Abstract
Allopurinol ameliorates endothelial dysfunction and arterial stiffness among patients without chronic kidney disease (CKD), but it is unknown if it has similar effects among patients with CKD. Furthermore, because arterial stiffness increases left ventricular afterload, any allopurinol-induced improvement in arterial compliance might also regress left ventricular hypertrophy (LVH). We conducted a randomized, double-blind, placebo-controlled, parallel-group study in patients with stage 3 CKD and LVH. We randomly assigned 67 subjects to allopurinol at 300 mg/d or placebo for 9 months; 53 patients completed the study. We measured left ventricular mass index (LVMI) with cardiac magnetic resonance imaging (MRI), assessed endothelial function by flow-mediated dilation (FMD) of the brachial artery, and evaluated central arterial stiffness by pulse-wave analysis. Allopurinol significantly reduced LVH (P = 0.036), improved endothelial function (P = 0.009), and improved the central augmentation index (P = 0.015). This study demonstrates that allopurinol can regress left ventricular mass and improve endothelial function among patients with CKD. Because LVH and endothelial dysfunction associate with prognosis, these results call for further trials to examine whether allopurinol reduces cardiovascular events in patients with CKD and LVH.
Patients with chronic kidney disease (CKD) have approximately 20 times the mortality risk of the general population, and they mainly die from cardiovascular-related deaths.1 However treatments that reduce cardiovascular events in non-CKD patients do not always do so in CKD; for example, statins alone do not always reduce cardiovascular events in severe CKD.2–4 This implies that one cannot necessarily extrapolate clinical trial results from non-CKD patients to CKD patients and that highly novel approaches might be required to reduce cardiovascular events in CKD patients.
In non-CKD patients, allopurinol has consistently been found to improve endothelial/vascular function and arterial wave reflection.5–7 However, no data exist as to whether it does the same in CKD patients. Our first aim was therefore to see if allopurinol improved endothelial/vascular function in CKD patients because such an effect might imply fewer atherothrombotic events in the future.
However, another major adverse cardiovascular consequence of CKD is left ventricular hypertrophy (LVH). LVH is highly prevalent in CKD8,9 and is a well known independent predictor of cardiovascular mortality. Indeed after age, LVH is claimed to be the strongest independent predictor of cardiovascular events, cardiovascular death, and total mortality.10 Conversely, LVH regression has been shown to deliver prognostic benefit independent of BP changes.11,12 Therefore, novel ways to regress LVH independent of BP could be a promising way to reduce cardiovascular events/mortality in CKD. Allopurinol could be such a novel therapy against LVH.
In fact, there are two good reasons to think that allopurinol might reduce LVH. The first reason is that left ventricular afterload is the main determinant of left ventricular mass; hence, treatments that reduce left ventricular afterload by improving arterial compliance and arterial wave reflection might also reduce LVH (even if they do not reduce BP itself). Thus, if allopurinol does improve endothelial function and/or arterial wave reflection in CKD, then in theory it might also regress LVH. The second reason for thinking this might be the case is that allopurinol does indeed regress LVH in two different animal models.13,14
Therefore, in this study our main aim was to see if allopurinol, a xanthine oxidase (XO) inhibitor, is able to regress left ventricular mass because no human data exist yet for any population that show that allopurinol can reduce LVH. Our other aim was to see if allopurinol reduces endothelial dysfunction in patients with CKD.
RESULTS
A total of 67 Caucasian patients who met the criteria were included for the study, and 53 (allopurinol, n = 27; placebo, n = 26) completed the study. There were no significant differences between both groups with respect to demographic or baseline characteristics, apart from the diastolic BP (DBP). Mean left ventricular mass, estimated GFR, and uric acid level were also similar at baseline. Patient disposition is summarized in Table 1.
Table 1.
Baseline characteristics
| Characteristic | Allopurinol at 300 mg (n = 27) | Placebo (n = 26) | P |
|---|---|---|---|
| Gender | |||
| Male (%) | 16 (59%) | 12 (46%) | 0.139 |
| Age, years | 70.6 ± 6.9 | 73.7 ± 5.3 | 0.070 |
| Body surface area, g/m2 | 1.90 ± 0.17 | 1.91 ± 0.23 | 0.954 |
| Blood pressure, mmHg | |||
| SBP | 139 ± 14 | 145 ± 18 | 0.164 |
| DBP | 70 ± 8 | 75 ± 8 | 0.036a |
| Causes of CKD | |||
| glomerulonephritis | 4 | 5 | |
| diabetic nephropathy | 5 | 1 | |
| vascular/hypertension | 11 | 12 | |
| chronic pyelonephritis | 0 | 2 | |
| others | 2 | 1 | |
| unknown | 5 | 7 | |
| Estimated GFR, ml/min per 1.73 m2 | 44 ± 11 | 46 ± 9 | 0.427 |
| Uric acid, mmol/L | 0.44 ± 0.09 | 0.42 ± 0.08 | 0.575 |
| Hemoglobin, g/dl | 13.1 ± 1.1 | 13.4 ± 1.5 | 0.375 |
| Glucose, mmol/L | 6.4 ± 3.5 | 5.3 ± 0.8 | 0.121 |
| UPCR, mg/mmol | 49.0 ± 115.5 | 26.1 ± 30.5 | 0.333 |
| Calcium, mmol/L | 2.37 ± 0.10 | 2.35 ± 0.84 | 0.526 |
| Phosphate, mmol/L | 1.17 ± 0.15 | 1.11 ± 0.18 | 0.218 |
| Parathyroid hormone, pmol/L | 8.39 ± 4.63 | 8.33 ± 5.17 | 0.961 |
| Total cholesterol, mmol/L | 4.22 ± 0.81 | 4.45 ± 1.13 | 0.393 |
| BNP, pg/ml | 161 ± 250 | 171 ± 236 | 0.884 |
| Cystatin C, ng/ml | 1676 ± 558 | 1508 ± 406 | 0.216 |
| Oxidized LDL | 30.85 ± 8.67 | 31.26 ± 9.03 | 0.867 |
| Smoking status | |||
| nonsmoker | 16 | 15 | 0.118 |
| active | 4 | 3 | |
| ex-smoker | 7 | 7 | |
| ACEI/ARB (%) | 21 (78%) | 18 (69%) | 0.192 |
| Diuretics (%) | 12 (44%) | 12 (46%) | 0.215 |
| Calcium channel blocker (%) | 13 (48%) | 17 (65%) | 0.101 |
| Beta-blocker (%) | 13 (48%) | 12 (46%) | 0.214 |
| Statin | 21 (78%) | 20 (77%) | 0.255 |
| LVMI, g/m2 (MRI) | 61.6 ± 13.7 | 62.1 ± 15.4 | 0.900 |
| EDV, ml | 124.9 ± 30.1 | 119.8 ± 34.4 | 0.564 |
| FMD, % | 5.02 ± 1.91 | 4.93 ± 2.50 | 0.885 |
| AIx, % | 18.5 ± 10.2 | 17.2 ± 6.3 | 0.585 |
| PWV, m/s | 7.7 ± 1.3 | 8.2 ± 1.2 | 0.194 |
ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker.
aP < 0.05.
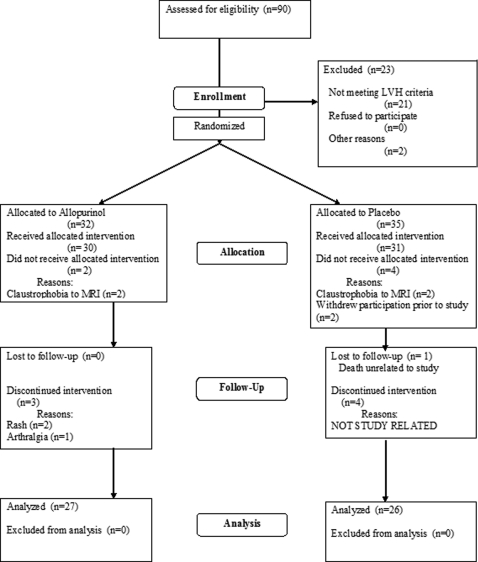
Fourteen patients withdrew during the course of the study for various reasons as set out in Figure 1. The three patients who withdrew because of rash and arthralgia on allopurinol developed these symptoms when the dose was increased to 300 mg once per day. Apart from these three subjects, the withdrawals were unrelated to the therapy and had more to do with the study demands, such as MRI (claustrophobia), the lengthy nature of the trial, and the complex end point measurements.
Figure 1.
Consort diagram of study, with a total of 67 patients randomized, but after 14 withdrawals, only 53 patients completed the study and had their data analyzed.
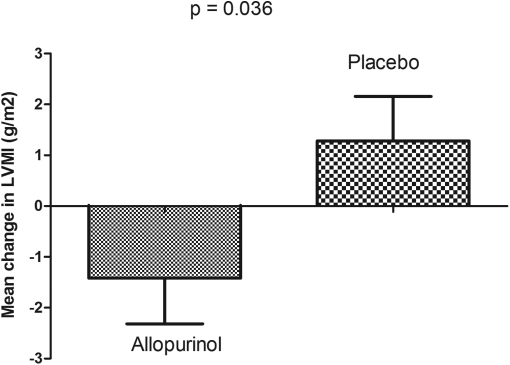
Treatment with allopurinol resulted in a decrease in left ventricular mass index (LVMI) (ΔLVMI in active group −1.42 ± 4.67 g/m2 compared with the placebo at +1.28 ± 4.45 g/m2 [P = 0.036], Figure 2). After correction for demographic factors that should most influence LVMI changes (age, systolic BP [SBP], DBP, and baseline LVMI), the result was little altered and remained significant (P = 0.030). The end-diastolic volume (EDV) also showed a corresponding fall in volume in the allopurinol group, although it did not reach statistical significance, whereby EDV change was −9.64 ± 16.10 ml with allopurinol compared with placebo at −1.65 ± 16.88 ml (P = 0.084). End-systolic volume and ejection fraction (EF) did not change with treatment of allopurinol.
Figure 2.
Significant regression of LVMI in the allopurinol group compared to the placebo group after 9 months, as measured by cardiac MRI.
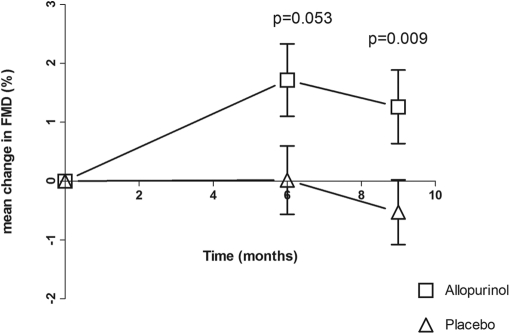
Baseline flow-mediated dilation (FMD) was found to be similar between both groups. Overall, the treatment with allopurinol was found to significantly improve FMD, especially at month 9 (Table 2 and Figure 3). In fact, FMD was virtually identical between baseline and 6 months in the placebo group. There was no difference in response to glyceryl trinitrate between both treatment arms (Table 2). These results imply that allopurinol's vascular effect was endothelial dependent and not endothelial independent to any extent.
Table 2.
Comparison of the change in LVMI, FMD response to hyperemia, FMD response to GTN, AIx, and PWV by treatment groups
| Allopurinol | Placebo | P | |
|---|---|---|---|
| Change in LVMI at 9 months (g/m2) | −1.42 (±4.67) | +1.28 (±4.45) | 0.036a |
| Change in FMD response to hyperemia at 6 months (%) | +1.72 (±2.95) | −0.03 (±2.84) | 0.053 |
| Change in FMD response to hyperemia at 9 months (%) | +1.26 (±3.06) | −1.05 (±2.84) | 0.009b |
| Change in FMD response to GTN at 6 months (%) | −0.29 (±6.16) | −1.91 (±8.38) | 0.729 |
| Change in FMD response to GTN at 9 months (%) | −0.50 (±5.87) | −1.06 (±6.65) | 0.918 |
| Change in AIx at 6 months (%) | −0.04 (±7.19) | +3.41 (±5.37) | 0.048a |
| Change in AIx at 9 months (%) | −4.70 (±9.30) | +0.77 (±6.06) | 0.015a |
| Change in PWV at 6 months (m/s) | −0.06 (±1.52) | −0.56 (±1.52) | 0.141 |
| Change in PWV at 9 months (m/s) | −0.39 (±1.13) | +0.20 (±1.28) | 0.086 |
GTN, glyceryl trinitrate.
aP < 0.05;
bP < 0.01.
Figure 3.
Significant improvement seen in FMD in the allopurinol group (especially after 9 months), compared to placebo. Data is mean ± SEM.
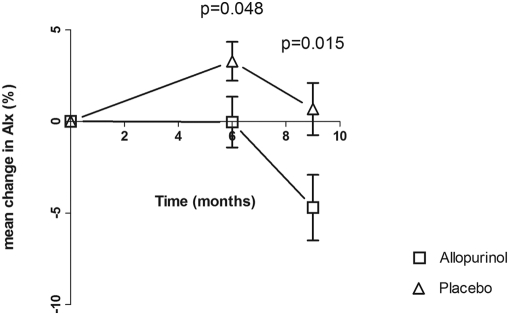
Similarly, treatment with allopurinol also improved the augmentation index (AIx), with a marked difference seen at month 9 (Table 2 and Figure 4). AIx worsened significantly at month 6 in the placebo group, and this effect was negated by allopurinol. As for pulse wave velocity (PWV), although no difference was noted at month 6, a trend toward improvement on allopurinol was seen at month 9 (Table 2).
Figure 4.
Significant improvement seen in AIx in the allopurinol group (especially after 9 months), compared to placebo. Data is mean ± SEM.
There were no correlations found between urate levels (either its baseline or its change) and the changes seen in LVMI, FMD, AIx, and PWV (data not shown). However, the change seen in LVMI did correlate significantly with the change in FMD, the change in PWV, the change in EDV, and even the change in urine protein-creatinine ratio (UPCR) (Table 3). When predictors of left ventricular mass change were subjected to multivariate analyses (using the linear regression model), ΔFMD (β coefficient −0.374, P = 0.003) and ΔUPCR (β coefficient 0.475, P = 0.0003) emerged as independent predictors. There was also a significant correlation between baseline LVMI and its change over 9 months (R = −0.426, P = 0.001).
Table 3.
Comparison of the change in FMD, AIx, PWV, EDV, and UPCR with change in LVMI
| Change in LVMI | |
|---|---|
| Change in FMD | R = −0.378 |
| P = 0.008b | |
| Change in AIx | R = 0.120 |
| P = 0.394 | |
| Change in PWV | R = 0.291 |
| P = 0.038a | |
| Change in EDV | R = 0.274 |
| P = 0.048a | |
| Change in UPCR | R = 0.465 |
| P = 0.0004b |
aP < 0.05;
bP < 0.01.
All of the subjects' renal function remained stable throughout the whole study period. SBP and DBP fell slightly in both groups, as is common over repeated measurement, but their change over 6 months and over 9 months was no different between groups (Table 4). However, there was a greater tendency for antihypertensives to be stopped in the allopurinol group (Table 4). Other parameters including hemoglobin, UPCR, bone metabolism, total cholesterol, glucose, hemoglobin A1C, and cystatin C remain unchanged during these 9 months (Table 4). However, despite an improvement in left ventricular mass and EDV, brain natriuretic peptide (BNP) did not change (possibly because the persistent renal dysfunction influences BNP clearance so much as to eclipse any small change in BNP production). Oxidized LDL increased in placebo but fell after 9 months of allopurinol, although this difference fell short of significance.
Table 4.
Comparison of changes in parameters between treatment groups at 9 months
| Allopurinol 300 mg (n = 27) | Placebo (n = 26) | P | |
|---|---|---|---|
| ΔBP, mmHg | |||
| SBP at 9 months | −6.9 ± 14.4 | −5.1 ± 15.1 | 0.644 |
| DBP at 9 months | −3.3 ± 8.6 | −2.5 ± 9.1 | 0.741 |
| SBP at 6 months | −4.9 ± 17.64 | −8.73 ± 21.36 | 0.701 |
| DBP at 6 months | −1.85 ± 11.64 | −4.15 ± 12.95 | 0.498 |
| ΔEstimated GFR, ml/min per 1.73 m2 | +0.2 ± 6.9 | +0.2 ± 5.5 | 0.997 |
| ΔUric acid, mmol/L | −0.18 ± 0.08 | +0.02 ± 0.06 | <0.00a |
| ΔUPCR, mg/mmol | −21.4 ± 94.0 | −5.2 ± 21.2 | 0.394 |
| ΔCystatin C, ng/ml | +71 ± 301 | +86 ± 526 | 0.898 |
| ΔGlucose, mmol/L | −0.80 ± 3.22 | −0.03 ± 0.80 | 0.240 |
| ΔHemoglobin A1C, % | −0.07 ± 0.58 | +0.08 ± 0.16 | 0.484 |
| ΔOxidized LDL | −0.44 ± 5.64 | +1.64 ± 5.47 | 0.180 |
| Medication change | |||
| antihypertensives commenced (%) | 2 (7%) | 5 (19%) | 0.150 |
| antihypertensives stopped (%) | 5 (18%) | 2 (8%) | 0.170 |
| Adverse events | 1 (4%) | 0 (0%) | 0.258 |
| Serious adverse eventsb | 3 (11%) | 3 (12%) |
aP < 0.001.
bSerious adverse events included hospitalizations for exacerbation of chronic obstructive pulmonary disease, angina, vasovagal episode, collapse secondary to severe bradycardia, stroke, elective orthopedic procedure.
Overall, allopurinol at 300 mg once daily was well tolerated in CKD stage 3 with no withdrawal of subjects due to a deterioration in renal function. Allopurinol at 300 mg once daily also reduced baseline urate level by 41% from 0.44 ± 0.09 to 0.26 ± 0.85 mmol/L after 9 months. During the course of the study period, several subjects from both groups had some minor changes made to their medications for necessary clinical reasons, including commencement and stopping of their antihypertensives, with no significant difference between both groups (Table 4). Because the allopurinol group had more discontinuations of antihypertensives and less starting of them, there appears to be a BP effect of allopurinol, although it was NS. Furthermore, we found no correlation between changes seen in SBP and DBP (at month 6 and month 9) with the change seen in LVMI. Only one patient was on erythropoietin, and the dose of this remained unchanged during the 9 months. Overall, the event rates of reported adverse events and serious adverse events were small, with no significant differences between both groups (Table 4).
DISCUSSION
This is the first study to demonstrate that left ventricular mass regression can be achieved in humans with a treatment that does not primarily act by reducing BP (i.e., allopurinol). Our study has also shown for the first time that allopurinol can improve endothelial dysfunction and AIx in patients with CKD.
LVH affects up to 75% of ESRD patients8 and up to 50% in milder CKD.9 The presence of LVH conferred almost 3 times the risk for total mortality and cardiovascular mortality in ESRD patients.15 The reason why LVH is such a strong cardiovascular risk factor is probably because it can predate so many different cardiovascular sequelae (i.e., LVH is arrhythmogenic; LVH reduces coronary perfusion reserve; LVH causes diastolic heart failure; and LVH leads to left atrium dilation, atrial fibrillation, and embolic stroke). We also know from the Losartan Intervention For Endpoint reduction (LIFE) study and others that LVH regression per se reduces sudden death,16 atrial fibrillation,17 heart failure,18 and stroke19 and that it does so independently of BP changes. Indeed, Schillaci et al.20 recently said “LVH stands out as the only available marker where treatment-induced regression has been unequivocally associated to a better prognosis, even after accounting for treatment-induced BP reduction.” This background information underscores the possible importance of our demonstration that allopurinol can regress left ventricular mass in CKD, although the LIFE study patients may have had higher left ventricular mass at baseline than our patients, and we cannot be sure that LVH regression in our range will deliver clinical benefits.
With respect to previous therapies in CKD, several recent studies have suggested that statins alone may not reduce cardiovascular events in hemodialysis patients.2–4 Indeed, it is thought that cardiovascular deaths in severe CKD/hemodialysis patients may be more related to LVH-mediated events, such as arrhythmic sudden deaths and heart failure.21 On the other hand, statins alone are effective in mild CKD, implying that the main mediator of cardiovascular deaths in this group might be coronary artery disease. If the above hypotheses are correct, it is encouraging that in this study allopurinol was able to improve LVH and vascular dysfunction because each of these factors/surrogates may represent the main cardiovascular culprits at either end of the disease spectrum of CKD.
The mechanism whereby allopurinol regressed left ventricular mass here is likely to be related to its vascular effects. This is because left ventricular afterload is reflected to a large extent by peripheral arterial compliance and arterial wave reflection, as indicated by AIx. The fact that allopurinol improved FMD and AIx at 9 months strengthens the likelihood that allopurinol regressed left ventricular mass because of less left ventricular afterload consequent upon better vascular compliance and reduced arterial wave reflection. This hypothesis is strengthened further by the strong correlation (P = 0.008) seen between the change in LVMI and the change in FMD. This correlation was still observed although the absolute changes seen in LVMI and FMD were both small (5 to 25% of their respective baseline values). It is also possible that changes in uric acid could contribute to our results.
The small increase in LVMI in the placebo group is normally found with aging, even with only 9 months of aging. The magnitude of this was very similar in our previous study.22 Indeed, our absolute LVMI values presented here are also similar to our previous cardiac MRI (CMR) study of echo LVH patients.22 Therefore it appears that allopurinol is able to prevent and even reverse the normal increase in LVMI associated with aging. It should be noted that the CMR-derived LVMI is lower than the enrollment criteria transthoracic echocardiogram-derived LVMI of >115 g/m2. This is a universal finding due to the very different methods by which left ventricular mass is calculated using echo and MRI and has been noted before by us and others.22,23 Echocardiography consistently overestimates left ventricular mass because it is a two-dimensional measure that assumes a cubic shape of the left ventricle, whereas MRI is a three-dimensional measure with fewer geometric assumptions.
Our study design was based on previous work in non-CKD patients in which we found a strong dose-response curve for allopurinol in that allopurinol improved endothelial function by a much greater degree when given at 600 mg/d as opposed to 300 mg/d.24 Other previous works had also implied that higher doses were much better than lower doses.25,26 However, we did not feel that there was enough safety data for us to give 600 mg/d of allopurinol to these CKD patients and therefore in this “proof-of-concept study” we reduced the dose to 300 mg/d. We did achieve a 41% reduction in plasma urate here in CKD patients, which is a substantial decrease, although not as much as the 60% decrease seen with 600 mg/d in non-CKD patients. Nevertheless, one consequence of using a moderately high dose of allopurinol in these CKD patients was that for safety reasons we did not want to prolong the treatment period for any longer than was necessary. Therefore to err on the side of caution, we used only a 9-month treatment period.
Although it was statistically significant, the effect size of allopurinol on left ventricular mass was small. After 9 months, the placebo-corrected change induced by allopurinol in LVMI was nearly 5% of its baseline value. However, one might expect this to be greater with a longer duration of therapy given that the vascular changes became more significant at 9 months than at 6 months. It is also worth emphasizing that left ventricular mass is not a parameter that changes to a huge extent with any single treatment because reduced left ventricular mass can produce increased wall stress if it is too great. In fact, LVMI is quite similar to BP, in which any one antihypertensive drug only reduces the BP by a magnitude of 5% to 7% and in which too big of a fall could produce unwanted symptoms. Furthermore, recent evidence has shown that a significant proportion of CKD patients with LVH have more of a diffuse myocardial fibrosis-type pattern,27 which suggests that regression of left ventricular mass in the CKD population may be more difficult and hence any degree of regression or attenuation of progression in LVH in CKD may be particularly noteworthy. A 5% reduction in absolute LVMI could still be important because a 10% reduction in left ventricular mass in ESRD patients, achieved by multiple interventions, resulted in a 28% risk reduction for cardiovascular deaths.28 Therefore, in our study, it is possible to speculate that a 5% reduction in absolute LVMI might translate into an approximate 14% relative risk reduction in cardiovascular events. Of course, baseline LVMI is higher in ESRD, which means that this speculation might be overoptimistic; although, on the other hand, LVMI is known to be a graded risk factor and not just a risk factor above an arbitrary threshold value.
Despite the small effect size on left ventricular mass, two major factors do increase confidence in our LVMI results. First, the significant correlation between the change in LVMI and the changes in FMD, PWV, EDV, and UPCR would be unlikely if the LVMI changes were chance, especially because these correlations underpin a credible mechanism linking afterload reduction with LVH reduction. Second, our finding in humans that allopurinol regressed left ventricular mass is consistent with two experimental studies. For example, Laakso et al.13 found that allopurinol prevented cardiac hypertrophy in rats with negligible effects on BP. Furthermore, XO inhibition with febuxostat was shown to attenuate systolic overload-induced LVH and dysfunction in mice.14
These data suggest many future studies would now be worthwhile. In addition to more LVH regression studies with larger doses, longer time frames, and possibly even severer CKD patients, future studies may now be warranted to see if allopurinol will actually reduce cardiovascular events and mortality in CKD. In fact, one recent, small study has found a 71% reduction in cardiovascular events with allopurinol in CKD.29
The main limitation of this study is that the effect of volume control is unclear because volume status was not formally assessed. On the other hand, crude measures of volume status such as weight, BP, and BNP were stable in both groups. Another limitation could be that 7% of patients had a rash with allopurinol, which might limit its widespread use.
In conclusion, allopurinol has been shown for the first time here to be able to regress LVH in humans. Allopurinol also improves several different measures of endothelial/vascular dysfunction in CKD. Furthermore, it had the above beneficial effects without having any apparent adverse events in these CKD patients. These results justify future work to explore the full therapeutic potential of regular allopurinol in CKD.
CONCISE METHODS
Study Population
Sixty-seven male and female adult subjects who were diagnosed with LVH by echocardiography (American Society of Echocardiography criteria LVMI ≥ 115 g/m2 for men and ≥ 95 g/m2 for women) and who were known to have CKD stage 3 (estimated GFR between 30 and 60 ml/min per 1.73 m2) were recruited from the General Nephrology clinics and Cardiovascular Risk Clinic for the study during the period of January 2008 to December 2008. The echocardiogram diagnosing LVH was performed within 12 months of study commencement. Patients were excluded if any of the following criteria were present: already on allopurinol; active gout; known left ventricular failure with EF < 45%; severe hepatic disease; usual contraindications to MRI; on current immunosuppressive therapy, warfarin, theophyllin, chlorpropamide, or 6-mercaptopurine; metastatic malignancy or other life-threatening diseases; pregnant or lactating women; and unable to give informed consent.
Study Design
This was a 9-month, placebo-controlled, randomized, double-blind, parallel-group study. After baseline assessments and investigations, patients were then randomly assigned to receive an allopurinol 100-mg capsule once daily or a placebo capsule once daily for 2 weeks (Figure 1). If this was tolerated, this was increased to an allopurinol 300-mg capsule once daily or a placebo capsule once daily. Baseline blood samples were taken for full blood count, renal function, liver function, random blood glucose, hemoglobin A1C, lipids, calcium, phosphate, parathyroid hormone, urate, BNP, oxidized LDL, and cystatin C, and these were repeated at 6 and 9 months. A spot urine sample was sent to the laboratory for calculation of UPCR and repeated at month 6 and month 9. Subjects were followed at baseline, week 2, week 6, month 6, and finally at month 9 with close monitoring of their full blood count and renal function. Office BP was measured at three different intervals at each visit.
Discontinuation of treatment was scheduled for those intolerant of treatment, those with an increase of >20% in serum creatinine from baseline, and for those who voluntarily withdrew from study. During the trial study, patients were allowed to continue all of their concomitant treatment. All patients provided written informed consent, and the Tayside Committee on Medical Research Ethics approved the study. The trial was carried out at Ninewells Hospital and Medical School. This study has been registered with clinicaltrials.gov with the identifier of NCT00688480 and with the International Standard Randomised Controlled Trial Number register with the identifier ISRCTN45773760.
CMR Methods
Baseline and repeat CMR examinations at month 9 were performed on a 1.5-T Magnetom Avanto scanner (Siemens, Erlangen, Germany). Serial contiguous short-axis cines were acquired from the vertical long axis and horizontal long axis of the left ventricle (electrocardiogram gated, steady-state free precession imaging [true fast imaging with steady-state precession], with the short-axis imaging parameters being a repetition time of 2.5 ms, echo time of 1.1 ms, flip angle of 60°, and slice thickness 6 mm). Analysis was performed offline (Argus Software, Siemens) by a single blinded observer (S.J.G.) for the assessment of ventricular volumes (EDV, end-systolic volume, stroke volume), EF, and left ventricular mass. The reproducibility of the left ventricular mass assessment using MRI was derived by a single observer from the above repeated measurements, and a single time-point (baseline) test-retest intraobserver coefficient of variation of 2.0% was achieved.
FMD
FMD on the brachial artery was performed on three visits (baseline, month 6, and month 9) using a Philips iE33 ultrasound machine (Phillips Medical Systems, United Kingdom) according to the guidelines set by the International Brachial Artery Reactivity Task Force.30 The brachial artery was longitudinally imaged above the elbow using an 11.3-MHz probe. The image was recorded for 2 minutes, followed by induction of forearm ischemia by inflating a cuff below the elbow to 200 mmHg (or 50 mmHg above SBP, whichever was higher) for 5 minutes and deflating rapidly. The resulting reactive hyperemia was recorded for a further 2 minutes. After a rest period of 10 minutes, the procedure was repeated, with 0.4 mg of glyceryl trinitrate being administered sublingually to determine the endothelium-independent dilation. FMD was expressed as percent change in diameter relative to the baseline diameter at rest. Analyses of all FMDs were performed on the Brachial Analyzer version 5.0 software (Medical Imaging Applications, LLC) by a single trained investigator (M.P.K.) to avoid interobserver variability. This investigator was blind to allocated treatments. The intraobserver coefficient of variation is 5.2%, and the repeatability coefficient is 0.3 ± 1.4%.
Applanation Tonometry
Pulse wave analysis and PWV were determined by recording the radial waveforms and radial-carotid waveforms, respectively, at three visits (baseline, month 6, and month 9) using the Sphygmocor system. The central AIx was corrected to a heart rate of 75 beats/min. A single trained investigator (M.P.K.) who was blind to the allocated treatment performed the PWA and PWV.
Statistical Analysis
Statistical analysis was performed using SPSS version 16.0 (SPSS, Chicago, IL). Data are expressed as mean ± SD unless stated otherwise. One-way ANOVA or χ2 test was used to determine the significance of differences between both groups (normally distributed variables). Analysis of covariance was also performed using the month 9 value as the dependent variable and the baseline value treated as a covariate, along with age, SBP, and DBP, to account for differences in baseline measures of the primary and secondary outcomes. Pearson's correlation was performed for univariate analysis. A P value <0.05 was considered significant. Our original power calculations led us to aim to recruit 60 patients (to allow for 10% dropouts) to have at least 90% power at P < 0.05 to detect a 5-g/m2 change in LVMI and 80% power to detect a 2% change in FMD. Our predesignated primary end point was LVMI.
DISCLOSURES
The University of Dundee and A.D.S. have submitted a patent on the use of XO inhibitors to treat anginal chest pain. None of the other authors have any conflicts of interests to disclose.
Acknowledgments
We thank the British Heart Foundation for support and Dr. Gwen Kennedy, Mrs. Lesley McFarlane, and Dr. Val Godfrey for laboratory assays. Trial registration: ISRCTN45773760.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
REFERENCES
- 1. Foley RN, Parfrey PS, Sarnak MJ: Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis 32[5 Suppl 3]: S112–S119, 1998 [DOI] [PubMed] [Google Scholar]
- 2. Wanner C, Krane V, Marz W, Olschewski M, Mann JF, Ruf G, Ritz E: Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med 353: 238–248, 2005 [DOI] [PubMed] [Google Scholar]
- 3. Fellstrom BC, Jardine AG, Schmieder RE, Holdaas H, Bannister K, Beutler J, Chae DW, Chevaile A, Cobbe SM, Gronhagen-Riska C, De Lima JJ, Lins R, Mayer G, McMahon AW, Parving HH, Remuzzi G, Samuelsson O, Sonkodi S, Sci D, Suleymanlar G, Tsakiris D, Tesar V, Todorov V, Wiecek A, Wuthrich RP, Gottlow M, Johnsson E, Zannad F: Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med 360: 1395–1407, 2009 [DOI] [PubMed] [Google Scholar]
- 4. Sharp Collaborative Group: Study of Heart and Renal Protection (SHARP): Randomized trial to assess the effects of lowering low-density lipoprotein cholesterol among 9,438 patients with chronic kidney disease. Am Heart J 160: 785–794.e710, 2010 [DOI] [PubMed] [Google Scholar]
- 5. Butler R, Morris AD, Belch JJ, Hill A, Struthers AD: Allopurinol normalizes endothelial dysfunction in type 2 diabetics with mild hypertension. Hypertension 35: 746–751, 2000 [DOI] [PubMed] [Google Scholar]
- 6. Guthikonda S, Sinkey C, Barenz T, Haynes WG: Xanthine oxidase inhibition reverses endothelial dysfunction in heavy smokers. Circulation 107: 416–421, 2003 [DOI] [PubMed] [Google Scholar]
- 7. Cardillo C, Kilcoyne CM, Cannon RO, III, Quyyumi AA, Panza JA: Xanthine oxidase inhibition with oxypurinol improves endothelial vasodilator function in hypercholesterolemic but not in hypertensive patients. Hypertension 30: 57–63, 1997 [DOI] [PubMed] [Google Scholar]
- 8. Foley RN, Parfrey PS, Harnett JD, Kent GM, Martin CJ, Murray DC, Barre PE: Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int 47: 186–192, 1995 [DOI] [PubMed] [Google Scholar]
- 9. Paoletti E, Bellino D, Cassottana P, Rolla D, Cannella G: Left ventricular hypertrophy in nondiabetic predialysis CKD. Am J Kidney Dis 46: 320–327, 2005 [DOI] [PubMed] [Google Scholar]
- 10. Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP: Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 322: 1561–1566, 1990 [DOI] [PubMed] [Google Scholar]
- 11. Koren MJ, Ulin RJ, Koren AT, Laragh JH, Devereux RB: Left ventricular mass change during treatment and outcome in patients with essential hypertension. Am J Hypertens 15: 1021–1028, 2002 [DOI] [PubMed] [Google Scholar]
- 12. Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Gattobigio R, Zampi I, Reboldi G, Porcellati C: Prognostic significance of serial changes in left ventricular mass in essential hypertension. Circulation 97: 48–54, 1998 [DOI] [PubMed] [Google Scholar]
- 13. Laakso JT, Teravainen TL, Martelin E, Vaskonen T, Lapatto R: Renal xanthine oxidoreductase activity during development of hypertension in spontaneously hypertensive rats. J Hypertens 22: 1333–1340, 2004 [DOI] [PubMed] [Google Scholar]
- 14. Xu X, Hu X, Lu Z, Zhang P, Zhao L, Wessale JL, Bache RJ, Chen Y: Xanthine oxidase inhibition with febuxostat attenuates systolic overload-induced left ventricular hypertrophy and dysfunction in mice. J Card Fail 14: 746–753, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Silberberg JS, Barre PE, Prichard SS, Sniderman AD: Impact of left ventricular hypertrophy on survival in end-stage renal disease. Kidney Int 36: 286–290, 1989 [DOI] [PubMed] [Google Scholar]
- 16. Wachtell K, Okin PM, Olsen MH, Dahlof B, Devereux RB, Ibsen H, Kjeldsen SE, Lindholm LH, Nieminen MS, Thygesen K: Regression of electrocardiographic left ventricular hypertrophy during antihypertensive therapy and reduction in sudden cardiac death: The LIFE Study. Circulation 116: 700–705, 2007 [DOI] [PubMed] [Google Scholar]
- 17. Okin PM, Wachtell K, Devereux RB, Harris KE, Jern S, Kjeldsen SE, Julius S, Lindholm LH, Nieminen MS, Edelman JM, Hille DA, Dahlof B: Regression of electrocardiographic left ventricular hypertrophy and decreased incidence of new-onset atrial fibrillation in patients with hypertension. JAMA 296: 1242–1248, 2006 [DOI] [PubMed] [Google Scholar]
- 18. Okin PM, Devereux RB, Harris KE, Jern S, Kjeldsen SE, Julius S, Edelman JM, Dahlof B: Regression of electrocardiographic left ventricular hypertrophy is associated with less hospitalization for heart failure in hypertensive patients. Ann Intern Med 147: 311–319, 2007 [DOI] [PubMed] [Google Scholar]
- 19. Okin PM, Devereux RB, Jern S, Kjeldsen SE, Julius S, Nieminen MS, Snapinn S, Harris KE, Aurup P, Edelman JM, Wedel H, Lindholm LH, Dahlof B: Regression of electrocardiographic left ventricular hypertrophy during antihypertensive treatment and the prediction of major cardiovascular events. JAMA 292: 2343–2349, 2004 [DOI] [PubMed] [Google Scholar]
- 20. Schillaci G, Pirro M, Mannarino E: Left ventricular hypertrophy reversal and prevention of diabetes: Two birds with one stone? Hypertension 50: 851–853, 2007 [DOI] [PubMed] [Google Scholar]
- 21. Stewart GA, Gansevoort RT, Mark PB, Rooney E, McDonagh TA, Dargie HJ, Stuart R, Rodger C, Jardine AG: Electrocardiographic abnormalities and uremic cardiomyopathy. Kidney Int 67: 217–226, 2005 [DOI] [PubMed] [Google Scholar]
- 22. Simpson HJ, Gandy SJ, Houston JG, Rajendra NS, Davies JI, Struthers AD: Left ventricular hypertrophy: Reduction of blood pressure already in the normal range further regresses left ventricular mass. Heart 96: 148–152, 2009 [DOI] [PubMed] [Google Scholar]
- 23. Stewart GA, Foster J, Cowan M, Rooney E, McDonagh T, Dargie HJ, Rodger RS, Jardine AG: Echocardiography overestimates left ventricular mass in hemodialysis patients relative to magnetic resonance imaging. Kidney Int 56: 2248–2253, 1999 [DOI] [PubMed] [Google Scholar]
- 24. George J, Carr E, Davies J, Belch JJ, Struthers A: High-dose allopurinol improves endothelial function by profoundly reducing vascular oxidative stress and not by lowering uric acid. Circulation 114: 2508–2516, 2006 [DOI] [PubMed] [Google Scholar]
- 25. Struthers AD, Donnan PT, Lindsay P, McNaughton D, Broomhall J, MacDonald TM: Effect of allopurinol on mortality and hospitalisations in chronic heart failure: A retrospective cohort study. Heart 87: 229–234, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wei L, Fahey T, Struthers AD, MacDonald TM: Association between allopurinol and mortality in heart failure patients: A long-term follow-up study. Int J Clin Pract 63: 1327–1333, 2009 [DOI] [PubMed] [Google Scholar]
- 27. Mark PB, Johnston N, Groenning BA, Foster JE, Blyth KG, Martin TN, Steedman T, Dargie HJ, Jardine AG: Redefinition of uremic cardiomyopathy by contrast-enhanced cardiac magnetic resonance imaging. Kidney Int 69: 1839–1845, 2006 [DOI] [PubMed] [Google Scholar]
- 28. London GM, Pannier B, Guerin AP, Blacher J, Marchais SJ, Darne B, Metivier F, Adda H, Safar ME: Alterations of left ventricular hypertrophy in and survival of patients receiving hemodialysis: Follow-up of an interventional study. J Am Soc Nephrol 12: 2759–2767, 2001 [DOI] [PubMed] [Google Scholar]
- 29. Goicoechea M, de Vinuesa SG, Verdalles U, Ruiz-Caro C, Ampuero J, Rincon A, Arroyo D, Luno J: Effect of allopurinol in chronic kidney disease progression and cardiovascular risk. Clin J Am Soc Nephrol 5: 1388–1393, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, Vallance P, Vita J, Vogel R: Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 39: 257–265, 2002 [DOI] [PubMed] [Google Scholar]