Abstract
Background
The aim of the present study was to determine the population-based prevalence of diabetes mellitus (DM) and prediabetes in a rural district of Daegu City, Korea.
Methods
Between August and November 2003, a community-based health survey of adults aged 20 years and older was performed in the rural district of Dalseong-gun in Daegu City. A total of 1,806 of all eligible individuals agreed to participate. Fasting plasma glucose was measured in all participants. Two hour oral glucose tolerance was measured in the 1,773 participants for whom there was neither an established diagnosis of DM nor evidence of DM according to fasting glucose levels. The prevalence of DM and prediabetes was determined according to the 2003 criteria of the American Diabetes Association. Subjects with prediabetes were classified into one of three categories of glucose intolerance: isolated impaired fasting glucose (IFG); isolated impaired glucose tolerance (IGT); or combined IFG and IGT.
Results
The prevalence of DM was 12.2%. The highest prevalence rates were observed in subjects in their seventies. A total of 34.7% of all subjects who were assigned a diagnosis of DM in the present study had not been diagnosed previously. The prevalence of prediabetes was 22.7%. The highest prevalence rates were observed in subjects in their fifties.
Conclusion
The present study identified prevalence rates of 12.2% for DM (age-standardized prevalence rate [ASR], 6.8%), and 22.7% for prediabetes (ASR 18.5%). These results emphasize the need for community health promotion strategies to prevent or delay the onset of DM in individuals with prediabetes.
Keywords: Diabetes mellitus, Epidemiology, Prediabetic state
INTRODUCTION
In South Korea, economic development and altered eating patterns have been accompanied by increased rates of overweight, obesity, and diabetes mellitus (DM) [1,2]. The prevalence of diabetes mellitus (DM) in South Korea has increased over the past three decades, from 0.91% in Jeollabuk-do Province in 1971 to 7.2% in Yonchon in 1993, and from 7.1% in Jungup in 1997 to 13.7% in Namwon in 1999, and most dramatically, to 20.5% and 22.1% in southwestern Seoul in 1999 and 2002, respectively [1-8].
A study in the Korean city of Daegu in 2001 demonstrated that endocrine disease was the fifth leading cause of death, and that DM in particular had been associated with a two-fold increase in mortality over the preceding decade [9]. In 2003, a hypertension-DM management center was established in Daegu to facilitate the prevention and early treatment of DM and hypertension. This initiative was the result of collaboration between public and private health care providers. An epidemiological research team was created to investigate the prevalence of hypertension, DM, and metabolic syndrome in local residents, and to recruit a cohort to investigate disease incidence over a 5-year period, as well as determination of risk and prognostic factors.
The aim of the present study was to determine the prevalence of DM and prediabetes in the population of the rural district of Dalseong-gun in Daegu, a population which is less mobile than those in other areas of Daegu City.
METHODS
Study subjects
Between August and November 2003, a community-based health survey was performed in Dalseong-gun to determine the prevalence of DM and prediabetes in adults aged 20 years or older. Dalseong-gun is a rural district of Daegu, Korea. According to the 2000 census, approximately 101,104 of its residents are above the age of 20 years. The study population was selected using a multi-stage cluster sampling method without use of a weight factor. The catchment areas of nine primary health care centers were selected as collection districts. Two or three villages from each collection district were then selected at random. Thus, a total of 26 villages were sampled and 1,806 individuals were recruited.
A total of 1,773 subjects (681 men and 1,092 women) underwent a full evaluation of glucose tolerance status. Since metabolic risk factor data were available for only 1,755 of the 1,773 subjects, only these were included in the analysis of metabolic risk factors. The study was approved by the Institutional Review Board of Kyungpook National University Hospital, and all subjects provided written informed consent.
Methods
All subjects underwent a standardized series of physical examinations that were performed by trained personnel. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured in the sitting position after a 10-minute period of rest. The average of two blood pressure readings was used in the analysis. Weight (measured without shoes and in light outdoor clothing) and height were measured, and body mass index (BMI, kg/m2) was calculated by dividing weight (kg) by height squared (m2). Waist circumference was measured midway between the lower rib margin and the iliac crest at the end of expiration.
All blood samples were taken in the morning following an overnight fast of at least eight hours. Venous blood was drawn with minimal stasis from the antecubital vein. In all subjects, fasting capillary whole blood glucose was measured with an Accu Check® glucometer (Roche Diagnostics, Penzberg, Germany), and fasting plasma glucose was measured with a Beckman Glucose Analyzer® (Beckman Instruments, Irvine, CA, USA). All eligible participants were then subjected to an oral glucose tolerance test (OGTT). A 75-g glucose solution was administered orally, and plasma glucose was measured after an interval of two hours. Participants with known DM or a fasting capillary whole blood glucose level of ≥200 mg/dL were excluded from the analysis of oral glucose tolerance. In these participants, DM was confirmed by re-checking fasting plasma glucose levels. Serum total cholesterol (TC), triglycerides (TG), and high density lipoprotein cholesterol (HDL-C) were measured using enzymatic methods (Dimension AR; Dade Behring Inc., Deerfield, IL, USA).
DM and prediabetes were diagnosed according to the 2003 criteria of the American Diabetes Association (ADA) [10]. A subject was considered to have known DM if they were receiving pharmacological treatment for DM at the time of inclusion in the study, irrespective of their measured glucose levels. Subjects with a fasting plasma glucose level of ≥126 mg/dL or a 2-hour post-load plasma glucose level of ≥200 mg/dL were assigned a diagnosis of DM. Subjects with prediabetes were classified into one of three categories: isolated impaired fasting glucose (I-IFG), isolated impaired glucose tolerance (I-IGT), or combined IFG and IGT (C-IFG/IGT) [10,11]. I-IFG was defined by a fasting plasma glucose level of between 100 and 125 mg/dL, and a 2-hour post-load plasma glucose level of <140 mg/dL. I-IGT was defined by a fasting plasma glucose level of <100 mg/dL, and a 2-hour post-load plasma glucose level of between 140 and 199 mg/dL. C-IFG/IGT was defined by a fasting plasma glucose level of between 100 and 125 mg/dL, and a 2-hour post-load plasma glucose level of between 140 and 199 mg/dL.
Statistical analysis
The age-standardized prevalence rate (ASR) of DM and prediabetes and the 95% confidence interval (CI) were calculated using the 2005 Korean population (aged 20 to 99 years) as the standard population. The age groups 20 to 39, 40 to 49, 50 to 59, 60 to 69, and ≥70 years were considered separately. The chi-square test was used to analyze differences in the prevalence of DM and prediabetes between the sexes and different age groups. For both DM and prediabetes, prevalence was analyzed without use of a weight factor. Logistic regression models were used to assess the relationship between metabolic risk factors and DM and prediabetes. All data were analyzed using the SPSS statistical package version 15.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Demographic characteristics
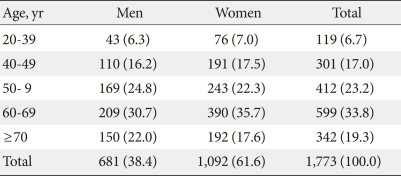
Data from 1,773 subjects were analyzed (681 men, 38.4%; 1,092 women, 61.6%). The mean age was 58.7 years (59.1 in men, 58.5 in women) (Table 1).
Table 1.
Age and sex of study subjects
Data are presented as number (%).
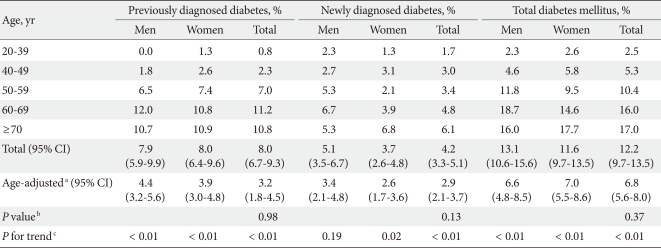
Prevalence of diabetes mellitus
The prevalence of DM was 12.2% (ASR 6.8%). No statistically significant difference in the prevalence of DM was observed between men and women (13.1% [ASR 6.6%] in men; 11.6% [ASR 7.0%] in women). A total of 34.7% of all subjects who were assigned a diagnosis of DM had not been previously diagnosed (39.3% men, 31.5% women). The prevalence of DM increased with age, and peaked in the age-group ≥70 years (P for trend<0.01). The highest prevalence rates were detected in the age group 60 to 69 years for men (P for trend<0.01) and in the age group ≥70 years for women (P for trend<0.01) (Table 2).
Table 2.
Prevalence of diabetes mellitus according to sex and age
CI, confidence interval.
aAge-adjusted prevalence (%), bP value for comparison between men and women, cP value for trend across increasing age.
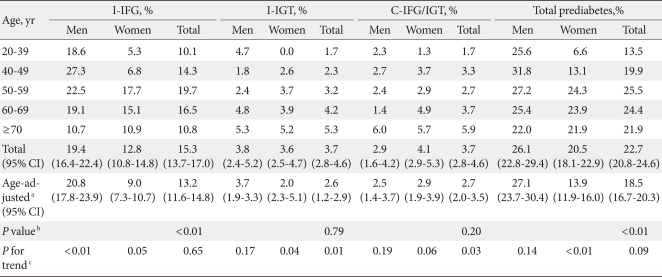
Prevalence of prediabetes
The prevalence of prediabetes was 22.7% (ASR 18.5%) overall, 26.1% (ASR 27.1%) in men and 20.5% (ASR 13.9%) in women. The prevalence of I-IFG was 15.3% (ASR 13.2%), 19.4% (ASR 20.8%) in men and 12.8% (ASR 9.0%) in women. The prevalence of I-IGT was 3.7% (ASR 2.6%), 3.8% (ASR 3.7%) in men and 3.6% (ASR 2.0%) in women. The prevalence of C-IFG/IGT was 3.7% (ASR 2.7%), 2.9% (ASR 2.5%) in men and 4.1% (ASR 2.9%) in women. The prevalence of I-IFG was significantly higher than that of I-IGT or C-IFG/IGT (P<0.01) (Table 3).
Table 3.
Prevalence of prediabetes according to sex and age
C-IFG/IGT, combined impaired fasting glucose and impaired glucose tolerance; I-IFG, isolated impaired fasting glucose; I-IGT, isolated impaired glucose tolerance, CI, confidence interval.
aAge-adjusted prevalence (%), bP value for comparison between men and women, cP value for trend across increasing age.
The prevalence of prediabetes increased with age and peaked at 25.5% in the 50 to 59 year age group (P for trend<0.01). In men, the prevalence of prediabetes peaked at 31.8% in the age group 40 to 49 years. In women, the prevalence of prediabetes peaked at 24.3% in the age group 50 to 59 years. The prevalence of I-IFG did not increase with age and peaked at 19.7% in the age group 50 to 59 years. In men, the prevalence of I-IFG peaked at 27.3% in the age group 40 to 49 years. In women, the prevalence of I-IFG peaked at 17.7% in the age group 50 to 59 years. The prevalence of I-IGT increased with age (P for trend=0.01), and peaked in the age group ≥70 years at 5.3% for men and 5.2% for women. When the sexes were considered separately, the prevalence of I-IGT was found to increase with age in women (P for trend=0.04), but not in men. The prevalence of C-IFG/IGT also increased with age (P for trend=0.03), and peaked in the age group ≥70 years at 6.0% for men and 5.7% for women (Table 3).
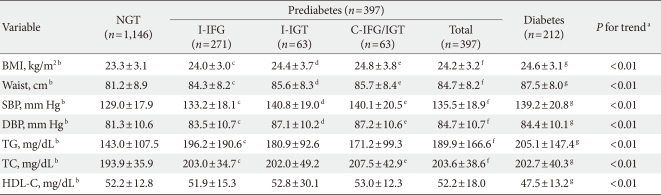
Associated metabolic risk factors
The analyses of metabolic risk factors revealed that BMI, waist circumference, SBP, and DBP were significantly higher in the I-IFG, I-IGT, C-IFG/IGT, and DM groups than in the normal glucose tolerance (NGT) group (P<0.01). TG levels were significantly higher in the I-IFG and DM groups than in the NGT group (P<0.01). TC was significantly higher in the I-IFG, C-IFG/IGT, and DM groups than in the NGT group (P<0.01). HDL-C was significantly lower only in the DM group compared to the NGT group (P<0.01). BMI, waist circumference, SBP, DBP, TG, and TC were significantly increased and HDL-C was significantly decreased in the prediabetes group compared to the NGT group. Differences with the NGT group were more pronounced for subjects with DM than for subjects with prediabetes (P for trend<0.01) (Table 4).
Table 4.
Associated metabolic risk factors according to diagnostic criteria (n=1,755)
NGT, normal glucose tolerance; I-IFG, isolated impaired fasting glucose; I-IGT, isolated impaired glucose tolerance; C-IFG/IGT, combined impaired fasting glucose and impaired glucose tolerance; BMI, body mass index; Waist, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TG, triglyceride; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol.
a"P for trend" was used to compare normal, prediabetes, and diabetes groups, bExpressed as mean±SD, cSignificant difference of normal/isolated impaired fasting glucose (P<0.05), dSignificant difference of normal/isolated impaired glucose tolerance (P<0.05), eSignificant difference of normal/combined impaired fasting glucose and impaired glucose tolerance (P<0.05), fSignificant difference of normal/prediabetes (P<0.05), gSignificant difference of normal/diabetes (P<0.05).
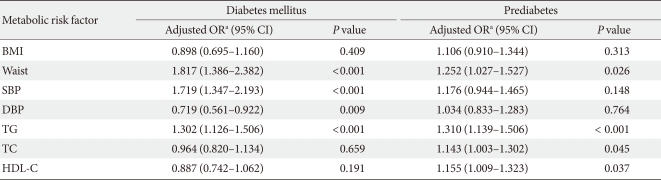
Multiple logistic regression analysis adjusted for age and sex, and using standardized values as variables, showed that the following metabolic risk factors were associated with DM: waist circumference (odds ratio [OR], 1.817; P<0.001), SBP (OR, 1.719; P<0.001), DBP (OR, 0.719; P=0.009), and TG (OR, 1.302; P<0.001). Multiple logistic regression analysis adjusted for age and sex, and using standardized values as variables, showed that the following metabolic risk factors were associated with prediabetes: waist circumference (OR, 1.252; P=0.026), TG (OR, 1.310; P<0.001), TC (OR, 1.143; P=0.045), and HDL-C (OR, 1.155; P=0.037) (Table 5).
Table 5.
Multiple logistic regression analysis of the relationship between metabolic risk factors and diabetes mellitus and prediabetes
OR, odds ratio; CI, confidence interval; BMI, body mass index; Waist, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TG, triglyceride; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol.
aOR adjusted for age and sex using standardized values as variables, P<0.05 is statistically significant.
DISCUSSION
The prevalence of DM in Dalseong-gun, Daegu, Korea was 12.2% (ASR 6.8%), 13.1% (ASR 6.6%) in men and 11.6% (ASR 7.0%) in women. In both sexes, the prevalence of DM increased significantly with age, and the most pronounced increase was observed in the fifth decade of life. The highest prevalence rates were found for men in the age group 60 to 69 years and women in the age group ≥70 years.
Previous studies have investigated the prevalence of DM in Korea using the 1997 criteria of the ADA. A prevalence of 7.1% was reported in Jungup in 1997, and a study in Namwon in 1999 reported a prevalence of 13.7% [5,7]. Studies performed within the context of the Korean National Health and Nutritional Survey reported that the prevalence of DM decreased between 1998 and 2001 in both sexes [12,13]. Rates of 12% in men and 9.7% in women were found in 1998, compared with 9.0% and 7.2%, respectively, in 2001 [12,13]. According to an analysis of the Korean National Health Insurance Database on Diabetes in 2003, the prevalence of DM was 7.7% [14]. The mean age of the subjects in the present study was 58.7 years, which is higher than in previous studies. The ASR of DM in the present study was lower than that reported in previous studies in Korea [5,7,12-14]. The reason for this is unclear. The prevalence of diabetes may be lower in rural areas, where the population follows a more traditional lifestyle, than in urban areas. Furthermore, the present study included relatively young subjects, because the inclusion criterion was an age of 20 years or above. Comparisons with previous findings may thus be limited, since previous studies tended to only include subjects who were above the age of 30 or 40 years.
Previous studies have shown that the prevalence of DM was positively correlated with age, and that there was a rapid increase in DM prevalence during the fifth and sixth decades of life [5-7,12,13]. The present results are consistent with those of a study in the Korean district of Jungup. This study showed that the prevalence of DM increased significantly throughout middle age in both sexes, and that the highest prevalence rates were in the age group 50 to 59 years for men and ≥70 years for women [5]. In the 1998 Korean National Health and Nutritional Survey study, the prevalence of DM increased throughout middle age, and the highest prevalence rates were observed in men in their fifties and in women in their sixties [12]. In the 2005 Korean National Health and Nutritional Survey study, the highest prevalence rates were found for men in their fifties and women in their seventies [13].
In the present study, 34.7% of all subjects who were assigned a diagnosis of DM had not been diagnosed previously. The percentage of newly diagnosed subjects was approximately 50% lower than the percentages reported from comparable studies [5,7]. In particular, the ratio of newly to previously diagnosed DM in the present population was lower in the ≥50 year age groups than in the 20 to 49 year age groups. Early detection of DM appears to have increased in recent years as a result of screening programs. However, the present study has demonstrated that many subjects with DM were undiagnosed and untreated.
In the present study, the prevalence of prediabetes was 22.7% (ASR 18.5%). The most common category of prediabetes was I-IFG, which accounted for 67.4% of all subjects with prediabetes. Together I-IGT and C-IFG/IGT accounted for 16.3% of all subjects with prediabetes. The prevalence of prediabetes was significantly higher in men than in women (P<0.01), and the prevalence of I-IFG was also significantly higher in men than in women (P<0.01). However, the prevalence of I-IGT and C-IFG/IGT did not differ between the sexes. The highest prevalence of I-IFG was found in subjects in their fifties, and the rate decreased above the age of 60. However, the prevalence of I-IGT and C-IFG/IGT increased significantly with age.
In 1999, Weyer et al. [15] were the first to classify prediabetes into three categories of glucose intolerance: I-IFG, I-IGT, and C-IFG/IGT. The normal range of fasting plasma glucose was defined as <110 mg/dL, and this cutoff was applied by both the ADA and the World Health Organization (WHO) in their 1997 diagnostic criteria [16,17]. In 2001, the International Diabetes Federation (IDF) defined prediabetes according to the same criteria as the WHO [11]. However, the 2003 criteria of the ADA defined the normal range of fasting plasma glucose as <100 mg/dL [10]. Therefore, the prevalence of prediabetes identified in the present study cannot be directly compared with that reported by previous studies in Korea because different fasting plasma glucose cutoff values were used. A population study performed at a health promotion center in Gyeonggi-do in 2006 reported that 46.4% of subjects had prediabetes. Of these, 20.7% had I-IFG, 7.7% had I-IGT, and 18.0% had C-IFG/IGT [18]. It is impossible to directly compare the results of this study with the present findings, since a fasting plasma glucose cut off value of <110 mg/dL was used [18]. Yet, the prevalence of prediabetes in the present study was lower, despite the use of a lower fasting plasma glucose cutoff value of <100 mg/dL. Recently, a pooled analysis of four large-scale Korean community-based studies was performed. This included data from the 1993 Yonchon study, the 1997 Mokdong study, the 1997 Jungup study, and the 2000 Ansan study [19]. Using the optimal cutoff point for fasting plasma glucose of 100 mg/dL, the prevalence of prediabetes was found to be 29.8% (I-IFG 17.0%, I-IGT 6.7%, and C-IFG/IGT 6.1%) [19]. Thus, the study reported a higher prevalence of prediabetes than in the present study. However, it disclosed lower rates of I-IFG compared to I-IGT and C-IFG/IGT than in the present study [19].
Several studies have investigated the pathophysiology of IFG and IGT [11,15,20-26]. In the majority of the populations studied, IGT was more prevalent than IFG, and differences in phenotype and gender distribution were observed between the two categories [11]. The 5-year Inter99 study of a Danish population suggested that I-IFG appears to be caused by impaired basal insulin secretion and first-phase insulin release, and a subsequent decline in hepatic insulin sensitivity [22]. In contrast, the authors suggested that the I-IGT may be caused by low whole body insulin sensitivity and a progressive decline in β-cell function, which indicates a loss of β-cell compensation [22]. This implies there are differences in pathogenesis between the various forms of prediabetes, and thus in the risk of developing DM. The findings of the present study suggest that Korean individuals with prediabetes are genetically more susceptible to inherent insulin secretory dysfunction and hepatic insulin resistance than to an inadequate compensatory insulin secretory response and peripheral insulin resistance. Further studies are warranted to determine whether IFG is more prevalent than IGT in the Korean population as a whole.
According to an IDF consensus statement on IGT/IFG in 2001, the prevalence of IFG tends to plateau in 40 to 50 year age group and is more common in men than in women in virtually all age groups [11]. Conversely, the prevalence of IGT is higher in women than in men in all age groups, with the exception of the over 60 age group in Asian populations [11]. These findings are consistent with the present findings. Other recent epidemiological studies have reported similar sex differences in the prevalence of IFG and IGT, with IFG being more common in men and IGT more common in women [27,28]. It has been hypothesized that the finding of a higher prevalence of IGT in women may result from the use of a fixed glucose load in the OGTT irrespective of body size, despite the fact that women generally have a smaller stature and less muscle mass than men [27]. It is unclear whether other factors may influence these results, since studies in a number of geographically and ethnically diverse populations have demonstrated sex differences [28]. Further studies will be necessary to establish whether our results apply to other populations, and to elucidate the mechanisms underlying sex differences in glucose metabolism.
The present study identified significant differences in DM-associated metabolic risk factors such as BMI, waist circumference, SBP, DBP, TG, TC, and HDL-C between the NGT group and the prediabetes and DM groups. Thus, the present findings are in accordance with those of previous studies and suggest that prediabetes is associated with cardiovascular risk factors, such as hypertension and dyslipidemia [7,11,12].
The present study had several limitations. Previous studies from Korea used different standard populations and applied different diagnostic criteria for DM and prediabetes. Thus, the prevalence of DM and prediabetes identified in the present study cannot be compared directly to those reported by previous studies. Caution should be exercised in interpreting the results as an indication of the epidemiology of DM in Korea, since the investigation of the Dalseong cohort represents a well-controlled epidemiological survey.
In conclusion, the prevalence of DM in the present rural cohort was 12.2% (ASR 6.8%), and that of prediabetes was 22.7% (ASR 18.5%). These findings could be used as baseline data for a 5-year follow-up study of the prevalence and incidence of DM and prediabetes, and of the risk factors associated with the development of DM in the Dalseong-gun community. The present study has demonstrated the effectiveness of community health promotion strategies in facilitating the early detection and prevention of DM through a liaison between public and private health services. Such strategies are a useful tool in evaluating past and current health promotion policies, and in establishing long-term national health promotion policies.
ACKNOWLEDGMENTS
This study was funded by a grant from the Daegu Medical Association. We are grateful to the Daegu Metropolitan City and to the Daegu Medical Association for their support. We also wish to thank the Dalseong Public Health Center, the Daegu and Kyungpook Committees of the Korean Diabetes Association, and the Korean Society of Cardiology. The authors have no competing financial interests to disclose.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129–2140. doi: 10.1001/jama.2009.726. [DOI] [PubMed] [Google Scholar]
- 2.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 3.Lee DY, Kim EJ, Kim KS, Choi CH. Epidemiological study on diabetes mellitus among rural Korean. J Korean Diabetes Assoc. 1972;1:17–24. [Google Scholar]
- 4.Park Y, Lee H, Koh CS, Min H, Yoo K, Kim Y, Shin Y. Prevalence of diabetes and IGT in Yonchon County, South Korea. Diabetes Care. 1995;18:545–548. doi: 10.2337/diacare.18.4.545. [DOI] [PubMed] [Google Scholar]
- 5.Kim YI, Choi CS, Kim SW, Lee JS, Kim HH, Lee MS, Lee SI, Park JY, Hong SK, Lee KU. Prevalence of diabetes mellitus and impaired glucose tolerance in Korean adults living in Jungup district, South Korea. J Korean Diabetes Assoc. 1998;22:363–371. [Google Scholar]
- 6.Oh JY, Lee HJ, Hong ES, Hong YS, Sung YA, Lee SH. The prevalence and incidence of diabetes in Mokdong, Seoul. J Korean Diabetes Assoc. 2003;27:73–83. [Google Scholar]
- 7.Kim SG, Yang SW, Jang AS, Seo JP, Han SW, Yeom CH, Kim YC, Oh SH, Kim JS, Nam HS, Chung DJ, Chung MY. Prevalence of diabetes mellitus in the elderly of Namwon county, South Korea. Korean J Intern Med. 2002;17:180–190. doi: 10.3904/kjim.2002.17.3.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee KW, Kim DJ, Park JR, Yoo HJ, Park SY, Kwon SB, Ryu OH, Park SS, Kim HY, Seo JA, Oh JH, Kim SG, Kim NH, Choi KM, Baik SH, Choi DS. The change of prevalence of diabetes mellitus for 3 years and incidence of diabetes in Koreans over 60 years old. Korean J Med. 2004;67:607–614. [Google Scholar]
- 9.Chun BY, Lee KS, Lee JY. Study on the problem diagnosis of the district health care 'death and life style'. Daegu: Medical Institute, Kyungpook National University Hospital; 2001. [Google Scholar]
- 10.Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, Nathan D, Palmer J, Rizza R, Saudek C, Shaw J, Steffes M, Stern M, Tuomilehto J, Zimmet P Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 11.Unwin N, Shaw J, Zimmet P, Alberti KG. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med. 2002;19:708–723. doi: 10.1046/j.1464-5491.2002.00835.x. [DOI] [PubMed] [Google Scholar]
- 12.Kim CS, Jeong EK, Park J, Cho MH, Nam JS, Kim HJ, Kong JH, Park JS, Nam JY, Kim DM, Ahn CW, Cha BS, Lim SK, Kim KR, Lee HC, Nam CM. Prevalence of diabetes mellitus (fasting plasma glucose by the ADA criteria) and impaired fasting glucose according to anthropometric characteristics and dietary habits: 1998 National Health and Nutrition Survey. J Korean Diabetes Assoc. 2005;29:151–166. [Google Scholar]
- 13.Oh KW, Jang MJ, Lee JM, Lee YK, Kim YT. A report of diabetes epidemic in the Korean population. The 3rd Korean National Health and Nutrition Examination Survey (2005) Clin Diabetes. 2007;8:361–365. [Google Scholar]
- 14.Korean Diabetes Association; Health Insurance Review & Assessment Service. Report of task force team for basic statistical study of Korean diabetes mellitus: diabetes in Korea 2007. Seoul: Goldfishery; 2007. pp. 1–57. [Google Scholar]
- 15.Weyer C, Bogardus C, Pratley RE. Metabolic characteristics of individuals with impaired fasting glucose and/or impaired glucose tolerance. Diabetes. 1999;48:2197–2203. doi: 10.2337/diabetes.48.11.2197. [DOI] [PubMed] [Google Scholar]
- 16.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation. Part1: diagnosis and classification of diabetes mellitus. Geneva: World Health Organization; 1999. [Google Scholar]
- 18.Kong MH, Choi HK, Jung AJ, Ahn BH, Kim BT, Kim KM. The prevalence of metabolic syndrome according to the degree of glucose metabolism impairment. J Korean Acad Fam Med. 2006;27:182–189. [Google Scholar]
- 19.Oh JY, Lim S, Kim DJ, Kim NH, Kim DJ, Moon SD, Jang HC, Cho YM, Song KH, Ahn CW, Sung YA, Park JY, Shin C, Lee HK, Park KS Committee of the Korean Diabetes Association on the Diagnosis and Classification of Diabetes Mellitus. A report on the diagnosis of intermediate hyperglycemia in Korea: a pooled analysis of four community-based cohort studies. Diabetes Res Clin Pract. 2008;80:463–468. doi: 10.1016/j.diabres.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 20.Sicree RA, Zimmet PZ, Dunstan DW, Cameron AJ, Welborn TA, Shaw JE. Differences in height explain gender differences in the response to the oral glucose tolerance test: the AusDiab study. Diabet Med. 2008;25:296–302. doi: 10.1111/j.1464-5491.2007.02362.x. [DOI] [PubMed] [Google Scholar]
- 21.Williams JW, Zimmet PZ, Shaw JE, de Courten MP, Cameron AJ, Chitson P, Tuomilehto J, Alberti KG. Gender differences in the prevalence of impaired fasting glycaemia and impaired glucose tolerance in Mauritius. Does sex matter? Diabet Med. 2003;20:915–920. doi: 10.1046/j.1464-5491.2003.01059.x. [DOI] [PubMed] [Google Scholar]
- 22.Faerch K, Vaag A, Holst JJ, Hansen T, Jorgensen T, Borch-Johnsen K. Natural history of insulin sensitivity and insulin secretion in the progression from normal glucose tolerance to impaired fasting glycemia and impaired glucose tolerance: the Inter99 study. Diabetes Care. 2009;32:439–444. doi: 10.2337/dc08-1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faerch K, Vaag A, Holst JJ, Glumer C, Pedersen O, Borch-Johnsen K. Impaired fasting glycaemia vs impaired glucose tolerance: similar impairment of pancreatic alpha and beta cell function but differential roles of incretin hormones and insulin action. Diabetologia. 2008;51:853–861. doi: 10.1007/s00125-008-0951-x. [DOI] [PubMed] [Google Scholar]
- 24.Hanefeld M, Koehler C, Fuecker K, Henkel E, Schaper F, Temelkova-Kurktschiev T Impaired Glucose Tolerance for Atherosclerosis and Diabetes study. Insulin secretion and insulin sensitivity pattern is different in isolated impaired glucose tolerance and impaired fasting glucose: the risk factor in Impaired Glucose Tolerance for Atherosclerosis and Diabetes study. Diabetes Care. 2003;26:868–874. doi: 10.2337/diacare.26.3.868. [DOI] [PubMed] [Google Scholar]
- 25.Laakso M, Zilinskaite J, Hansen T, Boesgaard TW, Vanttinen M, Stancakova A, Jansson PA, Pellme F, Holst JJ, Kuulasmaa T, Hribal ML, Sesti G, Stefan N, Fritsche A, Haring H, Pedersen O, Smith U EUGENE2 Consortium. Insulin sensitivity, insulin release and glucagon-like peptide-1 levels in persons with impaired fasting glucose and/or impaired glucose tolerance in the EUGENE2 study. Diabetologia. 2008;51:502–511. doi: 10.1007/s00125-007-0899-2. [DOI] [PubMed] [Google Scholar]
- 26.Bock G, Dalla Man C, Campioni M, Chittilapilly E, Basu R, Toffolo G, Cobelli C, Rizza R. Pathogenesis of pre-diabetes: mechanisms of fasting and postprandial hyperglycemia in people with impaired fasting glucose and/or impaired glucose tolerance. Diabetes. 2006;55:3536–3549. doi: 10.2337/db06-0319. [DOI] [PubMed] [Google Scholar]
- 27.Meyer C, Pimenta W, Woerle HJ, Van Haeften T, Szoke E, Mitrakou A, Gerich J. Different mechanisms for impaired fasting glucose and impaired postprandial glucose tolerance in humans. Diabetes Care. 2006;29:1909–1914. doi: 10.2337/dc06-0438. [DOI] [PubMed] [Google Scholar]
- 28.Abdul-Ghani MA, Jenkinson CP, Richardson DK, Tripathy D, DeFronzo RA. Insulin secretion and action in subjects with impaired fasting glucose and impaired glucose tolerance: results from the Veterans Administration Genetic Epidemiology Study. Diabetes. 2006;55:1430–1435. doi: 10.2337/db05-1200. [DOI] [PubMed] [Google Scholar]