Abstract
Glomerular injury and podocyte loss leads to secondary tubulointerstitial damage and the development of fibrosis. The possibility of genetically reprogramming adult cells, termed induced pluripotent stem cells (iPS), may pave the way for patient-specific stem-cell-based therapies. Here, we reprogrammed normal human mesangial cells to pluripotency by retroviral transduction using defined factors (OCT4, SOX2, KLF4 and c-Myc). The kidney iPS (kiPS) cells resembled human embryonic stem-cell-like colonies in morphology and gene expression: They were alkaline phosphatase-positive; expressed OCT3/4, TRA-1 to 60 and TRA-1 to 81 proteins; and showed downregulation of mesangial cell markers. Quantitative (qPCR) showed that kiPS cells expressed genes analogous to embryonic stem cells and exhibited silencing of the retroviral transgenes by the fourth passage of differentiation. Furthermore, kiPS cells formed embryoid bodies and expressed markers of all three germ layers. The injection of undifferentiated kiPS colonies into immunodeficient mice formed teratomas, thereby demonstrating pluripotency. These results suggest that reprogrammed kidney induced pluripotent stem cells may aid the study of genetic kidney diseases and lead to the development of novel therapies.
Over two-thirds of patients with chronic kidney disease who progress to end-stage renal failure suffer from glomerular disorders.1 Irreparable damage to glomerular cells leading to podocyte loss are common to a number of glomerulopathies that are responsible for the initiation and progression of tubulointerstitial fibrosis and impaired renal function.2–5 The major challenge in renal regeneration involves replacing damaged glomerular cells to enable the spontaneous regeneration of damaged tubules.6,7
The cellular components of the glomerulus are developmentally derived from the mesenchyme and are considered highly terminally differentiated with a limited capacity to replicate in situ.2,8,9 The location of progenitor cells within the kidney remains elusive.10 However, recently, Ronconi et al.11 reported a heterogenous subset of CD133+CD24+ progenitor cells capable of replacing both glomerular and tubular epithelial cells. These cells, located in the Bowman's capsule, may migrate to the glomerular tuft and differentiate into podocytes, leading to podocyte replacement following injury.11 Mesangial cells that comprise specialized pericytes of the glomerulus represent another cell type important in maintaining normal glomerular structure and in regulating blood flow of the glomerular capillaries through their contractile activity.12
The direct reprogramming of somatic cells to produce induced pluripotent stem (iPS) cells is a prominent recent advance in stem cell biology13 and has attracted considerable attention in disease modeling, drug screening and regenerative medicine.14 Pluripotent cells can be derived from fibroblasts in the mouse13 and human15,16 by the induced expression of four transcription factors (OCT4, SOX2, KLF4 and c-Myc). The derivation of iPS cell lines from patients with genetic disorders may be achieved by reprogramming somatic cells toward a pluripotent state.17–20 A fundamental question is whether terminally differentiated kidney cells can be reprogrammed to pluripotency, that is, generate stem cells that have the potential to differentiate into all three germ layers. Our study, for the first time, provides proof-of-concept for the direct nuclear reprogramming of adult human mesangial cells to generate kidney-derived iPS (kiPS) cells.
RESULTS
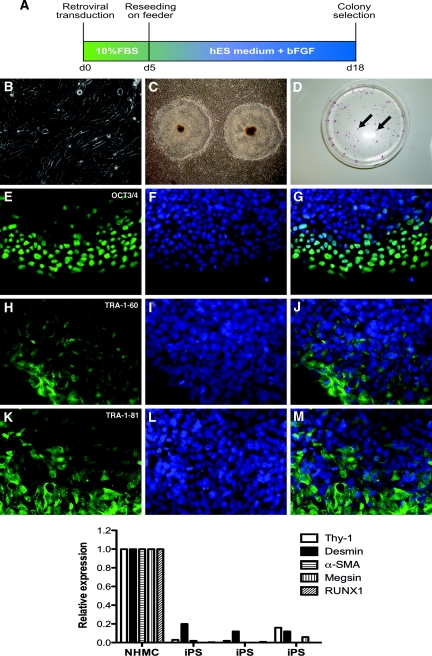
Normal human mesangial cells (NHMCs) were used to derive iPS cell lines using genetic programming that consisted of transfection of 293FT cells with retroviral vectors using the genes OCT3/4, SOX2, KLF4 and c-Myc, as previously reported.3,4 After 5 d of transfection, NHMCs were reseeded on mouse embryonic fibroblast (MEF) feeders (for timeline, see Figure 1A). Compared with cultured NHMCs (Figure 1B), as early as 12 days after retroviral transduction, distinct colonies were evident exhibiting morphology similar to human embryonic stem (hES) cells that contained spontaneous differentiation at colony centers, a morphologic trait of hES colonies (Figure 1C). From 5 × 104 NHMCs, an average of 40 iPS colonies were observed. These colonies stained alkaline phosphatase-positive, a phenotypic assessment of undifferentiated ES/iPS cells (Figure 1D). To confirm that kiPS cells had the characteristics of typical iPS cells, we examined stem cell marker expression. Immunofluorescence microscopy showed that kiPS cells localized for OCT3/4, TRA-1 to 60 and TRA-1 to 81 proteins (Figure 1E–M) after long-term culture at passage 22.
Figure 1.
Kidney mesangial cell-derived iPS cells express stem cell markers. (A) The timeline of induction of iPS cells from human mesangial cells following retroviral transduction. (B) Representative images of normal cultured human mesangial cells reprogrammed to generate iPS colonies (C). (D) Alkaline phosphatase-positive iPS colonies (arrows). Immunofluorescence staining of mesangial cell-derived iPS colonies shows localization of OCT3/4 protein (E; green), with corresponding DAPI-stained nuclei (F; blue) and a merged image (G). TRA-1-60 (H–J) and TRA-1-81 (K–M) proteins are also expressed. Original magnifications (B, E–M ×400, C ×10). The graph in the lower panel shows qPCR of mesangial cell markers in NHMCs, with a downregulated expression in iPS cells from 3 separate colonies at passage 4. 120 × 189mm (600 × 600 DPI).
The NHMCs were negative for protein expression of Factor VIII Related Antigen, cytokeratin 18/19 and von Willebrand factor (Lonza Walkersville Inc., USA). Using qPCR, a panel of markers was screened to determine the phenotype of the starting population, including the mesangial specific gene megsin.21 NHMCs were found to express megsin, Thy-1, desmin, α-smooth muscle actin (α-SMA) and RUNX1, which were downregulated following differentiation to iPS cells at passage 4 (Figure 1).
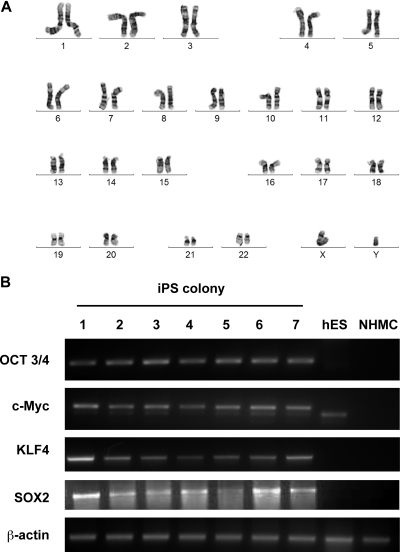
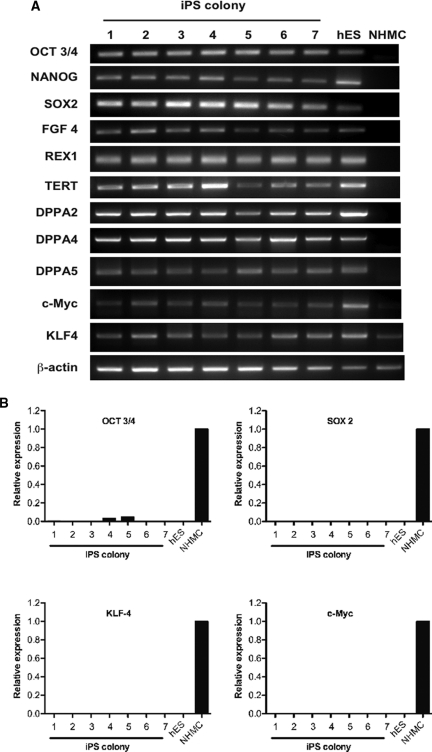
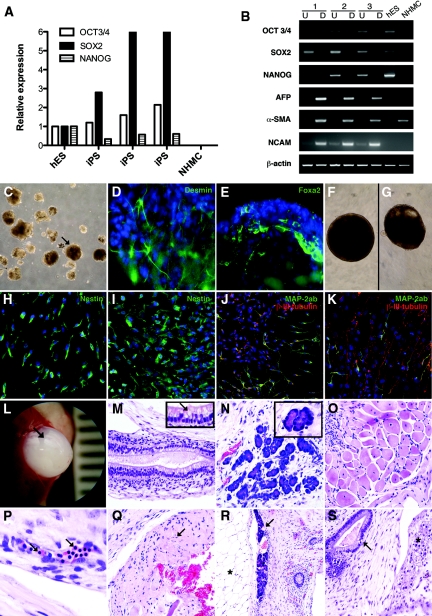
The kiPS cells displayed a normal karyotype of 46XY (Figure 2A). PCR of genomic DNA confirmed the integration of the target vectors in kiPS colonies (Figure 2B) but not in NHMCs. In addition, DNA genetic fingerprint analysis confirmed that the human iPS colonies were derived from the NHMC source and were not a result of cross contamination (Supplementary Figure 1). Reverse-transcriptase PCR (RT-PCR) analysis revealed that the kiPS cells expressed stem cell marker genes for OCT3/4, NANOG, SOX2, fibroblast growth factor (FGF)-4, reduced expression protein 1 (REX1), telomerase reverse transcriptase (hTERT), developmental pluripotency-associated (DPPA)-2, DPPA4 and DPPA5. This was comparable to hES cells but different from NHMCs (Figure 3A). qPCR using transgene-specific primers showed that the OCT3/4, SOX2, KLF4 and c-MYC transgenes were absent in all 7 kiPS clones after four passages confirming retroviral silencing (Figure 3B). In comparison, NHMCs at day 6 after retroviral transduction show an upregulated expression OCT3/4, SOX2, KLF4 and c-Myc transgenes (Figure 3B). qPCR confirmed that relative to hES cells, iPS cells expressed stem cell markers OCT3/4, SOX2 and NANOG, with an absence of mRNA expression in NHMCs (Figure 4A).
Figure 2.
(A) The iPS colonies display a normal 46XY karyotype. (B) PCR of genomic DNA shows the integration of the target vectors in mesangial cell-derived iPS cells at passage 4. Lanes 1–7 show representative iPS cells following retroviral transduction, confirming the expression of OCT3/4, c-Myc, KLF4 and SOX2, compared to human embryonic stem (hES) cells (Lane 8) and normal cultured mesangial cells (NHMC; Lane 9). β-actin is shown as a loading control and for positive amplification. 154x218mm (600 × 600 DPI).
Figure 3.
(A) RT-PCR analysis of stem cell marker genes in kiPS cells for expression of OCT3/4, NANOG, SOX2, FGF4, REX1, TERT, DPPA2, DPPA4, DPPA5, c-Myc and KLF4. Lanes 1–7 represent mesangial cell-derived iPS (kiPS) cells compared to hES cells (Lane 8) and the NHMC target cells at day 0 (Lane 9). The β-actin housekeeping gene is also shown. Panel (B) shows quantitative PCR using primers specific for the transgenes, and not detecting endogenous gene expression levels (shown in Panel A), which confirms retroviral transgene silencing in most kips colonies (passage 4). This is evidenced by a loss of OCT3/4, SOX2, KLF4 and c-Myc expression analogous to expression levels in hES cells. In comparison, an upregulated expression of OCT3/4, SOX2, KLF4 and c-Myc is observed in NHMCS at 6 days following retroviral induction. 112×196mm (150 × 150 DPI).
Figure 4.
Kidney-derived iPS cells demonstrate pluripotency. (A) qPCR of stem cell markers OCT3/4, SOX2 and NANOG in kidney-iPS cells (kiPS) relative to human embryonic stem cells (hES), with an absence of expression in normal human mesangial cells (NHMCs). (B) RT-PCR shows undifferentiated iPS cells (U; Lanes 1, 3, 5) and hES expressed stem cell marker genes OCT3/4, SOX2 and NANOG. In comparison, differentiated embryoid bodies (EBs) (B; Lanes 2, 4, 6) expressed markers from all three germ layers, including α-fetoprotein (AFP; endoderm), α-smooth muscle actin (α-SMA; mesoderm) and neural cell adhesion molecule (NCAM; ectoderm), but did not express undifferentiated stem cell markers. kips formed EBs (C; arrow) with protein localization evident for desmin (D; mesoderm) and Foxa2 (E; endoderm) by immunofluorescence staining. Brightfield images of neural-directed EBs (NDEBs) from hES cells (F) and kiPS cells (G) at day 14. Immunofluorescence staining of NDEBs from hES cells show expression of nestin (H), β-iii-tubulin and MAP2ab (merged, J). In Panels D–K, DAPI-stained nuclei are evident in blue. Nestin (I), β-iii-tubulin and MAP2ab (merged, K) are also observed in NDEBs from kiPS. Original Magnifications C ×10; D, E ×400; F–K ×200. Teratomas are evident following the injection of undifferentiated kiPS cells into immunodeficient mice (L; arrow). Panels M–S show hematoxylin and eosin staining of tissues from all three germ layers, including endoderm; (M) pseudostratified ciliated respiratory epithelium with goblet cells (arrow inset Mag ×1000), (N) serous glands (acini shown in inset Mag ×1000), mesoderm; (O) muscle, (P) nucleated red blood cells (arrows); and endoderm: (Q) neural tissue. At lower power (Mag ×100), panels R and S show glandular tissue (arrows) in cystic teratomas adjacent to adipocytes (asterisk; R) and immature cartilage (asterisk; S). Original magnifications (K × 400; H–J, L ×200; M, N ×100). 120 × 173mm (600 × 600 DPI).
After 18 d in suspension culture, iPS cells had differentiated into embryoid bodies (EBs). RT-PCR of differentiated EBs showed marker gene expression from endoderm (α-fetoprotein; AFP), mesoderm (α-SMA) and ectoderm (neural cell adhesion molecule; NCAM), shown in Figure 4B. The expression of these genes was absent in undifferentiated cells from the same colonies (Figure 4B). RT-PCR confirmed that α-SMA was expressed in kiPS cells and NHMCs but not in hES cells (Figure 4B). Furthermore, immunofluorescence microscopy of EBs at day 7 (Figure 4D,E) showed protein localization for desmin (mesoderm), Fox2 (endoderm) and nestin (ectoderm; not shown). To assess ectodermal lineage differentiation further, neural-directed EB differentiation was performed on hES and kiPS cells (Figure 4F and G) showing immunofluorescence staining of the neural stem cell marker nestin (Figure 4H, I) and β-iii-tubulin protein expression with microtubule-associated protein 2ab (MAP2ab) colocalization (Figure J, K) identifying neurons.
To test pluripotency in vivo, immunodeficient mouse recipients were injected with kiPS colonies. The formation of encapsulated cystic teratomas (Figure 4L) were observed (3/3 mice) and showed differentiated tissues from all three germ layers (Figure 4M-S). Notably, the teratomas showed evidence of endoderm (respiratory epithelium, serous glands), mesoderm (muscle, nucleated red blood cells, car-tilage), and ectoderm (neural tissue). Taken together, our analyses of iPS colonies derived from retrovirally transduced human mesangial cells confirm pluripotent potential.
DISCUSSION
The culture of immortalized cell lines from kidney disease patients is an invaluable resource for medical research but is largely limited to tumor cell lines or transformed derivatives of kidney tissue. Patient-derived iPS cell lines, using a reprogramming protocol of somatic cells from patients with genetic disorders,22 will provide an opportunity to generate pluripotent cells for the facilitation of pharmaceutical development and small molecule screening specifically targeted at genetic disorders.14 These cells could, in turn, be used for disease modeling and eventually autologous cell replacement therapies.
A fundamental question of reprogrammed somatic cells from patients with genetic kidney disease such as polycystic kidney disease [PKD23,24] and Alport Syndrome,25 is whether the iPS cells can mimic the disease phenotype. iPS cells derived from patients with PKD and Alport Syndrome that maintain the disease genotype and phenotype indefinitely could be used for disease modeling26 and screening compounds aimed at modifying epigenetic and/or transcriptional abnormalities,27 important regulators of these genetic disorders.
Kim et al.28 recently reported that iPS retain a lingering genome-wide epigenetic memory of their cell of origin.28 Furthermore, histone methylation patterns and transcription profiles of genetically identical iPS cell lines derived from different somatic cell types were found to be distinctive to their tissue origin.29 Our efficiency in generating iPS cells from human kidney mesangial cells was comparable to reports using human skin fibroblasts.15,16 Further analysis will be necessary to determine the molecular and functional differences and differentiation potential of kidney-derived iPS cells to more efficiently generate mesoderm and kidney cells compared with iPS cells derived from fibroblasts and target cells from other sources.
A residual cellular epigenetic memory of mesangial cell-derived iPS cell lines may open a new avenue for the generation other glomerular cells, such as podocytes. The directed differentiation of mesangial cell-derived iPS lines to other kidney cell types must rely on the identification of antigenic and molecular markers to establish differentially upregulated genes important in podocyte development. We have recently used a FACS-based selective strategy underpinned by transcriptional profiling to isolate hES-derived cells that had differentiated toward a renal progenitor state.30 A fraction of CD24+podocalyxcin+ GCTM2neg differentiated hES cells were shown to express upregulated genes associated with metanephric mesenchyme in comparison to other cell lineages.30
In the long term, PKD and Alport patient-derived iPS lines could be generated to correct the genetic defect identified in the cells. A fundamental goal is to reprogram the somatic cells derived from genetic kidney disease patients and establish iPS cell lines that are indistinguishable from healthy individuals to be used in the development of cellular-based therapies, as has recently been reported in hematopoietic cells from patients with Fanconi anemia,31 degenerative disorders including amyotrophic lateral sclerosis [ALS;18] and dyskeratosis congenita.20 Ultimately, kiPS cell lines could become an essential tool for the exploration of high throughput screening of drugs, natural compounds and toxin screens for new drug discovery and pharmacologic testing, and to determine the potential of induced pluripotency as a therapeutic strategy.
CONCISE METHODS
Retroviral Transfection of Human Mesangial Cells
Primary normal human mesangial cells (NHMC) from an 18-yr-old male kidney (Lonza) were cultured in MsGM Mesangial Growth Media with 5% fetal bovine serum (FBS) at 37 °C. Retroviral vectors containing human OCT3/4, SOX2, KLF4 and c-Myc were introduced into 293FT cells and the supernatant cultured with NHMCs for 24 h, as described previously.16 After 5 d, the transduced NHMCs were reseeded onto MEF feeders in KO DMEM (Life Technologies Invitrogen, CA, USA) containing 20% KO (knockout) serum replacement and human basic FGF (10ng/ml). Eighteen days after transduction, colonies were mechanically dissociated for replating.
Embryoid Body Differentiation and Neural Staining
To test the differentiation capacity of iPS cells, floating suspension cultures were used to form EBs after 18 d of culture, as described previously.15,16 For neural-directed EB differentiation, 3000 disassociated kiPS or HES3 cells were distributed to each well of a round-bottom ultra-low attachment 96-well plate (Corning, MA, USA) containing 100μl of Neurobasal Medium per well (Neurobasal A, 5% ITS-X, 2.5% Penicillin/Streptomycin, 5% Glutamax, 5% B27 and 5% N2; Invitrogen). Wells were also supplemented with 0.125% PVA, 1mM ROCK inhibitor Y-27632, 20ng/ml EGF and 20ng/ml FGF (R&D Systems, MN, USA) and incubated at 37 °C in 5% CO2 in air. 100ng/ml of noggin per well (R&D Systems) was added at day 0 and 4. After 24 h, cell suspensions aggregated to form spheres or ‘neural-directed embryoid bodies’ (NDEBs). Media was changed at days 4 and 8, and every 2 d thereafter.
Aliquots of NDEBs were plated after 14 d in suspension onto glass cover slips coated with 10mg/ml Poly-D-Lysine and 5mg/ml Laminin (BD, NJ, USA), grown for a further 7 d in Neurobasal Medium containing 20ng/ml EGF and 20ng/ml FGF, and stained with antibodies for Nestin (ABcam, MA, USA). Further aliquots of NDEBs were plated after 21 d in suspension and grown for a further 14 d before staining with antibodies for β-iii-tubulin and MAP2ab (Millipore, MA, USA).
Alkaline Phosphatase Staining and Immunofluorescence Microscopy
Following 4% paraformaldehyde fixation, immunofluorescence for the hES-cell specific proteins TRA-1 to 60 and TRA-1 to 81 were performed using an ES cell characterization kit (Millipore) and an OCT-3/4 primary antibody (Santa Cruz Biotechnology, CA, USA). Antibodies for desmin (Dako, CA, USA), Foxa2 (Santa Cruz), Nestin (ABcam) were used for EB wholemount staining at day 7. Alkaline phosphatase staining for the phenotypic characterization of iPS cells was assessed using a Leukocyte Alkaline Phosphatase kit (Sigma Chem Co., USA).
PCR, Karyotype and Fingerprinting Analysis
RNA was extracted from iPS cells (passage 4), embryoid bodies (day 18 of differentiation) and hES cells (H9 cell line obtained from the Australian Stem Cell Centre Core Laboratories, Monash University, Australia) using a Picopure RNA isolation kit (Bio-strategy, Victoria, Australia). PCR for endogenous stem cell marker genes was performed using platinum TaqDNA polymerase (Invitrogen) and a SuperScript III first-Strand Synthesis system (Invitrogen), according to the manufacturer's instructions, relative to a β-actin housekeeping gene. Quantitative PCR (qPCR) for mesangial cell and stem cell markers in NHMCs, iPS cells and hES (stem cell markers only) was performed using a Platinum SuperMix-UDG (Invitrogen) with primers listed in Supplementary Figure 2. Transgene-specific PCR primers allowed for analysis of the quantitative expression of retrovirally expressed transgenes in iPS cells (passage 4) and NHMCS at 6 d following retroviral induction using a Platinum SYBR Green qPCR superMix-UDG (Invitrogen) and published primer sequences.16
Karyotype analysis was assessed in iPS cells at passage 5 (Southern Cross Pathology, Clayton, Australia). DNA was extracted using a DNase blood and Tissue Kit (Qiagen, CA, USA). Short tandem repeats-based DNA profiling was used for fingerprinting analysis to verify the genetic source of the iPS to their parent mesangial cells. An ABI Prism 3100 DNA sequencer was used with Genescan software (Applied Biosystems).
Teratoma Assay
Xenografts of undifferentiated mesangial cell-derived iPS colonies at passage 3 were transplanted under the kidney capsule of immune-compromised NOD-SCID mice (n = 3 animals). Teratoma formation was assessed after 8 wk in hematoxylin and eosin-stained paraffin sections.
DISCLOSURES
None.
Supplementary Material
Acknowledgments
This project was supported from grant funding from the Australian Stem Cell Centre and the Alport Foundation, Australia. CA Bernard is a recipient of an Erdi Fellowship in Neurologic Diseases and funding from the Baker Foundation.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Induced Pluripotent Stem Cells from Human Kidney,” on pages 1179–1180.
Supplemental information for this article is available online at http://www.jasn.org/.
REFERENCES
- 1. Wiggins RC: The spectrum of podocytopathies: A unifying view of glomerular diseases. Kidney Int 71: 1205–1214, 2007 [DOI] [PubMed] [Google Scholar]
- 2. Kriz W: Progression of chronic renal failure in focal segmental glomerulosclerosis: Consequence of podocyte damage or of tubulointerstitial fibrosis? Pediatr Nephrol 18: 617–622, 2003 [DOI] [PubMed] [Google Scholar]
- 3. Ronconi E, Mazzinghi B, Sagrinati C, Angelotti ML, Ballerini L, Parente E, Romagnani P, Lazzeri E, Lasagni L: [The role of podocyte damage in the pathogenesis of glomerulosclerosis and possible repair mechanisms]. G Ital Nefrol 26: 660–669, 2009 [PubMed] [Google Scholar]
- 4. Abbate M, Zoja C, Remuzzi G: How does proteinuria cause progressive renal damage? J Am Soc Nephrol 17: 2974–2984, 2006 [DOI] [PubMed] [Google Scholar]
- 5. Mundel P, Shankland SJ: Podocyte biology and response to injury. J Am Soc Nephrol 13: 3005–3015, 2002 [DOI] [PubMed] [Google Scholar]
- 6. Humphreys BD, Bonventre JV: The contribution of adult stem cells to renal repair. Nephrol Ther 3: 3–10, 2007 [DOI] [PubMed] [Google Scholar]
- 7. Humphreys BD, Valerius MT, Kobayashi A, Mugford JW, Soeung S, Duffield JS, McMahon AP, Bonventre JV: Intrinsic epithelial cells repair the kidney after injury. Cell Stem Cell 2: 284–291, 2008 [DOI] [PubMed] [Google Scholar]
- 8. Quaggin SE, Kreidberg JA: Development of the renal glomerulus: good neighbors and good fences. Development 135: 609–620, 2008 [DOI] [PubMed] [Google Scholar]
- 9. Shankland SJ: The podocyte's response to injury: Role in proteinuria and glomerulosclerosis. Kidney Int 69: 2131–2147, 2006 [DOI] [PubMed] [Google Scholar]
- 10. Little MH, Bertram JF: Is there such a thing as a renal stem cell? J Am Soc Nephrol 20: 2112–2117, 2009 [DOI] [PubMed] [Google Scholar]
- 11. Ronconi E, Sagrinati C, Angelotti ML, Lazzeri E, Mazzinghi B, Ballerini L, Parente E, Becherucci F, Gacci M, Carini M, Maggi E, Serio M, Vannelli GB, Lasagni L, Romagnani S, Romagnani P: Regeneration of glomerular podocytes by human renal progenitors. J Am Soc Nephrol 20: 322–332, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schlondorff D: The glomerular mesangial cell: An expanding role for a specialized pericyte. FASEB J 1: 272–281, 1987 [DOI] [PubMed] [Google Scholar]
- 13. Takahashi K, Yamanaka S: Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126: 663–676, 2006 [DOI] [PubMed] [Google Scholar]
- 14. Nishikawa S, Goldstein RA, Nierras CR: The promise of human induced pluripotent stem cells for research and therapy. Nat Rev Mol Cell Biol 9: 725–729, 2008 [DOI] [PubMed] [Google Scholar]
- 15. Park IH, Zhao R, West JA, Yabuuchi A, Huo H, Ince TA, Lerou PH, Lensch MW, Daley GQ: Reprogramming of human somatic cells to pluripotency with defined factors. Nature 451: 141–146, 2008 [DOI] [PubMed] [Google Scholar]
- 16. Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, Yamanaka S: Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131: 861–872, 2007 [DOI] [PubMed] [Google Scholar]
- 17. Park IH, Arora N, Huo H, Maherali N, Ahfeldt T, Shimamura A, Lensch MW, Cowan C, Hochedlinger K, Daley GQ: Disease-specific induced pluripotent stem cells. Cell 134: 877–886, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dimos JT, Rodolfa KT, Niakan KK, Weisenthal LM, Mitsumoto H, Chung W, Croft GF, Saphier G, Leibel R, Goland R, Wichterle H, Henderson CE, Eggan K: Induced pluripotent stem cells generated from patients with ALS can be differentiated into motor neurons. Science 321: 1218–1221, 2008 [DOI] [PubMed] [Google Scholar]
- 19. Carvajal-Vergara X, Sevilla A, D'Souza SL, Ang YS, Schaniel C, Lee DF, Yang L, Kaplan AD, Adler ED, Rozov R, Ge Y, Cohen N, Edelmann LJ, Chang B, Waghray A, Su J, Pardo S, Lichtenbelt KD, Tartaglia M, Gelb BD, Lemischka IR: Patient-specific induced pluripotent stem-cell-derived models of LEOPARD syndrome. Nature 465: 808–812, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Agarwal S, Loh YH, McLoughlin EM, Huang J, Park IH, Miller JD, Huo H, Okuka M, Dos Reis RM, Loewer S, Ng HH, Keefe DL, Goldman FD, Klingelhutz AJ, Liu L, Daley GQ: Telomere elongation in induced pluripotent stem cells from dyskeratosis congenita patients. Nature 464: 292–296, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Inagi R, Nangaku M, Miyata T, Kurokawa K: Mesangial cell-predominant functional gene, megsin. Clin Exp Nephrol 7: 87–92, 2003 [DOI] [PubMed] [Google Scholar]
- 22. Park IH, Lerou PH, Zhao R, Huo H, Daley GQ: Generation of human-induced pluripotent stem cells. Nat Protoc 3: 1180–1186, 2008 [DOI] [PubMed] [Google Scholar]
- 23. Harris PC, Torres VE: Polycystic kidney disease. Annu Rev Med 60: 321–337, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Torres VE, Harris PC: Autosomal dominant polycystic kidney disease: The last 3 years. Kidney Int 76: 149–168, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hudson BG, Tryggvason K, Sundaramoorthy M, Neilson EG: Alport's syndrome, Goodpasture's syndrome, and type IV collagen. N Engl J Med 348: 2543–2556, 2003 [DOI] [PubMed] [Google Scholar]
- 26. Osafune K: In vitro regeneration of kidney from pluripotent stem cells. Exp Cell Res 316: 2571–2577, 2010 [DOI] [PubMed] [Google Scholar]
- 27. Yang J, Cai J, Zhang Y, Wang X, Li W, Xu J, Li F, Guo X, Deng K, Zhong M, Chen Y, Lai L, Pei D, Esteban MA: Induced pluripotent stem cells can be used to model the genomic imprinting disorder Prader-Willi syndrome. J Biol Chem 285: 40303–40311, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim K, Doi A, Wen B, Ng K, Zhao R, Cahan P, Kim J, Aryee MJ, Ji H, Ehrlich LI, Yabuuchi A, Takeuchi A, Cunniff KC, Hongguang H, McKinney-Freeman S, Naveiras O, Yoon TJ, Irizarry RA, Jung N, Seita J, Hanna J, Murakami P, Jaenisch R, Weissleder R, Orkin SH, Weissman IL, Feinberg AP, Daley GQ: Epigenetic memory in induced pluripotent stem cells. Nature 467: 285–290, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Polo JM, Liu S, Figueroa ME, Kulalert W, Eminli S, Tan KY, Apostolou E, Stadtfeld M, Li Y, Shioda T, Natesan S, Wagers AJ, Melnick A, Evans T, Hochedlinger K: Cell type of origin influences the molecular and functional properties of mouse induced pluripotent stem cells. Nat Biotechnol 28: 848–855, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lin SA, Kolle G, Grimmond SM, Zhou Q, Doust E, Little MH, Aronow B, Ricardo SD, Pera MF, Bertram JF, Laslett AL: Subfractionation of differentiating human embryonic stem cell populations allows the isolation of a mesodermal population enriched for intermediate mesoderm and putative renal progenitors. Stem Cells Dev 19: 1637–1648, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Raya A, Rodriguez-Piza I, Guenechea G, Vassena R, Navarro S, Barrero MJ, Consiglio A, Castella M, Rio P, Sleep E, Gonzalez F, Tiscornia G, Garreta E, Aasen T, Veiga A, Verma IM, Surralles J, Bueren J, Izpisua Belmonte JC: Disease-corrected haematopoietic progenitors from Fanconi anaemia induced pluripotent stem cells. Nature 460: 53–59, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.