Abstract
The glenohumeral joint is the most commonly dislocated joint in the body, and anterior instability is the most common type of shoulder instability. Depending on the etiology and the age of the patient, there may be associated injuries, for example, to the anterior-inferior labro-ligamentous structures (in young individuals with traumatic instability) or to the bony components (commoner in the elderly), which are best visualized using MRI and MR arthrography. Anterior instability is associated with a Bankart lesion and its variants and abnormalities of the anterior band of the inferior glenohumeral ligament (IGHL), whereas posterior instability is associated with reverse Bankart and reverse Hill-Sachs lesions. Cases of multidirectional instability often have no labral pathology on imaging but show specific osseous changes including increased chondrolabral retroversion. This article reviews the relevant anatomy in brief and describes the MRI findings in each type, with the imaging features of the common abnormalities.
Keywords: Bankart lesion, Glenohumeral instability, magnetic resonance arthrogram, magnetic resonance imaging
Introduction
The glenohumeral joint is the most mobile and most commonly dislocated joint in the body, and shoulder instability is a common clinical problem, especially in young active individuals. Glenohumeral instability can be classified in many ways,[1] for example, (a) according to degree (subluxation vs dislocation), (b) acute vs recurrent, (c) with respect to direction, i.e., unidirectional (when it may be anterior, posterior, or inferior) or multidirectional or gross instability.
Anterior shoulder instability is much more common than posterior instability.[2] The presentation of patients with posterior shoulder instability is with pain and a click on the posterior aspect of the shoulder.[3,4]
Instability can also be classified according to the etiology, i.e., traumatic or atraumatic.[5]
Relevant anatomy
The shoulder joint is a ball and socket type of joint that has two main stabilizers: the rotator cuff muscles (dynamic) and the labral-ligamentous complex (static). The primary function of the rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) is to centralize the humeral head, limiting superior translation during abduction.[6]
The glenoid labrum is the ring of fibrocartilage (triangular in cross-section) that provides attachment to the glenohumeral ligaments and the capsule at the glenoid rim and deepens the glenoid fossa. The normal glenoid labrum height and width are 3 mm and 4 mm, respectively, but the shape and size are subject to considerable variation.[6]
The rotator cuff interval (RCI) refers to the discontinuity of the rotator cuff seen between the superior border of the subscapularis and the anterior border of the supraspinatus tendon, which results from interruption of the rotator cuff by the coracoid process.[7]
Imaging technique
MRI arthrography (MRA) is the imaging method of choice in shoulder instability, especially recurrent instability in the young,[1] where labro-ligamentous pathologies are common. Direct MRA is a two-phase procedure in which intra-articular injection of contrast material (1:200 diluted gadolinium-based contrast material) is performed under image guidance, followed by transfer of the patient to the MRI scanner for diagnostic imaging. Abduction and external rotation (ABER) positioning increases the sensitivity and specificity for the detection of anteroinferior labral and glenohumeral ligament attachment abnormalities.[8]
Findings in anterior instability
MRI in anterior instability can reveal a large number of abnormalities affecting the soft tissue and the bony constituents of the joint [Table 1].
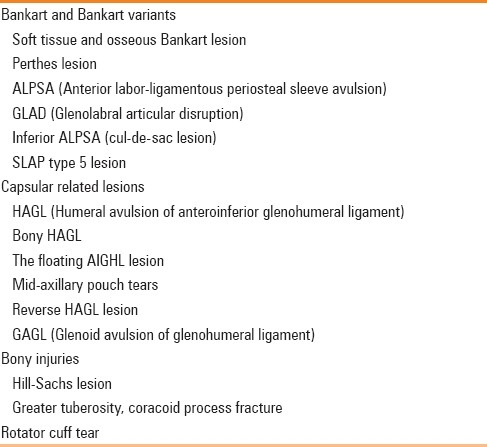
Table 1.
Imaging findings associated with anterior instability
Classic and bony Bankart lesion
Bankart lesion, an avulsion of the anterior-inferior glenohumeral ligament and labral complex from the glenoid rim, with rupture of the scapular periosteum [Figures 1–3], results from injury to the anterior-inferior labro-ligamentous structures in anterior dislocations.[9–11] It can either be purely cartilaginous or may involve the underlying bone also.
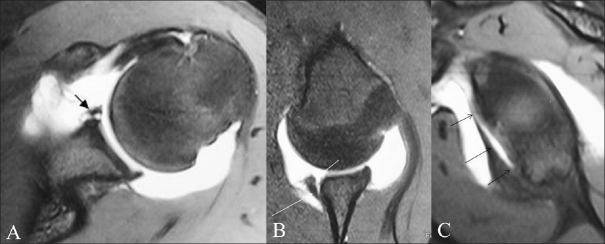
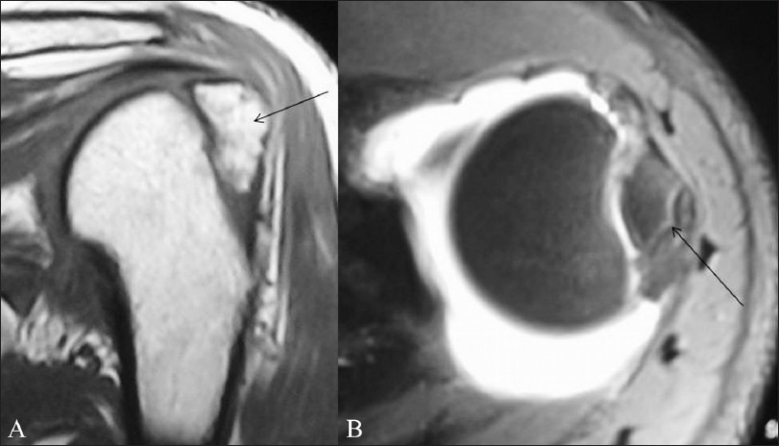
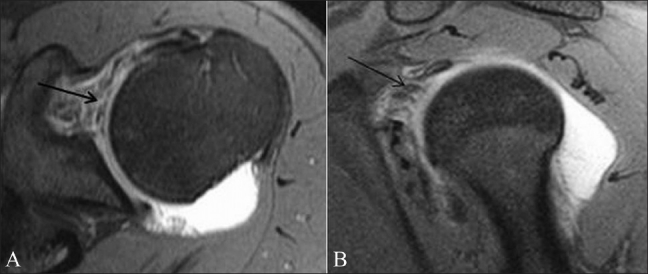
Figure 1 (A,B).
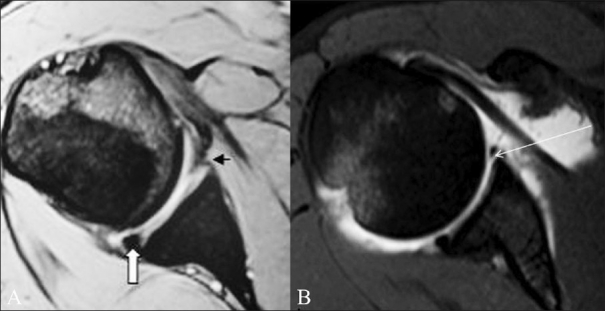
Classic Bankart lesion. A 36-year-old male presented with recurrent anterior shoulder dislocation. Conventional axial GRE MEDIC T2W MRI image (A) shows an attenuated anteroinferior labrum (small arrow). The posterior labrum appears intact and is triangular in shape (thick arrow). TSE T1W fat-saturated axial MRA image (B) shows a classic Bankart lesion as intercalation of contrast material (long arrow) beneath the hypointense anteroinferior labrum
Figure 3 (A-C).
Bony Bankart lesion in a 28-year-old male with recurrent anterior shoulder dislocation. Axial TSE T1W fat-saturated MRA image (A) shows an absent anteroinferior labrum with bony injury (arrow). Sagittal TSE T1W fat-saturated MRA (B) and sagittal MRA image (C) 5 mm medial to B, show the full extent of the bony Bankart lesion (arrow)
Figure 2.
TSE T1W fat-saturated sagittal MRA image shows a classic Bankart lesion (arrow) and its extent
In Bankart repair, the labral fragment is sutured back to the glenoid rim using suture anchors. Preoperative imaging can delineate the exact extent of the injury in these cases, thereby providing an estimate of the severity of the injury and the level of difficulty to be anticipated by the operating surgeon and also the number of anchors to be used in the procedures.
Bony Bankart lesions are treated by bony Bankart repair or “bony Bankart bridge procedure.” Preoperative imaging can help delineate the extent of bone loss and can be done using CT scan but is also well documented with MRI. MRI has the added advantage of being able to detect the labrocapsular and tendinous pathologies as well.
Chronic bony Bankart lesions with resorption of the detached fragment may need bone grafting and therefore exact assessment of the bony fragment is important.
Perthes lesion
Perthes lesion is a variant of Bankart lesion where there is a tear of the glenoid labrum, with an intact scapular periosteum. There is only minimal displacement of the torn anterior labrum, and hence the lesions are difficult to diagnose on routine MRI or MRA. MRA with arm in ABER stretches the anteroinferior joint capsule and IGHL and helps in better delineation of the lesion.[12,13] [Figure 4] It is important to detect this on MRA as it can be missed on arthroscopy because of the minimal displacement.
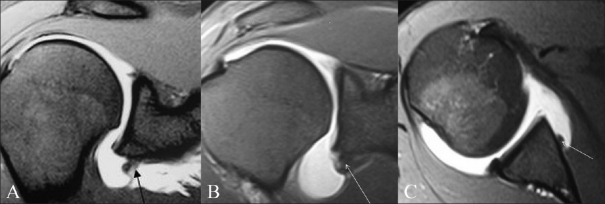
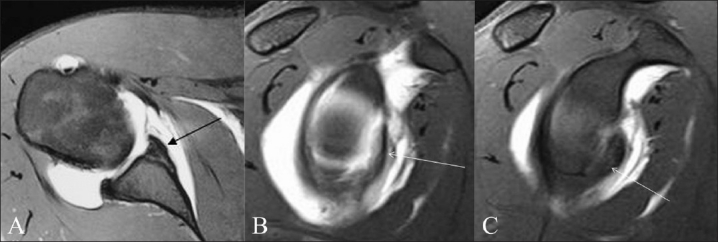
Figure 4 (A-C).
Perthes lesion. A 16-year-old male presented with post-traumatic recurrent anterior shoulder dislocation. TSE T1W fat-saturated axial MRA image (A) and TSE T1W fat-saturated oblique axial MRA image with arm in ABER position (B) show intercalation of intra-articular contrast beneath the anterior labrum (small arrow) with an intact scapular periosteum (long arrow); this suggests a diagnosis of Perthes lesion. TSE T1W fat-saturated oblique sagittal MRA image (C) shows the extent of the lesion (arrows)
Anterior labroligamentous periosteal sleeve avulsion (ALPSA)
ALPSA lesion was first defined by Neviaser et al.[13] as avulsion and medial rolling of the inferior labro-ligamentous complex along the scapular neck [Figure 5]. This is an important diagnosis to make as the lesion can be easily missed on arthroscopy.[10] An ALPSA lesion, during an operative procedure, needs to be converted to a Bankart lesion (reapposition of the medially rolled labrum to the glenoid rim) followed by a Bankart repair. The procedure needs relatively more expertise and more operating time. Preoperative knowledge of the severity of the lesion is useful for the operating surgeon.
Figure 5 (A-C).
ALPSA lesion in three different patients with anterior shoulder instability. TSE T1W fat-saturated coronal MRA images (A,B) and axial MRA image (C) show the anteroinferior labrum and antero-inferior glenohumeral ligament rolled back medially along the scapular neck (arrow)
Glenolabral articular disruption (GLAD)
As described by Neviaser[14] a GLAD lesion consists of a superficial anterior-inferior labral tear associated with an anterior-inferior articular cartilage injury [Figure 6]. The use of intra-articular contrast in the MRA helps to visualize small tears at the level of the anterior-inferior glenoid rim. GLAD lesions are usually not a cause of instability unless associated with other labral pathologies. They can present with clicking during shoulder joint movement.
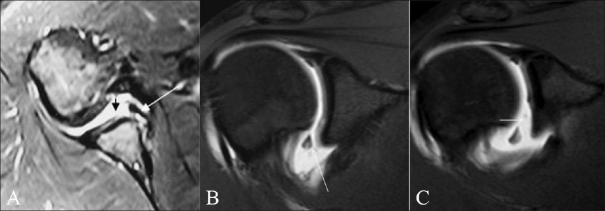
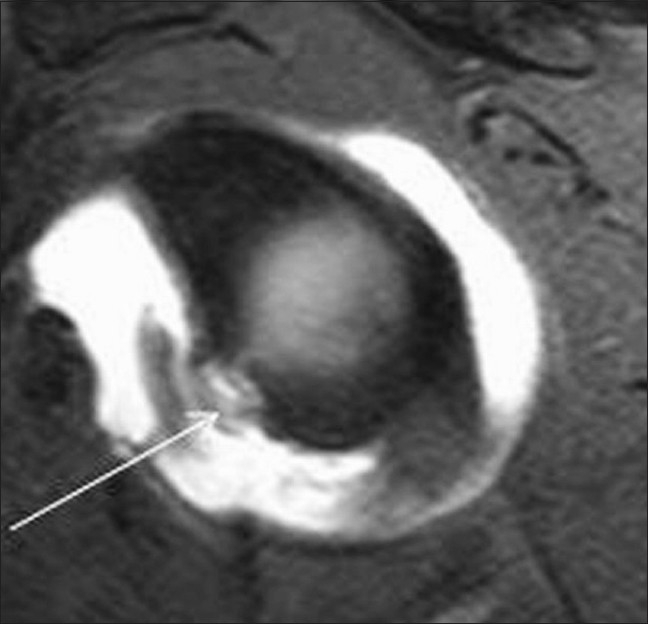
Figure 6 (A-C).
GLAD lesion in an 18-year-old male student. TSE T2W fat-saturated axial conventional MRI image (A) and coronal TSE T1W fat-saturated MRA images (B,C) show anterior-inferior labral injury (long arrow) with an articular cartilage defect (small arrow)
Superior labral anterior posterior (SLAP) type 5 lesion
The SLAP lesion, described by Snyder et al,[15] is an injury involving the superior aspect of the glenoid labrum, which includes the biceps tendon anchor. SLAP tears were initially classified by Snyder et al. into four distinct but related types of lesions. Maffet et al.[16] added three more types. Currently, ten types or patterns are recognized.[16,17] A sagittal MRI or MRA can demonstrate the complete extent of the labral tear [Figure 7].
Figure 7.
Type 5 SLAP lesion in a patient with recurrent anterior instability. Sagittal TSE T1W fat-saturated MRA image shows an anterior labral tear (small arrow) involving almost the whole of the anteroinferior labrum continuous with a SLAP lesion (long arrow)
Humeral avulsion of glenohumeral ligament (HAGL) lesion
HAGL lesions are much less common than Bankart lesions as a cause of anteroinferior instability.[18] On MRA, or in the presence of a joint effusion, the normal distended axillary pouch is a U-shaped structure, which changes into a J-shape as the anterior band of the inferior glenohumeral ligament (IGHL) droops inferiorly [Figure 8].
Figure 8.
Humeral avulsion of the glenohumeral ligment (HAGL). Coronal TSE T1W fat-saturated MRA image shows avulsion of the humeral attachment of the inferior glenohumeral ligament (arrow); note the loss of the normal U-shape of the axillary recess
Bony humeral avulsion of the glenohumeral ligaments (BHAGL) lesion
In BHAGL lesion, there is a small avulsed osseous fragment attached to the torn end of the humeral attachment of the IGHL.[19]
Glenoid avulsion of the glenohumeral ligaments (GAGL) lesion
Glenoid avulsion of the glenohumeral ligaments (GAGL) implies an avulsion of the IGHL from the inferior pole of the glenoid, without an associated inferior labral disruption[7] [Figure 9].
Figure 9.
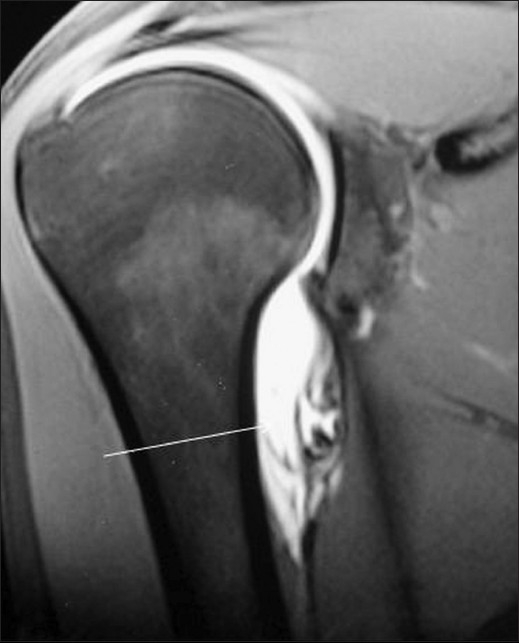
GAGL lesion. A 35-year-old male presented with recurrent anterior shoulder dislocation. Coronal STIR MRI image shows that the antero-inferior labrum is intact (small arrow) but the anterior band of the IGHL is avulsed at its glenoid attachment (long arrow). Also note the hyperintensity involving the supraspinatus tendon (arrowhead) and the fluid in the subdeltoid bursa (block arrow). The patient also had a full-thickness supraspinatus tendon tear
Inferior ALPSA or cul-de-sac lesion
In this entity, there is medial displacement of both the anterior-inferior labrum and the IGHL under the inferior neck of the glenoid. On coronal MRI images, there is characteristic greater medial displacement of the capsule (and IGHL) relative to the antero-inferior labrum[6] [Figure 10].
Figure 10.
Inferior ALPSA lesion (cul-de-sac lesion). Coronal TSE T1W fat-saturated MRA image shows avulsion and medial displacement of the anterior-inferior labrum (small arrow). The avulsed anterior band of the IGHL is more medially displaced (long arrow) relative to the avulsed labrum
Hill-Sachs lesion
Hill-Sachs lesion consists of bony injury [Figure 11] to the posterosuperior humeral head as a result of inferior displacement. In Hill-Sachs and reverse Hill-Sachs lesions, preoperative determination of the extent of bone loss is surgically important as greater than 30% loss increases the chance of repeated dislocations and necessitates bone grafting.
Figure 11.
Hill-Sachs lesion (arrow) seen as a bony defect in the posterosuperior humeral head on an axial GRE MEDIC T2W MRI image
Greater tuberosity fractures are also associated with traumatic anterior instability [Figure 12]. Rotator cuff tears [Figure 13] associated with anterior and inferior glenohumeral dislocation are commoner in the elderly.
Figure 12 (A-B).
Coronal TSE T1W MRI (A) and axial TSE T1W fat-saturated MRA (B) images show a comminuted greater tuberosity fracture (arrow) in this 38-year-old male presenting with traumatic shoulder instability
Figure 13.

Coronal TSE T1W fat-saturated MRA image of the same patient as in Figure 8 shows a full-thickness supraspinatus tendon tear with retraction (arrow)
Findings in posterior instability
Less common than anteroinferior instability, posterior instability represents only 2%–4% of instability cases.[20] It can occur as a component of multidirectional instability (MDI) as well as after trauma. The prevalence of posterior labral tears in patients with posterior instability is less and more variable. Ligamentous abnormality involving the posterior band of the inferior glenohumeral ligament may be seen in isolation or in posterior or anteroinferior instability.[21]
The MRI findings in posterior instability are enumerated in Table 2.
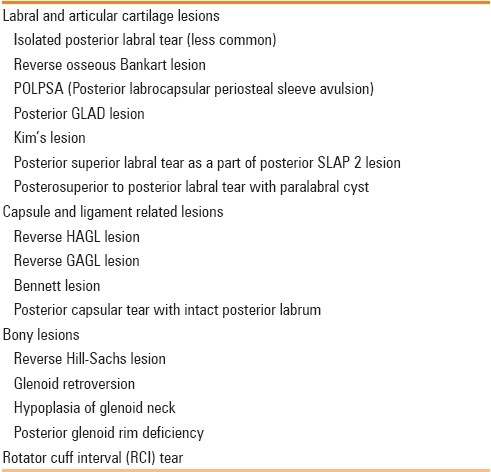
Table 2.
Imaging findings in posterior glenohumeral instability
Reverse Hill-Sachs lesion
This consists of an anteromedial superior humeral head impaction fracture [Figure 14] that is often associated with a reverse Bankart lesion [Figure 14] (posterior glenoid labrum disruption).
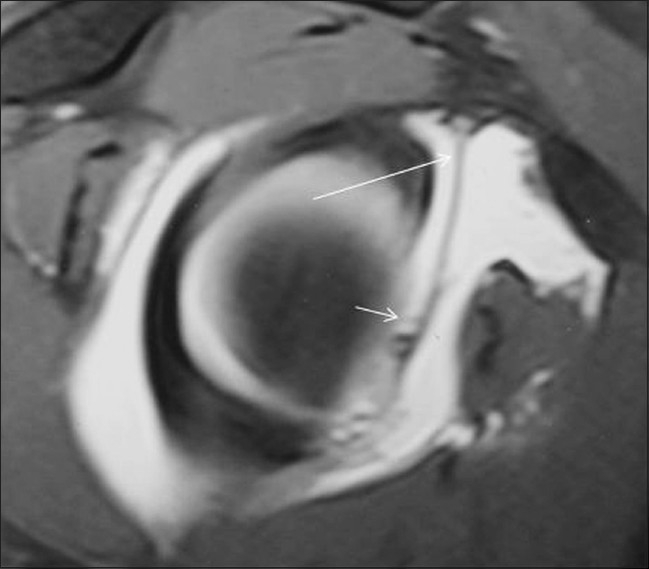
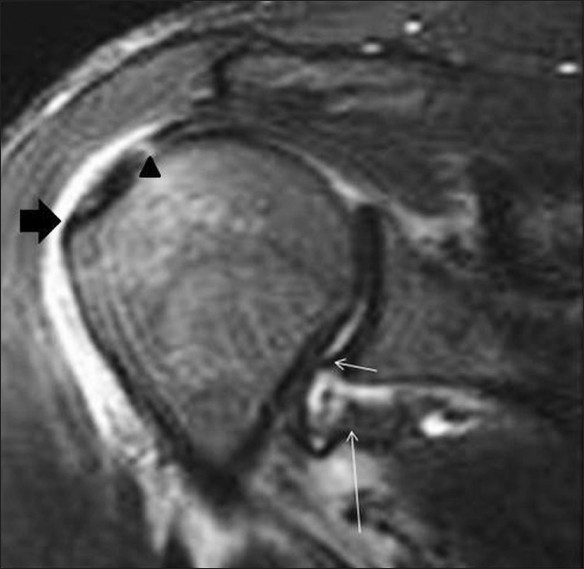
Figure 14 (A-B).
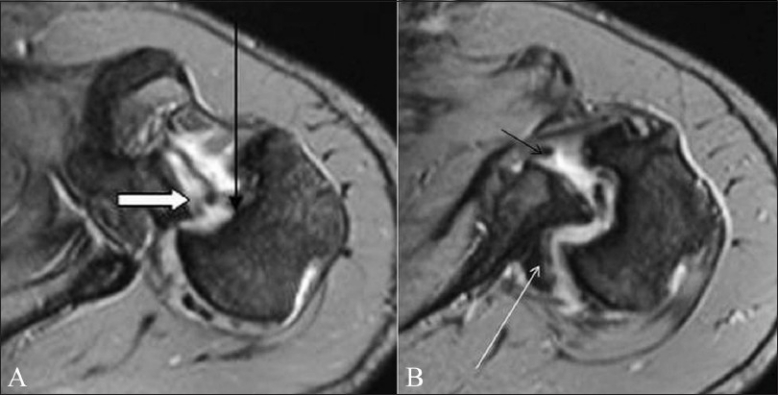
Reverse Hill-Sachs and reverse Bankart lesion in a 34-year-old male who had multidirectional instability with a posterior dislocation at presentation. Axial TSE T1W fat-saturated MRA images (A,B) show a reverse Hill-Sachs lesion (long arrow) as a bony defect in the anterior humeral head. A posterior labral tear is indicated with a thick arrow. The patient also had an anterior labral tear (small arrow in B) and a Hill-Sachs lesion from previous anterior dislocations. A Bennett lesion is seen as ossification, posteriorly along the scapular neck (long arrow in B)
Reverse HAGL lesion
In posterior instability there is sometimes complete avulsion of the posterior attachment of the shoulder capsule and the glenohumeral ligament from the posterior humeral neck[22] [Figure 15].
Figure 15.

Reverse HAGL seen as humeral avulsion of the posterior band of IGHL (arrow) in this sagittal TSE T1W fat-saturated MRA image
Posterior GLAD lesion (focal posterior cartilage deficiency)
This lesion has been described recently and can be associated with posterior instability.[23–24]
Posterior glenoid rim deficiency
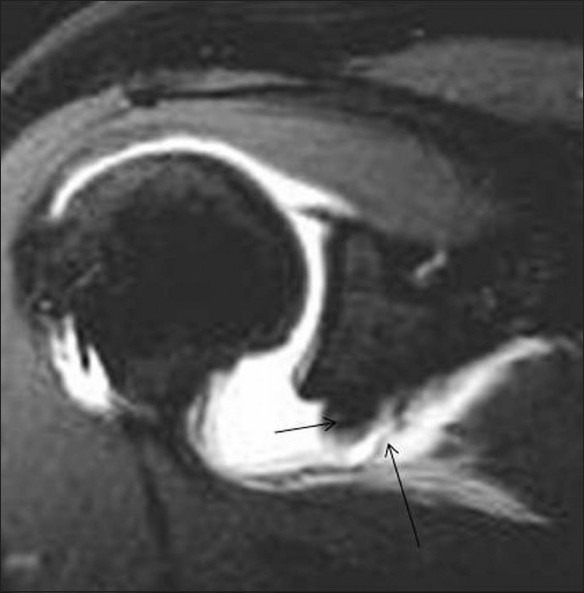
In recurrent posterior instability, two shapes of the posterior-inferior glenoid – the “lazy J” [Figure 16] and the “delta” shapes – are reported to be more often found than in normal subjects.[25]
Figure 16 (A-B).
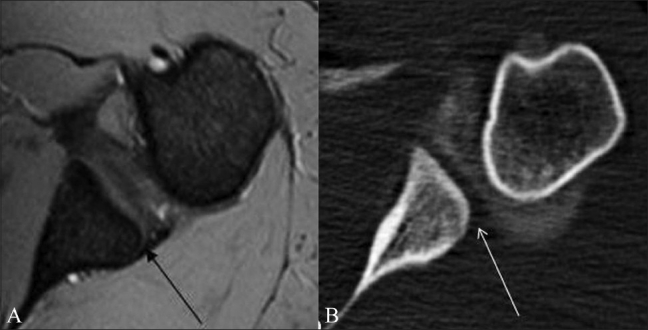
Morphologic abnormality of the posteroinferior glenoid in a patient with posterior instability. Axial GRE MEDIC T2W MRI image (A) and axial CT arthrogram image (B) reveal the “lazy J” deformity; better appreciated on CT scan
Bennett lesion
It is an extra-articular crescentic posterior ossification [Figure 14] associated with posterior labral injury and capsular avulsion. It is best visualized on CT; it may be missed on arthroscopy as it is extra-articular.[6,26]
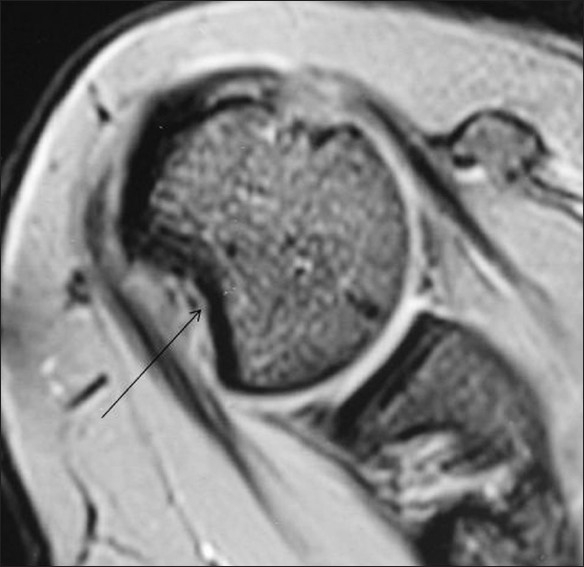
Rotator cuff interval tear
RCI tears typically do not appear as complete disruption of the fibers of its components but as thinning, irregularity, or focal discontinuity of the rotator interval capsule[7] [Figure 17].
Figure 17 (A-B).
Rotator cuff interval (RCI) tear. Axial TSE T1W fatsaturated MRA image (A) and sagittal TSE T1W fat-saturated MRA image (B) show irregularity of the RCI capsule (arrow). Contrast is seen in the subcoracoid recess
Posterosuperior labral tear in association with a paralabral cyst may be seen in patients with posterior instability [Figure 18]. The cysts are almost always associated with labral tears, but the communication with the joint space is often not visualized on MRI.
Figure 18 (A-D).
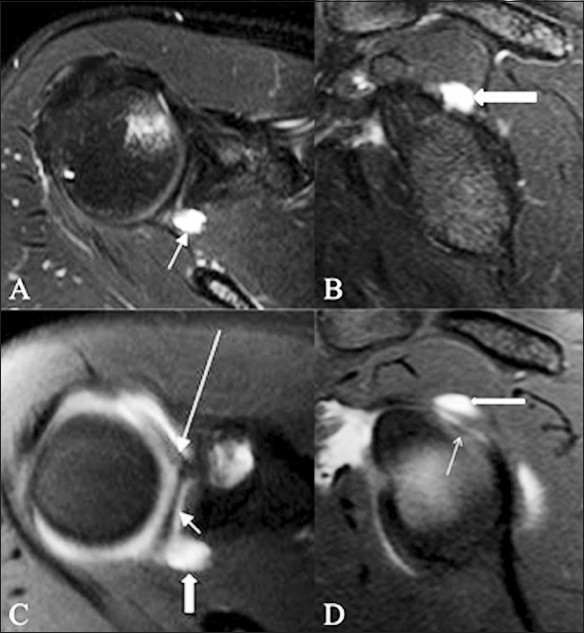
Paralabral cyst. A 22-year-old athlete presented with shoulder pain on overhead throwing movements and instability. TSE T2W fat-saturated axial (A) sagittal (B) MRI images show a welldefined, hyperintense, cystic lesion (arrow) in close relation to the posterosuperior labrum, suggestive of a paralabral cyst. No superior labral pathology is identified. Corresponding axial (C) and sagittal (D) TSE T1W fat-saturated MRA images show a superior labral anteroposterior (SLAP) tear (small arrow); the joint contrast is seen to communicate with the paralabral cyst through the SLAP lesion. The cyst and the insertion of the long head of the biceps tendon are indicated by a thick arrow and a long arrow, respectively
Conclusion
To conclude, the imaging findings in shoulder instability are variable and depend on the etiology of the dislocation as well as the age of the individual. In cases of instability, an MRA is the investigation of choice.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Lynne S, Steinbach, Tirman Philip FJ, Peterfy Charles G, Feller John F. Philadelphia: Lippincott Raven; 1998. Shoulder magnetic resonance imaging. [Google Scholar]
- 2.Bottoni CR, Franjs BR, Moore JH, DeBerardino TM, Taylor DC, Arciero RA. Operative stabilization of the posterior shoulder instability. Am J Sports Med. 2005;33:996–1002. doi: 10.1177/0363546504271509. [DOI] [PubMed] [Google Scholar]
- 3.Vidal LB, Bradley JP. Management of posterior shoulder instability in the athlete. Curr Opin Orthop. 2006;17:164–71. [Google Scholar]
- 4.Fronek J, Warren RF, Bowen M. Posterior subluxation of the glenohumeral joint. J Bone Joint Surg Am. 1989;71:205–16. [PubMed] [Google Scholar]
- 5.Sherbondy PS, McFarland EG. Shoulder instability in the athlete. Phys Med Rehabil Clin N Am. 2000;4:729–43. [PubMed] [Google Scholar]
- 6.Stoller DW. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2007. Magnetic resonance imaging in orthopaedics and sports medicine; pp. 1324–412. [Google Scholar]
- 7.Bigoni BJ, Chung CB. MR imaging of the rotator cuff interval. Magn Reson Imaging Clin N Am. 2004;12:61–73. doi: 10.1016/j.mric.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Cvitanic O, Tirman PF, Feller JF, Bost FW, Minter J, Carroll KW. Using abduction and external rotation of shoulder to increase the sensitivity of MR arthrography in revealing tears of anterior glenoid labrum. AJR Am J Roentgenol. 1997;169:837–44. doi: 10.2214/ajr.169.3.9275908. [DOI] [PubMed] [Google Scholar]
- 9.Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior shoulder instability: Accuracy of MR arthrography in the classification of anterior labroligamentous injuries. Radiol. 2005;237:578–83. doi: 10.1148/radiol.2372041429. [DOI] [PubMed] [Google Scholar]
- 10.Rowan KR, Keogh C, Andrews G, Cheong Y, Forster BB. Essentials of shoulder MR arthrography: A practical guide for the general radiologist. Clin Radiol. 2004;59:327–34. doi: 10.1016/j.crad.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 11.Shankman S, Bencardino J, Beltran J. Glenohumeral instability: Evaluation using MR arthrography of the shoulder. Skeletal Radiol. 1999;28:365–82. doi: 10.1007/s002560050533. [DOI] [PubMed] [Google Scholar]
- 12.Wischer TK, Bredella MA, Genant HK, Stoller DW, Bost FW, Tirman PF. Perthes lesion (a variant of the Bankart lesion): MR imaging and MR arthrographic findings with surgical correlation. AJR Am J Roentgenol. 2002;178:233–7. doi: 10.2214/ajr.178.1.1780233. [DOI] [PubMed] [Google Scholar]
- 13.Neviaser TJ. The anterior labroligamentous periosteal sleeve avulsion lesion: A cause of anterior instability of the shoulder. Arthroscopy. 1993;9:17–21. doi: 10.1016/s0749-8063(05)80338-x. [DOI] [PubMed] [Google Scholar]
- 14.Neviaser TJ. The GLAD lesion: Another cause of anterior shoulder pain. Arthtroscopy. 1993;9:22–3. doi: 10.1016/s0749-8063(05)80339-1. [DOI] [PubMed] [Google Scholar]
- 15.Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–9. doi: 10.1016/0749-8063(90)90056-j. [DOI] [PubMed] [Google Scholar]
- 16.Maffet MW, Gartsman GM, Moseley B. Superior Labrum-Biceps Tendon Complex Lesions of the Shoulder. Am J Sports Med. 1995;23:93–8. doi: 10.1177/036354659502300116. [DOI] [PubMed] [Google Scholar]
- 17.Waldt S, Burkart A, Lange P, Imhoff AB, Rummeny EJ, Woertler K. Diagnostic performance of MR arthrography in the assessment of superior labral anteroposterior lesions of the shoulder. AJR Am J Roentgenol. 2004;182:1271–8. doi: 10.2214/ajr.182.5.1821271. [DOI] [PubMed] [Google Scholar]
- 18.Wolf EM, Cheng JC, Dickson K. Humeral avulsion of glenohumeral ligaments as a cause of anterior shoulder instability. Arthroscopy. 1995;11:600–7. doi: 10.1016/0749-8063(95)90139-6. [DOI] [PubMed] [Google Scholar]
- 19.Oberlander MA, Morgan BE, Visotsky JL. The BHAGL lesion: A new variant of anterior shoulder instability. Arthroscopy. 1996;12:627–33. doi: 10.1016/s0749-8063(96)90205-4. [DOI] [PubMed] [Google Scholar]
- 20.Tung GA, Hou DD. MR arthrography of the posterior labrocapsular complex: Relationship with glenohumeral joint alignment and clinical posterior instability. AJR Am J Roentgenol. 2003;180:369–75. doi: 10.2214/ajr.180.2.1800369. [DOI] [PubMed] [Google Scholar]
- 21.Chung CB, Sorenson S, Dwek JR, Resnick D. Humeral avulsion of posterior band of inferior glenohumeral ligament: MR arthrography and clinical correlation in 17 patients. AJR Am J Roentgenol. 2004;183:355–9. doi: 10.2214/ajr.183.2.1830355. [DOI] [PubMed] [Google Scholar]
- 22.Snyder SJ. Posterior instability, chapter10. In: Snyder SJ, editor. Shoulder arthroscopy. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2003. p. 121. [Google Scholar]
- 23.Srinivasan H, Nagar A, Moro J, Pugh D, Rebello R, O’Neill J. Imaging findings in posterior instability of the shoulder. Skeletal Radiol. 2008;37:693–707. doi: 10.1007/s00256-008-0487-7. [DOI] [PubMed] [Google Scholar]
- 24.Resnick D, Kang HS, Pretterklieber ML. 2nd ed. Philadelphia: Saunders; 2007. Shoulder. Internal derangements of joinys; pp. 713–1122. [Google Scholar]
- 25.Weishaupt D, Zanetti M, Nyffeler RW, Gerber C, Hodler J. Posterior glenoid rim deficiency in recurrent (atraumatic) posterior shoulder instability. Skeletal Radiol. 2000;29:204–10. doi: 10.1007/s002560050594. [DOI] [PubMed] [Google Scholar]
- 26.Ferrari JD, Ferrari DA, Coumas J, Pappas AM. Posterior ossification of the shoulder: The Bannett lesion. Etiology, diagnosis, and treatment. Am J Sports Med. 1994;22:171–5. doi: 10.1177/036354659402200204. [DOI] [PubMed] [Google Scholar]