Johns Hopkins University School of Medicine.
Participants and setting
Participants were third-year students from two private mid-Atlantic region medical schools who participated in a formal assessment of their clinical skills at the Clinical Educational Center (CEC) of the Johns Hopkins University School of Medicine. All 177 students who participated in skill assessments between March 2002 and August 2002 were eligible for this study.
Standardized patient scenarios and training
Four standardized case scenarios were developed jointly by the CEC staff and the course directors at the respective schools. The four cases involved (1) abdominal pain attributable to ectopic pregnancy in a female patient, (2) low-back pain attributable to musculoskeletal strain in a male patient, (3) chest pain attributable to angina in a male patient, and (4) fatigue attributable to depression and domestic violence in a female patient. All four cases had been used extensively in previous assessments of third-year students. We trained one African American and one white actor to perform the SP role in each case. SP training followed a well-established protocol, with group and individual sessions conducted until each SP's performance was standardized. SPs were also trained to complete student assessments in a standardized manner. Each SP spent between six and eight hours in training. Their performance was monitored on examination days by trainers. SPs did not know the study hypotheses or the student's patient-centered scores.
Assignment of students to standardized patients
The African American and white SPs alternated on a daily basis across testing days. Students were assigned to test dates by their course directors. The course directors had no a priori knowledge when the assignments were made about which SP was going to be present. Therefore, each student would typically see two African American and two white SPs, although this could vary slightly if there were scheduling constraints.
Study measures
Our independent variable was students' patient-centered attitudes. Because there is no single gold standard for measuring patient-centered attitudes, and in fact great variability, we developed a measure of patient-centered attitudes that reflected each of five conceptual domains described by Mead and Bower.16 Because there is considerable theoretical overlap between the patient-centeredness and cultural competence,1, 5, 9, 10 we worded items such that the attitudes integral to cultural competence (curiosity, empathy, and respect)1 were also represented. Table 1 lists the nine items used in our scale. Possible response categories were on a five-point scale, where 5 = strongly agree, 3 = neither agree nor disagree, and 1 = strongly disagree. A patient-centered score was then derived from the sum of responses to the items and then multiplied by a factor of 2.222 to obtain scores on a 100-point scale, where 100 indicated the highest level of patient-centeredness, as measured by our instrument. Cronbach's alpha for our scale was 0.73, indicating satisfactory internal consistency.
Table 1. Items Used to Measure Patient-Centered Attitudes of 177 Third-Year Medical Students, Johns Hopkins Clinical Education Center, 2002.
| Item* | Patient-centered domain† | Cultural competence domain‡ |
|---|---|---|
| 1. Physicians need to “know where their patients are coming from” in order to treat their medical problems. | Biopsychosocial perspective | Curiosity |
| 2. A patient's background and culture, while worth noting, are not critical issues to explore in treating illness. | Biopsychosocial perspective | Curiosity |
| 3. I have a genuine interest in patients as people, apart from their disease. | The patient as person | Curiosity |
| 4. Patients usually know what is wrong with them. | Sharing power and responsibility | Respect |
| 5. Patients should always be given choice between medical treatments. | Sharing power and responsibility | Respect |
| 6. Patients should always be given information about their medical conditions. | Sharing power and responsibility | Respect |
| 7. Patients cannot get good care from a physician who does not entirely respect them. | Therapeutic alliance | Respect |
| 8. An important part of my role as a future physician is to provide emotional acceptance and empathy to patients. | Therapeutic alliance | Empathy |
| 9. Physicians should not allow patients to see their emotions. | The doctor as person | Empathy |
Possible responses were: strongly agree (five points), agree (four), neither agree nor disagree (three), disagree (two), or strongly disagree (one). Items 2 and 9 were reverse coded.
Domains of patient-centeredness, as described by Mead & Bower.16
Domains of cultural competence, as described by the Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care.1
Our main outcomes were derived from SPs' ratings of students' performance in the following domains: interpersonal skills, history taking, physical exam, and counseling behaviors. Interpersonal skills were rated by completion of a 23-item form reflecting verbal skills (such as “asks clear, unambiguous questions”), paraverbal skills (such as “conveys a sensitive and caring attitude to your needs or feelings”), and nonverbal skills (such as “makes comfortable eye contact with you”). Each of the 23 skills was rated on a five-point scale between poor and excellent. The total score was calculated as the sum of the scores on each individual item, and was then multiplied by a factor of 0.870 to obtain scores on a scale between 0 and 100.
History taking, physical exam maneuvers, and counseling scores were also reported by the SPs and were unique to each case. History-taking scores reflected between 10 and 20 facts per encounter (number of facts varied depending on case) that students ought to have elicited about the patient's symptoms and medical history; examples include “I have not had any burning when I urinate” for the patient with abdominal pain, and “the pain goes a little into my left arm” for the patient with chest pain. Physical exam scores reflected between 5 and 12 maneuvers (number of maneuvers varied depending on case) that ought to have been performed; examples include “checked my reflexes at both knees” for the patient with back pain, and “checked for rebound tenderness” for the patient with abdominal pain. Counseling scores reflected between 3 and 12 facts or ideas (number of facts varied depending on case) that students ought to have communicated to the patient; examples include “told me that my sleeping problem might be due to depression” for the patient with fatigue and “indicated what would happen next before leaving the encounter” for the patient with back pain. All scores were converted to a percent correct with range between 0 and 100.
Data analyses
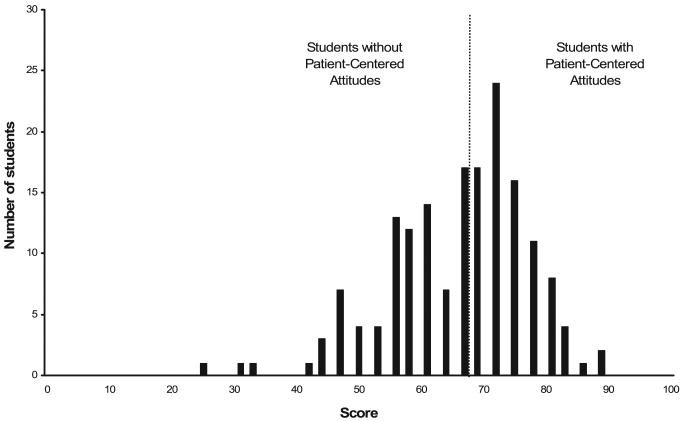
We dichotomized the scale of patient-centered attitudes on the basis of the distribution of scores such that students with scores below the median were considered not to have patient-centered attitudes and students with scores above the median were considered to have patient-centered attitudes (Figure 1). To determine which variables were potential confounders in our main analyses, we used χ2 tests to examine student characteristics associated with the presence of patient-centered attitudes or assignment to SPs, and t tests to examine student characteristics associated with exam performance in each of the four domains.
Figure 1.
Distribution of Patient-Centered Attitudes of 177 Third-year Medical Students, Johns Hopkins Clinical Education Center, 2002. Students were stratified by dividing the sample into two groups at the median, such that students without patient-centered attitudes (n = 85) had scores of <68 and students with patient-centered attitudes (n = 83) had scores ≥68, out of a possible 100 points.
Next, we examined whether students' patient-centered attitudes were associated with their exam performance in analyses that combined white and African American SPs using generalized estimating equations (GEE) analyses. This method minimizes any bias that could result if the SPs systematically differed in their scoring of students. The GEE analyses used a normal distribution and identity link function, an independent correlation structure, and the Huber/White/Sandwich estimator of variance. Then, to examine whether patient-centered attitudes were associated with exam performance with African American SPs separately, we stratified the sample by SP race and compared the scores of students with patient-centered attitudes with those of students without patient-centered attitudes using GEE analyses. Finally, we evaluated the presence of racial/ethnic disparities by comparing student exam performance with white versus African American SPs, stratified by patient-centeredness, using GEE. All data analyses were performed by Stata statistical software, Version 7 (StataCorp LP, College Station, Tex).
Results
Student characteristics and patient-centered attitudes
All of the 177 students who were eligible for this study participated. Each student completed all four scenarios, for a total of 708 encounters. Characteristics of the participants are presented in Table 2. One hundred and forty-six (86%) students were between 21 and 30 years of age; 91 (55%) were male; and 71 (47%) were white, 56 (37%) were African American, 19 (13%) were Asian, and four (3%) were Hispanic. Forty-nine students (29%) intended to have a future career in one of the primary care specialties (family practice, internal medicine, or pediatrics).
Table 2. Characteristics Associated with Patient-Centeredness for 177 Third-Year Medical Students, Johns Hopkins Clinical Education Center, 2002.
| Characteristics | Total students, no. (%) | Patient-centeredness | P-value | |
|---|---|---|---|---|
| Low, no. (%) | High, no. (%) | |||
| Age | 0.77 | |||
| 21–30 | 146 (86) | 75 (88) | 71 (86) | |
| >30 | 22 (14) | 10 (12) | 12 (14) | |
| Sex | 0.95 | |||
| Male | 91 (55) | 47 (55) | 44 (54) | |
| Female | 76 (45) | 38 (45) | 38 (46) | |
| Race/ethnicity | 0.35 | |||
| White | 71 (43) | 41 (48) | 30 (37) | |
| African American | 56 (34) | 25 (29) | 31 (38) | |
| Hispanic | 4 (2) | 1 (1) | 3 (4) | |
| Asian | 19 (11) | 10 (12) | 9 (11) | |
| Other | 17 (10) | 8 (9) | 9 (11) | |
| Future specialty | 0.03 | |||
| Primary care | 49 (29) | 18 (21) | 31 (39) | |
| Not primary care | 118 (71) | 67 (79) | 51 (62) | |
Students who intended to enter one of the primary care specialties were more likely to have patient-centered attitudes, though no other student characteristics were associated with patient-centered attitudes (Table 2). There were no student characteristics (e.g., race or primary care orientation) that were associated with assignment to African American versus white SPs. There was only one association between any student characteristics and exam performance in any of the four domains (interpersonal skills, history taking, physical exam, or counseling), namely, that female students performed statistically better in the interpersonal skills domain (mean interpersonal skill score 85.8 for females versus 83.6 for males, P = .018).
Association between patient-centered attitudes and student performance
In analyses combining students who interacted with African American and white SPs, students with patient-centered attitudes did not perform differently than students without patient-centered attitudes in interpersonal skills (74.4 versus 73.4, P = .123), history taking (65.1 versus 63.3, P = .110), physical exam (75.2 versus 73.0, P = .391), or counseling (92.2 versus 90.5, P = .075). Differences in exam performance for students with and without patient-centered attitudes, stratified by SP race, are shown in Table 3. When students interacted with white SPs, patient-centered attitudes were also not associated with performance in any domain; students with patient-centered attitudes performed similarly to students without patient-centered attitudes in interpersonal skills (77.6 versus 77.0, P = .559), history taking (66.5 versus 65.2, P = .526), physical exam (76.8 versus 76.4, P = .881), and counseling (92.3 vs 92.1, P = .891). However, when interacting with African American SPs, students with patient-centered attitudes performed significantly better than students without patient-centered attitudes in interpersonal skills (71.4 versus 69.4, P = .010), history taking (63.8 versus 61.1, P = .003), and counseling (92.1 versus 88.7, P = .002); and not significantly different in physical exam performance (73.6 versus 68.6, P = .311).
Table 3. Differences in Exam Performance for Students With and Without Patient-Centered Attitudes, Stratified by Standardized Patient Race*.
| Evaluation category | Students without patient-centered attitudes | Students with patient-centered attitudes | Mean difference | P-value | ||
|---|---|---|---|---|---|---|
| Mean score† | Standard error | Mean score | Standard error | |||
| White standardized patient | ||||||
|
| ||||||
| Interpersonal skills score | 77.0 | 5.3 | 77.6 | 5.4 | 0.6 | 0.559 |
|
| ||||||
| History score | 65.2 | 5.3 | 66.5 | 5.0 | 0.3 | 0.526 |
|
| ||||||
| Physical exam score | 76.4 | 5.9 | 76.8 | 7.8 | 0.4 | 0.881 |
|
| ||||||
| Counseling score | 92.1 | 1.6 | 92.3 | 1.4 | 0.2 | 0.891 |
|
| ||||||
| African American standardized patient | ||||||
|
| ||||||
| Interpersonal skills score | 69.4 | 2.3 | 71.4 | 2.0 | 2.0 | 0.010 |
|
| ||||||
| History score | 61.1 | 2.7 | 63.8 | 2.2 | 2.7 | 0.003 |
|
| ||||||
| Physical exam score | 68.6 | 5.6 | 73.6 | 6.6 | 5.0 | 0.311 |
|
| ||||||
| Counseling score | 88.7 | 3.1 | 92.1 | 3.2 | 3.4 | 0.002 |
The mean, standard error of the mean and statistical significance was determined using generalized estimating equations to adjust for clustering among SPs.
Each evaluation category was scored on a scale of 100, as evaluated by the standardized patient, using predetermined criteria, which varied for each clinical case. A student's overall score in each evaluation category was the equally weighted average of his or her performance on all four encounters.
Students without patient-centered attitudes demonstrated significant disparities by performing significantly more poorly with African American compared with white SPs in interpersonal skills (69.4 versus 77.0, P < .001) and physical exam performance (68.6 versus 76.4, P < .001). Similarly, students with patient-centered attitudes scored significantly lower in interpersonal skills (71.4 versus 77.6, P < .001) and physical exam (73.6 versus 76.8, P < .004) for African American compared with white SPs.
Discussion
To our knowledge, this is the first study to demonstrate that the attitudes of physicians-in-training are related to their performance on clinical exams, such that students with patient-centered attitudes performed better in encounters with African American SPs and not significantly different in encounters with white SPs. If patient-centered attitudes are stable over time, our study suggests that engendering a patient-centered approach in students may improve the quality of care for African American patients, and may reduce racial and ethnic disparities in some elements of medical care.
Although these findings are intriguing and potentially important, the absolute effects of patient-centeredness were modest. For example, the differences in history-taking performance with African American SPs between students with and without patient-centered attitudes (a mean difference of 2.7 points) amounts to an average loss of one history “fact” (or detail) on every one to four patients, depending on the scenario. Although this may not seem significant for any particular patient, this effect would compound over many patients. To the extent that we view the performance of certain details of the patient's history as important to appropriate diagnosis and treatment, these deletions could plausibly contribute to significant disparities in the health of populations. A similar case can be made for components of the interpersonal skills and counseling domains.
It is also worth noting that, although students with patient-centered attitudes performed better in interpersonal skills, history taking, and counseling with African American SPs than students without patient-centered attitudes, students with patient-centered attitudes still exhibited differences in their performance with white and African American SPs, as did students without patient-centered attitudes. This certainly suggests that a patient-centered approach will not eliminate all disparities in health care quality. Nonetheless, it is important to consider all means of disparity reduction, even modest means, because there is unlikely to be a single solution to the problem.
The measurement and correlation of attitudes with behaviors in physicians and physicians-in-training is a relatively undeveloped field of inquiry. In a study similar to ours, Haidet et al17 surveyed third-year medical students using the patient–practitioner orientation scale (PPOS) and found that higher PPOS scores (indicating a more patient-centered approach to medicine) were associated with higher SP ratings of humanism in students. Although that study did not examine differences across SPs' racial/ethnic groups or disparities in the care they received, its main implication, similar to ours, is that there was an association between students' attitudes and patients' experience of care. Further studies ought to explore this phenomenon, and enhance our understanding of which physician attitudes are associated with improved health care quality. As other studies have demonstrated the positive effects of cultural competence training on student attitudes,18 there is reason to be hopeful that patient-centered attitudes would be similarly susceptible to intervention.
One important source of potential bias in our study was that we relied on SPs' ratings of students' performance, and there were only eight total SPs (four African American and four white SPs). We believe that this threat to the validity of our study is somewhat moderated by the fact that our SPs were trained to rate students in a standardized manner and that the SPs were blinded as to how the students scored on the patient-centered attitude scale. We also used a clustering method to analyze our data that should minimize bias from potential differences in SP scoring. In addition, SP ratings are used widely in medical student assessments and have been found to be valid.19 Nevertheless, we believe that our data should be viewed in light of this limitation, and that efforts should be made to reproduce these findings in other settings.
Another potential limitation to our study was that our measure of patient-centeredness has not previously been validated. However, our measure was derived from a well-established conceptual framework and is associated with some of the same outcomes (such as intention to enter primary care) as are other measures of patient-centeredness.17 Therefore, our study provides preliminary data to assess the construct and predictive validity of the instrument. Finally, the generalizability of our study may be limited because we selected our participants from just two medical schools and because there was a higher proportion of African American students in our sample than in the overall population of U.S. medical students.
In conclusion, we believe that this study provides evidence that patient-centered attitudes may improve the quality of care for African American patients to a greater extent than it improves the quality of care for white patients, and, as such, that these attitudes may be important to consider in designing cultural competence training and other strategies to reduce disparities. Fostering such attitudes in students through techniques such as direct discussion, self-reflection and awareness exercises, and role modeling may contribute to a reduction in racial/ethnic disparities in health care quality. Future studies ought to explore the associations between the attitudes of health professionals and health care quality for racial/ethnic minority patients, and examine various educational strategies for engendering patient-centered attitudes in medical students.
Contributor Information
Dr. Mary Catherine Beach, Division of General Internal Medicine, Johns Hopkins University School of Medicine, with a joint appointment in the Department of Health, Behavior, & Society, Johns Hopkins University Bloomberg School of Public Health, and the Berman Institute of Bioethics, Johns Hopkins University, Baltimore, Maryland.
Ms. Mary Rosner, Clinical Education Center, Johns Hopkins University School of Medicine, Baltimore, Maryland.
Dr. Lisa A. Cooper, Division of General Internal Medicine, Johns Hopkins University School of Medicine, with a joint appointment in the Department of Health, Behavior, & Society, Johns Hopkins University Bloomberg School of Public Health, Baltimore, Maryland.
Mr. Patrick S. Duggan, Berman Institute of Bioethics, Johns Hopkins University, Baltimore, Maryland.
Dr. John Shatzer, Office of Teaching and Learning in Medicine, and associate professor of Medical Education and Administration, Vanderbilt University School of Medicine, Nashville, Tennessee.
References
- 1.Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Care. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 2.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient–physician relationship. JAMA. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 3.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient–physician communication during medical visits. Am J Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Soc Sci Med. 2000;50:813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 5.Green AR, Betancourt JR, Carrillo JE. Integrating social factors into cross-cultural medical education. Acad Med. 2002;77:193–197. doi: 10.1097/00001888-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Saha S, Arbelaez JJ, Cooper LA. Patient–physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003;93:1713–1719. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139:907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 8.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrillo JE, Green AR, Betancourt JR. Cross-cultural primary care: a patient-based approach. Ann Intern Med. 1999;130:829–834. doi: 10.7326/0003-4819-130-10-199905180-00017. [DOI] [PubMed] [Google Scholar]
- 10.Green AR, Carrillo JE, Betancourt JR. Why the disease-based model of medicine fails our patients. West J Med. 2002;176:141–143. [PMC free article] [PubMed] [Google Scholar]
- 11.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1 suppl):I140–I151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 12.Balint E. The possibilities of patient-centred medicine. J R Coll Gen Pract. 1969;17:269–276. [PMC free article] [PubMed] [Google Scholar]
- 13.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 14.Hooper EM, Comstock LM, Goodwin JM, Goodwin JS. Patient characteristics that influence physician behavior. Med Care. 1982;20:630–638. doi: 10.1097/00005650-198206000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Shatzer J, Rosner M, Beach MC, Haywood C, Verna R, Hayes R. The effects of race concordance on medical student clinical performance and interpersonal skills in an examination using standardized patients. Presented at the annual meeting of the Association of Medical Education in Europe; September, 2004. [Google Scholar]
- 16.Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51:1087–1110. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 17.Haidet P, Dains JE, Paterniti DA, et al. Medical student attitudes toward the doctor–patient relationship. Med Educ. 2002;36:568–574. doi: 10.1046/j.1365-2923.2002.01233.x. [DOI] [PubMed] [Google Scholar]
- 18.Beach MC, Price EG, Gary TL, et al. Cultural competence: a systematic review of health care provider educational interventions. Med Care. 2005;43:356–373. doi: 10.1097/01.mlr.0000156861.58905.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams RG. Have standardized patient examinations stood the test of time and experience? Teach Learn Med. 2004;16:215–222. doi: 10.1207/s15328015tlm1602_16. [DOI] [PubMed] [Google Scholar]