Depression, the common psychological disorder, affects about 121 million people worldwide. World Health Organization (WHO) states that depression is the leading cause of disability as measured by Years Lived with Disability (YLDs) and the fourth leading contributor to the global burden of disease. By the year 2020, depression is projected to reach second place in the ranking of Disability Adjusted Life Years (DALY) calculated for all ages. Today, depression already is the second cause of DALYs in the age category 15-44 years.
BURDEN OF DISEASE
An estimated 3-4% of India's 100 crore plus population suffers from major mental disorders and about 7-10% of the population suffers from minor depressive disorders. In the southeast Asian region, 11% of DALYs and 27% of YLDs are attributed to neuropsychiatric disease. A review of eight epidemiological studies on depression in South Asia shows that the prevalence in primary care was 26.3%. In the Goa study, the rate of depressive disorders was 46.5% in adult primary care attendees.
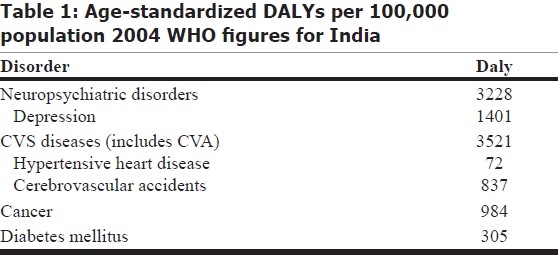
The above table 1 shows that disability due to depression exceeds disability due to all forms of cancer and diabetes mellitus combined, as well as exceeding the disability due to strokes and hypertensive heart diseases.
Table 1.
Age-standardized DALYs per 100,000 population 2004 WHO figures for India
The Global Burden of Disease (GBD) study (GBD 1990 Study) launched by the WHO in the 1990s showed that Depressive disorders account for 3.7% of total DALYs and 10.7% of total YLDs. GBD 2000 study (WHO 2001) showed that depression accounts for 4.46% of total DALYs and 12.1% of total YLDs. This clearly highlights a trend of increasing burden of disability secondary to depression.
SUICIDALITY
Depression is associated with high suicidality. About 50% of individuals who have committed suicide carried a primary diagnosis of depression. Because mood disorders underlie 50-70% of all suicides, effective treatment of these disorders on a national level should, in principle, drastically reduce this major complication of mood disorders. Indian union health ministry estimates state that 120,000 people commit suicide every year in India. Also over 400,000 people attempt suicide. A significant percentage of people who commit suicide in India (37.8%) are below 30 years of age. Ministry officials state that majority of those committing suicide suffer from depression or mental disorders.
MORBIDITY
Exactly 23% of depressed patients report health difficulties severe enough to keep them bedridden. A community sample of patients with MDD demonstrated increased health care utilization in comparison to patients in the general medical setting. Depression is associated with more impairment in occupational and interpersonal functioning in comparison to several common medical illnesses. The cost of depression, particularly the cost in lost work days, is as great as or greater than the cost of many other common medical illnesses.
MATERNAL AND CHILD HEALTH
Depression also has a large impact on maternal and child well being. A series of studies from South Asia have demonstrated that early childhood failure to thrive, as indicated by undernutrition and stunting of growth in babies under 1 year, is independently associated with depression in mothers. A study from Pakistan shows that babies of mothers who were depressed during pregnancy and in the postnatal period were more than five times at greater risk for being underweight and stunted at 6 months than babies of non-depressed mothers, even after adjustment for other confounding factors like socioeconomic status. Childhood failure to thrive is a major risk factor for child mortality. Depressed mothers are more likely to cease breastfeeding. Depression during pregnancy is strongly associated with low birth weight.
TREATMENT
The outcome of depression can be significantly improved by early detection. A wide range of highly effective treatments including antidepressant medications (at a cheaper cost), somatic therapies and psychotherapeutic interventions is available for the treatment of depression. Antidepressant medications and supportive psychological interventions are effective in about 80% of patients. But the number of trained professionals (Psychiatrists, Psychologists, Psychiatric nurses) in our country is very limited and spread out only in urban/semiurban areas.
THE PROBLEM OF AWARENESS
Less than 25% of those affected (in some estimates less than 10%) by depression receive treatment. Barriers to effective care include the lack of resources, lack of trained providers, and the stigma. Nearly half of the patients with depression, as in diabetes, remain undiagnosed for years or inadequately treated. Large numbers of patients from rural areas remain under care of religious healers and may never receive correct treatment. Special diets, tonics, appetite stimulants and energy pills dominate the prescriptions. Stigma still is a significant barrier. The majority of patients do not receive evidence-based treatments.
NEED FOR PRIMARY CARE INVOLVEMENT
Despite the fact that many patients with depressive disorders seek help in primary care, general practitioners have difficulties in diagnosing and treating depression. The point prevalence of major depressive disorder in general hospital setting care is higher than 10%. Concomitant depression increases the morbidity and mortality from concurrent medical illness. Depression increases the risk for cardiac illness, diabetes, hypertension, etc. Depressed patients have three times higher risk of developing MI compared to people not having depression.
Mood disorders, as highly prevalent and lethal disorders, must command a greater share in the clinical curriculum. Depressive disorders can be easily diagnosed at the primary care level and do not require any special investigations or hi-tech equipment. They can be detected early and managed very effectively by a primary care doctor, with a wide array of effective and safe medications available at reasonable cost. The challenge is to provide all primary care physicians with the requisite hands-on experience in this prevalent group of disorders. Emphasis on training in psychiatry during undergraduate medical training remains an issue of immediate attention.
It is highly imperative that Depressive Disorder be considered an issue of public health importance to provide effective treatment to the patients and to reduce the burden of disease on the nation.
REFERENCES
- 1.Chaudhury PK, Deka K, Chetia D. Disability associated with mental disorders. Indian J Psychiatry. 2006;48:95–101. doi: 10.4103/0019-5545.31597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chisholm D, Sekar K, Kumar KK, Saeed K, James S, Mubbashar M, et al. Integration of mental health care into primary care: Demonstration cost-outcome study in India and Pakistan. Br J Psychiatry. 2000;176:581–8. doi: 10.1192/bjp.176.6.581. [DOI] [PubMed] [Google Scholar]
- 3.Das M, Gupta N, Dutta K. Psychiatric training in India. Psychiatr Bull. 2002;26:70–2. [Google Scholar]
- 4.Druss BG, Rosenheck RA, Sledge WH. Health and disability costs of depressive illness in a Major U.S. Corporation. Am J Psychiatry. 2000;157:1274–8. doi: 10.1176/appi.ajp.157.8.1274. [DOI] [PubMed] [Google Scholar]
- 5.Greden JR. The burden of recurrent depression: Causes, consequences and future prospects. J Clin Psychiatry. 2001;62:5–9. [PubMed] [Google Scholar]
- 6.Gupta R, Narang RL. Training general practitioners in psychiatry. Indian J Psychiatry. 1987;29:349–52. [PMC free article] [PubMed] [Google Scholar]
- 7. [last cited on 2010]. Available from: http://www.who.int/gho/mortality_burden_disease/en/index.html .
- 8. [last cited on 2010]. Available from: http://www.who.int/mental_health/management/depression/definition/en/
- 9.Kapur RL. Mental health care in rural India: a study of existing patterns and their implications for future policy. Br J Psychiatry. 1975;127:286–93. doi: 10.1192/bjp.127.3.286. [DOI] [PubMed] [Google Scholar]
- 10.Katon WJ. Collaborative care: evidence-based models that improve primary care depressive outcomes. CNS Spectr. 2009;14:10–3. doi: 10.1017/s1092852900024652. [DOI] [PubMed] [Google Scholar]
- 11.Kermode M, Bowen K, Arole S, Joag K, Jorm AF. Community beliefs about treatments and outcomes of mental disorders: A mental health literacy survey in a rural area of Maharashtra, India. Public Health. 2009;123:476–83. doi: 10.1016/j.puhe.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Mehta P, Josep A, Verghese A. An epidemiologic study of psychiatric disorders in a rural area in Tamil Nadu. Indian J Psychiatry. 1985;27:153–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Neki JS. Psychotherapy in India. Indian J Psychiatry. 1977;19:1–10. [Google Scholar]
- 14.Patel V, Pereira J, Coutinho L, Fernandes R. Is the labelling of common mental disorders as psychiatric illness clinically useful in primary care? Indian J Psychiatry. 1997;39:239–46. [PMC free article] [PubMed] [Google Scholar]
- 15.Patel V, Pereira J, Coutinho L, Fernandes R, Fernandes J, Mann A. Poverty, psychological disorder and disability in primary care attenders in Goa, India. Br J Psychiatry. 1998;172:533–6. doi: 10.1192/bjp.172.6.533. [DOI] [PubMed] [Google Scholar]
- 16.Patel V, Rahman A, Jacob KS, Hughes M. Effect of maternal mental health on infant growth in low income countries: New evidence from South Asia. BMJ. 2004;61:946–52. doi: 10.1136/bmj.328.7443.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel V. Social origin, biological treatments: the public health implications of common mental disorders in India. Indian J Psychiatry. 2005;47:15–20. [Google Scholar]
- 18.Regier DA, Hirschfeld RM, Goodwin FK, Burke JD, Jr, Lazar JB, Judd LL. The NIMH Depression Awareness, Recognition, and Treatment Program: Structure, aims, and scientific basis. Am J Psychiatry. 1988;145:1351–7. doi: 10.1176/ajp.145.11.1351. [DOI] [PubMed] [Google Scholar]
- 19.Ustun TB, Ayuso-Mateos JL, Chatterji S, Mathers C, Murray CJ. Global burden of depressive disorders in the year 2000. Br J Psychiatry. 2004;184:386–92. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]
- 20.Varma VK, Das MK. Mental Illness in India: epidemiology, manifestations and outcome. Indian J Soc Psychiatry. 1995;11:16–25. [Google Scholar]
- 21.Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, et al. The functioning and well-being of depressed patients.Results from the Medical Outcomes Study. JAMA. 1989;262:914–9. [PubMed] [Google Scholar]


