Abstract
BACKGROUND
Cyclophosphamide and glucocorticoids have been the cornerstone of remission-induction therapy for severe antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis for 40 years. Uncontrolled studies suggest that rituximab is effective and may be safer than a cyclophosphamide-based regimen.
METHODS
We conducted a multicenter, randomized, double-blind, double-dummy, noninferiority trial of rituximab (375 mg per square meter of body-surface area per week for 4 weeks) as compared with cyclophosphamide (2 mg per kilogram of body weight per day) for remission induction. Glucocorticoids were tapered off; the primary end point was remission of disease without the use of prednisone at 6 months.
RESULTS
Nine centers enrolled 197 ANCA-positive patients with either Wegener’s granulomatosis or microscopic polyangiitis. Baseline disease activity, organ involvement, and the proportion of patients with relapsing disease were similar in the two treatment groups. Sixty-three patients in the rituximab group (64%) reached the primary end point, as compared with 52 patients in the control group (53%), a result that met the criterion for noninferiority (P<0.001). The rituximab-based regimen was more efficacious than the cyclophosphamide-based regimen for inducing remission of relapsing disease; 34 of 51 patients in the rituximab group (67%) as compared with 21 of 50 patients in the control group (42%) reached the primary end point (P = 0.01). Rituximab was also as effective as cyclophosphamide in the treatment of patients with major renal disease or alveolar hemorrhage. There were no significant differences between the treatment groups with respect to rates of adverse events.
CONCLUSIONS
Rituximab therapy was not inferior to daily cyclophosphamide treatment for induction of remission in severe ANCA-associated vasculitis and may be superior in relapsing disease. (Funded by the National Institutes of Allergy and Infectious Diseases, Genentech, and Biogen; ClinicalTrials.gov number, NCT00104299.)
Wegener’s granulomatosis and microscopic polyangiitis are classified as antineutrophil cytoplasmic antibody (ANCA)–associated vasculitides because most patients with generalized disease have antibodies against proteinase 3 or myeloperoxidase.1,2 The ANCA-associated vasculitides affect small-to-medium-size blood vessels, with a predilection for the respiratory tract and kidneys.3-6
Cyclophosphamide and glucocorticoids have been the standard therapy for remission induction for nearly four decades.7,8 This regimen transformed the usual treatment outcome of severe ANCA-associated vasculitis from death to a strong likelihood of disease control and temporary remission.3-5,9-11 However, not all patients have a remission with this combination of drugs, and those who do often have disease flares that require repeated treatment. Moreover, side effects of cyclophosphamide, including infertility, cytopenias, infections, bladder injury, and cancer, as well as the multiple adverse effects of lengthy courses of glucocorticoid treatment, are major causes of long-term disease and death.3-5,10-14
B lymphocytes play an important role in the pathogenesis of autoimmune diseases, including ANCA-associated vasculitis.15 In ANCA-associated vasculitis, the percentage of activated peripheral-blood B lymphocytes correlates with disease activity, and certain effects of cyclophosphamide on B lymphocytes are associated with treatment efficacy.16-19 Rituximab, an anti-CD20 monoclonal antibody, depletes B lymphocytes through a variety of mechanisms. In uncontrolled studies, rituximab has shown promise as a remission-induction agent in ANCA-associated vasculitis.20-23
We conducted the Rituximab in ANCA-Associated Vasculitis (RAVE) trial, a multicenter, randomized, double-blind, double-dummy, noninferiority trial to compare rituximab with standard cytotoxic therapy for the induction of complete remission by 6 months in patients with severe ANCA-associated vasculitis. We hypothesized that treatment with rituximab plus glucocorticoids would not be inferior to daily cyclophosphamide plus glucocorticoids for remission induction and would permit discontinuation of prednisone by 6 months. A related article on a randomized trial of rituximab versus cyclophosphamide in ANCA-associated vasculitis (RITUXVAS; Current Controlled Trials number, ISRCTN28528813) to assess the treatment response and rates of severe adverse events with a rituximab-based regimen appears elsewhere in this issue of the Journal.24
METHODS
STUDY DESIGN AND PATIENTS
The first and last authors designed the trial in collaboration with the clinical development team at the Immune Tolerance Network and clinical investigators of the RAVE research group. The site investigators gathered the data, and the data were analyzed by the RAVE data committee, which consisted of the two coprincipal investigators and representatives of the Immune Tolerance Network, the National Institute of Allergy and Infectious Diseases, and the coordinating center (Rho). The data committee did not include representatives of either Genentech or Biogen Idec, which provided funding and medications for the study. The manuscript was drafted and written by the first and last authors, with input as appropriate from members of the RAVE data committee and the clinical investigators. The RAVE data committee made the decision to submit the manuscript for publication, and the first and last authors vouch for the accuracy and completeness of the data and analyses.
Both the full study-entry criteria, included in the Supplementary Appendix, and the trial protocol are available with the full text of this article at NEJM.org. Briefly, patients with Wegener’s granulomatosis or microscopic polyangiitis were eligible to participate in the study if they had positive serum assays for proteinase 3–ANCA or myeloperoxidase-ANCA, manifestations of severe disease,11 and a Birmingham Vasculitis Activity Score for Wegener’s Granulomatosis (BVAS/WG) of 3 or more (scores range from 0 to 63, with higher scores indicating more active disease).25 Patients with either newly diagnosed or relapsing disease were eligible for enrollment. The RAVE trial was approved by the institutional review board at each participating site. All patients provided written informed consent.
Patients were randomly assigned, in a 1:1 ratio, to investigational therapy (the rituximab group) or standard therapy (the control group). Randomization was stratified according to clinical site and ANCA type.
TREATMENTS
The remission-induction period was 6 months. The rituximab group received intravenous rituximab (Rituxan, Genentech) (at a dose of 375 mg per square meter of body-surface area once weekly for 4 weeks) plus daily placebo–cyclophosphamide. The control group received placebo–rituximab infusions plus daily cyclophosphamide (2 mg per kilogram of body weight, adjusted for renal insufficiency). Patients in the control group who had a remission between 3 and 6 months were eligible to switch from cyclophosphamide to azathioprine (2 mg per kilogram per day).10 Patients in the rituximab group with a remission during the same 3-to-6-month period were switched from placebo–cyclophosphamide to placebo–azathioprine.
The two treatment groups received the same glucocorticoid regimen: one to three pulses of methylprednisolone (1000 mg each), followed by prednisone at a dose of 1 mg per kilogram per day. The dose was tapered so that by 5 months, all patients who had a remission without disease flares had discontinued glucocorticoids (see the Supplementary Appendix).
ASSESSMENTS
Study visits occurred at baseline; at weeks 1, 2, 3, and 4; and at 2, 4, and 6 months. Disease activity was measured on the basis of the BVAS/WG and the physician’s global assessment.25 Damage related to disease or treatment was scored according to the Vasculitis Damage Index (scores for this index range from 0 to 64, with higher scores indicating more severe damage).26 Health-related quality of life was scored with the use of the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36).27 Scores on this scale range from 0 to 100, with higher scores indicating better health.
Serial serum samples were tested for proteinase 3–ANCA and myeloperoxidase-ANCA by means of a direct enzyme-linked immunosorbent assay (ELISA).28
END POINTS
The primary end point was a BVAS/WG of 0 and successful completion of the prednisone taper at 6 months. Secondary end points included rates of disease flares, a BVAS/WG of 0 during treatment with prednisone at a dose of less than 10 mg per day, cumulative glucocorticoid doses, rates of adverse events, and SF-36 scores. A disease flare was defined as an increase in the BVAS/WG of 1 point or more. Patients who had severe flares during the first 6 months were eligible for crossover to the other treatment group in a blinded fashion. Those who crossed over received the other induction regimen in full. Limited flares were treated by increasing the dose of prednisone.
Patients were classified as having early treatment failure if at 1 month their BVAS/WG had not decreased by at least 1 point or a new manifestation of disease had emerged. Patients with early treatment failure discontinued their assigned treatments, received therapies according to best medical judgment, and were counted as having failure with respect to the primary end point.
ADVERSE EVENTS
All adverse events were graded according to the National Cancer Institute’s Common Terminology Criteria.29 During protocol development, the study team and the Food and Drug Administration identified nine major adverse events, termed selected adverse events, for priority analysis. These events included deaths (from all causes), malignant conditions, grade 2 or higher leukopenia or thrombocytopenia, grade 3 or higher infections, drug-induced cystitis, venous thromboembolic events, stroke, hospitalizations, and infusion reactions that contraindicated further infusions.
STATISTICAL ANALYSIS
In calculating the sample size, we assumed that 70% of the patients in both treatment groups would have disease remission after the discontinuation of prednisone at 6 months. We specified a noninferiority margin of −20 percentage points for the difference in remission rates (the rate in the rituximab group minus the rate in the control group) and a one-sided alpha level of 0.025. Assuming a 10% dropout rate, we calculated that we would need to enroll 100 patients in each group for an 83% statistical power to demonstrate non-inferiority.
Primary analyses were performed by the intention-to-treat method. Patients who dropped out of the study before 6 months were considered to have a treatment failure with respect to the primary end point. We assessed noninferiority by comparing the lower limit of the 95.1% confidence interval for the mean treatment difference (the rate in the rituximab group minus the rate in the control group) to −20 percentage points and testing the corresponding hypothesis that the difference would be greater than −20 percentage points. Superiority was assessed by means of a one-tailed t-test comparing the mean treatment difference with zero. To assess the consistency of the study results, analyses were repeated for predefined subgroups based on the following baseline variables: type of ANCA-associated vasculitis, type of ANCA, newly diagnosed disease, relapsing disease, alveolar hemorrhage, and severe renal disease. With analysis of eight subgroups, chance alone would result in 0.39 statistically significant results (P<0.05). We did not correct these subgroup analyses for multiplicity because they were prespecified and had biologically plausible bases.
For other analyses, two-sample comparisons were performed with the use of Student’s t-test or a Wilcoxon rank-sum test for continuous measures and a chi-square test or Fisher’s exact test for binary measures. Adjusted analyses were performed by means of analysis of covariance or logistic regression. Baseline covariates for these analyses included type of ANCA, new versus relapsing disease, renal function, and BVAS/WG. Rates of adverse events were compared with the use of Poisson regression. All statistical tests were two-sided, and a P value of less than 0.05 was considered to indicate statistical significance (see the Supplementary Appendix for details of the interim analysis).
RESULTS
PATIENTS
Between December 30, 2004, and June 30, 2008, a total of 197 patients with ANCA-associated vasculitis were enrolled at nine clinical sites participating in the study (Fig. 1). The baseline characteristics of the patients are listed in Table 1. Ninety-nine patients were assigned to the rituximab group, and 98 patients were assigned to the control group. The treatment groups were balanced with respect to Wegener’s granulomatosis versus microscopic polyangiitis, patients with newly diagnosed disease, disease activity, organ involvement, pre-enrollment therapy, past exposure to cyclophosphamide, and total glucocorticoids administered in the interval from 14 days before informed consent was obtained to the first investigational infusion (Table 1). Forty-eight patients (24%) had diagnoses of microscopic polyangiitis, and 148 (75%) had diagnoses of Wegener’s granulomatosis. The specific diagnosis was indeterminate in 1 patient. Approximately 49% of patients in both groups had a new diagnosis. The mean (±SD) BVAS/WG scores at entry were 8.5±3.2 in the rituximab group and 8.2±3.2 in the control group.
Figure 1. Randomization and Inclusion in the Analysis at 6 Months.
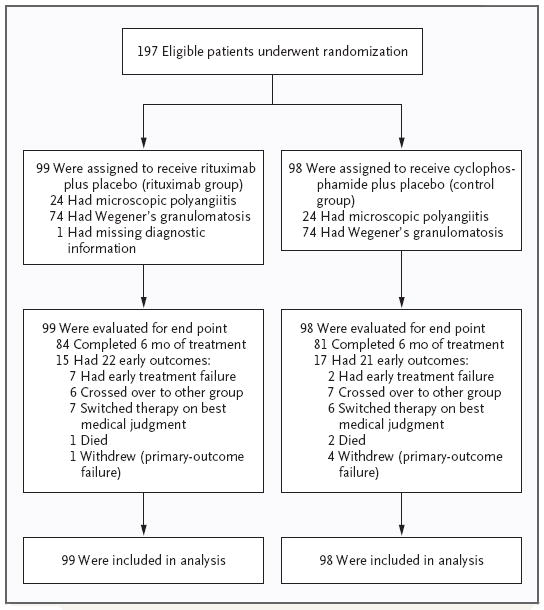
Patients were randomly assigned, in a 1:1 ratio, to the treatment and control groups. The study groups were balanced with respect to ANCA type. The majority of patients (84 patients in the rituximab group and 81 patients in the control group) completed 6 months of the treatment to which they were assigned. The remainder had one or more events that led to withdrawal from the study. Data related to the primary analysis were available for all patients. Five patients who withdrew voluntarily from the trial (1 patient in the rituximab group and 4 patients in the control group) were regarded as having had a treatment failure with respect to the primary end point.
Table 1.
Baseline Demographic and Clinical Characteristics of the Patients.*
| Variable | Rituximab Group (N = 99) | Control Group (N = 98) | P Value |
|---|---|---|---|
| Age at onset of symptoms (yr) | 54.0±16.8 | 51.5±14.1 | 0.26 |
| Sex (%) | 0.29 | ||
| Male | 46 | 54 | |
| Female | 54 | 46 | |
| Race or ethnic group (%) | 0.64 | ||
| White | 92 | 95 | |
| Black | 3 | 3 | |
| Asian | 1 | 0 | |
| Other | 4 | 2 | |
| Ethnic group (%) | 0.60 | ||
| Not Hispanic or Latino | 92 | 95 | |
| Hispanic or Latino | 6 | 3 | |
| Unknown | 2 | 2 | |
| ANCA-associated vasculitis type (%) | 0.61 | ||
| Wegener’s granulomatosis† | 75 | 76 | |
| Microscopic polyangiitis | 24 | 24 | |
| Indeterminate | 1 | 0 | |
| Newly diagnosed at enrollment (%) | 48 | 49 | 0.62 |
| Pre-enrollment disease duration in patients with relapsed disease (yr) | 6.5±6.7 | 5.3±7.4 | 0.31 |
| Pre-enrollment exposure to cyclophosphamide in patients with relapsed disease (%) | 82 | 74 | 0.10 |
| Disease-assessment scores | |||
| BVAS/WG‡ | 8.5±3.2 | 8.2±3.2 | 0.38 |
| Physician’s global assessment | 5.7±2.4 | 5.6±2.4 | 0.67 |
| Vasculitis Damage Index | 1.4±1.8 | 1.0±1.4 | 0.17 |
| SF-36§ | |||
| Physical component | 37.2±9.8 | 38.6±11.9 | 0.38 |
| Mental component | 41.7±13.2 | 44.0±11.4 | 0.20 |
| Organ involvement | |||
| Constitutional signs or symptoms (%)¶ | 56 | 66 | 0.12 |
| Cutaneous involvement (%) | 20 | 16 | 0.48 |
| Mucous membranes and eyes (%) | 27 | 26 | 0.78 |
| Ear, nose, and throat (%) | 61 | 56 | 0.52 |
| Pericarditis (%) | 0 | 1 | 0.50 |
| Mesenteric ischemia (%) | 2 | 0 | 0.50 |
| Pulmonary involvement (%) | 52 | 54 | 0.83 |
| Alveolar hemorrhage | 27 | 24 | 0.54 |
| Endobronchial lesions | 4 | 9 | 0.15 |
| Nodules or cavities | 18 | 28 | 0.12 |
| Other lung infiltrate | 25 | 21 | 0.53 |
| Pleurisy | 8 | 9 | 0.78 |
| Respiratory failure | 2 | 0 | 0.50 |
| Renal involvement (%)∥ | 66 | 66 | 0.92 |
| Hematuria (%) | 28 | 29 | 0.96 |
| Red-cell casts (%) | 37 | 36 | 0.81 |
| Creatinine clearance (ml/min) | 54±3 | 69±4 | 0.04 |
| Neurologic involvement (%) | 25 | 15 | 0.08 |
| Cranial-nerve palsy | 0 | 1 | 0.50 |
| Meningitis | 1 | 0 | 0.50 |
| Motor mononeuritis multiplex | 11 | 9 | 0.20 |
| Sensory peripheral neuropathy | 22 | 13 | 0.10 |
| ANCA-positive at diagnosis (%) | |||
| By immunofluorescence | |||
| All | 98 | 96 | |
| C-ANCA | 66 | 62 | |
| P-ANCA | 33 | 34 | |
| By ELISA | |||
| All | 98 | 100 | |
| Proteinase 3 ANCA | 67 | 66 | |
| Myeloperoxidase-ANCA | 32 | 34 | |
| Mean dose of glucocorticoids from 14 days before consent provided to first infusion of study drug | |||
| Methylprednisolone (g) | 0.8±1.28 | 0.7±1.10 | |
| Prednisone (mg) | 253.6±236.5 | 296.1±266.2 |
Plus-minus values are means ±SD, except for the values for creatinine clearance, which are means ±SE. Race and ethnic group were self-reported. The chi-square test or Fisher’s exact test was used for the comparison of categorical data, and Student’s t-test or the Wilcoxon rank-sum test was used for the analysis of continuous data. ANCA denotes antineutrophil cytoplasmic antibody, C-ANCA cytoplasmic ANCA-labeling pattern, ELISA enzyme-linked immunosorbent assay, and P-ANCA perinuclear ANCA-labeling pattern.
American College of Rheumatology Criteria were used for the classification of Wegener’s granulomatosis.
The Birmingham Vasculitis Activity Score for Wegener’s Granulomatosis (BVAS/WG) for new or worse disease ranges from 0 to 67, with higher scores indicating more active disease. A BVAS/WG of 0 indicates remission.
Scores on the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36), version 2, range from 0 to 100, with higher scores indicating better health. A score of 50 represents the mean score for the U.S. population.
Constitutional signs or symptoms of disease activity included arthritis, arthralgias, and fever (temperature ≥38.0°C).
On the BVAS/WG instrument, hematuria is not scored if red-cell casts are present or a renal-biopsy specimen shows active glomerulonephritis at the same time.
Ninety-seven percent of all patients received at least three study-drug infusions. None were lost to follow-up. Eighty-four of the patients who were randomly assigned to the rituximab group (85%) and 81 of those who were randomly assigned to the control group (83%) completed 6 months of treatment without meeting criteria for early treatment failure, crossing over to the other treatment group, switching to a therapy based on best medical judgment, or withdrawing from the protocol for other reasons (Fig. 1).
EFFICACY ASSESSMENTS
End Points
Sixty-three of the 99 patients in the rituximab group (64%) reached the primary end point, as compared with 52 of 98 in the control group (53%). The treatment difference of 11 percentage points between the groups met the criterion for non-inferiority (P<0.001). The proportion of patients who reached the primary end point was larger in the rituximab group than in the control group, but the difference was not significant (95.1% confidence interval [CI], −3.2 to 24.3 percentage points; P = 0.09) (Fig. 2). Seventy patients treated with rituximab (71%) reached the secondary end point of disease remission while receiving less than 10 mg per day of prednisone, as compared with 61 patients in the control group (62%, P=0.10).
Figure 2. Treatment Effect According to Prednisone Dose at 6 Months.
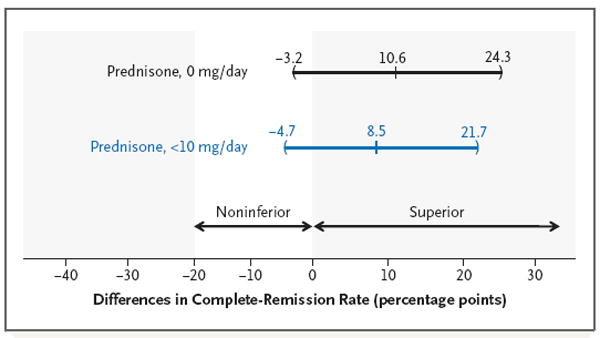
Point estimates and 95.1% confidence intervals are shown for the treatment effect, defined as the difference in rates of complete remission between the treatment groups. The criterion for the noninferiority of rituximab was a difference in remission rates of 20 percentage points, and the criterion for superiority was a difference of 0 percentage points. For both complete remission with 0 mg of prednisone per day and complete remission with less than 10 mg per day, the difference in remission rates was above 20 percentage points, meaning that the criterion for the noninferiority of rituximab was met (P<0.001 for both comparisons).
ANCA type, newly diagnosed disease, renal function, BVAS/WG, and age did not affect the primary comparison when examined in logistic-regression models (data not shown). However, among patients with relapsing disease at baseline, rituximab was more efficacious than cyclophosphamide: 34 of 51 patients in the rituximab group (67%) reached the primary end point, as compared with only 21 of 50 in the control group (42%, P = 0.01). Evidence of the superior efficacy of rituximab among patients with relapsing disease at baseline persisted even after adjustment for differences in ANCA type and clinical site (odds ratio, 1.40; 95% CI, 1.03 to 1.91; P = 0.03).
Disease Type
Among patients with Wegener’s granulomatosis, 46 of 73 assigned to rituximab (63%) and 37 of 74 treated with cyclophosphamide (50%) reached the primary end point (P = 0.11). Among the patients with microscopic polyangiitis, 16 of 24 in the rituximab group (67%) and 15 of 24 in the control group (62%) reached the primary end point (P=0.76).
Major Renal Disease at Baseline
A subgroup of patients had at least one major renal BVAS/WG item at baseline (i.e., urinary red-cell casts, biopsy-confirmed glomerulonephritis, or an increase in the baseline serum creatinine concentration of more than 30%). Fifty-one of the patients in the rituximab group (52%) had at least one major renal item at baseline, as compared with 51 in the control group (52%). In this subgroup, baseline renal function in the rituximab group was worse than in the control group (mean [±SD] estimated creatinine clearance, 53.8±29.8 ml per minute vs. 68.9±41.6 ml per minute; P = 0.04). However, the estimated creatinine clearances increased in parallel in the two groups during the first 6 months (by 11.2 ml per minute in the rituximab group and 10.5 ml per minute in the control group), and the percentages of patients who reached the primary end point were not significantly different (31 of 51 patients in the rituximab group [61%] vs. 32 of 51 patients in the control group [63%], P=0.92).
Alveolar Hemorrhage at Baseline
Twenty-eight patients in the rituximab group (28%) had alveolar hemorrhage at baseline, as compared with 27 in the control group (28%). Among these patients, 16 (57%) and 11 (41%), respectively, reached the primary end point (P = 0.48).
Severity of Flares
Six patients in the rituximab group and 10 in the control group had severe disease flares. The rates of severe flares were 0.011 and 0.018 per patient-month, respectively (P = 0.30). There was no significant between-group difference in the number of limited flares: there were 13 flares in 11 patients in the rituximab group and 15 flares in 14 patients in the control group. The rates of limited disease flares were 0.023 and 0.027 per patient-month, respectively (P = 0.81).
Damage and Quality of Life
Scores on the Vasculitis Damage Index increased by 1.3 points from baseline to 6 months in the rituximab group and by 1.5 points in the control group (P = 0.62). Quality-of-life outcomes did not differ significantly between the two groups (see the Supplementary Appendix).
Peripheral-Blood B-Lymphocyte Counts
The number of peripheral-blood CD19+ B cells decreased to less than 10 cells per cubic millimeter after two infusions of rituximab and remained at that level in most patients through 6 months (Fig. 3). In the rituximab group, 87 of 93 patients (94%) had this degree of B-cell depletion at 1 month. Among the patients who did not have B-cell depletion, 4 patients reached the primary end point and 1 patient did not. In the control group, peripheral-blood CD19+ B-cell counts also decreased, but the rate and magnitude of the decrease were less than in the rituximab group.
Figure 3. Peripheral-Blood B-Cell Counts.
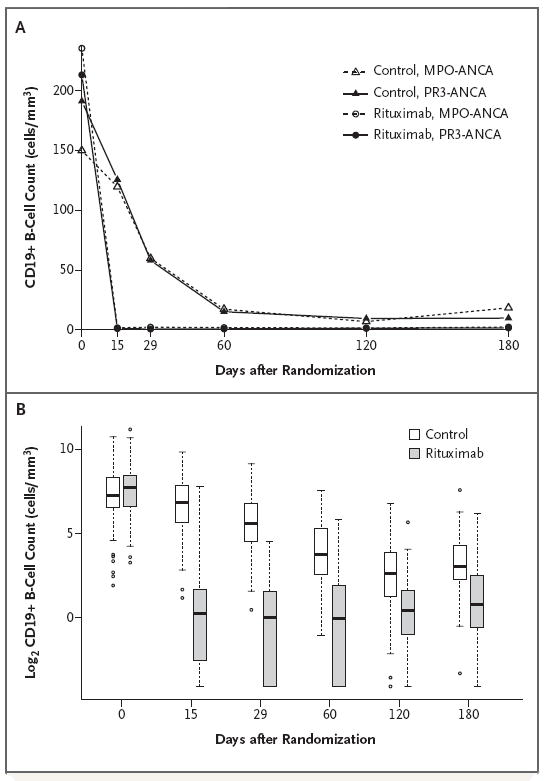
Panel A shows the peripheral-blood B-cell counts in the rituximab and control groups according to antineutrophil cytoplasmic antibody (ANCA) type. The counts in most patients who received rituximab decreased to less than 10 CD19+ cells per cubic millimeter after two infusions and remained at that level until 6 months. B-cell counts decreased more slowly in the control group than in the rituximab group and remained detectable, at low levels. MPO-ANCA denotes ANCA directed against myeloperoxidase, and PR3-ANCA ANCA directed against proteinase 3. Panel B shows box plots of log2-transformed values for CD19+ B cells at six time points, according to treatment group. The horizontal line within each box indicates the median value; the bottom and top lines of the box depict the 25th and 75th quartiles, respectively; and the whiskers show the upper and lower values at 1.5 times the interquartile range. The open circles represent values outside this range and are considered outliers. Values equaling 0 were converted to the lowest nonzero value of 0.06 before log2 transformation.
ANCA Response
Among patients who remained in their original treatment groups, 47% in the rituximab group and 24% in the control group became ANCA-negative by 6 months (P = 0.004). This difference between the two treatment groups in loss of ANCA reactivity was due to changes in the subgroup of patients who were initially positive for proteinase 3–ANCA. Fifty percent of such patients in the rituximab group became negative for proteinase 3–ANCA, as compared with only 17% in the control group (P<0.001). In contrast, equivalent percentages of patients in the rituximab and control groups became negative for myeloperoxidase–ANCA (40% vs. 41%, P = 0.95). The loss of ANCA reactivity, as measured by means of direct ELISA, was not significantly associated with attainment of the primary end point.
ADVERSE EVENTS
There were no significant differences between the treatment groups in the numbers of total adverse events, serious adverse events, or non–disease-related adverse events, or in the number of participants with at least one non–disease-related adverse event (Table 2). Fourteen patients in the rituximab group (14%) and 17 in the control group (17%) had events leading to discontinuation of treatment.
Table 2.
Adverse Events at 6 Months.*
| Variable | Rituximab Group (N = 99) | Control Group (N = 98) | Total (N = 197) |
|---|---|---|---|
| Total no. of selected adverse events† | 31 | 33 | 64 |
| >1 Selected adverse event — no. of patients (%) | 22 (22) | 32 (33) | 54 (27) |
| Annual rate of selected adverse events — % | 5 | 6 | 6 |
| Specific selected adverse events — no. of events (%)† | |||
| Death | 1 (1) | 2 (2) | 3 (2) |
| Cancer | 1 (1) | 1 (1) | 2 (1) |
| Leukopenia (≥grade 2) | 3 (3) | 10 (10) | 13 (7) |
| Thrombocytopenia (≥grade 3) | 3 (3) | 1 (1) | 4 (2) |
| Infection (≥grade 3) | 7 (7) | 7 (7) | 14 (7) |
| Hemorrhagic cystitis | 1 (1) | 1 (1) | 2 (1) |
| Venous thrombotic event | 6 (6) | 9 (9) | 15 (8) |
| Cerebrovascular accident | 0 | 0 | 0 |
| Hospitalization due to disease or treatment | 8 (8) | 2 (2) | 10 (5) |
| Infusion reaction preventing further infusions of investigational medication | 1 (1) | 0 | 1 (<1) |
| All adverse events — no. | 1035 | 1016 | 2051 |
| All adverse events ≥ grade 3 and serious adverse events — no. | 79 | 78 | 157 |
| All non-disease-related adverse events ≥ grade 3 and serious adverse events — no. | 58 | 53 | 111 |
| Patients with ≥1 non-disease-related adverse event — % | 29 | 29 | 58 |
| All adverse events ≥ grade 3 and serious adverse events leading to treatment discontinuation — no. | 6 | 8 | 14 |
| Grade 3 adverse events — no. | 61 | 77 | 138 |
| ≥1 Grade 3 adverse event — no. of patients (%) | 22 (22) | 32 (33) | 54 (27) |
| Grade 4 adverse events — no. | 11 | 5 | 16 |
| ≥1 Grade 4 adverse event — no. of patients (%) | 8 (8) | 4 (4) | 12 (6) |
| Grade 5 adverse events (death) — no. | 1 (1) | 2 (2) | 3 (2) |
Adverse events were categorized according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 3.
Selected adverse events were defined as death (from any cause), cancer, grade 2 or higher leukopenia or thrombocytopenia, grade 3 or higher infections, drug-induced cystitis, venous thromboembolic events, stroke, hospitalization, and infusion reactions leading to the discontinuation of further infusions.
More patients in the control group than in the rituximab group had one or more of the predefined selected adverse events: 32 (33%) versus 22 (22%) (P = 0.01) (Table 2). More episodes of grade 2 or higher leukopenia (white-cell count, <3000 per cubic millimeter) in the control group (10, vs. 3 in the control group) accounted for most of this difference (Table 2). Eight patients in the rituximab group were hospitalized for adverse events related to either the disease or its treatment, as compared with 2 in the control group. No pattern emerged with respect to causes of hospitalization. During the first 6 months of the trial, solid malignant tumors were diagnosed in 1 patient in each group; 2 patients in the control group and 1 in the rituximab group died.
Six malignant conditions developed in 5 additional patients after 6 months. Four of those patients had been assigned initially to rituximab and one had been assigned to cyclophosphamide. The specific types of solid malignant tumors among patients who received rituximab were papillary thyroid cancer (in 1 patient), uterine cancer (in 1 patient), prostate cancer (in 1 patient), colon cancer (in 2 patients), bladder cancer (in 1 patient), and lung cancer (in 1 patient). The specific types of solid malignant tumors among patients who received cyclophosphamide were prostate cancer (in 1 patient) and lung cancer (in 1 patient). Among patients with exposure to rituximab during the trial, malignant conditions developed in 6 of 124 (5%), as compared with 1 of 73 patients without exposure to rituximab (1%, P = 0.26). With the exception of two cases of prostate cancer, all patients in whom malignant conditions developed had histories of exposure to at least two medications known to increase the risk of cancer (cyclophosphamide, azathioprine, or methotrexate) (see the Supplementary Appendix).
DISCUSSION
Although a randomized, controlled trial involving patients with severe ANCA-associated vasculitis that compared cyclophosphamide head to head with another agent had long been deemed unethical,30 uncontrolled studies have suggested that rituximab has efficacy for remission induction in ANCA-associated vasculitis.21-23 Those promising results led to the current study, which suggests that rituximab plus glucocorticoids provides similar results to cyclophosphamide plus glucocorticoids for induction of remission.
The observed treatment effects were consistent across all measures of clinical efficacy. A higher percentage of rituximab-treated patients reached the primary end point (64% vs. 53%); the difference exceeded the prespecified noninferiority margin by 31%. In addition, in a prespecified subgroup analysis,31 patients who presented with relapsing disease and who received rituximab fared substantially better than did those with relapsing disease who received cyclophosphamide. Among patients with severe renal disease or alveolar hemorrhage, the outcomes were similar with the two treatment regimens.
The likelihood of remission at 6 months is affected by whether glucocorticoids have been tapered and discontinued entirely, as well as by the specific definition of remission.32-35 Several differences in trial design may explain why the remission rates in this trial were lower than those in some other vasculitis trials.10,11,32-35 Particularly important is the fact that in other vasculitis trials, patients have generally been permitted to continue to receive glucocorticoids for 1 year or longer. In addition, some of the patients in other trials who were classified as being in remission had the continuation of one or more minor BVAS items (i.e., a score higher than 0).
We anticipated lower rates of certain adverse events in the rituximab group, but we did not observe major differences between the two groups in overall adverse events. There are several possible reasons for this finding. First, adverse events, by their definition, include both disease and treatment complications, including those related to glucocorticoid use. Second, 6 months may have been too short a period in which to detect some of the cyclophosphamide-associated adverse events (e.g., infertility). Third, rigorous monitoring of all patients in our trial may have reduced the incidence of cyclophosphamide-induced leukopenia, which may occur in clinical practice if blood counts are not checked every 2 weeks.
Our trial had certain limitations. We enrolled only patients with severe ANCA-associated vasculitis who were ANCA-positive. Thus, it is not clear whether the treatment effects extend to patients with limited Wegener’s granulomatosis or those who are ANCA-negative.6 Patients with alveolar hemorrhage severe enough to require ventilatory support and those with advanced renal dysfunction (serum creatinine level, >4.0 mg per deciliter [354 μmol per liter]) were excluded. Thus, the comparative efficacy of these two regimens is uncertain in such patients.
Our study focused exclusively on remission induction but did not address the question of retreatment with rituximab. Rituximab was not re-administered after the return of peripheral-blood B cells (anticipated by 9 to 12 months). Longer follow-up in the present trial is important to understand the benefits and risks of rituximab therapy for ANCA-associated vasculitis. Evaluations of patients followed for a minimum of 18 months will explore issues such as the need for retreatment, particularly in the context of peripheral B-cell reconstitution. The finding that loss of proteinase 3–ANCA production occurred more frequently with rituximab therapy than with cyclophosphamide therapy suggests that these two treatment strategies modulate proteinase 3–producing cells differently. Since the ANCA response was not associated with the primary end point, it is possible that the clinical efficacies of both rituximab and cyclophosphamide are due to mechanisms beyond autoantibody suppression.
In conclusion, our data suggest that treatment with rituximab and glucocorticoids is not inferior to the standard regimen in patients with severe ANCA-associated vasculitis of recent onset. Moreover, the regimen may be superior to the standard regimen of cyclophosphamide and glucocorticoids for remission induction in severe relapsing ANCA-associated vasculitis.
Supplementary Material
Acknowledgments
Supported by a grant from the National Institute of Allergy and Infectious Diseases to the Immune Tolerance Network (N01-AI-15416; protocol no. ITN021AI). Genentech and Biogen provided the study medications and partial funding. At the Mayo Clinic and Foundation, the trial was supported by a Clinical and Translational Science Award from the National Center for Research Resources (NCRR) (RR024150-01); at Johns Hopkins University, by grants from the NCRR (RR025005) and career development awards (K24 AR049185, to Dr. Stone, and K23 AR052820, to Dr. Seo); and at Boston University, by a Clinical and Translational Science Award (RR 025771), grants from the National Institutes of Health (M01 RR00533) and a career development award (K24 AR02224, to Dr. Merkel), and an Arthritis Foundation Investigator Award (to Dr. Monach). Enzyme-linked immunosorbent assay kits for antineutrophil cytoplasmic antibody were provided by Euroimmun (Lübeck, Germany).
APPENDIX
Members of the RAVE-ITN Research Group are as follows: Protocol Cochairs — U. Specks (Mayo Clinic), J.H. Stone (Massachusetts General Hospital); Mayo Clinic — U. Specks, S.R. Ytterberg, F.C. Fervenza, K.A. Keogh, T. Peikert, J.M. Golbin, L. Klein, K. Mieras, C. Beinhorn, S. Fisher, M.L. Clawson, S. Bendel, A.M. Hummel (Mayo Clinic Eisenberg Research Pharmacy); Boston University — P.A. Merkel, E.Y. Kissin, P.A. Monach, M.R. Clark-Cotton, C.A. McAlear, J.L. Pettit, M.B. Sutton, R.L. Widom, G.A. Farina, M.J. DiMarzio, S.P. Johnson, A. Schiller Patel; Johns Hopkins University — P. Seo, J.H. Stone, D. Hellmann, D. Geetha, A. Saleh, P. Wung, L.P. Sejismundo, C. Humphrey, M. Marriott, Y. Goldsborough, A. Pinachos, K. Gauss, L. King; Cleveland Clinic Foundation — C.A. Langford, G.S. Hoffman, R.A. Hajj-Ali, J.J. Carey, E.S. Molloy, C.L. Koening, D. Bork, T.M. Clark, K.A. Tuthill, T. Markle, J. Petrich; Hospital for Special Surgery — R. Spiera, D.R. Alpert, S.J. DiMartino, J.K. Gordon, N.K. Moskowitz, K.A. Kirou, J. Samuels, S.A. Kloiber, E. Julevic, M. O’Donohue, A. Patel; University of Groningen — C.G.M. Kallenberg, C. Stegeman, P. Rasker, K. Mulder, P. Limburg, J. Kosterink; Duke University — E.W. St. Clair, N.B. Allen, E. Scarlett, M. Tochacek; University of Alabama–Birmingham — A. Turkiewicz, B. Fessler, W. Chatham, A. Turner; Coordinating Centers: Rho — D. Ikle, D. Weitzenkamp, W. Wu, T. D’Lugin, C. Jacob; National Institute of Allergy and Infectious Diseases — L. Webber, L. Ding, S. Adah; Immune Tolerance Network — N.K. Tchao, M. Mueller, K. Bourcier, A. Asare, V. Seyfert-Margolis, P. Tosta, N.B. Skeeter, C.L. Anderson, A.N. Archampong.
Footnotes
The views expressed in this article are those of the authors and do not necessarily reflect those of the Food and Drug Administration.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Jennette JC, Falk RJ, Andrassy K, et al. Nomenclature of systemic vasculitides: the proposal of an international consensus conference. Arthritis Rheum. 1994;37:187–92. doi: 10.1002/art.1780370206. [DOI] [PubMed] [Google Scholar]
- 2.Finkielman JD, Lee AS, Hummel AM, et al. ANCA are detectable in nearly all patients with active severe Wegener’s granulomatosis. Am J Med. 2007;120(7):643.e9–643.14. doi: 10.1016/j.amjmed.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman GS, Kerr GS, Leavitt RY, et al. Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med. 1992;116:488–98. doi: 10.7326/0003-4819-116-6-488. [DOI] [PubMed] [Google Scholar]
- 4.Guillevin L, Durand-Gasselin B, Cevallos R, et al. Microscopic polyangiitis: clinical and laboratory findings in eighty-five patients. Arthritis Rheum. 1999;42:421–30. doi: 10.1002/1529-0131(199904)42:3<421::AID-ANR5>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 5.Reinhold-Keller E, Beuge N, Latza U, et al. An interdisciplinary approach to the care of patients with Wegener’s granulomatosis: long-term outcome in 155 patients. Arthritis Rheum. 2000;43:1021–32. doi: 10.1002/1529-0131(200005)43:5<1021::AID-ANR10>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 6.Stone JH. Limited versus severe Wegener’s granulomatosis: baseline data on patients in the Wegener’s Granulomatosis Etanercept Trial. Arthritis Rheum. 2003;48:2299–309. doi: 10.1002/art.11075. [DOI] [PubMed] [Google Scholar]
- 7.Novack SN, Pearson CM. Cyclophosphamide therapy in Wegener’s granulomatosis. N Engl J Med. 1971;284:938–42. doi: 10.1056/NEJM197104292841703. [DOI] [PubMed] [Google Scholar]
- 8.Fauci AS, Wolff SM. Wegener’s granulomatosis: studies in eighteen patients and a review of the literature. Medicine (Baltimore) 1973;52:535–61. doi: 10.1097/00005792-197311000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Walton EW. Giant-cell granuloma of the respiratory tract (Wegener’s granulomatosis) BMJ. 1958;2:265–70. doi: 10.1136/bmj.2.5091.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jayne D, Rasmussen N, Andrassy K, et al. A randomized trial of maintenance therapy for vasculitis associated with antineutrophil cytoplasmic autoantibodies. N Engl J Med. 2003;349:36–44. doi: 10.1056/NEJMoa020286. [DOI] [PubMed] [Google Scholar]
- 11.The Wegener’s Granulomatosis Etanercept Trial (WGET) Research Group. Etanercept plus standard therapy for Wegener’s granulomatosis. N Engl J Med. 2005;352:351–61. doi: 10.1056/NEJMoa041884. [DOI] [PubMed] [Google Scholar]
- 12.Seo P, Min YI, Holbrook JT, et al. Damage caused by Wegener’s granulomatosis and its treatment: prospective data from the Wegener’s Granulomatosis Etanercept Trial (WGET) Arthritis Rheum. 2005;52:2168–78. doi: 10.1002/art.21117. [DOI] [PubMed] [Google Scholar]
- 13.Stone JH, Holbrook JT, Marriott MA, et al. Solid malignancies among patients in the Wegener’s Granulomatosis Etanercept Trial. Arthritis Rheum. 2006;54:1608–18. doi: 10.1002/art.21869. [DOI] [PubMed] [Google Scholar]
- 14.Pagnoux C, Hogan SL, Chin H, et al. Predictors of treatment resistance and relapse in antineutrophil cytoplasmic antibody-associated small-vessel vasculitis: comparison of two independent cohorts. Arthritis Rheum. 2008;58:2908–18. doi: 10.1002/art.23800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin F, Chan AC. Pathogenic roles of B cells in human autoimmunity: insights from the clinic. Immunity. 2004;20:517–27. doi: 10.1016/s1074-7613(04)00112-8. [DOI] [PubMed] [Google Scholar]
- 16.Popa ER, Stegeman CA, Bos NA, Kallenberg CG, Tervaert JW. Differential Band T-cell activation in Wegener’s granulomatosis. J Allergy Clin Immunol. 1999;103:885–94. doi: 10.1016/s0091-6749(99)70434-3. [DOI] [PubMed] [Google Scholar]
- 17.Stevenson HC, Fauci AS. Activation of human B lymphocytes. XII. Differential effects of in vitro cyclophosphamide on human lymphocyte subpopulations involved in B-cell activation. Immunology. 1980;39:391–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Cupps TR, Edgar LC, Fauci AS. Suppression of human B lymphocyte function by cyclophosphamide. J Immunol. 1982;128:2453–7. [PubMed] [Google Scholar]
- 19.Zhu LP, Cupps TR, Whalen G, Fauci AS. Selective effects of cyclophosphamide therapy on activation, proliferation, and differentiation of human B cells. J Clin Invest. 1987;79:1082–90. doi: 10.1172/JCI112922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson P, Glennie M. The mechanisms of action of rituximab in the elimination of tumor cells. Semin Oncol. 2003;30:3–8. doi: 10.1053/sonc.2003.50025. [DOI] [PubMed] [Google Scholar]
- 21.Specks U, Fervenza FC, McDonald TJ, Hogan MC. Response of Wegener’s granulomatosis to anti-CD20 chimeric monoclonal antibody therapy. Arthritis Rheum. 2001;44:2836–40. doi: 10.1002/1529-0131(200112)44:12<2836::aid-art471>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 22.Keogh KA, Wylam ME, Stone JH, Specks U. Induction of remission by B lymphocyte depletion in eleven patients with refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2005;52:262–8. doi: 10.1002/art.20718. [DOI] [PubMed] [Google Scholar]
- 23.Keogh KA, Ytterberg SR, Fervenza FC, Carlson KA, Schroeder DR, Specks U. Rituximab for refractory Wegener’s granulomatosis: report of a prospective, open-label pilot trial. Am J Respir Crit Care Med. 2006;173:180–7. doi: 10.1164/rccm.200507-1144OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones RB, Tervaert JWC, Hauser T, et al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med. 2010;363:211–20. doi: 10.1056/NEJMoa0909169. [DOI] [PubMed] [Google Scholar]
- 25.Stone JH, Hoffman GS, Merkel PA, et al. A disease-specific activity index for Wegener’s granulomatosis: modification of the Birmingham Vasculitis Activity Score. Arthritis Rheum. 2001;44:912–20. doi: 10.1002/1529-0131(200104)44:4<912::AID-ANR148>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 26.Exley AR, Bacon PA, Luqmani RA, et al. Development and initial validation of the Vasculitis Damage Index for the standardized clinical assessment of damage in the systemic vasculitides. Arthritis Rheum. 1997;40:371–80. doi: 10.1002/art.1780400222. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998;51:903–12. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- 28.Damoiseaux JG, Slot MC, Vaessen M, Stegeman CA, Van Paases P, Tervaert JW. Evaluation of a new fluorescent-enzyme immuno-assay for diagnosis and follow-up of ANCA-associated vasculitis. J Clin Immunol. 2005;25:202–8. doi: 10.1007/s10875-005-3863-2. [DOI] [PubMed] [Google Scholar]
- 29.National Cancer Institute. [April 29, 2010];Common terminology criteria for adverse events v3.0 (CTCAE) at http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf.
- 30.Fauci AS, Haynes BF, Katz P. Assessing treatments with cyclophosphamide (in comment) Ann Intern Med. 1983;98:1026–7. [Google Scholar]
- 31.Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM. Statistics in medicine — reporting of subgroup analyses in clinical trials. N Engl J Med. 2007;357:2189–94. doi: 10.1056/NEJMsr077003. [DOI] [PubMed] [Google Scholar]
- 32.Goek ON, Stone JH. Randomized controlled trials in vasculitis associated with anti-neutrophil cytoplasmic antibodies. Curr Opin Rheumatol. 2005;17:257–64. doi: 10.1097/01.bor.0000160777.28259.c2. [DOI] [PubMed] [Google Scholar]
- 33.Pagnoux C, Mahr A, Hamidou MA, et al. Azathioprine or methotrexate maintenance for ANCA-associated vasculitis. N Engl J Med. 2008;359:2790–803. doi: 10.1056/NEJMoa0802311. [DOI] [PubMed] [Google Scholar]
- 34.De Groot K, Rasmussen N, Bacon PA, et al. Randomized trial of cyclophosphamide versus methotrexate for induction of remission in early systemic antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2005;52:2461–9. doi: 10.1002/art.21142. [DOI] [PubMed] [Google Scholar]
- 35.De Groot K, Harper L, Jayne DR, et al. Pulse versus daily oral cyclophosphamide for induction of remission in antineutrophil cytoplasmic antibody-associated vasculitis: a randomized trial. Ann Intern Med. 2009;150:670–80. doi: 10.7326/0003-4819-150-10-200905190-00004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


