Abstract
Mutism, defined as an inability or unwillingness to speak, resulting in an absence or marked paucity of verbal output, is a common clinical symptom seen in psychiatric as well as neurology outpatient department. It rarely presents as an isolated disability and often occurs in association with other disturbances in behavior, thought processes, affect, or level of consciousness. It is often a focus of clinical attention, both for the physician and the relatives. Mutism occurs in a number of conditions, both functional and organic, and a proper diagnosis is important for the management. We hereby present three cases, who presented with mutism as the presenting symptom and the differential diagnosis and management issues related to these cases are discussed. The authors also selectively reviewed the literature on mutism, including psychiatric, neurologic, toxic-metabolic, and drug-induced causes.
Keywords: Differential diagnosis, mutism, presenting symptom
INTRODUCTION
Mutism is defined as an inability or unwillingness to speak, resulting in the absence or marked paucity of verbal output. It is a common presenting symptom seen in various disorders, including psychiatric as well as medical disorders. Though, it often is the main focus of clinical attention, both for the patients and the treating physicians, it rarely presents as an isolated disability and often occurs in association with other disturbances in behavior, thought processes, affect, or level of consciousness. Despite its association with a variety of neuropsychiatric disorders, mutism has received relatively little attention in the psychiatric literature.[1,2] Mutism occurs in a number of conditions, both functional and organic, and a proper diagnosis is important for the management. We hereby present three cases, who presented with mutism as the presenting symptom and the differential diagnosis and management issues related to these cases are discussed. The literature on mutism, including psychiatric, neurologic, toxic-metabolic, and drug-induced causes, is also selectively reviewed.
CASE REPORTS
Case A
A 26-year-old unmarried male educated upto high school presented with abrupt onset progressive complaints of not speaking at all and decreased oral intake for the past 2 days. The symptoms started after the patient had an altercation with his brother. This was also associated with anxiety symptoms and hiccups that would occur in episodes for hours together. There was no other significant history suggestive of any organicity or psychosis, mood disorder, or any history of substance use. The patient had past history of an episode of acute stress reaction with mutism around 7 years back when he witnessed murder of his friend. Also, he would have episodes of mutism in between lasting few hours to 1 day around three to four times in the last 3 years. His family and personal history were non-significant. He had submissive and dependant traits in his pre-morbid personality. Positive findings in the mental status examination (MSE) were that the patient was following commands given to him, he would respond in non-verbal manner or by writing, his eyes were open and movements were normal, he would cough and clear throat when asked to do so, would have hiccups (around 20 times in interview of around 30 min), and his psychomotor activity (PMA) was decreased. He was mute through out the interview. All his routine investigations were normal. A diagnosis of dissociative (conversion) disorder-motor type was made and the patient was started on sertraline 50 mg per day along with chlorpromazine 100 mg per day. He was engaged in supportive psychotherapy and suggestion under pentothal was given and patient showed improvement in symptoms. His ongoing life stressors were discussed and coping skill enhancement was done. He was subsequently discharged and had been maintaining well for the past 9 months of follow up.
Case B
A 29-year-old unmarried male was brought by police personnel with acute onset complaints of not speaking for 9 and a half months and history of irrelevant talks for 2 weeks associated with inability to speak in between. The patient had been under trial for the last 3 years for alleged charge of rape and murder. The patient would generally prefer to remain quiet when asked about any thing. He would ask for his daily requirements by gestures/writing down. He would however maintain his routine daily chores and his vegetative functions were maintained. MSE revealed a young male with little speech output and occasional irrelevant talks in between. On formal questioning, he reported sadness of mood but did not reply to other questions asked. A provisional diagnosis of depressive stupor versus dissociative stupor was kept and started on imipramine 50-125 mg per day along with risperidone 2 mg per day and lorazepam 1.5 mg per day in divided doses. Inj. lorazepam 4 mg was given on stat basis, with no improvement in his symptoms. Cat scan head plain and contrast was also normal. On evaluation, he would follow simple commands and was able to write properly on persuasion. He would show appropriate facial expressions. He did not respond to suggestions given. He would speak out of the context and would start quarreling with jail inmates for no apparent reason. Risperidone was increased without any response and he was subsequently admitted. No other significant history could be elicited. History from patient's father was also taken and no pervious history of psychiatric illness or substance use other than tobacco was obtained. There was no family history of any psychiatric illness. On admission, it was observed that the patient had rashes present on dorsum of left hand. MSE revealed that eye contact could be established but not maintained, decreased PMA, his speech was decreased in output but was clear and comprehensible, his mood was sad but affect appeared euthymic with full range as shown by facial expressions. He would also on occasions give approximate answers to various questions asked (e.g. date: said 10th instead of 9th, month: said December instead of November,). He would be able to comprehend simple things. He would be able to write what was given to him. All his routine blood investigations were within normal limits. Observing him unobserved did not reveal any abnormality in behavior. Though, he would talk irrelevantly and would give wrong/approximate answers when talked too. Information from collateral sources revealed that he was told to behave in this manner to plead his case. A diagnosis of malingering was made. Skin opinion was taken and a diagnosis of factitious dermatitis was made which further supported our diagnosis. The patient was confronted,and was explained the possible outcome of his behavior. All his medicines were tapered and there were no relapse of symptoms.
Case C
A 35-year-old married male was brought by police personnel with chief complaints of not speaking for the last 3 months. The patient had been under trial for the last 6 months for the alleged charge of setting fire in a cowshed. He would not interact with any of the jail inmates. He would however ask for food by non-verbal communication/gestures and would perform all his daily chores normally as reported. He was asked to follow up with family members. History reviewed from wife and elder brother reveled history of 18 years history characterized by violent abusive behavior, wandering behavior, irritability, decreased sleep, restlessness, muttering to self, and at times reporting that other would harm him, associated with withdrawn behavior and socio-occupational dysfunction. On one occasion, he became mute also and did not talk for a period of around 4 months associated with sadness of mood and decreased interest in surroundings. 6 months back, he had symptoms of muttering to self, would often roam about naked and get irritable on minor issues. No other significant history was obtained. MSE revealed decreased PMA, rapport not established, eye to eye contact could not be maintained, he was mute and would communicate nonverbally appropriately. His affect was blank with no facial expressions. All his routine investigations were within normal limits. A diagnosis of schizophrenia was entertained, and he was started on risperidone 6 mg per day and lorazepam 4 mg per day. Gradually the patient started showing improvement in symptoms.
DISCUSSION
Proper diagnosis is important for management. Firstly, it is important to distinguish between various disorders of speech. Some of these besides mutism are as follows:
Aphonia: Defined as the absence of definable laryngeal tone i.e. loss power of vocal chords to adduct.
Aphasia: This is a disorder of the content of speech, seen generally in organic conditions and occasionally as gargon aphasia in schizophrenia
Dysarthria: A motor speech disorder characterized by difficulty in articulation of speech. Any of the speech subsystems (respiration, phonation, resonance, prosody, articulation and movements of jaw and tongue) can be affected.
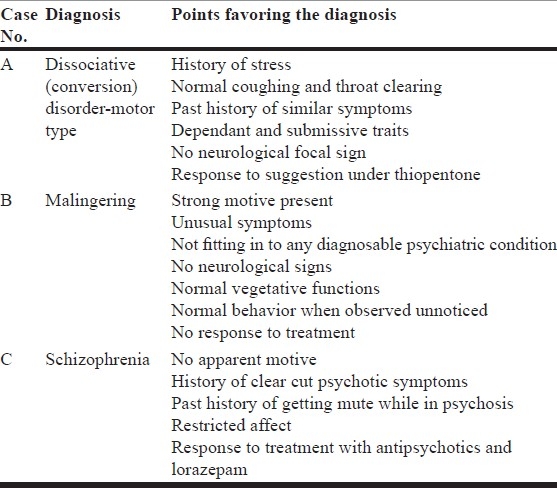
All of our patients had no signs or symptoms suggestive of organicity. One important aspect in case B was that one should keep a possibility of malingering in such group of patients. Though case C was also brought by police personnel and was under trial, he had past history of psychotic illness and also his crime was not that serious/grave as compared to case B. The points favoring our diagnosis in respective cases have been summarized in Table 1.
Table 1.
Summary of the cases
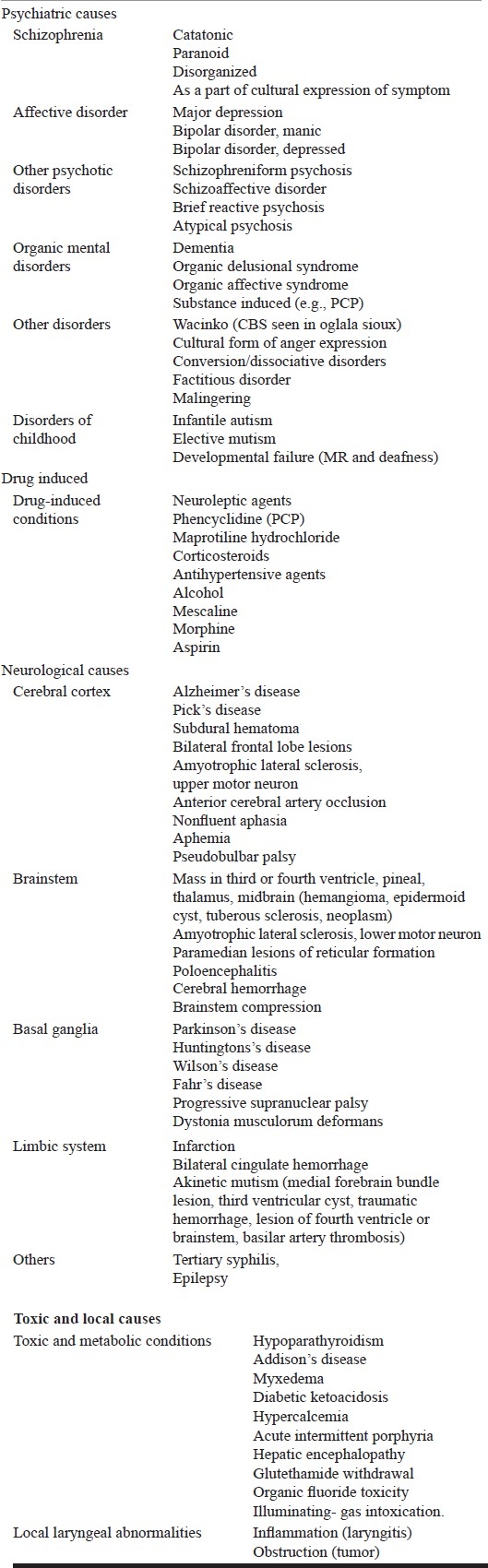
Besides psychiatric causes, there are other many causes of mutism. Some of these are summarized in Table 2.
Table 2.
Differential diagnosis of mutism
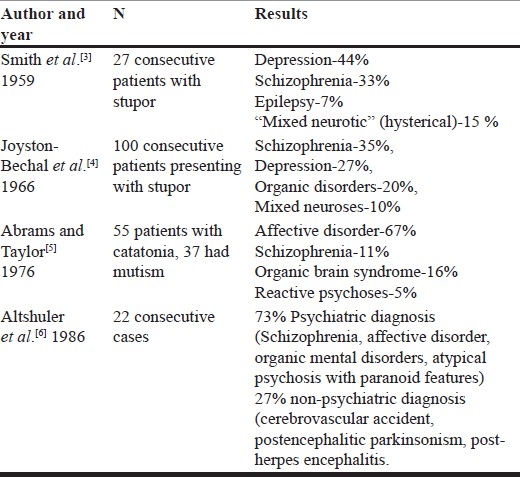
Regarding the frequency of various causes of mutism, besides case reports describing mute patients, there are few studies that report a series of patients presenting with mutism and describing various diagnostic categories. Some of these studies are summarized in Table 3.
Table 3.
Frequency of causes for mutism
Proper history is important to reach a diagnosis. One must perform a thorough physical and systemic examination to rule out organic causes for mutism.
Also, at times, observation for some time period may be warranted and should be done to reach final diagnosis.
The utility of pentothal interview[7] in some cases can be therapeutic also as in our case A. Besides being a useful tool to differentiate organic from functional conditions, it can be used to give suggestions and thus help in the immediate management of dissociative disorders.
To conclude, it is important to recognize the correct cause for proper management of mutism. Though our cases had psychiatric cause for mutism, one must have a high index of suspicion and look for various other non-psychiatric causes for mutism, as this will decide the management and prognosis of the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: The cases were presented as a poster presentation in the 62th Annual Conference of Indian Psychiatric Society, held at Jaipur, in January, 2010.
REFERENCES
- 1.Kaplan HI, Sadock BJ, editors. Comprehensive textbook of psychiatry. 9th ed. New York: Williams and Wilkins; 2009. [Google Scholar]
- 2.MacKinnon RA, Michels R. The psychiatric interview in clinical practice. Philadelphia: WB Saunders; 1971. [Google Scholar]
- 3.Smith S. An investigation and survey of twenty-seven cases of akinesis and mutism (stupor) J Ment Sci. 1959;105:1088–94. doi: 10.1192/bjp.105.441.1088. [DOI] [PubMed] [Google Scholar]
- 4.Joyston-Bechal MP. The clinical features and outcome of stupor. Br J Psychiatry. 1966;112:967–81. doi: 10.1192/bjp.112.491.967. [DOI] [PubMed] [Google Scholar]
- 5.Abrams R, Taylor MA. Catatonia, a prospective clinical study. Arch Gem Psychiatry. 1976;33:579–82. doi: 10.1001/archpsyc.1976.01770050043006. [DOI] [PubMed] [Google Scholar]
- 6.Altshuler LL, Cummings JL, Mills MJ. Mutism: review, differential diagnosis, and report of 22 cases. Am J Psychiatry. 1986;143:1409–14. doi: 10.1176/ajp.143.11.1409. [DOI] [PubMed] [Google Scholar]
- 7.Sbrigho R. The amytal interview in emergency and psychiatric settings. Hosp Physician. 1984;22:91–9. [Google Scholar]


