Abstract
Objectives:
To investigate the relationship between different clinical findings and condyle position.
Methods:
Tenderness on masseter (MM), temporal (TM), lateral pyterigoid (LPM), medial pyterigoid (MPM) and posterior cervical (PSM) muscles, limitation, deviation and deflection in opening of mouth, clicking, crepitating, tenderness on lateral palpation of temporomandibular joint (TMJ) area for each side of 85 patients were evaluated. Each side of patients was categorized into the clinical findings: no sign and/or symptom of temporomandibular dysfunctions (TMDs), only extraarticular findings and only intraarticular findings, extra and intraarticular findings. Condyle positions of 170 TMJs were determined the narrowest anterior (a) and posterior interarticular distance (p) on mid-sagittal MRIs of condyles and expressed as p/a ratio and these ratio were transformed into logarithmic base e. Spearman’s Correlation was used to investigate the relationship between the condyle position and the clinical findings. The difference between the condyle positions of different groups was tested by T test. Reliability statistic was used to determine intra-observer concordance of two measurements of condylar position.
Results:
A significant relationship was found between the condyle position and tenderness of PSM. There was no significant difference between the groups in aspect of the condyle position. Occlusion and condyle position correlated with significantly.
Conclusions:
The inclination of the upper cervical spine and craniocervical angulations can cause the signs and symptoms of TMD and condyle position is not main cause of TMDs alone but it may be effective together with other possible etiological factors synergistically.
Keywords: Condyle, Temporomandibular dysfunction, MRI
INTRODUCTION
Temporomandibular joint dysfunctions (TMDs) are nonspecific umbrella-term representing a wide variety of painful and/or dysfunctional jaw conditions. The gold standard of diagnosis of TMDs consists of patient history, physical evaluation and, in most chronic cases, behavioral or psychological assessments. Treatment has been also planned based on symptoms such as dysfunction and/or pain.1,2 In general, the symptoms and/or signs of TMDs can be categorized into: extrajoint and/or intrajoint.
Although there have been some controversies, no concentric condyle position has been still proposed as an implicated factors in development of TMDs.3–8 It has been stated that there has been a relationship between the position of the condyle and displacement of the disk, as well as a relationship between the position of the condyle and tenderness of the TMJs.9 It has been also supposed that superior disc position was found to be statistically significant for centric condylar position.4 It was found that condyles of patients with anterior disc displacement were situated more posterior and superior in the fossa than those in the control group and in the anterior disc displacement group, the posterior condylar displacement was noted to be 2.4 times greater than the superior condylar displacement.3 Weinberg mentioned that condylar displacement also contributes to TMDs depending on its direction. Anterior condylar displacement can initially affect the muscles by inducing over functional response in the proprioseptive system. Posterior condylar displacement usually results in an intrajoint response consisting of a disc displacement and clicking.10
The aim of this study was to evaluate the correlation between the condyle position and tenderness of masseter (MM), temporal (TM) and posterior cervical muscles (PSM), clicking, jaw deviation and deflection, jaw limitation, lateral palpation of TMJ and occlusion.
MATERIALS AND METHODS
Sample
In two months, 100 patients applied to Oral Diagnosis Clinic of faculty of dentistry for pain in face and/or jaws. The clinical signs and/or symptoms of 85 persons (170 joints) with TMDs were evaluated and were included to the study. Fifteen persons have had pain in face and/or jaws caused from different causes such as tooth ache, impacted teeth, lesions in soft tissues, lymphadenitis and sialadenitis. The patients with TMD signs and/or symptoms were included to detailed evaluation. Right and left sides of patients were evaluated and recorded separately. The age range of subjects was 19–65. The mean age of subjects was 29 in total, 28 for female patients and 34 for male patients.
Clinical examination
The clinical signs and symptoms clicking, crepitating, limitation, deviation, deflection, tenderness of masseter, temporal, lateral pyterigoid, medial pyterigoid and posterior cervical muscles, lateral palpation of TMJ area, occlusion were recorded by a clinician for each patient according to the Okeson.2 In Table 1, the criterion of clinical examination of each sign and symptom were presented. The joints were categorized into four groups: joints without the signs and/or symptoms of TMDs (C), intraarticular-articular group (IA) (clicking, deviation, deflection, limitation (hard-end-feel), and tenderness to the lateral palpation of TMJ), extra-articular group (EA) (tenderness on the MM, LPM, MPM and/or TM), complex group (IA+EA) (intra and extra-articular) according to the clinical signs and symptoms. Right and left joints and sides were categorized separately in a patient.
Table 1.
Clinical signs and symptoms were evaluated and defined according to the Okeson.2
| Sign and Symptoms | Definition |
|---|---|
| clicking | a single click sound by digital palpation of external ear-way at the opening of mouth |
| deviation | deviation of jaw to one side from midline with turn back to midline at the opening of mouth |
| deflection | deflection of jaw to one side without turn back to midline at the opening of mouth |
| limitation (hard-end-feel) | mouth opening limited at 25–30 mm (rotational amount) |
| lateral palpation of TMJ | tenderness at condylar head to manuel palpation |
| tenderness of MM | tenderness at any region of entire body of muscle |
| tenderness of TM | tenderness at any region of entire body of muscle |
| tenderness of PSM | tenderness at any region of entire body of muscle |
| tenderness of LP | tenderness at any region of entire body of muscle |
| tenderness of MP | tenderness at any region of entire body of muscle |
| occlusion | categorized into class 1, 2 and 3 according to the first molars relationship for left and right sides |
If the deviation occurred during opening and the jaw than returned to midline before 30 to 35 mm of total opening and if the speed of opening altered the location of the deviation, this condition was accepted as intraarticular deviation. The deviation with muscular origin is commonly large, inconsistent, sweeping movement not associated with the clicking sounds. The deflection with intraarticular origin was differentiated from the deflection with muscular origin by observing the protrusive movement. On the protrusion, if mandible deflected to the side of the involved joint this condition was recorded as intraarticular deflection. In the deflection with muscular origin, the direction of deflection depends on the position of the involved muscle with respect to the joint and deflection was not observed in protrusive movement. Clicking was identified by placing a stethoscope over the joint area. The intraarticular limitation (hard-end-feel) was differentiated from extraarticular limitation by the mild passive force to lower incisors. When the mouth could not opened wider even if mild force, the limitation was recorded as hard-end-feel. The amount of opening could increase by the mild passive force; this condition was accepted as myogenous limitation (soft-end-feel).2 During the patient was opening the mouth, condylar head was localized by the digital palpation and the fingertips of clinician were placed over the lateral aspects of joint. After the fingertips felt the lateral pole of condyle medial force was applied to the joint area. The feels of tenderness or pain at that area, was recorded as the tenderness of lateral palpation. The MM was palpated bilaterally at its superior and inferior attachments. First, the fingers were placed on each zygomatic arch and then were dropped down slightly just anterior to the joint and that area was palpated. Subsequently, the fingers were dropped to inferior attachment on the inferior border of the ramus. Anterior, middle and posterior regions of TM was independently palpated. The anterior region was above the zygomatic arch and anterior to the TMJ. The middle region was palpated directly above the TMJ and superior to the zygomatic arch. The posterior region was palpated above and behind the ear. Lateral and medial pyterigoid muscles were examined by functional manipulation according to Okeson.2 In palpating of PSM, the examiner’s fingers were slipped behind the patient’s head. The right hand palpated the right occipital area and the left hand palpated the left occipital area at the origins of muscles. The fingers moved down the length of the neck muscles trough the cervical area. Each side was palpated twice within a 5 min interval and subjects were asked to indicate pain or not. Two consecutive positive answers were considered to indicate tenderness of palpation for all muscles.
Condyle position
The condylar position were determined the narrowest anterior (a) and posterior interarticular distance (p) on mid-sagittal MRIs of condyles, in similar way as described in the literature.4 MRIs of joints were scanned and converted into digital images. Images were magnified and the measurements were made on these images as millimeters by computer. Most superior part of the glenoid fossa was used for the determination of condyle position. Posterior joint space (PJS) and anterior joint space (AJS) were measured in this area. Condyle position was expressed as PJS/AJS ratio and these ratio were transformed into logarithmic base (base e) according to the Blaschake and Blaschake11,12 and Pullinger and Hollender.13,14 The measurements were repeated in two weeks by same clinician blindly and the reproducibility of measurements was calculated. In Figures 1, 2 and 3, examples of centric, anterior and posterior condyle postions were presented.
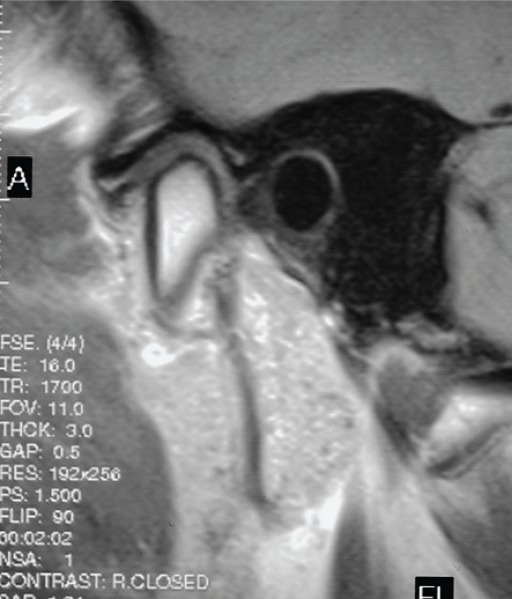
Figure 1.
An example of concentric condyle position.
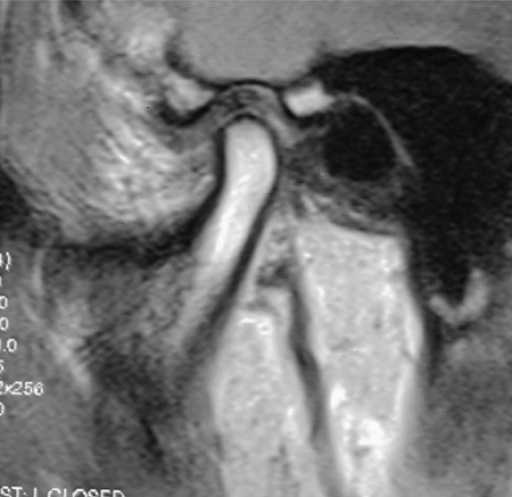
Figure 2.
An example of anterior condyle position.
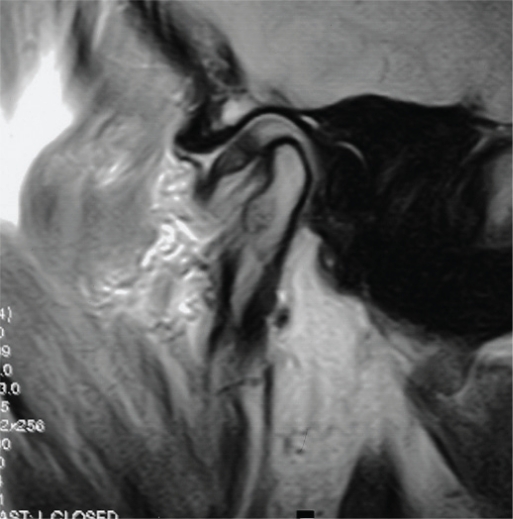
Figure 3.
An example of posterior condyle position.
Statistical analysis
Spearman’s correlation was used to investigate the relationship between the condyle position and the clinical findings. The difference between the condyle positions of different groups was tested by T test. Reliability statistic was used to determine intra-observer concordance of two measurements of condylar position.
RESULTS
Reliability value was 0.97. This measurement method is reproducible and reliable for the assessment of condyle position. The frequency and percentage of clinical findings were presented in Table 2. No case with deviation or deflection with muscular origin and crepitating was identified in sample.
Table 2.
The frequency of each group.
| Group | Number | Percentage |
|---|---|---|
| C | 35 | 20.6 |
| EA | 48 | 28.2 |
| IA | 50 | 29.4 |
| EA+IA | 37 | 21.8 |
There were 37 (22%) sides without extra or intraarticular symptom or sign. Forty and seven sides, (34%) have had only extraarticular symptoms (tenderness on MM, TM, LPM and MPM). In 40 (23%) sides, only intraarticular signs and/or symptoms were found. Both extra and intraarticular findings were observed in 36 sides (21%). (Table 2) The distribution of 85 patients was presented as number and percentage in Table 3. The distribution of number and percentage of occlusion 127 (74.7%), 21 (12.4%), 22 (12.9%) for class 1, class 2 and class 3 occlusions, respectively.
Table 3.
Frequency (%) and number of clinical findings.
| Tenderness on TMJ | 18 (11) |
| Deviation | 34 (20) |
| Deflection | 22 (13) |
| Tenderness of MM | 70 (41) |
| Tenderness on TM | 55 (32) |
| Tenderness of PSM | 59 (35) |
| Tenderness on LPM | 31 (18) |
| Tenderness on MPM | 31 (18) |
A significant relationship was found between the condyle position and the tenderness of PSM (at 0.05 level, spearman’s rho value:−0.164), occlusion (at 0.01 level, spearman’s rho value:−209). Posterior condyle position significantly correlated with the tenderness of PSM. There was no significant difference (P>.05) between the groups in aspect of condyle positions.
0 value represents real concentricity and + values and − values represent anterior and posterior positions respectively. According to this finding in Table 4, the frequency and percentage of the condyle positions were presented for each group.
Table 4.
Condyle positions categorized into concentric (0), posterior position (negative values) and anterior position (positive values) in each clinical group.
| Groups | |||||
|---|---|---|---|---|---|
| Condyle position | C | EA | IA | EA+IA | Total |
| 0 value | 1 | 1 | 0 | 0 | 2 |
| − values | 16 | 31 | 17 | 22 | 86 |
| + values | 20 | 25 | 23 | 14 | 82 |
| Total | 37 | 57 | 40 | 36 | 170 |
DISCUSSION
Tomography or magnetic resonance imagings (MRI) use to display TMJ structures and their pathologies. However, in tomographic imaging, the patients expose radiation. MRI and tomography aren’t available in every country. Signs and symptoms such as clicking, deviation, deflection or limitation of TMDs are fairly definitive for treatment planning. In TMDs, the purpose of treatment is the elimination or minimization of dysfunctions such as limitation, intermittent locking and extraarticular or intraarticular pain.1,2 Existing treatment approaches are generally sufficient to elimination of signs and symptoms. For this reason, we classified the patients according to the clinical findings in this study. However, in cases that resist to conventional treatments, proper imaging modalities should be necessary.
Several papers pointed out that the relationships between the disc position and condyle position.3 There has been limited information about the relationship between the clinical signs or symptoms and the condyle position. It was stated that there has been a relationship between the position of the condyle and displacement of the disk, as well as a relationship between the position of the condyle and tenderness of the TMJs.9 No significant relationship was found between the tenderness on lateral palpation and condyle position in this study. Surprisingly, condyle position was correlated with only the tenderness on PSM. Tenderness on masseter, temporal, lateral pyterigoid and medial pytreigoid muscles are the most common signs of TMDs but the sensitivity of PSM is considered as an accompanying feature.15 It was stated that TMD was seen in connection with a marked forward inclination of the upper cervical spine and an increased cranio cervical angulations.16 The asymmetric activation of jaw and neck muscles was interpreted as a compensatory strategy to achieve stability for the mandibular and cervical systems during masticatory function.17 It was also found that severe TMD showed a tendency to cervical spine hyperlordosis prevalence.18 In a systematic review which assessed the evidence concerning the association between head and cervical posture and TMD, it has been concluded that the association between intraarticular and muscular TMD and head and cervical posture is still unclear, and better controlled studies with comprehensive TMD diagnoses, greater sample sizes, and objective posture evaluation are necessary.2 Cervical posture and/or head position can be important etiological factors in development of muscular or articular TMDs. TMDs may be accompanying sign or symptom of cervical pathologies. Therefore, the treatment strategy of TMDs may be directed to improve the inclination of upper cervical spine and cranio cervical angulations or vice versa, condyle position may change the activation of neck muscles. This relationship needs to new investigation.
Weinberg10 mentioned that condylar displacement contributes to TMDs depending on its direction. Anterior condylar displacement can initially affect the muscles by inducing over functional response in the proprioseptive system. Posterior condylar displacement usually results in an intra-joint response consisting of a disc displacement and clicking. No significant difference was found between the groups in aspect of condyle position in this study. Furthermore, there were no relationships between the intrajoint signs and posterior condyle position or extrajoint findings and anterior condyle position. Contrary to the opinions of Weinberg, we found that a significant relationship between the posterior condyle position and the tenderness of PSM which is extraarticular finding. In addition, no significant difference was found between the groups in aspect of condyle position in this study. According to Table 4, only two cases with concentric condyle position and condyle position of 99% of total cases located in posterior or anterior position in glenoid fossa in this study. According to this finding, it can be concluded that condyle position is not main etiological factor in development of TMDs. Furthermore, the position of condyle in glenoid fossa can be different in normal persons. This finding is in accordance with the literature.6–8 However, it may effective together with other possible etiological factors synergistically. In the unilateral extra and intraarticular cases which have not other possible etiological factors; the affect of condyle position should be investigated by new studies. Furthermore, whether the condyle position varies with the age and gender should be examined to confirm its effect on the development of TMDs.
A significant relationship was found between the condyle position and occlusion type. This finding is accordance with the literature.19 However, there were several studies were reported that no relationship between these parameters.5,20,21 In this study, the number and percentage of class 1 (127, 74.7%) occlusion was significantly higher than the others (21, 12.4% and 22, 12.9%). Therefore, this finding is not sufficient to reach a reliable conclusion. The number of occlusion types in each group must be equal and large sample should be evaluated to obtain reliable results
CONCLUSIONS
Within the limitation of this study, the inclination of the upper cervical spine and craniocervical angulations can cause the signs and symptoms of TMD and condyle position is not main cause of TMDs alone but it may be effective together with other possible etiological factors synergistically.
REFERENCES
- 1.Goldstein BH. Temporomandibular disorders: a review of current understanding. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:379–385. doi: 10.1016/s1079-2104(99)70048-x. [DOI] [PubMed] [Google Scholar]
- 2.Okeson JP. Management of temporomandibular disorders and occlusion. 4th ed. Mosby-Year Book; St. Louis, Missouri: 1998. p. 298. [Google Scholar]
- 3.Gateno J, Anderson PB, Xia JJ, Horng JC, Teichgraeber JF, Liebschner MA. A comparative assessment of mandibular condylar position in patients with anterior disc displacement of temporomandibular joint. J Oral Maxillofac Surg. 2004;62:39–43. doi: 10.1016/j.joms.2003.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Incesu L, Taşkaya-Yilmaz N, Oḡütcen-Toller M, Uzun E. Relationship of condylar position to disc position and morphology. Eur J Radiol. 2004;51:269–273. doi: 10.1016/S0720-048X(03)00218-3. [DOI] [PubMed] [Google Scholar]
- 5.Serra MD, Gaviao MBD. Evaluation of condyler position from transcranial projections in primary dentition. Dentomaxillofac Radiol. 2006;35:110–116. doi: 10.1259/dmfr/23165237. [DOI] [PubMed] [Google Scholar]
- 6.Bonilla-Aragon H, Tallents RH, Katzberg RW, Kyrkanides S, Moss ME. Condyle position as a predictor of temporomandibular joint internal derangement. J Prosthet Dent. 1999;82:205–208. doi: 10.1016/s0022-3913(99)70157-5. [DOI] [PubMed] [Google Scholar]
- 7.Brand JW, Whinery JG, Jr, Anderson QN, Keenan KM. Condylar position as a predictor of temporomandibular joint internal derangement. Oral Surg Oral Med Oral Pathol. 1989;67:469–476. doi: 10.1016/0030-4220(89)90394-0. [DOI] [PubMed] [Google Scholar]
- 8.Bean LR, Thomas CA. Significance of condylar positions in patients with temporomandibular disorders. J Am Dent Assoc. 1987;114:76–77. doi: 10.14219/jada.archive.1987.0043. [DOI] [PubMed] [Google Scholar]
- 9.Vasconcelos Filho JO, Menezes AV, Freitas DQ, Manzi FR, Bóscolo FN, de Almeida SM. Condylar and disk position and signs and symptoms of temporomandibular disorders in stress-free subjects. JADA. 2007;138:1251–1255. doi: 10.14219/jada.archive.2007.0351. [DOI] [PubMed] [Google Scholar]
- 10.Weinberg LA. Role of condylar position in TMJ dysfunction-pain syndrome. J Prosthet Dent. 1979;41:636–643. doi: 10.1016/0022-3913(79)90062-3. [DOI] [PubMed] [Google Scholar]
- 11.Blaschke DD, Blaschke TJ. A method for quantitatively determining temporomandibular joint bony relationships. J Dent Res. 1981;60:35–43. doi: 10.1177/00220345810600010701. [DOI] [PubMed] [Google Scholar]
- 12.Blaschke DD, Blaschke TJ. Normal TMJ bony relationships in centric occlusion. J Dent Res. 1981;60:98–104. doi: 10.1177/00220345810600021901. [DOI] [PubMed] [Google Scholar]
- 13.Pullinger A, Hollender L. Assessment of mandibular condyle position: A comparison of transcranial radiographs and linear tomograms. Oral Surg Oral Med Oral Pathol. 1985;60:329–334. doi: 10.1016/0030-4220(85)90319-6. [DOI] [PubMed] [Google Scholar]
- 14.Pullinger A, Hollender L. Variation in condyle-fossa relationships according to different methods of evaluation in tomograms. Oral Surg Oral Med Oral Pathol. 1986;62:719–727. doi: 10.1016/0030-4220(86)90270-7. [DOI] [PubMed] [Google Scholar]
- 15.Olivo SA, Bravo J, Magee DJ, Thie NM, Major PW, Flores-Mir C. The association between head and cervical posture and temporomandibular disorders: a systematic review. J Orofac Pain. 2006;20:9–23. [PubMed] [Google Scholar]
- 16.Sonnesen L, Bakke M, Solow B. Temporomandibular disorders in relation to craniofacial dimensions, head posture and bite force in children selected for orthodontic treatment. Eur J Orthod. 2001;23:179–192. doi: 10.1093/ejo/23.2.179. [DOI] [PubMed] [Google Scholar]
- 17.Ries LG, Alves MC, Bérzin F. Asymmetric activation of temporalis, masseter, and sternocleidomastoid muscles in temporomandibular disorder patients. Cranio. 2008;26:59–64. doi: 10.1179/crn.2008.008. [DOI] [PubMed] [Google Scholar]
- 18.Cohlmia JT, Ghosh J, Sinha PK, Nanda RS, Currier GF. Tomographic assessment of temporomandibular joints in patients with malocclusion. Angle Orthod. 1996;66:27–35. doi: 10.1043/0003-3219(1996)066<0027:TAOTJI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Langberg BJ, Arai K, Miner RM. Transverse skeletal and dental asymmetry in adults with unilateral lingual posterior crossbite. Am J Orthod Dentofacial Orthop. 2005;127:6–15. doi: 10.1016/j.ajodo.2003.10.044. [DOI] [PubMed] [Google Scholar]
- 20.Munhoz WC, Marques AP, Siqueira JT. Radiographic evaluation of cervical spine of subjects with temporomandibular joint internal disorder. Braz Oral Res. 2004;18:283–289. doi: 10.1590/s1806-83242004000400002. [DOI] [PubMed] [Google Scholar]
- 21.Stamm T, Hohoff A, Van Meegen A, Meyer U. On the three-dimensional physiological position of the temporomandibular joint. J Orofac Orthop. 2004;65:280–289. doi: 10.1007/s00056-004-0402-3. [DOI] [PubMed] [Google Scholar]