Abstract
Parenting, including nonresponsive feeding styles, has been related to under- or overweight among young children. The relationship between maternal mental health and feeding styles has not been examined. We hypothesized that mothers who report more symptoms of stress, depression, or anxiety report less responsive (e.g. more controlling, indulgent, and uninvolved) feeding styles than mothers who report fewer symptoms of stress, depression, or anxiety. Our analyses included 702 mother-infant pairs from a statewide sample of Special Supplemental Nutrition Program for Women, Infants, and Children mothers. We assessed maternal mental health and feeding styles by a telephone survey. After adjusting for potential confounding variables, maternal stress symptomatology was significantly associated with forceful (β = 0.03; 95% CI = 0.02, 0.05) and uninvolved (OR = 1.4; 95% CI = 1.1, 1.7) feeding style scores, maternal depression symptomatology was significantly associated with forceful (β = 0.03; 95% CI = 0.004, 0.05), indulgent (β = 0.03; 95% CI = 0.004, 0.06), and uninvolved (OR = 1.5; 95% CI = 1.001, 2.2) feeding styles scores, and maternal anxiety symptomatology was significantly related to restrictive (β = 0.11;95% CI = 0.01, 0.21), forceful (β = 0.04;95% CI=0.02, 0.06), and uninvolved (OR = 1.4;95% CI = 1.01, 1.9) feeding style scores. Among mothers who perceived their infant as temperamentally fussy, there was a significant positive relationship between restrictive feeding styles scores and 3 indices of maternal mental health (stress, β = 0.18; 95% CI = 0.07, 0.28; depression, β = 0.21; 95% CI = 0.04, 0.38; and cumulative mental health symptomatology, β = 0.29; 95% CI = 0.10, 0.48). Mothers who report stress, depression, or anxiety symptoms are at risk for nonresponsive feeding styles. These findings provide support for broadening the focus of existing child nutrition programs to include strategies that recognize how issues of maternal mental health can affect feeding styles.
Introduction
Parenting, including nonresponsive feeding styles, has been associated with risk of both underweight (1) and overweight (2) among young children. A responsive feeding style is embedded in an authoritative style of parenting (3,4) and refers to an interaction in which the caregiver provides guidance, recognizes the child’s cues of hunger and satiety, and responds in an age-appropriate and nurturant manner (5). Conversely, a controlling feeding style is embedded in an authoritarian style of parenting (3,4) and includes practices such as pressuring children to eat more food and restricting children from certain amounts or types of food. Controlling feeding styles are associated with low child self-regulation of intake, feeding fussiness, low fruit and vegetable consumption, child dietary restraint, disinhibition, and childhood overweight (2,6–14). An indulgent feeding style is embedded in an indulgent style of parenting, is often based exclusively on the child’s wishes with little or no structure or guidelines, and may result in a diet low in vegetables and high in fat and sugar (4). An uninvolved feeding style is embedded in an uninvolved parenting style in which parents may be unengaged, ignore child feeding recommendations, and are insensitive to their children’s dietary needs or cues (4).
Maternal mental health, including symptoms of stress, depression, or anxiety, can interfere with responsive parenting (15–23). Although feeding practices are a fundamental component of parenting, the relationship between maternal mental health and feeding styles has not been well explored.
The objective of this study is to assess how maternal mental health (including symptoms of stress, depression, or anxiety) is related to feeding styles among mothers and infants. We hypothesize that mothers who report more symptoms of stress, depression, or anxiety report less responsive (e.g. more controlling, indulgent, and uninvolved) feeding styles than mothers who report fewer symptoms of stress, depression, or anxiety.
Mothers who perceive their infants as having difficult temperaments may experience greater parenting challenges than those who perceive their infants to be easy-going (24). Thus, mothers’ perceptions of the infant’s temperament may also be related to maternal mental health and feeding (25). We hypothesize that maternal perception of infant temperament moderates the relationship between feeding styles and symptoms of stress, depression, or anxiety such that mothers with maternal mental health symptomatology who perceive their infants to be temperamentally difficult or fussy are more likely to use nonresponsive feeding styles than mothers with neither or only one condition.
Materials and Methods
Sample and study design
This study is nested within the Maryland Infant Feeding Study, a cross-sectional study investigating feeding styles and infant nutritional status among a statewide sample of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC)5 participants. WIC is the largest supplemental food program in the United States, providing food, nutrition counseling, and health referrals to low-income pregnant and postpartum women, infants, and children up to age 5 y (26). We conducted a telephone survey of WIC participants between July 2004 and July 2005. The Maryland State WIC Program provided contact information of all mothers with infants from birth to 12 mo of age (n = 33,804). Potential study participants were stratified by age of infant (0–4, 5–8, and 9–12 mo); race/ethnicity (White, Hispanic, or African-American); and geographic location of residence (urban/peri-urban vs. rural/suburban). Using a random-number table, a sample (n = 10,376) was selected from the stratified population. With a goal of 800 study participants, contacts were made or attempted for 3285 individuals. Potential participants were ineligible if they were, <18 y old, had an infant >12 mo old, or were not the infant’s primary caregiver. Study details are provided elsewhere (27).
A brief description of the project was sent to potential participants, informing them how to contact us if they did not want to participate. All materials were written in English and Spanish and respondents were given a choice of completing the interview in English or Spanish. Six trained telephone interviewers (3 bilingual) collected data. Each interview lasted ~45 min.
Approximately 52% (n = 1705) of the randomly selected WIC participants could not be located. Although there were no differences between participants located and not located in geographic residence, infant gender, and maternal prepregnancy weight, Hispanic mothers and mothers of younger infants (0–4 mo) were more likely to be located than White or African-American mothers and mothers of older infants (9–12 mo). Of the participants who could be located and were eligible (n = 1209), 65% completed the interview (n = 781), 24% refused, and 10% failed to keep or complete scheduled appointments. Data on 79/781 (10%) were excluded because they terminated the interview before the mental health questions were administered and 5 infants in their 13th mo at the completion of the interview were retained, resulting in a final analytic dataset of 702 mothers and infants. Participants with complete data and those without complete data did not differ in race/ethnicity, maternal age, education, parity, marriage, infant age, gender, or birth weight.
All data collection instruments and procedures were approved by the Maryland Department of Health and Mental Hygiene Institutional Review Board, the University of Maryland Institutional Review Board, and the Johns Hopkins Committee on Human Research. All participants received written information on the study, were informed that participation in the study was voluntary, and were assured of the confidentiality of their data received. Verbal consent from each respondent was obtained. Mothers received a $10 gift certificate to a local store and a list of health and social services for mothers and infants.
Feeding styles
Based on theories of parenting and feeding, we developed a 25-item questionnaire to assess responsive, forceful, restrictive, indulgent, and uninvolved feeding styles. To access responsive and controlling feeding styles, we used the Feeding Your Baby scale (28) and adapted items from the Child Feeding Questionnaire (29) and the Infant Feeding Questionnaire (30). Six questions were added to assess indulgent and uninvolved feeding styles. The final questionnaire used a 5-point Likert scale in which higher scores represented the feeding style under investigation.
Confirmatory factor analysis was employed on the complete dataset (n = 781) to identify the 5 hypothesized styles of feeding: responsive, forceful, restrictive, indulgent, and uninvolved. We used oblique rotations to evaluate the factor structure. A minimum factor loading of 0.30 was used and items within each factor were averaged to yield factor values. In factors with at least 6 items (e.g. responsive, forceful, and restrictive), cases missing ≤2 individual feeding items were assigned the mean of their available items. In factors with <6 items (e.g. indulgent and uninvolved), cases missing 1 individual feeding style item were assigned the mean of their available items. The forceful and restrictive feeding style factors included imputed items that were intentionally skipped if the infant had not yet started solids. Multivariate analyses were conducted using imputed and nonimputed feeding style data; imputed scores are presented. A change in significance between imputed and nonimputed data occurred in only 1 test with a marginally significant nonimputed finding becoming significant after imputation.
Maternal stress
The Perceived Stress Scale is the most widely used psychological instrument for measuring the perception of stress (31). In this study, stress was measured with the 4-item Perceived Stress Scale (PSS-4). The PSS-4 measures the perceived stress associated with daily life situations; the reliability and validity of the PSS-4 have been established for telephone interviews. PSS-4 scores are obtained by reverse coding the positive items and then summing across all 4 items on a continuous scale. Higher scores reflect higher degrees of perceived stress. Cases missing 1 (n = 10) individual PSS-4 variable were assigned the mean of available variables. The internal consistency reliability within the current sample was 0.70.
Maternal depression
Maternal depressive symptomatology was assessed by adapting 7 items from the 10-item self-report version of the PRIME-MD [Primary Care Evaluation of Mental Disorders Patient Health Questionnaire (PHQ)]. To satisfy ethical review, we did not assess if mothers were a danger to themselves; therefore, the item related to maternal suicidal ideation was removed. The PHQ offers validity comparable to the original PRIME-MD (32). In addition, the PHQ detects atypical depressive symptoms (e.g. overeating and sleeping too much) that may be common in low-income communities. Depressive mood scale scores were summed to yield a total score, with higher scores indicating more depressive symptoms. The internal consistency reliability within the current sample was 0.75. Cases missing 1 (n = 7) individual PRIME-MD (PHQ) variable were assigned the mean of available variables.
Maternal anxiety
The 6-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) was administered. The validity and reliability of the 6-item STAI scale have been established (33,34). The qualities evaluated by this scale are current feelings of apprehension, tension, nervousness, and worry. The 4-point continuous scale was employed with higher scores reflecting higher levels of anxiety. Cases missing 1 (n = 4) individual STAI variable were assigned the mean of available variables. The internal consistency reliability within the current sample was 0.79.
Cumulative maternal mental health symptomatology
In addition to symptoms of stress, depression, and anxiety, we also evaluated the relationships between cumulative maternal mental health symptomatology and feeding styles. To isolate the most extreme cases of maternal mental health symptomatology, we constructed a dichotomous variable identifying mothers who scored in the top quartile on ≥2 mental health measures.
Maternal perception of infant temperament
Maternal perception of infant temperament was measured by adapting 6 items from the fussy-difficult factor of the Infant Characteristics Questionnaire (IchQ) (35). Items were selected that represented fussiness or irritability, such as time spent crying or soothing difficulty. To simplify response choices, the 7-point scale used in the IchQ was shortened to a 3-point scale ranging from 1 “very easy” to 3 “very difficult.” Items from the IchQ were summed to form a total score. Validity and reliability evidence for the unadapted version of the IchQ include adequate factor structure, internal consistency, and test-retest reliabilities (35). Cases missing 1 (n = 9) individual IchQ variable were assigned the mean of available variables. The internal consistency reliability within the current sample was 0.68.
Statistical analysis
Descriptive data analyses included examining frequencies, means, and SD for study variables. To deal with skewed data, forceful and indulgent feeding style factors were normalized using the natural logarithm and the uninvolved feeding style factor was dichotomized. Associations between demographic characteristics and feeding styles were examined with bivariate linear or logistic regression models. Associations among mental health (e.g. stress, depression, or anxiety), feeding styles, and maternal perceptions of infant temperament measures were assessed with Pearson product-moment or Spearman correlations. Multivariate linear regression models were used to examine associations between maternal mental health and continuous feeding style variables (i.e. responsive, forceful, restrictive, and indulgent) by computing the β coefficient (i.e. average change in feeding style scores per unit change in mental health scores), adjusting for demographic factors related to the feeding style variables. A multivariate logistic regression model was used to estimate the odds of reporting higher uninvolved feeding style scores with increases in maternal mental health symptomatology scores, adjusting for demographic factors related to the feeding style variables (36).
We assessed whether these associations were moderated by maternal perceptions of infant temperament. Interactions were statistically tested by the addition of the relevant cross-product (e.g. stress × infant temperament) term and were further evaluated in stratified analyses. The results are means ± SD and percentages; the significance level throughout was P < 0.05. Analyses were conducted using SPSS version 15.0 (37).
Results
Complete data were available on 702 mothers and infants. Fifty percent (n = 348) of the infants were White, 36% (n = 252) were African-American, and 15% (n = 102) were Hispanic. Infants were stratified approximately equally between age group (0–4, 5–8, and 9–13 mo) and gender. The mean infant birth weight was 3263 g (SD = 640) and 8.7% weighed <2500 g at birth. The mean age of mothers was 27 y, nearly 80% (n = 558) had at least a high school education, 60% (n = 424) were single at the time of the interview, and 40% (n = 289) were primiparous. Approximately two-thirds of the mothers (n = 450) initiated breast-feeding and of these, 25% (n = 177) were breast-feeding at the time of the interview (Table 1).
TABLE 1.
Background characteristics of 702 Maryland Infant Feeding Study participants1
| n = 702 | |
|---|---|
| Maternal characteristics | |
| Age, y | 26.9 ± 6.4 |
| Education category, % | |
| Less than high school | 20.5 |
| High school | 34.1 |
| College | 45.4 |
| Primiparous, % | 41.3 |
| Single, % | 60.3 |
| Stress (1–5)2 | 2.0 ± 0.79 |
| Depression (1–4)2 | 1.4 ± 0.46 |
| Anxiety (1–5)2 | 1.5 ± 0.56 |
| Infant characteristics | |
| Age, % | |
| 0–4 mo | 30.6 |
| 5–8 mo | 35.8 |
| 9–13 mo | 33.6 |
| Race/ethnicity, % | |
| White | 49.6 |
| Hispanic | 14.5 |
| African-American | 36.0 |
| Female infant, % | 47.6 |
| Currently breast-fed, % | 25.2 |
| Ever breast-fed, % | 64.1 |
| Birth weight, g | 3262 ± 640 |
| Low birth weight, % | 8.7 |
Values presented are means ± SD or %.
Mental health scales, with the range of scale scores provided in parentheses.
Seventy-five percent of mothers reported “never” or “almost never” feeling stressed to the 4 symptoms of stress,40%answered “not at all” to the 7 symptoms of depression, and 34% reported “not at all” to the 6 symptoms of anxiety. African-American mothers (2.1 ± 0.82) reported significantly more symptoms of stress than White (1.9 ± 0.74) or Hispanic (2.0 ± 0.86) mothers. Symptoms of maternal stress, depression, or anxiety were not significantly related to maternal age, education, parity, marriage, or infant age, gender, or birth weight.
A 5-factor solution of the feeding style items accounted for 24% of the total variance (Table 2). Items within the responsive feeding style factor negatively correlated with items representing the restrictive (r = −0.36; P < 0. 001) and forceful (r = −0.16; P < 0. 001) feeding factors.
TABLE 2.
Factor-loading matrix of identified child feeding styles
| Description of the individual feeding style items as grouped by factor | Factor loading |
|---|---|
| Factor 1. Responsive feeding style | |
| If my baby fusses or get upset during feeding, I try to figure out the problem.1 | 0.39 |
| I feed my baby when she acts hungry.1 | 0.37 |
| My baby's actions tell me what she wants.1 | 0.47 |
| I keep feeding until my baby shows me she is full.1 | 0.53 |
| I stop feeding my when she turns away or shuts her mouth.1 | 0.34 |
| My baby knows how much she needs to eat.1 | 0.38 |
| Factor 2. Forceful feeding style | |
| I have to trick, distract, or entertain my baby to get her to eat.1 | 0.39 |
| I wake my baby to feed her.1 | 0.30 |
| I have to push the nipple or spoon into my baby's mouth to get her to eat.1 | 0.36 |
| I try to get my baby to eat more to last longer between feedings.1 | 0.37 |
| Do you try to get your baby to finish his breast milk or formula?2 | 0.67 |
| Do you try to get your baby to finish his food?2 | 0.55 |
| Factor 3. Restrictive feeding style | |
| If my baby is hungry before feeding time, I try to get her to wait.1 | 0.39 |
| If I let my baby eat as much as she wants, she will get too big or heavy.1 | 0.60 |
| If I do what my baby wants it will spoil her.1 | 0.40 |
| Are you very careful not to feed your baby too much?2 | 0.39 |
| When others feed your baby, do you worry she'll eat too much?2 | 0.40 |
| Do you carefully control how much your baby eats?2 | 0.44 |
| When others feed your baby, do you worry about the kinds of foods she'll eat?2 | 0.33 |
| Factor 4. Indulgent feeding style | |
| Do you let your baby eat whatever she wants?3 | 0.49 |
| If your baby likes sugary drinks, do you always let her have them?3 | 0.40 |
| If your baby prefers to eat while watching TV, do you let her?3 | 0.37 |
| When your baby cries, do you immediately feed her?3 | 0.30 |
| Factor 5. Uninvolved feeding style | |
| Do you know what infant is eating?3 | 0.55 |
| Do you know when infant is eating?3 | 0.49 |
There were significant associations between maternal and infant background characteristics and feeding style factors. Responsive feeding style scores were positively associated with maternal education, breast-feeding (including current and ever breast-feeding), and female infant gender, and negatively associated with being African American. All other feeding style scores were positively associated with being African American. There were no other characteristics associated with forceful feeding style scores. Restrictive feeding style scores were associated with young maternal age, low education, single parenthood, not currently breast-feeding, male infant gender, and heavier birth weight infant. Indulgent feeding style scores were associated with young maternal age, low education, and male infant gender. Uninvolved feeding style scores were associated with single parenthood and not currently breast-feeding.
The maternal mental health measures were intercorrelated (r = 0.51–0.67; P < 0.001) and were associated with maternal perceptions of infant temperament (r = 0.20–0.26; P < 0.001). Maternal perceptions of difficult infant temperament were associated with low scores on responsive feeding style (r = −0.09; P = 0.02) and high scores on forceful (r = 0.14; P < 0.001), indulgent (r = 0.09; P = 0.04), and uninvolved feeding styles (Spearman’s rho = 0.16; P < 0.001).
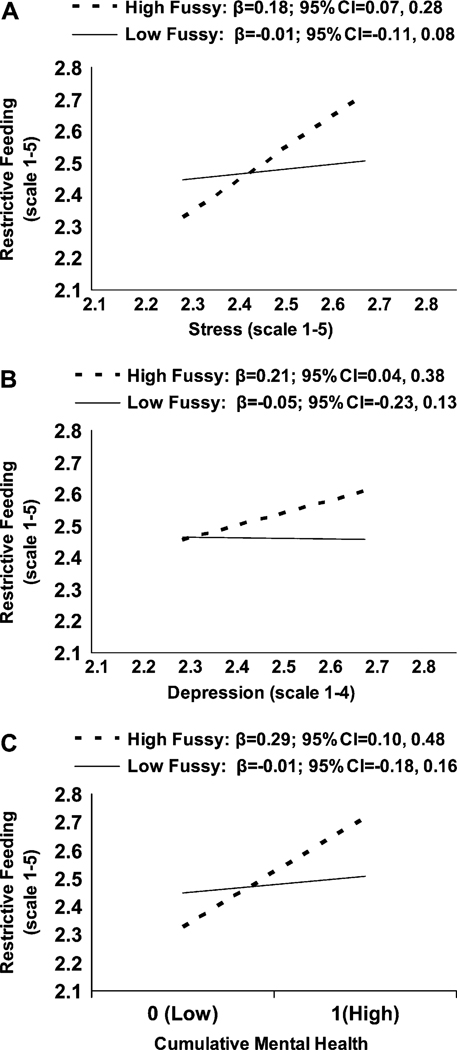
In the prediction of restrictive feeding styles, adjusting for demographic characteristics related to the feeding style variable, there were significant interactions between maternal perceptions of infant temperament and maternal stress (β = 0.26; 95% CI = 0.08, 0.44), depressive symptoms (β = 0.43; 95% CI = 0.14, 0.73), and cumulative mental health symptomatology (β = 0.45; 95% CI = 0.12, 0.78). Among mothers who perceived their infant as temperamentally fussy, there was a significant positive relationship between 3 indices of maternal mental health symptoms (stress, depression, and cumulative mental health) and restrictive feeding style (Fig. 1). In contrast, among mothers who perceived their infant as temperamentally easygoing, there was no relation between maternal mental health indicators and restrictive feeding style.
FIGURE 1.
Moderating effects of perceived infant temperament on the relationship between symptoms of maternal stress (A), depression (B), and cumulative mental health symptomatology (C) and restrictive feeding style scores exist. Because there was a significant interaction between perceived infant temperament and maternal stress, depression, and cumulative mental health symptomatology in the multivariate regression model analysis, the slopes and CI were calculated for both low fussy infant (perceived infant temperament ≤ 1.4) and high fussy infant (perceived infant temperament > 1.4) data.
In multivariate regression analyses, adjusting for demographic characteristics related to the feeding style variable, maternal stress symptomatology was significantly associated with forceful and uninvolved feeding style scores, maternal depression symptomatology was significantly associated with forceful, indulgent, and uninvolved feeding styles scores, and maternal anxiety symptomatology was significantly related to forceful, restrictive, and uninvolved feeding style scores. Finally, the cumulative effects of maternal mental health symptomatology had a significant positive association with forceful and uninvolved feeding style scores (Table 3).
TABLE 3.
Adjusted relationships between maternal mental health scores and feeding styles scores
| Stress | Depression | Anxiety | Cumulative mental health symptomatology | |||||
|---|---|---|---|---|---|---|---|---|
| Feeding styles1 | β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI |
| Responsive feeding2 | 0.13 | (−0.04, 0.07) | 0.05 | (−0.05, 0.14) | −0.03 | (−0.10, 0.05) | 0.004 | (−0.10, 0.09) |
| Forceful feeding3 | 0.03* | (0.02, 0.05) | 0.03* | (0.004, 0.05) | 0.04* | (0.02, 0.06) | 0.04* | (0.02, 0.07) |
| Restrictive feeding4 | IE5 | IE5 | 0.11* | (0.01, 0.21) | IE5 | |||
| Indulgent feeding6 | 0.02 | (−0.002, 0.03) | 0.03* | (0.004, 0.06) | 0.02 | (−0.004, 0.04) | 0.02 | (−0.01, 0.05) |
| Uninvolved feeding7 | 1.4* | (1.1, 1.7) | 1.5* | (1.001, 2.2) | 1.4* | (1.01, 1.9) | 1.5* | (1.1, 2.2) |
Continuous feeding style variables include responsive, forceful, restrictive, and indulgent. Forceful and indulgent feeding style variables were normalized using the natural logarithm, and the uninvolved feeding style factor was dichotomized. Relationship with continuous and dichotomous feeding variables examined using multiple linear and logistic regression models, respectively.
P < 0.05.
Multivariate linear regression used to adjust for maternal education, breastfeeding status, race/ethnicity, and infant age, and infant gender.
Multivariate linear regression used to adjust for race/ethnicity.
Multivariate linear regression used to adjust for maternal age, maternal education, marriage, current breast-feeding status, and race/ethnicity, infant gender, and low birth weight.
Significant interaction effects (IE) between the restrictive feeding style and depression, stress, and cumulative mental health symptomatology were detected in the multivariate regression model and were thus not included in the main effects models but further evaluated in stratified analyses (see Fig. 1).
Multivariate linear regression used to adjust for maternal age, maternal education, race/ethnicity, infant age, and infant gender.
Multivariate logistic regression used to adjust for current breast-feeding status, marriage, and race/ethnicity; findings presented as OR.
Discussion
The findings support our hypothesis that symptoms of maternal stress, depression, or anxiety are significantly associated with maternal reports of nonresponsive (controlling, indulgent, or uninvolved) feeding styles. However, it is unclear whether the effects are specific depending on the type of mental health problem or whether symptoms of mental health in general are related to nonresponsive feeding styles. Conceptually and empirically, symptoms of stress, depression, and anxiety are highly interrelated (38). Mothers who report any mental health symptomatology are more likely to engage in nonresponsive feeding styles. Thus, the current findings suggest that nonresponsive feeding styles are sensitive to an array of maternal mental health symptoms and that a single measure of maternal mental health (e.g. depression screener) may be effective in detecting an increased likelihood of nonresponsive feeding styles.
Consistent with ecological theories of parenting (39–41), the current findings suggest that feeding styles reflect aspects of the mother, the infant, and their relationship. Maternal perceptions of infant temperament are influenced by maternal mental health status (24); mothers who report any mental health symptoms are at risk for reporting temperamental difficulties (fussiness) among their infants (38). Mothers who experience symptoms of stress, depression, or anxiety are likely to view their infant’s behavior in a negative light, which may impact their interactions with their infant. Thus, maternal perceptions of infant temperament may also help detect the likelihood of nonresponsive feeding styles, given the positive relationships with maternal mental health symptomatology and nonresponsive feeding styles.
The association between mental health symptoms and restrictive feeding style varied by maternal perceptions of infant temperament, highlighting the vulnerability of infants perceived to be temperamentally difficult. Under conditions of both mental health symptoms and perceptions of infant fussiness, mothers were likely to report that they used a restrictive feeding style. A restrictive feeding style has been associated with childhood overweight, possibly because children overeat to compensate for the restrictions imposed on them (42,43). There are several possible explanations for the relationship among mental health symptoms, maternal perceptions of infant temperament, and a restrictive feeding style. One possibility is that mothers with mental health symptoms (of depression or stress) restrict their infant’s intake and then misinterpret the infant’s signals of hunger as fussiness. This interpretation is consistent with evidence that mothers with mental health symptoms are not responsive to their infants because they either miss or misinterpret cues (24). Another possibility is that mothers confronted with mental health symptoms and perceptions of a temperamentally fussy infant feel overwhelmed regarding feeding and restrict their infant’s intake, perhaps as a method of punishment. This interpretation is consistent with the anger toward others that often accompanies mental health symptoms (44).
Despite the generality seen between mental health symptomatology and perceived infant temperament, our findings also suggest that specificity may exist between mental health symptomatology and the type of nonresponsive feeding style. Mothers who report stress associated with daily life also report engaging in both forceful and uninvolved feeding styles. Maternal stress may be present when parents are experiencing negative or challenging life situations, and in times of stress, parents tend to exhibit both controlling and uninvolved parenting styles (18). Depending on the situation and personality of the caregiver, 1 or both of these extreme feeding styles may be used in attempt to decrease stress symptomatology.
Mothers with depressive symptoms are likely to engage in forceful, uninvolved, and indulgent feeding styles. The prevalence of maternal depressive symptoms and its associated consequences on parental behaviors and child health, development, and growth have been well documented (45–50). The current findings, extended specifically to mother-infant feeding interactions, are consistent with other studies that have documented that mothers who report depressive symptomatology tend to display a negative affect and be disengaged with their children rather than engaging in positive parent-child interactive behaviors, such as playing, and following routines and infant-care guidelines (46–48).
Finally, this study detected associations between maternal anxiety and controlling feeding styles (6). When children are fussy, messy, or refuse foods, parental anxiety may increase and mealtime experiences can become confrontational and aversive (6). Similar to stress, maternal anxiety may also be present when parents are experiencing negative life events and challenges. These types of situations can be frustrating to parents, causing them to doubt their parenting skills and to increase their level of control. Anxiety is often relieved by exerting control over situations; thus, anxious parents may adopt authoritarian, rather than child-centered, parenting and feeding styles (18).
Parenting is rooted in cultural and social processes and although the authoritative (responsive) parenting typology has generally been considered the optimal parenting style (3,4) there is conflicting evidence regarding generalizability across ethnic groups (51–53). For example, aspects of authoritarian (or controlling) parenting styles have been less predictive of negative outcomes for African American children compared with Caucasian children (54). Thus, further exploration is needed on the role of authoritative parenting styles among African American families.
This research was based on a large, ethnically diverse population-based sample of low-income mothers and infants and is one of the first studies to our knowledge to investigate associations between maternal mental health and feeding styles. Several methodological limitations should be considered when interpreting these findings. First, findings from the current analysis are cross-sectional and do not warrant a causal interpretation of the relationship between maternal mental health and feeding styles. Second, approximately one-half of the mothers in the sampling frame could not be located. Although geographic location of residence, infant gender, or maternal prepregnancy weight did not differ between participants who could and could not be located, Hispanic mothers and mothers of younger infants were more likely to be located than White and African American mothers and mothers of older infants. Third, the findings are based on self-reported questionnaire data, which are subject to reporting bias and inaccuracies that may have underestimated certain associations (55). To date, the 2 studies that have compared self-reported and observed feeding styles have yielded inconsistent findings (30,56). Concordance between self-reported and observed feeding styles is an area requiring further investigation.
This study lays the foundation for further longitudinal and observational studies that utilize multiple measures of feeding styles during early development. These strategies would allow investigators to examine the stability of maternal mental health symptoms, maternal perception of infant temperament, feeding styles, and the specificity and sensitivity of their relationships at different points during early childhood. Finally, these findings provide support for broadening the focus of child nutrition programs to include strategies that incorporate assessment of and counseling about feeding styles and recognize that maternal mental health is related to feeding styles. Further investigations should examine whether interventions that address aspects of maternal mental health have beneficial effects on feeding styles and children’s nutritional status.
Acknowledgments
We thank Kathleen Knolhoff (Maryland WIC Program Director) and Mary Dallavalle (Maryland WIC Nutrition Education Specialist) for their advice regarding study design. The results of this study formed part of the first author’s dissertation research at The Johns Hopkins Bloomberg School of Public Health.
Footnotes
Supported by the Maryland Special Supplemental Nutrition Program for Women, Infants, and Children (WIC).
Author disclosures: K. M. Hurley, M. M. Black, M. A. Papas, and L. E. Caufield, no conflicts of interest.
Abbreviations used: IchQ, Infant Characteristics Questionnaire; PHQ, Patient Health Questionnaire; PSS-4, 4-item Perceived Stress Scale; PRIME-MD, Primary Care Evaluation of Mental Disorders Patient Health Questionnaire; STAI, Spielberger State-Trait Anxiety Inventory; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Literature Cited
- 1.Black M, Hutcheson J, Dubowitz H, Berenson-Howard J. Parenting style and developmental status among children with nonorganic failure-to-thrive. J Pediatr Psychol. 1994;19:689–708. doi: 10.1093/jpepsy/19.6.689. [DOI] [PubMed] [Google Scholar]
- 2.Birch L, Fisher J. Mothers’ child-feeding practices influence daughters’ eating and weight. Am J Clin Nutr. 2000;71:1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baumrind D. Current patterns of parental authority. Dev Psychol Monogr. 1971:1–103. [Google Scholar]
- 4.Hughes S, Power TG, Fisher JO, Mueller S, Nicklas T. Revisiting a neglected construct: parenting styles in a child-feeding context. Appetite. 2005;44:83–92. doi: 10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Birch L, Fisher J. Appetite and eating behavior in children. Pediatr Clin N Am. 1995;42:931–953. doi: 10.1016/s0031-3955(16)40023-4. [DOI] [PubMed] [Google Scholar]
- 6.Farrow C, Blissett J. Is maternal psychopathology related to obesigenic feeding practices at 1 year? Obes Res. 2005;13:1999–2005. doi: 10.1038/oby.2005.245. [DOI] [PubMed] [Google Scholar]
- 7.Fisher J, Mitchell D, Smickiklas-Wright H, Birch L. Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. J Am Diet Assoc. 2002;102:58–64. doi: 10.1016/s0002-8223(02)90017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wardle J, Carnell S, Cooke L. Parental control over feeding and children’s fruit and vegetable intake: how are they related? J Am Diet Assoc. 2005;105:227–232. doi: 10.1016/j.jada.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Johnson S, Birch L. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94:653–661. [PubMed] [Google Scholar]
- 10.Lingberg L, Bohlin G, Hagekull B, Palmerus K. Interactions between mothers and infants showing food refusal. Infant Ment Health J. 1996;17:334–347. [Google Scholar]
- 11.Sander M, Patel R, Le Grice B, Shepherd R. Children with persistent feeding difficulties: an observational analysis of the feeding interactions of problem and non-problem eaters. Health Psychol. 1996;12:64–73. doi: 10.1037//0278-6133.12.1.64. [DOI] [PubMed] [Google Scholar]
- 12.Birch L, Fisher J. The role of experience in the development of children’s eating behavior. In: Capaldi ED, editor. Why we eat what we eat. Washington, DC: American Psychological Association; 1996. pp. 113–141. [Google Scholar]
- 13.Carper J, Fisher J, Birch L. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;35:131–139. doi: 10.1006/appe.2000.0343. [DOI] [PubMed] [Google Scholar]
- 14.Fisher J, Birch L, Smiciklas-Wright H, Picciano M. Breast-feeding through the first year predicts maternal control in feeding and subsequent toddler energy intakes. J Am Diet Assoc. 2000;100:641–646. doi: 10.1016/S0002-8223(00)00190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Albright M, Tamis-LeMonda C. Maternal depressive symptoms in relation to dimensions of parenting in low-income mothers. Appl Dev Sci. 2002;6:24–34. [Google Scholar]
- 16.Bosquet M, Egeland B. Associations among maternal depressive symptomatology, state of mind and parent and child behaviors: implications for attachment-based interventions. Attach Hum Dev. 2001;3:173–199. doi: 10.1080/14616730010058007. [DOI] [PubMed] [Google Scholar]
- 17.Goodman S, Gotlib I. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- 18.Gorden M. Roots of empathy: responsive parenting, caring societies. Keio J Med. 2003;52:236–243. doi: 10.2302/kjm.52.236. [DOI] [PubMed] [Google Scholar]
- 19.Hammen C, editor. Depression runs in families: the social context of risk and resilience in children of depressed mothers. New York: Springer-Verlag; 1991. [Google Scholar]
- 20.Kochanska G, Kuczynski L, Radke-Yarrow M, Welsh J. Resolutions of control episodes between well and affectively ill mothers and their young children. J Abnorm Child Psychol. 1987;15:441–456. doi: 10.1007/BF00916460. [DOI] [PubMed] [Google Scholar]
- 21.Lyons-Ruth K, Wolfe R, Lyubchik A. Depression and parenting of young children: making the case for early preventive mental health services. Harv Rev Psychiatry. 2000;8:148–153. [PubMed] [Google Scholar]
- 22.McCarty C, McMahon R. Mediators of the relation between maternal depressive symptoms and child internalizing and disruptive behavior disorders. J Fam Psychol. 2003;17:545–556. doi: 10.1037/0893-3200.17.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McClure E, Brennen P, Hammen C, Le Brocque R. Parental anxiety disorder, child anxiety disorder, and the perceived parent-child relationship in an Australian high risk sample. J Abnorm Child Psychol. 2001;29:1–10. doi: 10.1023/a:1005260311313. [DOI] [PubMed] [Google Scholar]
- 24.Wachs T. The nature, etiology, and consequences of individual differences in temperament. In: Balter L, Tamis-LeMonda CS, editors. Child psychology: a handbook of contemporary issues. 2nd ed. New York: Psychology Press; 2006. pp. 27–52. [Google Scholar]
- 25.Carey W. Temperament and increased weight gain in infants. Dev Behav Pediatr. 1985;6:128–131. [PubMed] [Google Scholar]
- 26.WIC nutrition risk criteria: a scientific assessment. Washington, DC: National Academy of Science; 1996. Institute of Medicine; pp. 114–169. [PubMed] [Google Scholar]
- 27.Hurley K, Black M, Papas M, Quigg A. Variation in breastfeeding behaviours, perceptions, and experiences by race/ethnicity among a low-income statewide sample of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participants in the United States. Matern Child Nutr. 2008 doi: 10.1111/j.1740-8709.2007.00105.x. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Satter E, Estes P. Feeding your baby. [cited 2008 Jan 21]. Available from: http://www.ellynsatter.com/pdfs/FYB.pdf.
- 29.Birch L, Fisher J, Grimm-Thomas K, Markey C, Sawyer R, Johnson S. Confirmatory factor analysis of the Child Feeding Questionnaire; a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 30.Sacco L, Bentley M, Carby-Shields K, Borja J, Goldman B. Assessment of infant feeding styles among low-income African American mothers: comparing reported and observed reports. Appetite. 2007;49:131–140. doi: 10.1016/j.appet.2007.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 32.Spitzer R, Kroenke K, Williams J. Validation and utility of a self-report version of PRIME_MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Quesitonnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 33.van Knippenberg F, Duivenvoorden H, Bonke B, Passchier J. Shortening the state-trait anxiety inventory. J Clin Epidemiol. 1990;43:995–1000. doi: 10.1016/0895-4356(90)90083-2. [DOI] [PubMed] [Google Scholar]
- 34.Marteau T, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) Br J Clin Psychol. 1992;31:301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 35.Bates J, Freeland C, Lounsbury M. Measurement of infant difficulties. Child Dev. 1979;50:794–803. [PubMed] [Google Scholar]
- 36.Rosner B. Fundamental of biostatistics. 6th ed. Duxbury: Sage Thomson Brooks/Cole; 2006. [Google Scholar]
- 37.Base SPSS. 15 for Windows. Rel. 15. Chicago: SPSS Inc; 2007. [Google Scholar]
- 38.Moffitt T, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory A, Poulton R. Depression and generalized anxiety disorder: cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Arch Gen Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- 39.Belsky J. The determinents of parenting: a process model. Child Dev. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- 40.Bronfenbrenner U. Making human beings human: bioecological perspectives on human development. Thousand Oaks (CA): Sage Publication Ltd; 2005. [Google Scholar]
- 41.Bronfenbrenner U, Ceci S. Nature-nurture reconceptualized in developmental perspective: a bioecological model. Psychol Rev. 1994;101:568–586. doi: 10.1037/0033-295x.101.4.568. [DOI] [PubMed] [Google Scholar]
- 42.Faith M, Scanlon K, Birch L, La F, Sherry B. Parent-child feeding strategies and their relationships to child eating and weight status. Obes Res. 2004;12:1711–1722. doi: 10.1038/oby.2004.212. [DOI] [PubMed] [Google Scholar]
- 43.Faith M, Kerns J. Infant and child feeding practices and childhood overweight: the role of restriction. Matern Child Nutr. 2005;1:164–168. doi: 10.1111/j.1740-8709.2005.00024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lovejoy M, Graczyz P, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 45.Dennis C, McQueen K. Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatr. 2007;96:590–594. doi: 10.1111/j.1651-2227.2007.00184.x. [DOI] [PubMed] [Google Scholar]
- 46.McLearn K, Minkovitz C, Strobino D, Marks E, Hou W. Maternal depressive symptoms at 2 to 4 months post partum and early parenting practices. Arch Pediatr Adolesc Med. 2006;160:279–284. doi: 10.1001/archpedi.160.3.279. [DOI] [PubMed] [Google Scholar]
- 47.McLearn K, Minkovitz C, Strobino D, Marks E, Hou W. The timing of maternal depressive symptoms and mothers’ parenting practices with young children: implications for pediatric practice. Pediatrics. 2006;118:e174–e182. doi: 10.1542/peds.2005-1551. [DOI] [PubMed] [Google Scholar]
- 48.Paulson J, Dauber S, Leiferman J. Individual and combined effects of postpartum depression in mothers and fathers on parening behavior. Pediatrics. 2006;118:659–668. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- 49.Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness. Arch Gen Psychiatry. 2004;61:946–952. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- 50.Tomlinson M, Cooper PJ, Stein A, Swartz L, Molteno C. Post-partum depression and infant growth in a South African peri-urban settlement. Child Care Health Dev. 2006;32:81–86. doi: 10.1111/j.1365-2214.2006.00598.x. [DOI] [PubMed] [Google Scholar]
- 51.Avenevoli S, Sessa F, Steinberg L. Family structure, parenting practices, and adolescent adjustement: an ecological examination. In: Hetherington EM, editor. Coping with divorce, single parenting, and remarriage: a risk and resiliency perspective. Mahwah (NJ): Erlbaum; 1999. [Google Scholar]
- 52.Deater-Deckard K, Dodge K, Bates J, Pettit G. Physical discipline among African-American and European American mothers: links to children’s externalizing behaviors. Dev Psychol. 1996;32:1065–1072. [Google Scholar]
- 53.Gonzales N, Hirage Y, Cauce A. Observing mother-daughter interaction in African-American and Asian American families. In: McCubbin HI, Thompson EA, Thompson AI, Futrell JA, editors. Resiliency in African-American Families. Thousand Oaks (CA): Sage; 1998. pp. 259–286. [Google Scholar]
- 54.Iannotti R, O’Brian R, Spillman D. Parental and peer influences on food consumption of preschool African-American children. Percept Mot Skills. 1994;79:747–752. doi: 10.2466/pms.1994.79.2.747. [DOI] [PubMed] [Google Scholar]
- 55.Baranowski T, Cullen KW, Baranowski J. Psychosocial correlates of dietary intake: advancing dietary intervention. Annu Rev Nutr. 1999;19:17–40. doi: 10.1146/annurev.nutr.19.1.17. [DOI] [PubMed] [Google Scholar]
- 56.Hughes S, Patrick H, Power T, Fisher J, Anderson C, Nicklas T. The impact of child care providers’ feeding on children’s food consumption. J Dev Behav Pediatr. 2007;28:100–107. doi: 10.1097/01.DBP.0000267561.34199.a9. [DOI] [PubMed] [Google Scholar]