Abstract
Background. Augmentation index (AIx) is traditionally obtained from pressure waveforms via arterial applanation tonometry. We sought to evaluate the association between AIx obtained from peripheral arterial tonometry (PAT) with cardiovascular risk factors (CRF) and coronary artery disease (CAD). Methods. 186 patients were enrolled in the study. The presence or absence of CRFs and CAD was assessed in each subject. AIx was calculated by an automated algorithm averaging pulse wave amplitude data obtained via PAT. Central blood pressures were assessed in a subset of patients undergoing clinically indicated cardiac catheterization. Results. An association was observed between AIx and age, heart rate, systolic blood pressure, mean arterial pressure, pulse pressure, body weight and body mass index. AIx was significantly lower in patients with <3 CRFs compared to those with >5 CRFs ( P = .02). CAD+ patients had significantly higher AIx compared to CAD− patients ( P = .008). Area under the ROC curve was 0.604 (P < .01). In patients undergoing cardiac catheterization, after adjusting for age, height and heart rate, AIx was a significant predictor of aortic systolic and pulse pressures (P < .05) Conclusion. AIx derived from PAT correlates with cardiac risk factors and CAD. It may be a useful measure of assessing overall risk for coronary artery disease.
1. Introduction
A portion of the arterial pressure wave travelling towards the extremities is reflected back from peripheral impedance points. In healthy individuals, the reflected wave returns to the aorta during diastole. With age and in the presence of vascular disease, arterial compliance decreases, and the arteries become stiff, thereby reducing the transit time for the incident and reflected waves. Consequently, the reflected wave arrives at the aorta during systole of the same cardiac cycle augmenting the central blood pressures. This augmentation of central pressure can be quantified by augmentation index (AIx), defined as the percentage of the central pulse pressure attributed to the reflected pulse wave.
AIx has been shown to be associated with cardiovascular risk [1], predicts the presence or absence of coronary artery disease (CAD) [2, 3], and has been shown to be an independent predictor of cardiovascular events and all-cause mortality in select patient populations [4, 5]. Conventionally, AIx is obtained from pressure waveforms via applanation tonometry of the carotid or radial arteries. Recently, it has been demonstrated that AIx can be measured from digital pulse wave volumes by peripheral arterial tonometry (PAT) [6, 7], and that it is associated with ventricular-vascular coupling [8]. The value obtained by AIx derived by PAT correlates with that obtained by conventional radial applanation tonometry; however, they cannot be used interchangeably since the actual values do not match since they are obtained from two distinct vascular beds via two different methods. Little is known about the pathophysiological correlates of PAT-derived AIx. Therefore, we sought to evaluate the association between PAT-derived AIx and cardiovascular risk factors (CRFs) and/or CAD.
2. Methods
2.1. Patient Population
Study 1 —
146 patients recruited from the Cardiology Clinic at Tufts Medical Center in Boston were enrolled in the study. Subjects were instructed to fast overnight and to refrain from smoking, caffeine, or alcohol on the day of testing. Vasoactive medicines were withheld for a period of 12 hours prior to testing.
Study 2 —
40 consecutive patients undergoing clinically indicated nonemergent left heart catheterization were retrospectively identified for inclusion into this study. As part of the standard catheterization protocol, blood pressures were measured within the femoral artery, ascending aorta, and the left ventricle using a 6-French end hole fluid-filled catheter and a pressure manometer prior to injection of any contrast agent. Pressures within the ascending aorta were considered as the central blood pressure (CBP) in the study.
The presence or absence of the following cardiovascular risk factors was assessed in all the subjects from both substudies: male gender, hypertension (systolic blood pressure >140 mmHg, diastolic blood pressure >90 mmHg, or being on an antihypertensive medication), hyperlipidemia (serum cholesterol >220 mg/dL or taking lipid-lowering medication), diabetes mellitus (fasting blood glucose >140 mg/dL or on oral hypoglycemics or insulin), family history of CAD (first-or second-degree relatives with premature CAD), postmenopausal women, and smoking (having smoked at least five times per day within last month). CAD was defined as the presence of ischemia or infarction on single-photon emission-computed tomographic (SPECT) nuclear myocardial perfusion imaging or >50% stenosis of an epicardial coronary artery by angiography.
Patients with moderate to severe heart failure (NYHA class III-IV, LVEF < 35), hemodynamic instability, peripheral arterial disease (Ankle-brachial Index <0.9), and finger deformities were excluded from the study. This study was approved by the Institutional Review Board at Tufts Medical Center. A written informed consent was obtained from all subjects.
2.2. Augmentation Index Measured by Peripheral Arterial Tonometry (PAT-AIx)
Prior to collecting vascular measures, all study subjects rested in a quiet dark room for a period of 10 minutes. Post-acclimatization, the vascular data was recorded by PAT (EndoPAT2000, Itamar Medical Ltd, Caesarea, Israel) for a period of 5 minutes with the patient in supine position. The procedure for obtaining AIx is essentially the same as described in previous reports [9]. The probes, lined by inflatable balloons, are connected to isolated volume reservoirs within the machine, which buffer pressure changes and provide a uniform pressure field. Also, the counter-pressure imparted by the balloon prevents distal venous distension and blood pooling, which might induce a local venoarteriolar vasoconstriction reflex [10, 11]. The PAT system is designed to unload arterial wall tension and increase the range of arterial wall motion without inducing potentially confounding vasomotor changes. Pressure sensors within this cap capture beat-by-beat finger pulse wave amplitude (PWA) which is then filtered, amplified, and graphically displayed on a computer screen. A computerized algorithm has been generated to automatically identify peak pressures and inflection point as previously described by Kelly et al. [12] and Takazawa [13]. PAT-AIx is calculated by averaging the PWA data over an epoch of 3.5 minutes and is calculated by the following formula: PAT-AIx = (P2 − P1) × 100 / P1(%), where P1 = pulse pressure and P2 = pressure corresponding to the inflection point.
2.3. Statistical Analysis
Data were entered into MS-Excel and analyzed with SPSS (SPSS Inc., Chicago, Ill, USA). Data are expressed as mean ± SEM. A priori significance was set at P < .05. Normality of distributions was assessed using Kolmogorov-Smirnov and Shapiro-Wilk tests. Continuous variables were analyzed according to the student t-test and Pearson correlation. Dichotomous variables were analyzed by means of the χ2 analysis. Cardiac risk factors (age >45 yrs in men and >55 yrs in women, male gender, menopause, hypertension, hypercholesterolemia, cigarette smoking, diabetes mellitus and family history of CAD) were tabulated as nominal variables. Depending upon the total number of CRFs per patient, the study population was divided into tertiles, including those with <3 CRFs, 3–5 CRFs, and >5 CRFs. Analysis of variance (for parametric data) with Scheffe post hoc testing was performed to assess difference in continuous variables between groups. A stepwise multiple regression analysis was performed to examine predictors of AIx. Binary logistic regression analysis (0.05 to enter, 0.10 to remove) was used to evaluate for relationship between AIx and CAD and to evaluate for potential confounders including age, gender, height, heart rate, presence of hypertension, hypercholesterolemia, diabetes mellitus, tobacco use, and family history of CAD. A receiver operator characteristic (ROC) curve was generated to determine the predictive power of AIx for CAD.
3. Results
3.1. Subject Population
186 subjects (129 men, 57 women) with an average age of 59 ± 1 years were enrolled. 61% of women were postmenopausal, and 35% were on hormone replacement therapy. 55% patients had CAD, 52% patients had hypertension, 24% were diabetic, 58% had hypercholesterolemia, 44% were smokers, and 35% had family history of CAD. Detailed characteristics of the study population are described in Table 1.
Table 1.
Study population characteristics.
| Total population (n = 186) | Number of cardiac risk factors | P value | |||
|---|---|---|---|---|---|
| <3 (n = 64) | 3–5 (n = 77) | >5 (n = 44) | |||
| Age, yrs | 59 ± 1 | 54 ± 1∗† | 60 ± 1 | 61 ± 1 | .0001 |
| Females, n (%) | 57 (36) | 18 (51)∗† | 28 (41) | 11 (13) | .01 |
| Menopause, n (%) | 35 (61) | 12 (67)* | 14 (50) | 9 (81)‡∗ | .01 |
| Heart rate, beats per minute | 68 ± 1 | 70 ± 1∗† | 66 ± 1 | 64 ± 2 | .04 |
| Mean arterial pressure, mmHg | 103 ± 1 | 99 ± 2∗† | 103 ± 1 | 106 ± 1 | .009 |
| Systolic blood pressure, mmHg | 128 ± 1 | 124 ± 2 | 129 ± 2 | 127 ± 2 | .18 |
| Diastolic blood pressure, mmHg | 76 ± 1 | 78 ± 1 | 76 ± 1 | 71 ± 1∗‡ | .006 |
| Pulse pressure, mmHg | 51 ± 1 | 45 ± 1∗† | 52 ± 1 | 56 ± 2 | .008 |
| Height, inches | 67.8 ± 0.5 | 65 ± 1∗† | 68 ± 0.5 | 70 ± 0.3 | .01 |
| Weight, pounds | 192.9 ± 2.8 | 183 ± 6† | 191 ± 3† | 209 ± 4 | .02 |
| Body mass index, kg/m2 | 29.7 ± 0.4 | 29.5 ± 1 | 29.4 ± 1.8 | 30.7 ± 0.6∗‡ | .06 |
| Total cholesterol, mg/dL | 174 ± 3 | 194 ± 5∗† | 168 ± 4 | 155 ± 6.3 | .03 |
| HDL cholesterol, mg/dL | 42 ± 9 | 50 ± 2∗† | 39 ± 2 | 36 ± 9 | .03 |
| LDL cholesterol, mg/dL | 103 ± 3 | 116 ± 7∗† | 99 ± 5 | 92 ± 5 | .04 |
| Triglycerides, mg/dL | 158 ± 10 | 131 ± 11 | 170 ± 19 | 152 ± 15 | .290 |
| Hypertension, n (%) | 96 (52) | 6 (17) | 31 (46)†‡ | 59 (71)∗‡ | .03 |
| Diabetes mellitus, n (%) | 44 (24) | 0 (0) | 9 (14)‡† | 35 (42)∗‡ | .0001 |
| Hypercholesterolemia, n (%) | 109 (58) | 2 (6) | 37 (54)‡† | 70 (84)∗‡ | .0001 |
| Smoke, n (%) | 82 (44) | 7 (20) | 27 (40) | 48 (58) | .201 |
| Family history, n (%) | 65 (35) | 5 (14) | 23 (34)‡† | 37 (45)‡ | .001 |
| Coronary artery disease, n (%) | 102 (55) | 7 (11) | 53 (68)‡† | 42 (95)‡ | .001 |
| Augmentation index, (%) | −4.86 ± 1.4 | −5.15 ± 2.09† | −3.60 ± 1.69 | 5.65 ± 2.55 | .02 |
‡Significantly different from cohort with <3 CRFs.
*Significantly different from cohort with 3–5 CRFs
†Significantly different from cohort with >5 CRFs.
3.2. Relationship between Peripheral AIx and Cardiac Risk Factors
A significant association was observed between PAT-AIx and age (r = 0.265, P < .0001), heart rate (r = −0.299, P < .0001), diastolic blood pressure (r = −0.285, P < .0001), mean arterial pressure (r = 0.170, P < .045), and pulse pressure (r = 0.198, P = .012). The relationship between PAT-AIx and age best fitted a quadratic regression model (P = .01). AIx was not associated with diabetes mellitus, smoking status, or family history of CAD. Similarly, no significant correlation was observed between PAT-AIx and systolic blood pressure, gender, height, and lipids. Stepwise multiple regression analysis identified age, heart rate, diastolic blood pressure, weight, and cigarette smoking as predictors of PAT-AIx. Analysis of variance (Scheffe post hoc testing) revealed a significant difference in AIx between patients with <3 CRFs (−5.15 ± 2.09%) and those having >5 CRFs (5.65 ± 2.55%, P = .02, Figure 1). PAT-AIx in patients with 3–5 cardiac risk factors was not significantly different than in those with either <3 or >5 CRFs.
Figure 1.
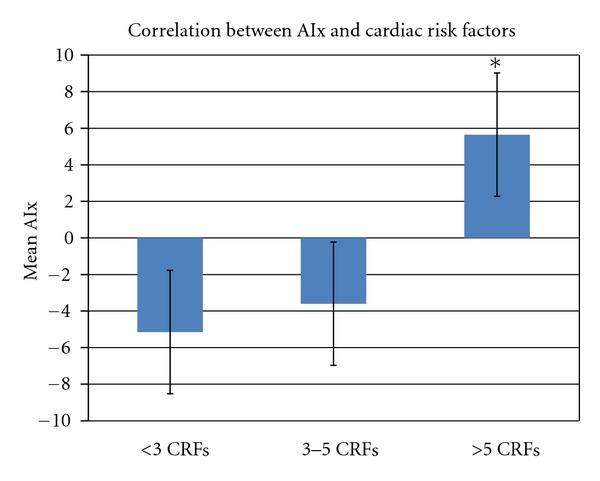
Patients with >5 cardiac risk factors had a significantly higher PAT-AIx compared to those with <3 CRFs (P = .02). PAT-AIx in patients with 3–5 cardiac risk factors was not significantly different from those with <3 or >5 CRFs.
3.3. Relationship between Peripheral AIx and CAD
PAT-AIx was significantly higher amongst CAD+ patients (1.01 ± 1.6%) as compared to CAD− patients (−5.46 ± 1.7%, P = .008, Figure 2). To examine the ability of PAT-AIx to predict CAD+, the area under the ROC curve yielded a value of 0.604 (P < .01, Figure 3). After dividing the study population into tertiles based on the PAT-AIx values, there was a stepwise increase in prevalence of CAD with an increase in PAT-AIx (P < .05, Figure 4). However, after adjusting for potential confounders, including age, sex, heart rate, smoking, diabetes, hypertension, and hypercholesterolemia, PAT-AIx was not significantly different between these two groups.
Figure 2.
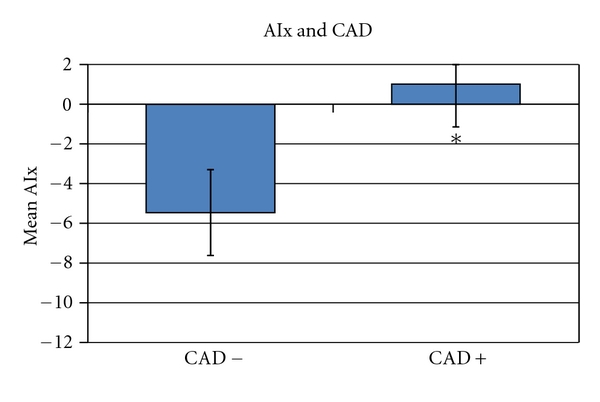
CAD− patients have significantly lower PAT-AIx values than CAD+ patients (P = .008).
Figure 3.
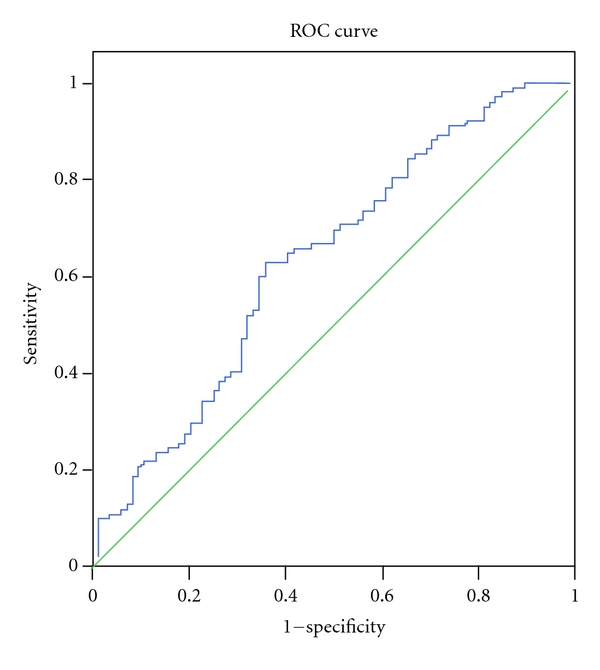
The classification performance of peripheral AIx, assessed by generating a receiver operated characteristic curve, revealed an AUC of 0.604 (P < .01).
Figure 4.
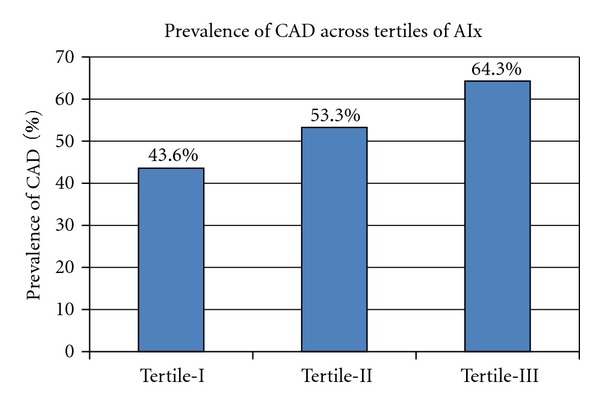
Prevalence of CAD in study patients divided into tertiles based on their PAT-AIx results. The highest number of CAD cases was found in the tertile with the highest PAT-AIx values (Tertile III). Tertile I, having the lowest PAT-AIx values, had the lowest number of CAD cases.
3.4. Relationship between Digital AIx and Central Blood Pressures
A positive correlation was noted between peripherally derived AIx and centrally measured blood pressures. PAT-AIx correlated with aortic systolic pressure (r = 0.480, P = .002, Figure 5), and aortic pulse pressures (r = 0.455, P = .004, Figure 6). After adjusting for age, height, and heart rate, AIx remained a significant predictor of aortic systolic pressure (β = 0.449, 95% CI 0.187–0.712, P = .001) and aortic pulse pressure (β = 0.424, 95% CI 0.042–0.805, P = .0031).
Figure 5.
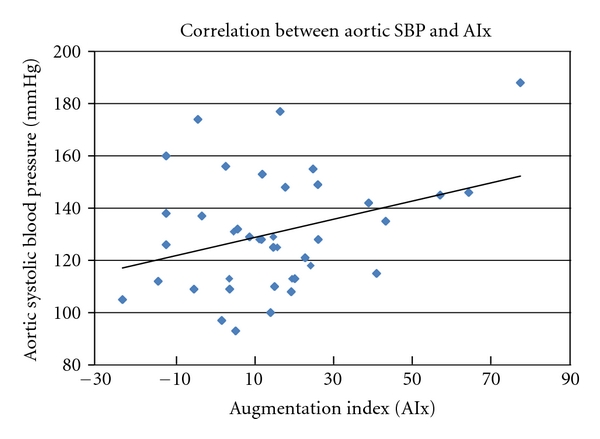
Positive correlation between PAT-AIx and aortic systolic blood pressure (r = 0.480, P = .002).
Figure 6.
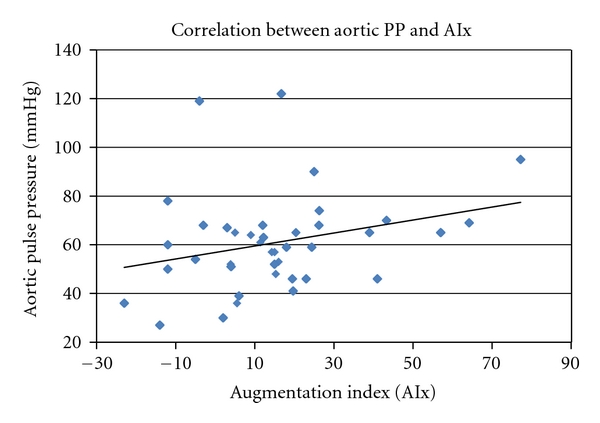
Positive correlation between PAT-AIx and aortic pulse pressure (r = 0.455, P = .004).
3.5. Relationship between Peripheral AIx and Medications
Analysis focusing on effects of medications on peripheral augmentation index revealed a significant association between PAT-AIx with beta-blockers (P = .018) and ACE inhibitors (P = .03). There was no association between PAT-AIx and calcium blockers, angiotensinogen receptor blockers, nitrates, statins, digoxin, diuretics, oral hypoglycemics, insulin, thyroid hormone supplements, antidepressants, and steroids.
4. Discussion
Our study was undertaken to evaluate the association of peripheral AIx and cardiovascular risk factors. Similar to what has been found with AIx derived from applanation tonometry [1], PAT-derived AIx correlates with age, weight, BMI, heart rate, diastolic blood pressure, pulse pressure, and mean arterial pressure. PAT-AIx was also significantly related to age. Previous studies have noted that the increase in AIx with age is not linear [1]. In alignment with previously published data, a quadratic model best illustrates the relationship between age and PAT-AIx. AIx values increased with age up to 65–70 years of age. Beyond that, the AIx values tended to plateau and then decrease shortly after that. It has been observed that AIx measured by conventional applanation tonometry begins to plateau at the age of 60 years. This observed difference can be explained in part by impedance matching. Impedance matching may differ in the hand circulation versus the aorta as there may not be changes in digital endothelial function with aging [14].
PAT-AIx was associated with the cumulative CRFs burden in this study population. Patients with >5 CRFs had a significantly higher PAT-AIx as compared with those having only a few CRFs. Similarly, when the prevalence of CAD was assessed across tertiles of PAT-AIx, it was noted that patients in the highest tertile had a significantly higher prevalence of CAD as compared to those in the lower tertiles.
PAT-AIx was able to discern the presence or absence of CAD amongst a heterogeneous patient population with varying in cardiovascular risk. The classification performance of peripheral AIx was assessed by generating a receiver-operated characteristic curve which revealed an AUC of 0.604. However, after adjusting for traditional risk factors such as age, sex, heart rate, height, weight, hypertension, diabetes mellitus, hypercholesterolemia, smoking, and family history of premature coronary heart disease, AIx lost its statistical significance. Thus, PAT-derived AIx is not an independent predictor of CAD in this population.
The importance of assessing central blood pressure lies in the fact that traditionally measured brachial artery blood pressure is often a poor representation of actual central pressures. Due to pressure wave amplification, the brachial systolic pressure can be up to 20 mmHg higher than the aortic systolic pressure [15–17]. Since the left ventricle works against pressures within the ascending aorta, aortic pressures play a significant role in the pathophysiology of cardiac disease. As such, aortic systolic and pulse pressures can be considered as novel cardiovascular risk factors since they are predictors of cardiovascular events, target organ damage, and mortality [18]. Compared to brachial systolic and pulse pressure, aortic pulse pressure appears to be a better predictor of the presence and extent of coronary atherosclerosis [19, 20] and restenosis after coronary intervention [21]. Furthermore, a reduction in central blood pressure results in a reduction in cardiac hypertrophy, vascular thickness, and adverse cardiac events [22–24]. For example, a 10 mmHg reduction in aortic pulse pressure has been shown to translate into a 13–15% reduction in CV events and all-cause mortality [25, 26]. In alignment with data published by Munir et al. [27], our study reveals that AIx measured by PAT also closely correlates with central aortic blood pressures.
We do acknowledge certain limitations in this study. While it has been suggested that arterial stiffness and augmented pressure from wave reflections make the most significant contributions to the digital volume pulse inflection point, vascular correlates or PAT-AIx remain unexplored. CAD was defined on the basis of diagnosis with angiography and/or positive SPECT imaging. It is true that SPECT imaging results do not always correlate with severity of coronary artery stenosis. However, we chose stress testing because it provides physiologic information regarding ischemia and prior infarction. While SPECT imaging does not confer 100% sensitivity and specificity, this technique is a reliable, noninvasive assessment of myocardial ischemia/infarction. In Substudy 2, central pressures were obtained using conventional fluid-filled catheters, rather than high-fidelity pressure transducers. In addition, AIx was not obtained simultaneously during catheterization when actual central pressure values were obtained. Rather, PAT was performed at the bedside following cardiac catheterization.
5. Conclusion
PAT has been under investigation over recent years as a technique for assessment of vascular endothelial function. The present data suggest that this simple, noninvasive technique may also provide information regarding augmentation index. Our findings suggest that finger-derived AIx may be comparable to applanation tonometry for measurement of augmentation index and evaluation of cardiovascular risk. However, as observed by Haller et al. [6], although the values of AIx obtained by PAT correlate with that obtained by conventional radial applanation tonometry, they cannot be used interchangeably since the actual numbers do not match. Additional research is needed to identify the underlying vascular physiology modulating PAT-AIx. Further validation is warranted in large scale studies comparing PAT-AIx with that obtained by the current gold standard radial applanation tonometry in a wider patient population.
Disclosures
Funding for K. S. Heffernan provided by NIH T32 HL069770-06. The peripheral arterial tonometer (PAT) finger probes were provided by Itamar Medical, LTD, Caesarea, Israel.
References
- 1.Nurnberger J, Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schafers RF. Augmentation index is associated with cardiovascular risk. Journal of Hypertension. 2002;20(12):2407–2414. doi: 10.1097/00004872-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Weber T, Auer J, O’Rourke MF, et al. Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation. 2004;109(2):184–189. doi: 10.1161/01.CIR.0000105767.94169.E3. [DOI] [PubMed] [Google Scholar]
- 3.Hayashi T, Nakayama Y, Tsumura K, Yoshimaru K, Ueda H. Reflection in the arterial system and the risk of coronary heart disease. American Journal of Hypertension. 2002;15(5):405–409. doi: 10.1016/s0895-7061(02)02260-4. [DOI] [PubMed] [Google Scholar]
- 4.Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. European Heart Journal. 2006;27(21):2588–2605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 5.London GM, Blacher J, Pannier B, Guérin AP, Marchais SJ, Safar ME. Arterial wave reflections and survival in end-stage renal failure. Hypertension. 2001;38(3):434–438. doi: 10.1161/01.hyp.38.3.434. [DOI] [PubMed] [Google Scholar]
- 6.Haller MJ, Silverstein JH, Shuster JJ. Correlation between radial artery tonometry- and fingertip tonometry-derived augmentation index in children with type 1 diabetes. Diabetes and Vascular Disease Research. 2007;4(1):p. 66. doi: 10.3132/dvdr.2007.011. [DOI] [PubMed] [Google Scholar]
- 7.Peled N, Shitrit D, Fox BD, et al. Peripheral arterial stiffness and endothelial dysfunction in idiopathic and scleroderma associated pulmonary arterial hypertension. Journal of Rheumatology. 2009;36(5):970–975. doi: 10.3899/jrheum.081088. [DOI] [PubMed] [Google Scholar]
- 8.Heffernan KS, Patvardhan EA, Hession M, Ruan J, Karas RH, Kuvin JT. Elevated augmentation index derived from peripheral arterial tonometry is associated with abnormal ventricular-vascular coupling. Clinical Physiology and Functional Imaging. 2010;30(5):313–317. doi: 10.1111/j.1475-097X.2010.00943.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuvin JT, Patel AR, Sliney KA, et al. Assessment of peripheral vascular endothelial function with finger arterial pulse wave amplitude. American Heart Journal. 2003;146(1):168–174. doi: 10.1016/S0002-8703(03)00094-2. [DOI] [PubMed] [Google Scholar]
- 10.Henriksen O. Local reflex in microcirculation in human subcutaneous tissue. Acta Physiologica Scandinavica. 1976;97(4):447–456. doi: 10.1111/j.1748-1716.1976.tb10284.x. [DOI] [PubMed] [Google Scholar]
- 11.Rayman G, Hassan A, Tooke JE. Blood flow in the skin of the foot related to posture in diabetes mellitus. British Medical Journal. 1986;292(6513):87–90. doi: 10.1136/bmj.292.6513.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelly R, Hayward C, Ganis J, Daley J, Avolio A, O’Rourke M. Non-invasive registration of the arterial pressure pulse waveform using high-fidelity applanation tonometry. Journal of Vascular Medicine and Biology. 1989;3:142–149. [Google Scholar]
- 13.Takazawa K. A clinical study of the second component of left ventricular systolic pressure. Journal of Tokyo Women's Medical College. 1987;45:256–270. [Google Scholar]
- 14.Hamburg NM, Keyes MJ, Larson MG, et al. Cross-sectional relations of digital vascular function to cardiovascular risk factors in the framingham heart study. Circulation. 2008;117(19):2467–2474. doi: 10.1161/CIRCULATIONAHA.107.748574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nichols WW, O’Rourke MF. McDonald's Blood Flow in Arteries: Theoretical, Experimental and Clinical Principles. Hodder Arnold; 2005. [Google Scholar]
- 16.Protogerou AD, Papaioannou TG, Blacher J, Papamichael CM, Lekakis JP, Safar ME. Central blood pressures: do we need them in the management of cardiovascular disease? Is it a feasible therapeutic target? Journal of Hypertension. 2007;25(2):265–272. doi: 10.1097/HJH.0b013e3280114f23. [DOI] [PubMed] [Google Scholar]
- 17.Pauca AL, Wallenhaupt SL, Kon ND, Tucker WY. Does radial artery pressure accurately reflect aortic pressure? Chest. 1992;102(4):1193–1198. doi: 10.1378/chest.102.4.1193. [DOI] [PubMed] [Google Scholar]
- 18.Agabiti-Rosei E, Mancia G, O’Rourke MF, et al. Central blood pressure measurements and antihypertensive therapy: a consensus document. Hypertension. 2007;50(1):154–160. doi: 10.1161/HYPERTENSIONAHA.107.090068. [DOI] [PubMed] [Google Scholar]
- 19.Jankowski P, Kawecka-Jaszcz K, Czarnecka D, et al. Ascending aortic, but not brachial blood pressure-derived indices are related to coronary atherosclerosis. Atherosclerosis. 2004;176(1):151–155. doi: 10.1016/j.atherosclerosis.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 20.Danchin N, Benetos A, Lopez-Sublet M, Demicheli T, Safar M, Mourad JJ. Aortic pulse pressure is related to the presence and extent of coronary artery disease in men undergoing diagnostic coronary angiography: a multicenter study. American Journal of Hypertension. 2004;17(2):129–133. doi: 10.1016/j.amjhyper.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Nakayama Y, Tsumura K, Yamashita N, Yoshimaru K, Hayashi T. Pulsatility of ascending aortic pressure waveform is a powerful predictor of restenosis after percutaneous transluminal coronary angioplasty. Circulation. 2000;101(5):470–472. doi: 10.1161/01.cir.101.5.470. [DOI] [PubMed] [Google Scholar]
- 22.Poulter NR, Wedel H, Dahlöf B, et al. Role of blood pressure and other variables in the differential cardiovascular event rates noted in the anglo-scandinavian cardiac outcomes trial-blood pressure lowering arm (ascot-bpla) Lancet. 2005;366(9489):907–913. doi: 10.1016/S0140-6736(05)67186-3. [DOI] [PubMed] [Google Scholar]
- 23.Williams B, Lacy PS, Thom SM, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the conduit artery function evaluation (CAFE) study. Circulation. 2006;113(9):1213–1225. doi: 10.1161/CIRCULATIONAHA.105.595496. [DOI] [PubMed] [Google Scholar]
- 24.Boutouyrie P, Bussy C, Hayoz D, et al. Local pulse pressure and regression of arterial wall hypertrophy during long-term antihypertensive treatment. Circulation. 2000;101(22):2601–2606. doi: 10.1161/01.cir.101.22.2601. [DOI] [PubMed] [Google Scholar]
- 25.Jankowski P, Kawecka-Jaszcz K, Czarnecka D, et al. Pulsatile but not steady component of blood pressure predicts cardiovascular events in coronary patients. Hypertension. 2008;51(4):848–855. doi: 10.1161/HYPERTENSIONAHA.107.101725. [DOI] [PubMed] [Google Scholar]
- 26.Chirinos JA, Zambrano JP, Chakko S, et al. Aortic pressure augmentation predicts adverse cardiovascular events in patients with established coronary artery disease. Hypertension. 2005;45(5):980–985. doi: 10.1161/01.HYP.0000165025.16381.44. [DOI] [PubMed] [Google Scholar]
- 27.Munir S, Guilcher A, Kamalesh T, et al. Peripheral augmentation index defines the relationship between central and peripheral pulse pressure. Hypertension. 2008;51(1):112–118. doi: 10.1161/HYPERTENSIONAHA.107.096016. [DOI] [PubMed] [Google Scholar]


