Abstract
Reviews of the dropout literature note significant attrition from addiction treatment. However, consistent predictors have not been identified and few studies have examined factors related to retention and engagement for women in gender-specific treatment. The current study consisted of 102 women and their partners randomized to individual or couples outpatient alcoholism treatment. Women attended more treatment sessions if they were assigned to individual treatment, older, had fewer symptoms of alcohol dependence, had more satisfying marital relationships, had spouses who drank, and had matched preference for treatment condition. Women were more engaged in treatment (i.e., completed more assigned homework) if they had fewer children at home, fewer alcohol dependence symptoms, later age of onset of alcohol diagnosis, more satisfying marital relationships, and spouses who accepted or encouraged their drinking. Results highlight important associations of treatment and relationship variables with treatment retention and engagement.
Keywords: Alcoholism, Retention, Engagement, Women
Given tightening of resources in the health care system, efforts continue to be made to provide the most effective and efficient treatments for clients with substance use disorders. However, these efforts are hindered by problems with engagement and retention. Treatment attrition results in programs spending considerable resources on individuals who do not subsequently engage in the treatment process. Additionally, clients who do not show up for treatment contribute to staff frustration and burnout.1,2 Further, time in treatment is a predictor of positive outcome among patients with substance use disorders,2,3 and thus, attrition may contribute to poorer outcome compared to clients who remain in treatment. While good retention has clear clinical implications, high rates of attrition also create problems for researchers. In treatment efficacy studies, retention is crucial to addressing the main research questions, as both internal and external validity are compromised by subject attrition.4,5
A number of studies have found that dropout is a major problem in substance abuse treatment, especially during the first 3 months.2, 6–8 Dropout rates of 50%–80% during this time are typical.2 For instance, 56% of clients dropped out before the eight session in a study of treatment for cocaine dependence.9 A similar range of attrition rates is seen for clients in outpatient alcohol treatment, with reports of 52–75% of clients dropping out by the fourth session.6,10
Over the last 30 years, studies have attempted to identify both client and treatment predictors of retention in substance abuse treatment. Client factors include demographic variables (gender, ethnicity, age, education, marital status, social stability, socioeconomic status, and employment status), alcohol/drug use severity and treatment history, legal history, motivation for change, psychopathology, and social network.8,11 There is some evidence that age is related to attrition, with younger clients more likely to drop out of treatment.12,13 Similarly, some evidence suggests that lack of social stability and support are related to treatment attrition. For example, in several studies, clients who are single, living alone, or separated have been found to be more likely to drop out.9,14 Substance use severity, legal status, and psychopathology have not been consistent predictors of treatment attrition.
The research on treatment attrition and gender is mixed. Several studies have shown women to have poorer retention rates than men,15–17 but other studies have found that men were more likely to drop out of treatment than women.18,19 In a recent literature review, Greenfield et al.11 report that, contrary to equivocal results found in smaller-study analyses of gender differences in substance abuse retention, population-based studies suggest no clear gender difference in treatment retention, although different predictors have been associated with attrition in each group. Some have suggested that women have more difficulty engaging in treatment due to gender-specific barriers such as child care, finances, stigma, extreme feelings of depression and guilt, lack of family support for treatment, and difficulty with confrontational types of treatment.20–23 These gender-specific barriers to treatment may also contribute to differences in predictors of treatment retention among males and females.11
In addition to patient characteristics, treatment factors affecting retention have been studied and include the therapeutic alliance, ancillary programming (medical, employment, financial, etc.) offered, counselor characteristics, program barriers, program awareness of dropout as a problem, and treatment modality (individual, couples, group).8,24 Positive therapeutic alliance consistently has been related to lower attrition rates.25–27 Counselor characteristics such as gender and race have not been related to client attrition, but clinician experience has been related to attrition.28 Relatively little research has focused on the relationship between treatment attrition and treatment modality, specifically, couples treatment modality. Generally, the likelihood that participants will enter and complete treatment is significantly increased when spouses or significant others are involved in treatment,29–31 but only a few studies have compared retention in individual and couples treatment. Zweben et al.32 found that couples treatment was associated with better treatment engagement and retention than individual treatment. More recent studies have reported no difference in treatment attendance between individual and conjoint therapy in treatment of male substance use.33, 34
Although treatment retention generally is conceptualized as the converse of treatment dropout and attrition, the construct of engagement in therapy is not as clearly defined. Engagement has been defined as a function of duration of treatment and intensity (i.e., number of individual and group sessions attended in a particular program),35 participation and therapeutic relationship,36 number of sessions attended,37 and motivation.38 Further, definitions of substance abuse treatment engagement specifically in women are lacking. In a study defining engagement as a function of duration and participation intensity, treatment factors (e.g., therapist empathy, ancillary services) were found to explain a higher percent of variance in engagement among women in treatment for drug abuse than client characteristics.35 This result may have been because ancillary treatment services were particularly valuable to women, and provision of additional support allowed women to engage more in treatment. The lack of a clear measure of treatment engagement, the possibility that predictors of engagement might be different for women and men, and the importance of an understanding of process measures for conceptualization of substance abuse treatment models39 all underscore a need for further research in this area.
To date, we are aware of no published studies that have examined the relationship between treatment modality and retention and engagement in a women-specific treatment program for alcohol use disorders (AUDs). The present study was conducted to examine three questions: (1) Will alcohol-dependent women in couples treatment have higher rates of treatment retention and engagement than women in individual treatment? (2) What specific factors are related to women’s retention and engagement in treatment? (3) Do predictors of treatment engagement and retention differ between women in couples treatment and women in individual treatment?
Method
Participants
Participants were 102 women seeking outpatient treatment for alcohol problems and their male spouse or partner (married, cohabitating for at least 6 months, or in a non-cohabitating committed relationship for at least one year). Women were eligible for the study if they were at least 18 years old; in a stable, heterosexual relationship; had a partner willing to participate in treatment and follow up; met criteria for a DSM-IV alcohol abuse or dependence disorder diagnosis in the past 12 months; and used alcohol at least once in the 60 days prior to recruitment. Couples were excluded from the study if either partner exhibited current signs of psychosis or organic brain syndrome, if there was significant domestic violence, or if the woman was physiologically dependent on substances other than alcohol.
Couples were recruited through newspaper advertising and referrals from community outpatient addiction treatment programs, other community agencies, and physicians. A total of 442 individuals made a telephone inquiry about the treatment program and were screened for eligibility. Out of the callers screened, 254, or 57%, were excluded from the study for the following reasons: (1) woman did not meet eligibility criteria (12%), (2) various partner-related reasons (10%), (3) caller did not call back (26%), or (4) inability to determine eligibility (9%). In-person clinical screen interviews were scheduled with the 188 couples that met the initial eligibility criteria. Clinical screen interviews were completed and informed consents were signed by 124 of the scheduled couples (66%). These 124 couples were then scheduled for a baseline research assessment, which was completed by 109 couples (88%). An additional 7 couples dropped out of the study after the baseline assessment, leaving 102 (94%) of the scheduled participants from the baseline assessment that attended at least one treatment session. For more detail on the flow of subject recruitment see McCrady et al. in press.40
Measures
Demographics
Information about subject’s age, ethnicity, employment, years of education, household income, marital status and children living at home was collected in a self-report intake form at the clinical screen interview.
The Time-Line Follow-back Interview41 (TLFB)
The TLFB was used to assess alcohol and drug use for both the woman and her partner in the 3 months prior to the baseline interview to determine: the percentage of days in which alcohol and drugs were consumed (actual days of use divided by days of possible use), the average number of standard drinks (defined as 5 ounces of wine, 12 ounces of regular beer, or 1.5 ounces of 80 proof liquor or equivalent42) consumed on a drinking day, and types of drugs used. Test-retest reliability for the TLFB has been high and correlations of drinkers’ self-report with collateral report have ranged from r = .84 to r = .94.43
The Rutgers Consequences of Use Questionnaire44 (RCU)
The RCU is a 78-item self-report measure that assesses how often the woman and her partner experienced alcohol- and drug-related consequences during the past 6 months. A 0–4 scale is used to measure frequency of occurrence over the previous 6 months of 39 consequences related to various domains including social/familial relationships, physical health, legal problems, and psychological health. Rhines et al.44 reported high internal reliability (Cronbach’s alpha = .94) for alcohol consequences, and acceptable response variability.
Readiness to Change Questionnaire45 (RCQ)
This 12-item self-report measure determines the woman’s stage of readiness to change (precontemplation, contemplation, or action). Items were rated on a 5-point Likert scale from “strongly disagree” to “strongly agree.” Higher scores on the contemplation and action scales, and lower scores on the precontemplation scale indicate a greater readiness to change. A single stage was assigned to the woman based on the stage for which she received the highest score; in the case of a tie, assignment was made to the stage higher on the continuum.46 The RCQ has satisfactory reliability (Cronbach’s alphas range from .73 – .85 and test-retest correlations range from .78 – .86) and validity for the three subscales.46,47 An additional item asked about the woman’s desired drinking goal, which was coded as complete abstinence, time-limited abstinence, or moderated drinking.48
Structured Clinical Interview for DSM-IV49 (SCID-IV)
Current and lifetime Axis I and Axis II diagnoses were assessed according to DSM-IV criteria. Alcohol and drug use diagnoses were assessed as present in the past 30 days and/or in the past year using the alcohol and drug modules of the SCID. Age of onset was determined for any alcohol or drug use diagnosis. The SCID was administered separately to both partners by trained doctoral, masters and bachelors level staff. In a previous study using a mixed gender sample, our lab found the mean inter-rater reliability (kappa) for this instrument to be .87.50 Additionally, good overall inter-rater reliability has been reported for alcohol diagnoses (kappa = .75) and other substance use disorder diagnoses (kappa = .84).51
Profile of Mood States52 (POMS)
The POMS consists of 65 items on which participants rate their mood over the past week. Each item is rated on a 5-point Likert scale. The POMS yields six subscale scores (Tension-Anxiety, Depression-Dejection, Anger-Hostility, Vigor-Activity, Fatigue-Inertia, and Confusion-Bewilderment) and an overall total score. Higher scores indicate more current emotional distress. The POMS has excellent reliability (Cronbach’s alphas range from .84 – .95 and test-retest correlations range from .65 – .74) and validity for the six subscales.52
Dyadic Adjustment Scale53,54 (DAS)
The DAS is a 32-item self-report questionnaire that measures global marital satisfaction and commitment. The women and their partners both completed the DAS. Internal consistency of the DAS has been reported as .9655 and split-half reliability as .88.54 A cutoff score of 100 typically has been used to define “happy” couples; higher scores indicate greater marital satisfaction.
Important People and Activities56 (IPA)
The IPA assesses number of individuals in the subject’s social network. In addition, the IPA asks about the alcohol/drug use of network members as well as the degree to which members of the network are supportive of treatment and abstinence. The drinking status of the partner was categorized as 1) abstinent or in recovery, 2) light drinking, or 3) moderate or heavy drinking. Partner encouragement for drinking was categorized as 1) encouraged or accepted her drinking, 2) neutral, or 3) didn’t accept or left when she was drinking.
Condition preference
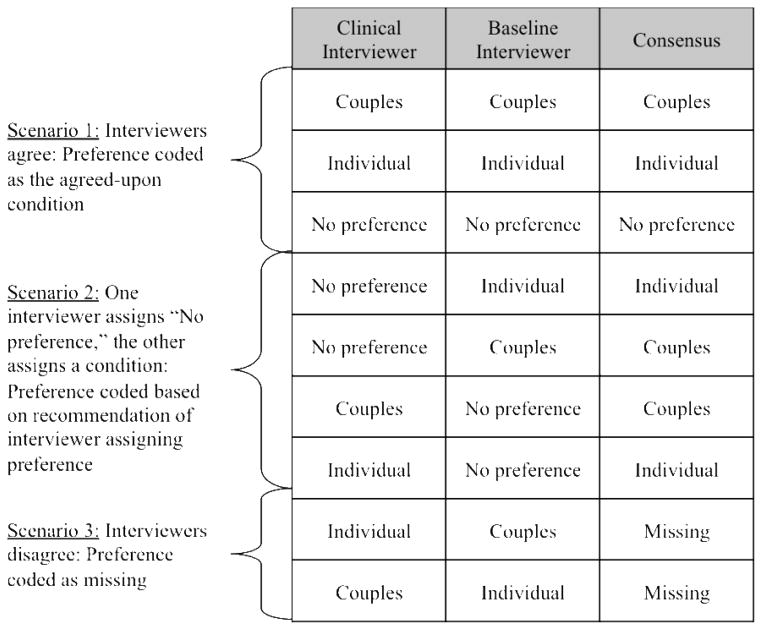
The women’s preference for treatment condition assignment was measured through a consensus rating done by members of the research staff (the clinical screener and baseline interviewer). Each rater indicated their perception of the woman’s condition preference resulting in one of four responses: “wanted individual,” “wanted couples,” “no preference,” and “unknown.” Decision rules were developed to assist in making ratings. For cases that had no clear consensus, group discussion by the research team ensued to resolve discrepancies. All codeable cases were eventually classified according to one of three scenarios: agreement between interviewers on the same condition (preference coded as agreed-upon condition), disagreement between interviewers on the same condition (preference coded as “missing”), and ranking by one interviewer for a condition and by the other as “no preference” or “missing” (preference coded as condition, not missing). For further information on decision rules, see Figure 1. The condition preference variable was then determined to be either 1) “matched” or 2) “mismatched” based on the assigned condition and the rating for the women’s condition preference. If the rating for the women’s condition preference was “no preference” then the condition preference variable was coded as a match. If the condition preference was rated as “unknown” then the condition preference variable was rated as missing. Because treatment preference was not a primary outcome of the main study and was determined to be a variable of interest after a portion of recruitment was done, the majority of ratings (80%) were done retrospectively.
Figure 1.
Decision table of treatment preference assignment.
Daily drinking log
A self-report daily drinking log was used to track drinking behavior during treatment. Women recorded the number of alcohol-related urges experienced, the quantity and type of any alcohol consumed during the day, and level of marital satisfaction.
Homework record
Homework was assigned after each session for individuals and couples. Homework was designed to reinforce skills practiced during session, and typically included a combination of self-monitoring of drinking or cravings, several short psychoeducational handouts (e.g., “How to Refuse a Drink,” “Handling Slips and Relapses,” “For the Partner – Changing your Triggers for her Drinking”), and worksheets extending the topic discussed in session (e.g., self-management planning, for partners: recording positive partner actions). Therapists recorded the number of homework assignments assigned and completed on a homework record form. Percentage of homework completed was calculated for assignments made individually (for men and women in the couples condition and women in the individual condition) and assignments made to the couple in the couples condition. The percentage of homework the woman completed was used as an indicator of treatment engagement. Among samples of cognitive-behavioral treatment for cocaine dependence, homework completion has been found to be a significant predictor of treatment retention,57 increase in coping skills,58 therapeutic alliance,58 and reduction in substance use.57, 58 We chose to use homework completion as a proxy for treatment engagement because it is a key component to nearly every cognitive-behavioral treatment for substance abuse and is easily measureable. Moreover, lacking a universally-accepted measure in the field, homework completion by substance abusers is compelling as a measure of engagement in that it is an index for time spent in activities designed to practice and reinforce concepts discussed in treatment.
Therapist empathy
Therapist empathy was measured using rating scales adapted from Project MATCH59 and Project IMPACT.60 Four raters listened to audiotapes of the second and fifth sessions in their entirety and rated the extent and quality of the empathy shown by the clinician in the session. Empathy was defined as the therapist’s demonstration of sensitivity and warmth, genuine concern, extent to which the therapist was non-judgmental, and understanding of the patients’ feelings and concerns. The quality of therapist empathy rated in the second session was used for analyses in this study. Higher scores on a 5-point Likert scale (1 = very poor, 5 = excellent) indicated higher ratings of therapist empathy. For more information about the therapist ratings see McCrady et al.40
Treatment retention
The total number of sessions attended by the female was used to define treatment retention.
Procedures
Telephone Screen
The telephone screen took approximately 10 minutes to complete and described the treatment project to the caller, assessed potential eligibility of participants, and determined whether to schedule an in-person clinical screen.
Clinical screen interview
Couples who were determined to be eligible for the study through the telephone screen were scheduled for a 2-hour semi-structured clinical screen interview. Clinical interviews were administered by master’s level social workers, advanced doctoral students in clinical psychology, or doctoral-level psychologists. The purpose of the clinical interview was to establish rapport with the couple, further explain study procedures, and assess potential eligibility. The interview consisted of a collection of demographic and screening measures. Interested couples were informed of the details of the research study, informed consent was obtained, and a baseline research assessment was scheduled.
Baseline research assessment
The baseline interview included an assessment of the woman’s psychosocial functioning, the nature and extent of her social network, systematic collection of both partners’ alcohol and drug use over the three months prior to the interview, a diagnostic assessment of the male’s alcohol and drug use, and an evaluation of male and female Axis I and Axis II disorders. Baseline interviews were administered by trained research interviewers.
Treatment
After the baseline interview, couples were randomly assigned to either Alcohol Behavioral Individual Treatment (ABIT) or Alcohol Behavioral Couples Treatment (ABCT). In the ABCT condition, all treatment sessions were delivered in a conjoint format. Both conditions included 20 sessions over a 26-week treatment period and emphasized a goal of abstinence from alcohol. Treatment was administered by doctoral-level psychologists or advanced doctoral students in psychology. All therapists were trained to deliver both ABCT and ABIT using treatment-specific manuals developed by the third and fourth authors (EEE; BSM). Each therapist was assigned a consultant from the treatment team who regularly reviewed session audiotapes to assist in maintaining treatment fidelity. Additionally, weekly group supervision was provided for study therapists to address treatment integrity and clinical issues. For a more detailed description of the treatment, see McCrady et al.40 All study procedures were approved by the Rutgers University Institutional Review Board (IRB).
Results
Sample Characteristics
The characteristics of the sample of 102 couples that entered treatment by gender and modality are seen in Table 1. Overall, couples had a mean household income of $93,631 (SD = $58,717), 95% of the couples were married or living as married, and about 56% of couples had children living at home. All women met criteria for a DSM-IV alcohol use disorder within the prior 12 months, and 98% of women met criteria for current alcohol dependence. On average, the women abstained from alcohol approximately 33% (SD = 28.5) of the days during the 3 months prior to the baseline assessment. Women drank a mean of 8.22 (SD = 4.86) standard drinks per drinking day in the 3 months prior to the baseline assessment. Across both conditions, women attended a mean of 13.7 (SD = 6.5) treatment sessions out of a total of 20 possible, and on average, women completed about 73% of all homework.
Table 1.
Participant Characteristics, Relationship and Treatment Factors by Gender and Treatment Modality
| ABCT | ABIT | |||
|---|---|---|---|---|
| Females (n = 50) | Males (n = 50) | Females (n = 52) | Males (n = 52) | |
| Demographics | ||||
| Age (SD) | 44.8 (9.1) | 48.0 (9.6) | 45.3 (9.3) | 49.0 (11.1) |
| Years of Education (SD) | 14.6 (2.6) | 15.3 (2.8) | 14.5 (2.6) | 15.2 (3.3) |
| Ethnicity (% Caucasian) | 46 (92%) | 47 (94%) | 51 (98%) | 51 (98%) |
| Employed Full-time (%) | 18 (36%) | 44 (88%) | 14 (27%) | 43 (83%) |
| Household Income – median | $87,500.00 | $73,500.00 | ||
| Any Children at Home (% yes) | 30 (60%) | 27 (52%) | ||
| Substance Severity | ||||
| TLFB % Abstinent Days (SD) | 35.0 (29.2) | 66.3 (32.3) | 32.0 (28.0) | 66.5 (33.3) |
| TLFB Mean drinks per day (SD) | 8.3 (4.1) | 3.6 (2.7) (n=44) | 8.2 (5.6) | 3.4 (2.7) (n=47) |
| Total Alcohol-Related Consequences (RCU) (SD) | 38.6 (15.1) | 5.4 (6.8) | 36.4 (17.3) | 3.8 (6.0) |
| Current alcohol use disorder1 (%) | 49 (96%) | 6 (12%) | 52 (100%) | 7 (13%) |
| Number of Current Alcohol Dependence Symptoms1 (SD) | 5.4 (1.4) | 0.5 (1.2) | 5.1 (1.5) | 0.5 (1.2) |
| Age of onset of alcohol use disorder (when current) 1 (SD) | 31.5 (10.9) | 24.8 (11.9) (n=5) | 35.1 (10.7) | 30.6 (19.3) (n=7) |
| Relationship Factors | ||||
| Dyadic Adjustment Scale (SD) | 97.1 (24.0) | 100.7 (21.3) | 105.1 (19.2) | 105.0 (16.7) |
| Spouse encouraging drinking (%yes/accepted) | 18 (39%) | n/a | 15 (31%) | n/a |
| Spouse drinking status (%moderate or heavy) | 22 (45%) | n/a | 21 (40%) | n/a |
| Treatment Factors | ||||
| Therapist empathy (SD) | 4.0 (0.8) | 4.0 (1.0) | n/a | |
| Female condition preference matched (%) | 16 (43%) (n=37) | n/a | 27 (61%) (n=44) | n/a |
| Sessions attended (SD) | 12.4 (6.4)* | n/a | 14.9 (6.5)* | n/a |
| Percent homework completed (SD) | 73% (17%) | 75% (20%) | 74% (24%) | n/a |
Diagnosis missing for 1 ABCT patient
p =.05
Male partners were older than females (t(202) = −2.51, p= 0.013) and nearly all (88%) males were employed full-time. At baseline, the mean number of drinks per day consumed by the women was substantially higher than the mean number of drinks per day consumed by the men (8.2 (SD = 4.9) vs. 3.5 (SD = 2.7), t(161) = 8.46, p < 0.001). That said, more than a quarter of males met current or past criteria for an alcohol use disorder, and as such, there was substantial variability in mean drinks per drinking day among men. Men with a current alcohol use disorder (n = 13) drank 6.4 (SD = 2.8) drinks per day. Further information on sample characteristics can be obtained from McCrady et al.40
Condition Differences in Treatment Retention and Engagement
An independent sample t-test was conducted to examine differences in treatment retention (sessions attended) and engagement (percent homework completed) for the women in the individual and couples treatment conditions. Women in the individual treatment condition attended significantly more sessions than women in the couples condition (t(100) = −1.98; p = .05). There were no significant differences between conditions in the percent of homework completed by the women in ABIT versus ABCT. There were no significant differences by condition and gender on any other demographic, substance severity, relationship, or treatment factor tested (see table 1).
Correlates of Treatment Retention
In Table 2, results are presented from Pearson correlations, t-tests, and ANOVAs testing client and treatment factors associated with treatment sessions attended. There were significant relationships between treatment sessions attended and client factors, such as the women’s age, her total number of current alcohol dependence symptoms, DAS scores, and spouse drinking status. Women who were older, with fewer alcohol dependence symptoms, more satisfying marital relationships or with partners who were drinkers tended to attend more treatment sessions. In terms of treatment factors, women randomized to the individual condition and whose assigned treatment condition matched her preference attended significantly more sessions. Sessions attended was not significantly related to client motivation, current psychological distress, heavy drinkers in her social network, or therapist empathy.
Table 2.
Relationship between treatment retention and engagement and selected variables
| Female treatment retention and engagement | ||||
|---|---|---|---|---|
| Sessions attended | Percent homework completed | |||
| Pearson | t-test/ANOVA | Pearson | t-test/ANOVA | |
| Demographics | ||||
| Age | .27** (n=102) | .32*** (n=101) | ||
| Children at home | t=−0.63 (n=102) | t=2.61* (n=101) | ||
| Substance Severity | ||||
| Current dependence symptoms | −.20* (n=101) | −.22* (n=100) | ||
| Age of onset for alcohol diagnosis | .17 (n=101) | .21* (n=100) | ||
| Motivation | ||||
| Treatment goal | t=−0.02 (n=96) | t=1.66 (n=95) | ||
| Psychological distress | ||||
| POMS total score | −.08 (n=101) | .01 (n=100) | ||
| Relationship characteristics | ||||
| Female DAS score | .34*** (n=101) | .30** (n=100) | ||
| Social support for drinking/abstinence | ||||
| Heavy drinkers in network | −.17 (n=102) | −.11 (n=101) | ||
| Spouse drinking status | F=9.13*** (n=101) | F=1.39 (n=100) | ||
| Spouse encouraging drinking | F=2.39 (n=94) | F=3.64* (n=93) | ||
| Treatment factors | ||||
| Therapist empathy | .07 (n=97) | −.08 (n=97) | ||
| Female condition preference | t=−2.73** (n=81) | t=−1.08 (n=81) | ||
| Treatment condition | t=−1.98* (n=102) | t=−0.21 (n=101) | ||
Note:
p <.05;
p<.01;
p<.001.
Correlates of Treatment Engagement
Pearson correlation, t-test, and ANOVA analyses of women’s homework completion and both client and treatment factors are presented in Table 2. Significant relationships were found between percent homework completed and women’s age, having children at home, her total number of current alcohol dependence symptoms, age of onset of alcohol dependence, DAS scores, and spouse encouragement of her drinking. Women who were older, had no children at home, had fewer alcohol dependence symptoms, later age of onset of an alcohol diagnosis, more satisfying marital relationships, and had partners who encouraged or accepted her drinking tended to complete a higher percentage of homework. The percent of women’s homework completed was not significantly related to treatment preference or condition, motivation, current psychological distress, heavy drinkers in her social network, or therapist empathy.
Predictors of Treatment Retention
Using multiple regression, sessions attended was simultaneously regressed on the strongest significant correlates in each category, which were women’s age, total number of current alcohol dependence symptoms, female relationship quality score, spouse drinking status, and women’s condition preference. The equation containing these five variables accounted for approximately 40% of the variance in sessions attended (F (5, 72) = 9.39, p < .001). Beta weights were examined to assess the relative importance of these variables in the prediction of sessions attended (See Table 3). Results show that women’s relationship satisfaction and spouse drinking status (abstinent vs. any drinking) both had significant beta weights at p < .01. Women having a more satisfying relationship and a spouse/partner who was a drinker predicted more treatment sessions attended. Women whose condition matched her treatment preference attended more sessions at p = 0.095.
Table 3.
Beta weights and t-values obtained in multiple regression analyses predicting treatment sessions attended (N = 78)
| Sessions attended by female participant
| ||
|---|---|---|
| Predictor | Betaa | t-value |
| Age | 0.10 | 1.00 |
| Sum of dependence symptoms | −0.02 | −0.17 |
| Female DAS score | 0.34 | 3.35** |
| Spouse drinking status | 0.40 | 4.09*** |
| Female condition preference | 0.17 | 1.69† |
F(5, 72) = 9.39, p<0.001; R2 = 0.395, adjusted R2 = 0.353
p<0.1;
p <.05;
p<.01;
p<.001.
Beta weights are standardized multiple regression coefficients obtained when Treatment Sessions Attended was regressed on the five predictor variables
Predictors of Treatment Engagement
Since there was more than one significant variable within the demographic and substance severity domains, the variable with the strongest correlation within each domain was retained and entered into the regression analyses in order to maintain power to observe at least medium effects. Percent of homework completed was then regressed on the linear combination of women’s age, total number of current alcohol dependence symptoms, female DAS score, and spouse encouragement of drinking. The equation containing these four variables accounted for 20% of the variance in women’s homework completed (F (4, 86) = 5.48, p < .001). Beta weights are shown in Table 4. Results show that only women’s age had a significant beta weight at p < .05 and that women who were older completed higher percentages of homework. Additionally, spouse encouragement of her drinking had a beta weight at a trend level (p < .07); women with spouses who encouraged or accepted her drinking tended to complete a higher percentage of homework.
Table 4.
Beta weights and t-values obtained in multiple regression analyses predicting percentage homework completed (N=91)
| Percentage of homework completed by female participant
| ||
|---|---|---|
| Predictor | Betaa | t-value |
| Age | 0.25 | 2.43* |
| Sum of dependence symptoms | −0.14 | −1.37 |
| Female DAS score | 0.16 | 1.60 |
| Spouse encouragement of drinking | 0.18 | 1.80† |
F(4,86) = 5.48, p<0.001; R2 = 0.203, adjusted R2 = 0.166;
p<0.1;
p <.05.
Beta weights are standardized multiple regression coefficients obtained when Percentage of Homework Completed was regressed on all four predictor variables
Relationship Factors Related to Treatment Retention and Engagement by Treatment Condition
Since many of the women’s relationship factors (relationship quality, spouse encouragement for drinking, spouse drinking status, and woman’s condition preference) were significantly related to sessions attended and homework completed, we examined these factors separately for each condition. For the couples condition, significant relationships were found between sessions attended and woman’s DAS score (r = 0.35, p < 0.05) and treatment condition preference (t(35) = −2.07, p < 0.05). Those women with more satisfying relationships and those whose preference for couples condition was matched attended significantly more treatment sessions. In the individual condition, only spouse drinking status was significantly related to sessions attended (t(50) = −4.34, p < 0.01), with women who had abstinent spouses attending significantly fewer sessions than women with light or moderate/heavy drinking partners.
Relationship factors were more strongly related to percentage of homework completed in the couples rather than the individual condition. In the couples condition, higher DAS scores (r = 0.38, p < 0.01), spouse encouragement of drinking (t(44) = −2.16, p < 0.05) and woman’s condition preference (t(35) = −2.13, p < 0.05) were significantly related to homework completion. Women with higher relationship satisfaction, spouses who accepted or encouraged her drinking, and with a matched treatment condition preference completed significantly more homework. In the individual condition, there were no significant associations between homework completed and any of the relationship factors.
Due to smaller sample sizes, limited power to detect medium effects, and the exploratory nature of this analysis, regression analyses were not conducted to identify predictors of treatment retention and engagement within each treatment condition.
Discussion
This study examined the relationship between treatment modality and better treatment retention and engagement for women with alcohol problems. Additionally, the study sought to identify client and treatment factors that were predictive of participant retention and engagement. Finally, this study focused on whether the relationship between retention/engagement and predictive variables differed between couples and individual therapy. We defined treatment retention as the total number of sessions attended within a prescribed period of time (6 months). Additionally, treatment engagement was defined by the client’s active participation in treatment through the completion of homework assignments.
Results showed that women in the individual treatment condition were retained in treatment longer than women in the couple condition. This finding does not replicate results found in the literature that show having a spouse involved in treatment either improves treatment engagement and retention29–31 or does not significantly impact the number of treatment sessions attended.61 The former studies specifically addressed male alcoholics: our finding may be explained by our study’s position as one of the first to assess the role of spouse involvement in treatment for women alcoholics. In the latter study, a recent trial of behavioral couples versus an individual or psychoeducational condition for women alcoholics and their spouses61, couples in which the male partner met criteria for substance dependence were excluded, which was not the case in our study. There may be several reasons why women in couples treatment may not be retained as long as those women in individual treatment. In general, studies suggest that approximately 50% of partners of women with alcohol problems also have a substance abuse/dependence problem.62 The male partner may find attending treatment uncomfortable or threatening to his own alcohol and/or drug use. Also, women tend to have family and friends, particularly men, who are opposed to her getting treatment.63–65 The spouses of women alcoholics may be somewhat ambivalent about their partner’s treatment. Thus, when scheduling conflicts arise, the treatment may not be a priority. Finally, in general, women alcoholics experience a great deal of shame when addressing their addiction.17 Having exclusively conjoint sessions, especially if the partner is extremely frustrated and angry, might lead both participants to view treatment as particularly unappealing.
In this study, women who attended more treatment sessions were older, had fewer current symptoms of alcohol dependence, had more satisfying marital relationships, had spouses who drank, and had been randomly assigned to their preferred treatment condition. Additionally, women who completed more homework were older, had fewer children at home, fewer alcohol dependence symptoms, later age of onset of alcohol diagnosis, more satisfying marital relationships, and partners who encouraged her drinking. Age, alcohol severity, and relationship satisfaction are client characteristics that have had some support in the literature as impacting attrition. However, the finding that women attended more treatment sessions with partners who were drinkers and completed more homework with partners who encouraged or accepted her drinking is somewhat surprising. Generally, one would expect a spouse who is abstinent to provide a more supportive environment for a woman’s recovery and make it more likely she would attend and engage in treatment sessions. However, it may be that women attended more treatment not only to assist in their own recovery, but also to have a refuge to discuss ways of coping with a drinking spouse and to receive support for her change. On the other hand, it may be that a spouse who is abstinent provides enough support and modeling for the woman to make changes in her drinking without treatment. Further, it may be that a woman whose spouse encourages her to drink is driven to treatment more by her own perception of her problem instead of external pressures, and thus, she may be more likely to engage in treatment. The impact of spouse drinking and spousal encouragement of drinking is important but not well studied. Further studies are needed to examine the influence of spouse attitudes toward drinking on women’s alcohol use and recovery through interview and/or women’s self report. Specifically, women with heavily drinking spouses might particularly value discussion of topics related to their spouses’ drinking (e.g., shared activities that do not involve drinking, partner-related functional analysis) and, as such, attendance may be further enhanced by providing more time for these discussions with their spouses present.
There has been little work examining the influence of preference for treatment modality on retention. Some studies have been conducted on patient choice of treatment goal,66 but we are aware of only a few studies67,68 that examined the effect of choice in substance abuse treatment modality on retention and outcome, and none that compare choice of individual versus couples treatment with women alcoholics. Results of the extant literature suggest that treatment preference does not make a difference on client retention or outcome. This is contrary to our finding that women who received their treatment of preference attended significantly more sessions than women who were not assigned to their condition of choice. Our finding that treatment preference does make a difference in terms of sessions attended may be due to differences in sample characteristics or treatment modalities provided. For example, it may be that treatment preference is not associated with attrition for a cocaine-dependent mixed gender sample assigned to either intensive group therapy or weekly individual therapy, but treatment preference may be a predictor of attendance for alcohol-dependent females assigned to either individual or couples therapy. Indeed, factors contributing to treatment retention may be much more personal when an individual is assigned to individual versus conjoint therapy with their spouse. Our result is consistent with studies on client input in treatment planning,69 although more research is needed in this area, specifically in client choice of treatment modality by gender and substance of abuse. Many have noted the numerous differences between men and women in the onset and effects of problematic alcohol use,70, 71 but generally, treatment has been developed and programmed based on a model of treating male alcoholics.72 Providing a choice in treatment modality may be particularly important to women entering treatment in order to feel a sense of empowerment and commitment to the treatment.
The regression analysis showed that spouse drinking status and the woman’s marital satisfaction were significant independent predictors of sessions attended. Age and (at a trend level) spouse encouragement of drinking were significant independent predictors of treatment engagement. Prior attrition studies that have focused on client characteristics have not included specific relationship factors or substance use characteristics of the spouse. This is somewhat surprising given the recognition that spouses/family have a significant influence on the help-seeking and change processes. The results of this study suggest the importance of assessing the impact of specific relationship factors on treatment retention and broadening the definition of “client characteristics” to include these relationship factors in predicting treatment attrition. In addition, an important issue to consider is how information about predictors of attrition, especially client or spouse characteristics, can be used to improve treatment retention. Understanding the process of how certain client characteristics influence attrition is crucial and may provide valuable insight for treatment programming.
Given that substance abuse treatments designed specifically for women have only been developed and studied relatively recently with promising results,11 much of what we know about treatment retention and engagement is based on mixed gender or primarily male samples. Our findings, some of which are somewhat surprising considering existing literature, underscore the importance of continuing to identify the unique predictors of retention and engagement among women generally as well as in gender-specific treatment.
Study Limitations
This study had several limitations. The sample was primarily Caucasian and middle- to upper-class, and our retention was unusually high (only about 13% of women in our sample completed 4 or fewer treatment sessions, compared with dropout rates greater than 50% by the fourth session for outpatient alcohol treatment samples.6,10) Further, our study required that women have male partners who are willing to participate in treatment. As described in McCrady et al.40, a number of potentially eligible women were thus excluded from the study, either because they or their partners were not amenable to couples treatment. As such, our study may have oversampled women with alcohol use disorders with particularly functional relationships. All of these factors limit the generalizability of our results.
Another limitation was the assessment of the condition preference variable, which was done retrospectively for a majority of the sample and relied on judgments made by research personnel. Baseline and clinical interviewers spent upwards of 6 hours with each subject before randomization. As such, their perceptions of treatment preference may have been freer from bias than those who had greater interaction with the subject later on in the study (i.e., the therapists). Further, although there are many ways to define treatment engagement (e.g., mean number of days between sessions, strength of the therapeutic relationship, percent days abstinent throughout treatment, and percentage of homework completed), we decided to use the percentage of homework completed as a proxy for treatment engagement. There may be disagreements about whether this is an optimal measure of treatment engagement. However, homework completion has been measured in many manual-guided treatments and has recently been evaluated as a potential mediator for substance abuse treatment outcomes,58 suggesting both the accessibility and importance of the variable. Also, homework completion may be particularly valuable as a broad marker of treatment engagement as it indicates client activity between sessions related to relevant treatment tasks. That said, as evidenced by the variety of ways of testing engagement in substance abuse treatment, consensus on universal measurement in the field is warranted and is an area for future research. It is likely that homework completion is only one of many valuable measures of the multidimensional construct of treatment engagement.
Conclusions
Research on the influence of treatment modality on treatment retention and specific factors related to attrition in a women’s-specific treatment program has been limited. Results of this study show that women attended significantly more treatment sessions when they were in individual treatment rather than couples treatment. In addition, results highlight important associations between treatment and relationship variables with retention and engagement. Specific relationship factors, such as marital satisfaction, spouse encouragement for drinking, and spouse drinking status were significant predictors of treatment engagement and retention and need further study. Results also reinforced the importance of providing clients choices in their treatment, which has implications for treatment matching.
Acknowledgments
Funding for this research was provided by the National Institute on Alcohol Abuse and Alcoholism, grant R37 AA07070. We would like to gratefully acknowledge the assistance of research and clinical staff and graduate students who worked on the study, including Nicola Chung, Sadi Delaney, Michelle Drapkin, Nick Giardino, Rachel Golum, Jumi Hayaki, Linda Hirsch, Sandy Hoffmann, Rosa Kim, Jennifer Knapp-Manuel, Greta Kugler, Maureen McGuire, Charles Neighbors, Helen Raytek, Karen Rhines, Debbi Share, Jean Schellhorn, Janine Swingle, Danielle Walker, Barbara Zdep-Mattocks, and Rene Zweig.
Footnotes
Presented as a poster at the 109th Annual Convention of the American Psychological Association, August 24 – August 28, 2001, San Francisco, CA.
The views herein are those of the authors and not necessarily those of the National Institute of Alcohol Abuse and Alcoholism.
References
- 1.Festinger DS, Lamb RJ, Marlowe DB, Kirby KC. From telephone to office: Intake attendance as a function of appointment delay. Addict Behav. 2002;27(1):131–137. doi: 10.1016/s0306-4603(01)00172-1. [DOI] [PubMed] [Google Scholar]
- 2.Stark MJ. Dropping out of substance abuse treatment: A clinically oriented review. Clin Psychol Rev. 1992;12(1):93–116. [Google Scholar]
- 3.Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the drug abuse treatment outcome study (DATOS) Psychology of Addictive Behaviors. 1997;11(4):294–307. [Google Scholar]
- 4.Carroll KM. Beyond the therapeutic alliance: Keeping the drug-dependent individual in treatment. National Institute on Drug Abuse (NIDA); 1997. Enhancing retention in clinical trials of psychosocial treatments: Practical strategies. NIDA Research Monograph 165. [PubMed] [Google Scholar]
- 5.Ribisl KM, Walton MA, Mowbray CT, Luke DA, Davidson WS, Bootsmiller BJ. Minimizing participant attrition in panel studies through the use of effective retention and tracking strategies: Review and recommendations. Evaluation and Program Planning. 1996;19:1–25. [Google Scholar]
- 6.Baekeland F, Lundwall L. Dropping out of treatment: A critical review. Psychol Bull. 1975;82(5):738–783. doi: 10.1037/h0077132. [DOI] [PubMed] [Google Scholar]
- 7.Craig RJ. Reducing the treatment drop out rate in drug abuse programs. J Subst Abuse Treat. 1985;2:209–219. doi: 10.1016/0740-5472(85)90003-0. [DOI] [PubMed] [Google Scholar]
- 8.Hser YI, Anglin MD, Grella C, Longshore D, Prendergast ML. Drug treatment careers. A conceptual framework and existing research findings. J Subst Abuse Treat. 1997;14:543–558. doi: 10.1016/s0740-5472(97)00016-0. [DOI] [PubMed] [Google Scholar]
- 9.Gainey RR, Wells EA, Hawkins JD, Catalano RF. Predicting treatment retention among cocaine users. Int J Addict. 1993;28:487–505. doi: 10.3109/10826089309039643. [DOI] [PubMed] [Google Scholar]
- 10.Jefferson L. The relationship between stages of change and dropout from treatment among addicted clients in an outpatient addictions treatment program. Dissertation Abstracts International. 1991;53:7-B. [Google Scholar]
- 11.Greenfield S, Brooks A, Gordon S, et al. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug Alcohol Depend. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kravitz HM, Fawcett J, McGuire M, Kravitz GS, Whitney M. Treatment attrition among alcohol-dependent men: Is it related to novelty seeking personality traits? J Clin Psychopharmacol. 1999;19:51–56. doi: 10.1097/00004714-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Siqueland L, Crits-Christoph P, Frank A, et al. Predictors of dropout from psychosocial treatment of cocaine dependence. Drug Alcohol Depend. 1998;52:1–13. doi: 10.1016/s0376-8716(98)00039-8. [DOI] [PubMed] [Google Scholar]
- 14.Carroll KM, Rounsaville BJ, Gordon LT, et al. Psychotherapy and pharmacotherapy for ambulatory cocaine abusers. Arch Gen Psychiatry. 1994;51:177–187. doi: 10.1001/archpsyc.1994.03950030013002. [DOI] [PubMed] [Google Scholar]
- 15.Bell K, Cramer-Benjamin D, Anastas J. Predicting length of stay of substance-using pregnant and postpartum women in day treatment. J Subst Abuse Treat. 1997;14:393–400. doi: 10.1016/s0740-5472(96)00111-0. [DOI] [PubMed] [Google Scholar]
- 16.Monras M, Gual A. Attrition in group therapy with alcoholics: A survival analysis. Drug and Alcohol Review. 2000;19:55–63. [Google Scholar]
- 17.Nelson-Zlupko L, Kauffman E, Dore MM. Gender differences in drug addiction and treatment: Implications for social work intervention with substance-abusing women. Soc Work. 1995;40:45–54. [PubMed] [Google Scholar]
- 18.Agosti V, Nunes E, Stewart JW, Quitkin FM. Patient factors related to early attrition from an outpatient cocaine research clinic: A preliminary report. Int J Addict. 1991;26:327–334. doi: 10.3109/10826089109058888. [DOI] [PubMed] [Google Scholar]
- 19.Weisner C, Mertens J, Tam T, Moore C. Factors affecting the initiation of substance abuse treatment in managed care. Addiction. 2001;96:705–16. doi: 10.1046/j.1360-0443.2001.9657056.x. [DOI] [PubMed] [Google Scholar]
- 20.Beckman LJ, Amaro H. Personal and social difficulties faced by women and men entering alcoholism treatment. J Stud Alcohol. 1986;47:135–145. doi: 10.15288/jsa.1986.47.135. [DOI] [PubMed] [Google Scholar]
- 21.Beckman LJ, Bardsley PE. Individual characteristics, gender differences and drop-out from alcoholism treatment. Alcohol Alcohol. 1986;21:213–224. [PubMed] [Google Scholar]
- 22.Gomberg E. Women. In: Epstein E, McCrady B, editors. Addictions: A Comprehensive Guidebook. New York: Oxford University Press; 1999. pp. 527–541. [Google Scholar]
- 23.McCrady B, Raytek H. Women and substance abuse: Treatment modalities and outcomes. In: Gomberg E, Nirenberg T, editors. Women and Substance Abuse. Norwood, NJ: Ablex Publishing; 1993. pp. 314–338. [Google Scholar]
- 24.Mattson ME, Del Boca FK, Carroll KM, et al. Compliance with treatment and follow-up protocols in project MATCH: Predictors and relationship to outcome. Alcohol Clin Exp Res. 1998;22:1328–1339. [PubMed] [Google Scholar]
- 25.Connors GJ, DiClemente CC, Dermen KH, Kadden R, Carroll KM, Frone MR. Predicting the therapeutic alliance in alcoholism treatment. J Stud Alcohol. 2000;61:139–149. doi: 10.15288/jsa.2000.61.139. [DOI] [PubMed] [Google Scholar]
- 26.Hyams G, Cartwright A, Spratley T. Engagement in alcohol treatment: The client’s experience of, and satisfaction with, the assessment interview. Addictions Research. 1996;4:105–123. [Google Scholar]
- 27.Raytek HS, McCrady BS, Epstein EE, Hirsch LS. Therapeutic alliance and the retention of couples in conjoint alcoholism treatment. Addict Behav. 1999;24:317–330. doi: 10.1016/s0306-4603(98)00085-9. [DOI] [PubMed] [Google Scholar]
- 28.Epstein EE, McCrady BS, Miller KJ, Steinberg M. Attrition from conjoint alcoholism treatment: Do dropouts differ from completers? J Subst Abuse. 1994;6:249–265. doi: 10.1016/s0899-3289(94)90447-2. [DOI] [PubMed] [Google Scholar]
- 29.Azrin NH. Improvements in the community-reinforcement approach to alcoholism. Behav Res Ther. 1976;14:339–348. doi: 10.1016/0005-7967(76)90021-8. [DOI] [PubMed] [Google Scholar]
- 30.Noel NE, McCrady BS, Stout RL, Fisher-Nelson H. Predictors of attrition from an outpatient alcoholism treatment program for couples. J Stud Alcohol. 1987;48:229–235. doi: 10.15288/jsa.1987.48.229. [DOI] [PubMed] [Google Scholar]
- 31.O’Farrell T, Cutter H, Floyd F. Evaluating behavioral marital therapy for male alcoholics: Effects on marital adjustment and communication from before to after therapy. Behavioral Therapist. 1985;16:147–167. [Google Scholar]
- 32.Zweben A, Pearlman S, Li S. Reducing attrition from conjoint therapy with alcoholic couples. Drug Alcohol Depend. 1983;11:321–331. doi: 10.1016/0376-8716(83)90023-6. [DOI] [PubMed] [Google Scholar]
- 33.Fals-Stewart W, O’Farrell T, Birchler G. Behavioral couples therapy versus individual-based treatment for male substance abusing patients: An evaluation of significant individual change and comparison of improvement rates. J Subst Abuse Treat. 2000;18:249–254. doi: 10.1016/s0740-5472(99)00059-8. [DOI] [PubMed] [Google Scholar]
- 34.McKay JR, Longabaugh R, Beattie MC, Maisto SA, Noel NE. Does adding conjoint therapy to individually focused alcoholism treatment lead to better family functioning? J Subst Abuse. 1993;5:45–59. doi: 10.1016/0899-3289(93)90122-r. [DOI] [PubMed] [Google Scholar]
- 35.Fiorentine R, Nakashima J, Anglin MD. Client engagement in drug treatment. J Subst Abuse Treat. 1999;17:199–206. doi: 10.1016/s0740-5472(98)00076-2. [DOI] [PubMed] [Google Scholar]
- 36.Simpson DD, Joe GW. A longitudinal evaluation of treatment engagement and recovery stages. J Subst Abuse Treat. 2004;27:89–97. doi: 10.1016/j.jsat.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 37.Simpson DD, Joe GW, Rowan-Szal G, Greener J. Client engagement and change during drug abuse treatment. J Subst Abuse. 1995;7:117–134. doi: 10.1016/0899-3289(95)90309-7. [DOI] [PubMed] [Google Scholar]
- 38.Joe GW, Simpson DD, Broome KM. Retention and patient engagement models for different treatment modalities in DATOS. Drug Alcohol Depend. 1999;57:113–125. doi: 10.1016/s0376-8716(99)00088-5. [DOI] [PubMed] [Google Scholar]
- 39.Simpson DD. A conceptual framework for drug treatment process and outcomes. J Subst Abuse Treat. 2004;27:99–121. doi: 10.1016/j.jsat.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 40.McCrady B, Epstein E, Cook S, Jensen N, Hildebrandt T. A randomized trial of individual and couple behavioral alcohol treatment for women. J Consult Clin Psychol. doi: 10.1037/a0014686. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sobell L, Sobell M. TimeLine Follow Back: A Calendar Method for Assessing Alcohol and Drug use. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- 42.NIAAA. Helping Patients Who Drink Too Much: A Clinician’s Guide. U.S. Department of Health and Human Services; 2005. [Google Scholar]
- 43.Maisto SA, Sobell MB, Sobell LC. Reliability of self-reports of low ethanol consumption by problem drinkers over 18 months of follow-up. Drug Alcohol Depend. 1982;9:273–278. doi: 10.1016/0376-8716(82)90066-7. [DOI] [PubMed] [Google Scholar]
- 44.Rhines KC, McCrady BS, Morgan TJ, Hirsch LS. Integrated assessment of alcohol and drug use: The Rutgers consequences of use questionnaire. Alcohol Clin Exp Res. 1997;21(94A) [Google Scholar]
- 45.Heather N, Gold R, Rollnick S. Readiness to change questionnaire: User’s manual. New South Wales, Australia: University of New South Wales, National Drug and Alcohol Research Center; 1991. [Google Scholar]
- 46.Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. Br J Addict. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- 47.Heather N, Rollnick S, Bell A. Predictive validity of the readiness to change questionnaire. Addiction. 1993;88:1667–1677. doi: 10.1111/j.1360-0443.1993.tb02042.x. [DOI] [PubMed] [Google Scholar]
- 48.Hall SM, Havassy BE, Wasserman DA. Effects of commitment to abstinence, positive moods, stress, and coping on relapse to cocaine use. J Consult Clin Psychol. 1991;59:526–532. doi: 10.1037//0022-006x.59.4.526. [DOI] [PubMed] [Google Scholar]
- 49.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version. New York: New York State Psychiatric Institute; 1996. Patient Edition. [Google Scholar]
- 50.Epstein EE, Labouvie E, McCrady BS, Jensen NK, Hayaki J. A multi-site study of alcohol subtypes: Classification and overlap of unidimensional and multi-dimensional typologies. Addiction. 2002;97:1041–1053. doi: 10.1046/j.1360-0443.2002.00164.x. [DOI] [PubMed] [Google Scholar]
- 51.Williams JB, Gibbon M, First MB, et al. The structured clinical interview for DSM-III-R (SCID). II. multisite test-retest reliability. Arch Gen Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- 52.McNair DM, Lorr M, Droppleman LF. POMS Manual: Profile of Mood States. San Diego, CA: Educational and Industrial Testing Service; 1992. [Google Scholar]
- 53.Spanier G. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- 54.Busby DM, Christensen C, Crane DR, Larson JH. A revision of the dyadic adjustment scale for use with distressed and nondistressed couples: Construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21:289–308. [Google Scholar]
- 55.Spanier GB. The measurement of marital quality. J Sex Marital Ther. 1979;5:288–300. doi: 10.1080/00926237908403734. [DOI] [PubMed] [Google Scholar]
- 56.Longabaugh R, Wirtz PW, Beattie MC, Noel N, Stout R. Matching treatment focus to patient social investment and support: 18-month follow-up results. J Consult Clin Psychol. 1995;63:296–307. doi: 10.1037//0022-006x.63.2.296. [DOI] [PubMed] [Google Scholar]
- 57.Gonzalez VM, Schmitz JM, DeLaune KA. The role of homework in cognitive-behavioral therapy for cocaine dependence. J Consult Clin Psychol. 2006;74:633–637. doi: 10.1037/0022-006X.74.3.633. [DOI] [PubMed] [Google Scholar]
- 58.Carroll KM, Nich C, Ball SA. Practice makes progress? Homework assignments and outcome in treatment of cocaine dependence. J Consult Clin Psychol. 2005;73:749–755. doi: 10.1037/0022-006X.73.4.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carroll KM, Connors GJ, Cooney NL, et al. Internal validity of project MATCH treatments: Discriminability and integrity. J Consult Clin Psychol. 1998;66:290–303. doi: 10.1037//0022-006x.66.2.290. [DOI] [PubMed] [Google Scholar]
- 60.Morgenstern J, Morgan TJ, McCrady BS, Keller DS, Carroll KM. Manual-guided cognitive-behavioral therapy training: A promising method for disseminating empirically supported substance abuse treatments to the practice community. Psychol Addict Behav. 2001;15:83–88. [PubMed] [Google Scholar]
- 61.FalsStewart W, Birchler GR, Kelley ML. Learning sobriety together: A randomized clinical trial examining behavioral couples therapy with alcoholic female patients. J Consult Clin Psychol. 2006;74:579–591. doi: 10.1037/0022-006X.74.3.579. [DOI] [PubMed] [Google Scholar]
- 62.McCrady B. Alcoholism. In: Blechmand EA, Brownell KD, editors. Handbook for Behavioral Medicine for Women. New York: Pergamon Press; 1988. pp. 357–368. [Google Scholar]
- 63.Beckman LJ, Amaro H. Patterns of women’s use of alcohol treatment agencies. In: Wilsnack SC, Beckman LJ, editors. Alcohol Problems in Women: Antecedents, Consequences and Intervention. New York: Guilford Press; 1984. pp. 319–348. [Google Scholar]
- 64.Mays V, Beckman L, Oranchak E, Harper B. Perceived social support for help-seeking behaviors of black heterosexual and homosexually active women alcoholics. Psychol Addict Behav. 1994;8:235–242. [Google Scholar]
- 65.Wilsnack C. Barriers to treatment for alcoholic women. Addiction and Recovery. 1991:10–12. [Google Scholar]
- 66.Miller WR, Leckman AL, Delaney HD, Tinkcom M. Long-term follow-up of behavioral self-control training. J Stud Alcohol. 1992;53:249–261. doi: 10.15288/jsa.1992.53.249. [DOI] [PubMed] [Google Scholar]
- 67.Sterling RC, Gottheil E, Glassman SD, Weinstein SP, Serota RD. Patient treatment choice and compliance. data from a substance abuse treatment program. Am J Addict. 1997;6:168–176. [PubMed] [Google Scholar]
- 68.Adamson SJ, Sellman DJ, Dore GM. Therapy preference and treatment outcome in clients with mild to moderate alcohol dependence. Drug and Alcohol Review. 2005;24:209–216. doi: 10.1080/09595230500167502. [DOI] [PubMed] [Google Scholar]
- 69.Kadden R, Skerker P. Treatment decision making and goal setting. In: Epstein E, McCrady B, editors. Addictions: A Comprehensive Guidebook. New York: Oxford University Press; 1999. pp. 216–231. [Google Scholar]
- 70.Smith WB, Weisner C. Women and alcohol problems: A critical analysis of the literature and unanswered questions. Alcohol Clin Exp Res. 2000;24:1320–1. [PubMed] [Google Scholar]
- 71.Weisner C, Schmidt L. Gender disparities in treatment for alcohol problems. JAMA. 1992;268:1872–1876. [PubMed] [Google Scholar]
- 72.Kauffman E, Dore MM, Nelson-Zlupko L. The role of women’s therapy groups in the treatment of chemical dependence. Am J Orthopsychiatry. 1995;65:355–63. doi: 10.1037/h0079657. [DOI] [PubMed] [Google Scholar]