Abstract
Objective
To identify stress and stress-relieving mechanisms among second-year pharmacy students in a 3-year doctor of pharmacy (PharmD) program using a Mastery Learning Educational Model and to compare findings with those from a 4-year program.
Methods
Second-year PharmD students in a 3-year program were asked to complete a series of questionnaires including the Perceived Stress Scale (PSS) regarding stress and stress-relieving activities.
Results
The average PSS score for the 3-year PharmD cohort was significantly higher than the score of demographically similar students enrolled in a 4-year PharmD program (P = 0.04). There were significant differences between the 2 groups’ scores on 5 items on the PSS including how often they: were upset because something happened unexpectedly, felt unable to control important things, felt nervous and stressed, thought about things that had to be accomplished, and were able to control the way they spent their time. The rate of prescription drug misuse among those in the 3-year PharmD program was 11.6%.
Conclusions
Students in a 3-year PharmD program with a unique educational model experienced more stress than students in a traditional 4-year PharmD program.
Keywords: doctor of pharmacy students, mental health, stress
INTRODUCTION
Stress can cause deleterious effects on health, academic performance, and job performance.1-5 Common stress-relieving activities among college students include the use of alcohol and prescription medications.6 Because of its potentially negative effects, stress has been measured in health professions students, including PharmD students.7-12
According to the Accreditation Council for Pharmacy Education (ACPE), colleges and schools of pharmacy should actively investigate students’ levels of stress.13 Such analyses potentially could result in the elimination of certain stress-causing activities, possibly improving students’ overall health and academic performance. Only a few colleges and schools of pharmacy have published findings on student stress.8-12 Recently, student stress results from a 4-year PharmD program were published.11 A 3-year PharmD program may be more stressful than a 4-year traditional program because the curricular requirements are completed in a shorter timeframe. This was observed in nursing students in an accelerated program who experienced consistently higher stress levels compared to nursing students in a traditional program.14
The 3-year PharmD program at the University of Southern Nevada (USN) uses a mastery-learning model and a block system of curricular design. This educational model has been in place since the inception of the college in 2001. The program includes 72 weeks of didactic instruction and 14 weeks of introductory pharmacy practice experiences (IPPE) in the first 2 years of the program. The third year consists of a minimum of 36 weeks of advanced pharmacy practice experiences (APPE). During the didactic component of the curriculum, students focus on a single block of material until the block is complete. The material is presented for 6 hours each day, consisting of traditional classroom instruction along with active-learning activities. This focused time allows for active learning and formative feedback to ensure that the students master the content of the block of material. Summative assessments are scheduled every other week, and students are required to achieve a score of 90% or better to demonstrate mastery of the content. Students are required to achieve this passing standard on every assessment, and a traditional letter grading system is not used. If a score of 90% or better is not achieved, a student is required to attend a remediation session and then be reassessed. If the material is not mastered after the reassessment, then the student is required to remediate the material in the summer; however, only a limited number of blocks may be remediated in the summer. Despite the 90% mastery requirement, attrition rates have not exceeded 3% since the program's inception.
The purpose of this study was to identify the degree of perceived stress and coping mechanisms in second-year pharmacy students in a 3-year PharmD program in which a block system of curricular design and a mastery learning educational model are used. A secondary objective was to compare the amount of student stress identified in this 3-year program to that identified in a published study of a 4-year program.11,15
METHODS
Second-year doctor of pharmacy students in a 3-year program were asked to complete a series of questionnaires regarding stress and stress-relieving activities. The timing of questionnaire administration, 6 weeks prior to starting APPEs, was chosen to best represent an average level of stress throughout the year based on student performance on assessments, and to approximate the point in the curriculum at which the published study of the 4-year program took place. Students eligible for the study included all second-year PharmD students. The research protocol and tools were approved by the university's institutional review board, and the students were informed that all survey responses were anonymous and could not be identified by the researchers. Students also were able to anonymously opt out of the study at any time or skip any items on the questionnaire that they did not wish to answer.
The previously validated Perceived Stress Scale (PSS),17 which is an objective measure of psychological stress, was administered in addition to the questionnaire created by the research team. The questionnaire encompassed demographic information, stressful events and stress-relieving activities identified in the comparative study, and possible stress-causing and stress-relieving activities identified by the authors, including medication use habits. The surveys were conducted in a classroom setting using SurveyMonkey, an online electronic survey instrument that can be completed anonymously.
Study participants were given the 14-question PSS, which asks students to identify how often they experience specific feelings related to stress.17 All responses on the PSS are ranked using a Likert type 5-point scale ranging from 0 to 4. However, positively stated questions are scored in reverse order, ie, the lowest possible stress score is 0, while the highest possible stress score is 56. Because the PSS is not a diagnostic tool, specific score ranges do not indicate a clinical degree of stress.
Students were given a sufficient time window to complete the survey instrument, and then responses were collected electronically from SurveyMonkey. Data pertaining to perceived stress, stressful events, and stress-relieving activities were reported using mean, median, and mode. Categorical variables were reported as percentages and compared using Fisher exact test. Continuous data were calculated and compared to published data using a one-sample t test.11 A two-tailed p < 0.05 was considered significant. The statistical analyses were calculated using SPSS, version 17 (SPSS, Inc, Chicago, IL).
RESULTS
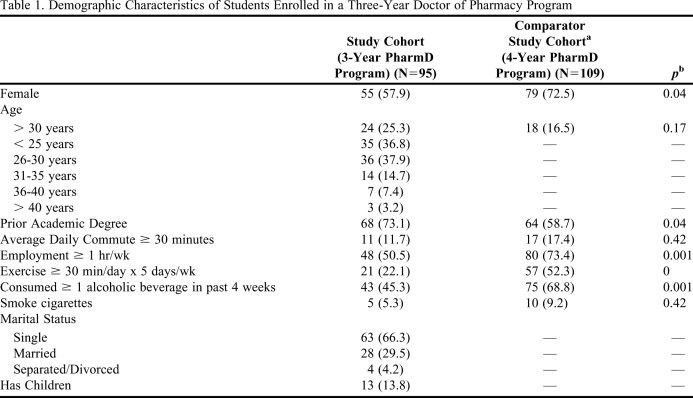
Of the 135 students asked to participate in the study, 95 successfully completed the electronic survey instrument, yielding a response rate of 70.4%. The demographic information for the study participants and the published comparative study is reported in Table 1. Significant differences were found between the 2 groups in the following areas: percentage of female students, prior academic degree, employment status, and exercise and alcohol habits.
Table 1.
Demographic Characteristics of Students Enrolled in a Three-Year Doctor of Pharmacy Program
Marshall LL, Allison A, Nykamp D, Lanke S. Perceived stress and quality of life among doctor of pharmacy students. Am J Pharm Educ. 2008;72(6):137-146.
Fisher exact test was used to determine significance.
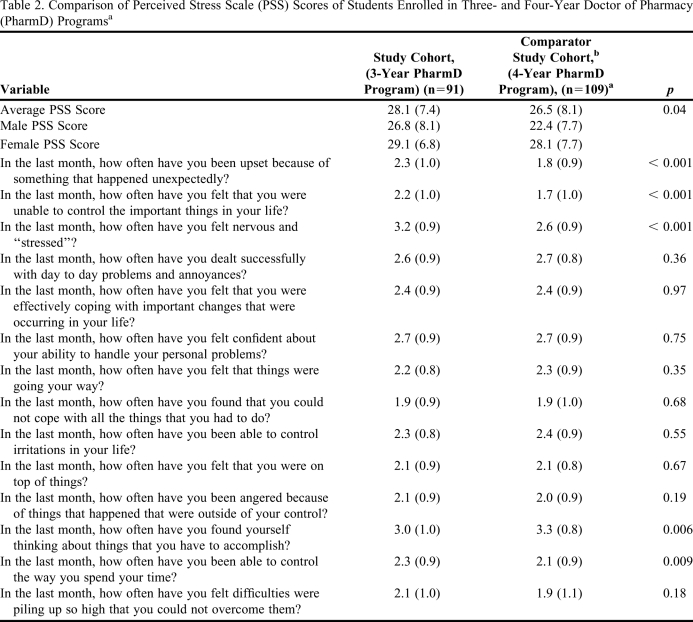
There were no significant differences between demographic characteristics and PSS scores within the 3-year PharmD cohort. The average PSS score in the 3-year PharmD cohort was 28.1, which was 1.6 points higher than that of students in the 4-year PharmD cohort in the comparative study, indicating a greater overall level of stress among students in the 3-year program. Of the 14 questions in the PSS, there were significant differences between the 2 groups in students’ responses to 5 questions (Table 2).
Table 2.
Comparison of Perceived Stress Scale (PSS) Scores of Students Enrolled in Three- and Four-Year Doctor of Pharmacy (PharmD) Programsa
Cohen S. Laboratory for the Study of Stress, Immunity, and Disease. http://www.psy.cmu.edu:16080/~scohen/. Accessed April 1, 2011. PSS score ranges from 0 (lowest stress score) to 56 (highest stress score).
Marshall LL, Allison A, Nykamp D, Lanke S. Perceived stress and quality of life among doctor of pharmacy students. Am J Pharm Educ. 2008;72(6):137-146. Data have been reformatted to match the experimental data (ie, scale of 1-5 converted to 0-4).
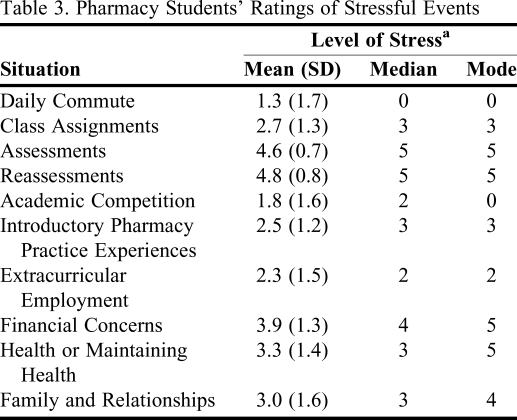
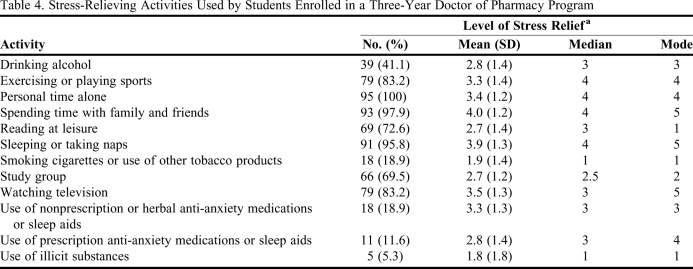
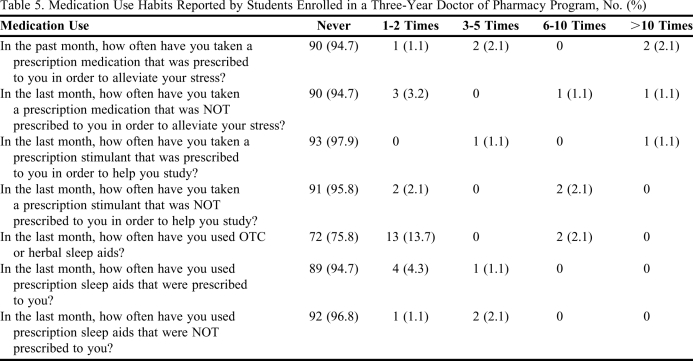
Students in the 3-year PharmD cohort rated 10 different stress-causing events on a scale of 0 to 5 (0 = no stress while 5 = high level of stress). The results are listed in Table 3. Study participants also rated how well certain activities alleviated stress, again using a scale of 0 to 5 (0 = no stress relief while 5 = significant stress relief) (Table 4). Use of prescribed and nonprescribed medications to aid in stress, studying, and sleep, are reported in Table 5.
Table 3.
Pharmacy Students’ Ratings of Stressful Events
Range 0-5; 0 = not stressful, 5 = highly stressful
Table 4.
Stress-Relieving Activities Used by Students Enrolled in a Three-Year Doctor of Pharmacy Program
Range 0-5; 0 = no stress relief, 5 = most stress relief
Table 5.
Medication Use Habits Reported by Students Enrolled in a Three-Year Doctor of Pharmacy Program, No. (%)
DISCUSSION
To our knowledge, this was the first study to compare student stress in a 3-year and 4-year PharmD program. In addition, this research provides additional insight into the most stressful components of the PharmD program for students, and students’ common stress-relieving activities, including the use of prescription medications.
The study found a higher average perceived-stress score among students enrolled in the 3-year program compared to the average score reported in a published study of students in a 4-year program.11 One possible reason for students’ higher stress level was the condensed format of the 3-year PharmD curriculum. Another reason may be the mastery learning model used in our program. Because students were required to achieve 90% on each assessment in order to progress academically, taking each assessment may have been seen as a critically important event. However, in a traditional grading system where 70% is considered passing and grades are averaged over a semester or quarter, a student may be able to do poorly in certain components of the curriculum but do well in others to improve the overall grade. Additionally, pass rates for the curriculum blocks that the students completed during and around the time the questionnaire was administered were similar to pass rates for those blocks in previous years. Thus, the higher level of stress students experienced could not be attributed to the difficulty of the block they were completing at the time of testing. While the 3-year PharmD cohort reported higher stress levels than the comparison group in response to 4 of the questions, students in the comparison group were more likely to be stressed about tasks they had to accomplish.11 A potential explanation for this difference may be that the students in the 4-year PharmD program may have had multiple courses, projects, or assignments occurring simultaneously. While the block curriculum in the 3-year program at USN does not completely eliminate this, the number of concurrent tasks that students have at any given time may be less than that for students in the 4-year PharmD program. Because of this, students in the 3-year program may feel less burdened. One of the significantly different responses pertained to students feeling upset over unexpected events. The difference in responses between the 2 groups may have been influenced by the death of a classmate in the 3-year PharmD program. When PSS scores were stratified by demographic characteristics, female students in the 4-year PharmD cohort identified higher levels of stress than male students,11 but there was no statistical difference in stress between the 2 genders in the 3-year program.
Another interesting result from the study was the use of prescription medications among the study cohort. The prevalence of nonmedical prescription drug use among college students ranges from 4.4% to 17%, and the prevalence of nonmedical use of prescription stimulants is 6.9% to 18.3%.18-21 These rates pertain to lifetime usage rather than 30-day usage, but the results in this study were similar. While direct research on drug use among health professions students is lacking, Tuttle and colleagues reported that 10.1% of a cohort of medical students admitted using prescription stimulants for nonmedical purposes at some point in their lifetime.22
This study has limitations. Each of the student groups was comprised of only 1 class of pharmacy students; thus, external validity cannot be assumed and this may limit the interpretation of the data and prevent extrapolation to all pharmacy students. Surveying only 1 class also increases susceptibility to confounding events that may have occurred during the study period. In addition, we assumed that students in their second year of the 3-year program were at a similar academic point as students in the 4-year program. Because there were several differences between the 2 programs (eg, length of program, type of block curricular design, and use of a mastery learning educational model), the differences seen in students’ stress levels cannot be attributed to any particular component of either program. Furthermore, students’ stress levels may vary throughout the academic year. Differences in demographic characteristics also limit interpretation of the data. Finally, the study questions that dealt with alcohol and drug use may have made some students uncomfortable and affected individual responses, despite anonymity.
While the study has limitations, it does provide data for future research. Studies that may provide additional insight include 3-year vs. 4-year programs that use similar educational models and two 3-year programs that use different educational models.
CONCLUSION
Students in a 3-year PharmD program using a block curriculum and mastery learning model were more stressed than students in a traditional 4-year PharmD program. In addition, pharmacy students may be using prescription medications that were not prescribed to them to help them to study or sleep. The authors recommend that the American Association of Colleges of Pharmacy (AACP) work to develop a universal stress assessment tool to encourage measurement of student stress in all colleges and schools of pharmacy. This also would allow for direct comparisons and promote areas of intervention in a population of students who often are significantly stressed.
REFERENCES
- 1.Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5(3):243–251. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- 2.Lin YH, Chen CY, Hong WH, Lin YC. Perceived job stress and health complaints at a bank call center: comparison between inbound and outbound services. Ind Health. 2010;48(3):349–356. doi: 10.2486/indhealth.48.349. [DOI] [PubMed] [Google Scholar]
- 3.Lantz PM, House JS, Mero RP, Williams DR. Stress, life events, and socioeconomic disparities in health: results from the Americans’ Changing Lives study. J Health Soc Behav. 2005;46(3):274–288. doi: 10.1177/002214650504600305. [DOI] [PubMed] [Google Scholar]
- 4.Stewart SM, Lam TH, Betson CL, Wong CM, Wong AM. A prospective analysis of stress and academic performance in the first two years of medical school. Med Educ. 1999;33(4):243–250. doi: 10.1046/j.1365-2923.1999.00294.x. [DOI] [PubMed] [Google Scholar]
- 5.LeBlanc VR. The effects of acute stress on performance: implications for health professions education. Acad Med. 2009;84(10 Suppl):825–33. doi: 10.1097/ACM.0b013e3181b37b8f. [DOI] [PubMed] [Google Scholar]
- 6.Herrman G, Schuckit MA, Hineman S, Pugh W. The association of stress with drug use and academic performance among university students. J Am Coll Health Assoc. 1976;25(2):97–101. [PubMed] [Google Scholar]
- 7.Beck DL, Hackett MB, Srivastava R, McKim E, Rockwell B. Perceived level and sources of stress in university professional schools. J Nurs Educ. 1997;36(4):180–186. doi: 10.3928/0148-4834-19970401-08. [DOI] [PubMed] [Google Scholar]
- 8.Gupchup GV, Borrego ME, Konduri N. Impact of student life-stress on health related quality of life among Doctor of Pharmacy students. Coll Stud J. 2004;38:292–301. [Google Scholar]
- 9.Dutta AP, Pyles MA, Miederhoff PA. Stress in health professions students: myth or reality? A review of the existing literature. J Natl Black Nurses Assoc. 2005;16(1):63–68. [PubMed] [Google Scholar]
- 10.Canales PL, Kranz P. Perceived stress by students in a pharmacy curriculum. Education. 2008;129(1):139–146. [Google Scholar]
- 11.Marshall LL, Allison A, Nykamp D, Lanke S. Perceived stress and quality of life among doctor of pharmacy students. Am J Pharm Educ. 2008;72(6) doi: 10.5688/aj7206137. Article 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hirsch JD, Do AH, Hollenbach KA, Manoguerra AS, Adler DS. Students’ health-related quality of life across the preclinical pharmacy curriculum. Am J Pharm Educ. 2009;73(8) doi: 10.5688/aj7308147. Article 147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Accreditation Council for Pharmacy Education. Chicago, Illinois: Accreditation Council for Pharmacy Education; 2006. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org Accessed October 7, 2010. [Google Scholar]
- 14.Youssef FA, Goodrich N. Accelerated versus traditional nursing students: a comparison of stress, critical thinking ability and performance. Int J Nurs Stud. 1996;33(1):76–82. doi: 10.1016/0020-7489(95)00033-x. [DOI] [PubMed] [Google Scholar]
- 15.Mercer University. Lafayette, IN: School Datebooks, Inc.; 2010. Mercer University College of Pharmacy and Health Sciences Student Handbook 2010-2011. http://cophs.mercer.edu/pdfs/handbook.pdf. Accessed January 25, 2011. [Google Scholar]
- 16.Frick J, Bhakta R, Frick L, Kullgren J, Whittaker A. Correlation of pharmacy students’ perceived difficulty and level of interest in pharmacotherapeutic topics [abstract]. 111th AACP Annual Meeting: July 10-14, 2010, Seattle, WA. Am J Pharm Educ. 2010;74(5) Article 96. [Google Scholar]
- 17.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 18.Ford JA. Nonmedical prescription drug use among college students: a comparison between athletes and nonathletes. J Am Coll Health. 2008;57(2):211–219. doi: 10.3200/JACH.57.2.211-220. [DOI] [PubMed] [Google Scholar]
- 19.McCabe SE. Screening for drug abuse among medical and nonmedical users of prescription drugs in a probability sample of college students. Arch Pediatr Adolesc Med. 2008;162(3):225–231. doi: 10.1001/archpediatrics.2007.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96–106. doi: 10.1111/j.1360-0443.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- 21.Judson R, Langdon SW. Illicit use of prescription stimulants among college students: prescription status, motives, theory of planned behaviour, knowledge and self-diagnostic tendencies. Pyschol Health Med. 2009;14(1):97–104. doi: 10.1080/13548500802126723. [DOI] [PubMed] [Google Scholar]
- 22.Tuttle JP, Scheurich NE, Ranseen J. Prevalence of ADHD diagnosis and nonmedical prescription stimulant use in medical students. Acad Psychiatry. 2010;34(3):220–223. doi: 10.1176/appi.ap.34.3.220. [DOI] [PubMed] [Google Scholar]