Abstract
Objective
To implement a simulated interprofessional rounding experience using human patient simulators as a required activity for third-year pharmacy students in a clinical assessment course.
Design
Interprofessional student teams consisting of pharmacy, medical, and physician assistant students participated in a simulated interprofessional rounding experience in which they provided comprehensive medical care for a simulated patient in an inpatient setting.
Assessment
Students completed a survey instrument to assess interprofessional attitudes and satisfaction before and after participation in the simulated interprofessional rounding experience. Overall student attitudes regarding interprofessional teamwork and communication significantly improved; student satisfaction with the experience was high and students’ self-perceived clinical confidence improved after participation. The mean team clinical performance scores were 65% and 75% for each simulated interprofessional rounding experience.
Conclusion
Incorporating a simulated interprofessional rounding experience into a required clinical assessment course improved student attitudes regarding interprofessional teamwork and was associated with high student satisfaction.
Keywords: simulation, interprofessional, assessment, cardiovascular, patient assessment
INTRODUCTION
Interprofessional education and practice is viewed as an essential component of health professions education. Interprofessional education occurs when 2 or more professions learn with, from, and about each other to improve collaboration and the quality of care.1,2 The American Association of Colleges of Pharmacy and the Association of American Medical Colleges include interprofessional health education and practice as strategic areas for member engagement.3-5 Common competencies for interprofessional education include team organization/function; assessment and enhancement of team performance; intrateam communication; leadership; conflict resolution and consensus building; and setting common patient care goals.6 One approach to achieve these interprofessional competencies in a clinical team is through simulation exercises.
High-fidelity simulators are a unique learning tool increasingly used in health professions education. A human patient simulator is a mannequin interfaced with a computer program that can produce physiologic responses to student actions including changes in the mannequin's simulated heart rhythm, respiratory rate, pulse, and heart sounds. Human patient simulators are used to simulate direct patient care and allow learning in a low-stakes environment.7 Human patient simulators have been used successfully to train teams of licensed healthcare practitioners to deliver safer and more effective care; however, little is known about the use of simulation to train health professions’ students in interprofessional healthcare teams.8,9
The Accreditation Council for Pharmacy Education (ACPE) encourages the use of simulation as an active-learning technique according to Standard 11. Standard 12 encourages curricular development surrounding the provision of patient-centered care within an interprofessional healthcare team.10 In addition, the Center for the Advancement of Pharmaceutical Education (CAPE) outcomes also highlight practicing pharmaceutical care in collaboration with an interprofessional team.11 The development of an interprofessional inpatient rounding experience using human patient simulators fulfills these curricular standards and outcomes using an active-learning strategy.
Limited information regarding use of human patient simulators in pharmacy education has been published in the literature.12-15 These findings describe the use of simulation related to blood pressure, cardiovascular pharmacotherapy, and advanced cardiovascular life support (ACLS) in pharmacotherapy and clinical assessment courses. A single publication described using human patient simulators to teach interprofessional team skills to pharmacy students.16 However, this simulation did not use other health professions’ students; instead, other people played the role of nurses and physicians. All of these simulation exercises were associated with positive outcomes related to attitudes about simulation or increased knowledge after the simulation.
At the Medical University of South Carolina (MUSC), a simulated interprofessional rounding experience was developed. This program was integrated into the curriculum for all third-year pharmacy students as well as selected medical and physician assistant students. The objectives of the study were to: (1) establish the simulated interprofessional rounding experience pilot program, (2) determine the effect of the experience on student attitudes toward interprofessional collaboration in the clinical setting, (3) determine student self-perceived confidence in clinical skills related to the simulation, (4) determine student satisfaction with a simulated interprofessional rounding experience, and (5) determine mean scores on clinical performance of the interprofessional team during simulation.
DESIGN
Incorporation of this interprofessional simulation into the required curriculum for pharmacy students provided for the integration of pharmacotherapy and teamwork skills. This simulation fulfilled ACPE accreditation standards and CAPE outcomes while incorporating active learning and IPE with an emphasis on andragogy learning. Specific learning objectives of the simulated interprofessional rounding experience included the following: (1) determine roles and responsibilities of an interprofessional healthcare team member in a simulated clinical environment, (2) demonstrate effective teamwork skills in an interprofessional clinical environment, and (3) deliver appropriate care to an unstable patient within an interprofessional healthcare team.
The South Carolina College of Pharmacy (SCCP) offers a traditional 4-year doctor of pharmacy (PharmD) program delivered at 2 campuses (at the University of South Carolina campus in Columbia and the MUSC campus in Charleston). The same curriculum is taught at both campuses using distance education. This paper only addresses the simulated interprofessional rounding experience project at the MUSC campus. Currently, MUSC is engaged in a 10-year interprofessional education initiative, Creating Collaborative Care. This is a campus-wide initiative to promote an institutional culture, learning environment, and infrastructure that enhances MUSC graduates’ abilities to participate as effective team members in interprofessional collaborative healthcare delivery or research. MUSC has an 11,000-square-foot simulation center with 14 rooms for multipurpose use. This simulation center is an interprofessional training facility available to all colleges located on the campus.
Clinical Assessment is a required application-based course offered in the spring semester of the third year of the PharmD curriculum. At this point, students have completed 4 pharmacotherapy courses, and Clinical Assessment serves to integrate pharmacotherapy knowledge with patient communication and physical assessment skills. The Clinical Assessment course includes a weekly laboratory section that covers many topics and uses a variety of active-learning teaching methods.The simulated interprofessional rounding experience was held during one of the laboratory sections in the final 2 weeks of the spring semester in April 2009. Earlier in the semester, students were given an orientation of the simulation center and used the simulation mannequins to perform a blood pressure laboratory assignment. In addition, the clinical topics covered in a simulated interprofessional rounding experience had been taught in previous pharmacotherapy courses. The simulated interprofessional rounding experience required several planning meetings of interprofessional faculty and staff members at the simulation center prior to the exercise. The development of simulations, pilot testing, and training faculty facilitators required 15 hours of faculty time.
All third-year pharmacy students enrolled in the Clinical Assessment course were required to participate in the simulated interprofessional rounding experience (n=77). Third- or fourth-year medical students and first-year physician assistant students were required to participate depending on what experiential rotation they were completing (n=37). Although the students were informed that they would care for a patient in the hospital within an interprofessional team, they were not informed of the clinical content of a simulated interprofessional rounding experience. The students were instructed to show up prepared for rounds (bring white coats, stethoscopes) and were permitted to bring any pocket resources that they would ordinarily use on rounds. The students were divided into 22 groups consisting of either 3 pharmacy students, 1 medical student, and 1 physician assistant student, or 3 pharmacy students and 2 medical students. These interprofessional student teams were assigned 1 time slot (a total of 75 minutes) during the 3 laboratory days when the experience was offered. Each day, 4 patient rooms were used and simulation scenarios were conducted simultaneously in all rooms, 3 times per day. All students who participated in the experience signed a confidentiality agreement for the MUSC Simulation Center, stating they would not share the content of the simulation scenarios. This was to discourage students who participated in the experience first from providing information from the simulation scenario to those participating later in the week. Students were not graded on their performance but did receive standard laboratory participation points for completing the simulated interprofessional rounding experience.
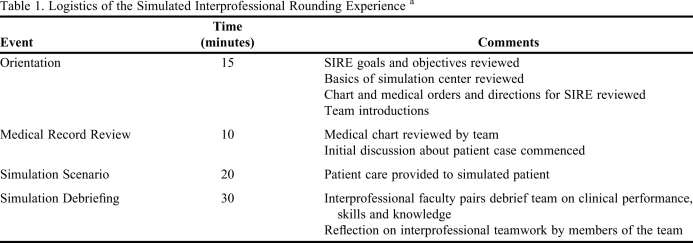
The interprofessional teams participated in a 15-minute orientation in which a course instructor explained the objectives of the experience and the function of the mannequins, and provided instructions on how to write orders and provide care for their simulated patient. The students were encouraged to meet their team members and discuss interprofessional team roles. After the orientation, the interprofessional teams were directed to the patient room where each was provided with the patient's medical record and given 10 minutes to review the chart. After 10 minutes, the simulation commenced and the interprofessional team cared for the simulated patient just as they would for an actual patient during hospital rounds. They conducted a patient interview and physical examination, ordered laboratory and diagnostic tests, observed vital signs on the patient monitor, and ordered medications. The interprofessional team had 20 minutes to stabilize and treat the patient; then faculty members debriefed the student team about the simulation. The logistics of the simulated interprofessional rounding experience are provided in Table 1.
Table 1.
Logistics of the Simulated Interprofessional Rounding Experience a
Abbreviations: SIRE=Simulated Interprofessional Rounding Experience
Total encounter for students was 75 minutes
Each interprofessional team participated in 1 of 2 possible scenarios. These scenarios were selected randomly for each student group and 2 scenarios were piloted with the intent of expanding the program the following year to use both cases. The scenarios consisted of either a patient with gastrointestinal bleeding related to warfarin or a patient with digoxin toxicity and related cardiac arrhythmias. Each simulation scenario also had a medication error and medication interaction imbedded in the case. The simulations were developed by an interprofessional group of faculty members, pilot tested by an interprofessional student group, and modified based on feedback and pilot student performance. The simulation scenarios were uploaded into the human simulator controlled by Sim-Man software (Laerdal Corporation, Stavanger, Norway). Sim-Man was connected to a cardiac monitor and displayed real-time vital signs, physical findings, results of diagnostic tests (electrocardiogram, echocardiogram, etc), palpable pulse, and heart and lung sounds. The clinical steps (including medications) ordered by the interprofessional teams were programmed with an appropriate physiological response related to the simulated scenario. Interprofessional faculty pairs (PharmD and MD or PharmD and PA) were in a simulation booth where 1 person controlled the simulation and computerized clinical checklist, while the other role-played as the patient voice through the simulator and responded to the student interview questions using scripted responses. After the simulated interprofessional rounding experience ended, the pair of interprofessional faculty members debriefed the student team using the Sim-Man debriefing tool (that included the clinical checklist and scores) and a faculty facilitator guide that contained major teaching points associated with each scenario. In addition to the clinical pearls reviewed, the student teams also reflected on interprofessional teamwork in the clinical setting.
EVALUATION AND ASSESSMENT
The simulated interprofessional rounding experience was assessed by several methods. The objectives of determining the effect on student attitudes toward interprofessional collaboration in the clinical setting and confidence were assessed using a survey instrument that was administered to all students before the experience and after the experience. Additional items included on the post-experience survey instrument that were not addressed on the pre-experience survey instrument assessed student attitudes toward interprofessional collaboration, confidence, and satisfaction. The overall interprofessional team clinical performance was assessed using the clinical outcomes checklist and percent scores from the simulated interprofessional rounding experience. Clinical performance scores were calculated and based on a 100% scale; competent clinical performance was determined by a score of 70% or greater by the interprofessional team. Seventy percent was chosen as the minimum clinical competency score based on pharmacy certification scores (eg, American Pharmacist Association Immunization Program) and the university's grading system. These clinical performance scores were used only for feedback and learning purposes for the students. The actual grades were not recorded and remediation was not required for teams with less than competent scores. In addition to comparing the overall pre-experience and post-experience survey results that included all students, the survey responses also were compared within each profession represented. Theme identification from student qualitative comments after completing a simulated interprofessional rounding experience also was assessed. The study objectives were linked to the specific student learning objectives developed for the experience.
Data were collected using anonymous, voluntary student survey instruments and clinical performance scores for each of the interprofessional teams. The surveys were administered using SurveyMonkey software (SurveyMonkey, Inc., Palo Alto, CA). For purposes of this pilot project, lengthy validated scales assessing interprofessional attitudes were not used. The survey instrument included 6 questions on the pre-experience survey and 14 questions on the post-experience survey using a 5-point Likert scale (responses ranged from 1 = strongly disagree to 5 = strongly agree). The survey items were developed to track and assess a broad array of learning activities, which are aspects of the student learning outcomes outlined in the MUSC campus-wide interprofessional education initiative. These outcomes address students’ appreciation for interprofessional collaboration, knowledge about professions other than their own, and teamwork skills. This survey instrument was developed and promoted by the interprofessional institute and is widely used on the MUSC campus. In addition, the survey assessed student self-perceived clinical confidence. The interprofessional team clinical performance scores were assessed during the rounding experience based on the students’ patient interview skills, assessment skills, and quality of the orders written during the simulation.
Statistical analyses were performed using SAS, v9.2 (Cary, NC). Pre- and post-experience survey results were analyzed using Wilcoxon rank sum tests stratified by students’ health profession. Descriptive statistics were used to characterize demographic data, clinical outcome checklists, post-experience survey responses not included on the pre-experience survey instrument, and qualitative student comments. Comparisons between demographic data were analyzed using student t test and chi-square test. This study was approved as exempt by the university's institutional review board.
Overall, 114 students (n = 77 pharmacy students and n = 37 medical/physician assistant students) participated in the simulated experience. Ninety-nine students (72 pharmacy students and 27 medical/physician assistant students) completed the pre-experience survey instrument (87% response rate) and 104 students (67 pharmacy students and 37 medical/physician assistant students) completed the post-experience survey instrument (91% response rate). There were no significant differences between the groups with respect to age (pharmacy group mean ± SD = 25.4 ± 2.8; medical/physician assistant group = 25.5 ± 2.3, p = 0.90) or gender (pharmacy group: 70.0% female; medical/physician assistant group: 55.6% female, p = 0.18).
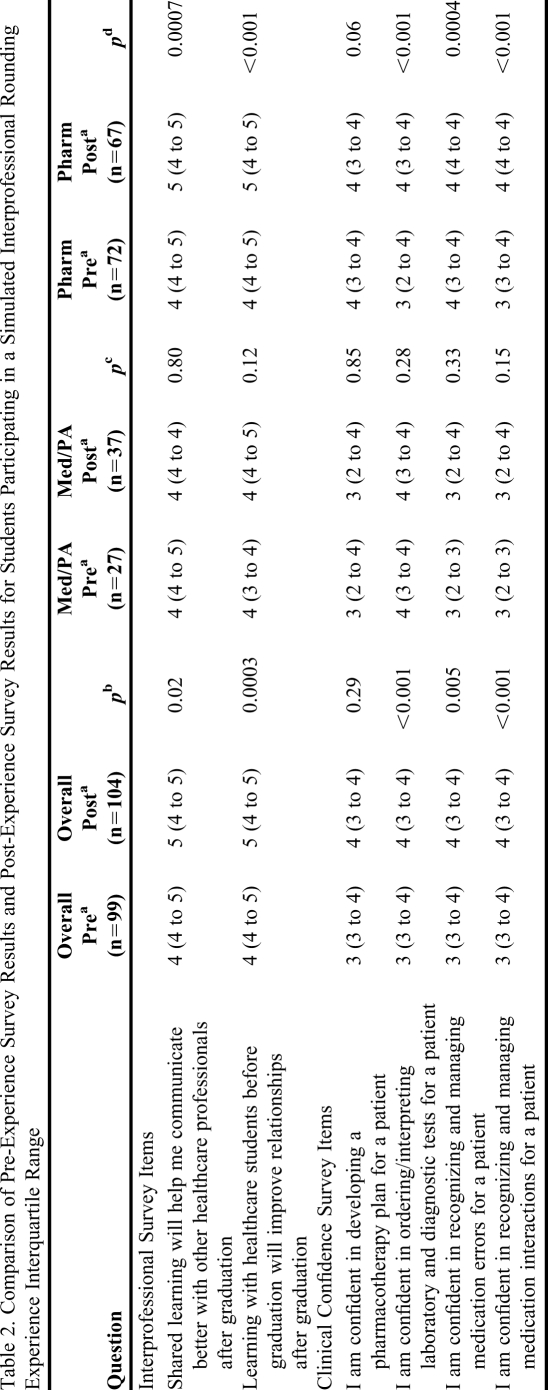
Overall, when comparing pre-experience survey results to post-experience survey results for all students, there were significant improvements in all of the interprofessional attitudes and in the majority of clinical confidence questions. The pre-experience and post-experience comparisons also were assessed within the specific professions (Table 2).
Table 2.
Comparison of Pre-Experience Survey Results and Post-Experience Survey Results for Students Participating in a Simulated Interprofessional Rounding Experience Interquartile Range
Abbreviations: Med = medical, PA = physician assistant, Pharm = pharmacy
Median score (and interquartile range) using 5-point likert scale: 1-strongly disagree to 5-strongly agree
Wilcoxon rank sum tests to compare overall pre-simulation and post-simulation scores
Wilcoxon rank sum tests to compare med/PA pre-simulation and post-simulation scores
Wilcoxon rank sum tests to compare pharm pre-simulation and post-simulation scores
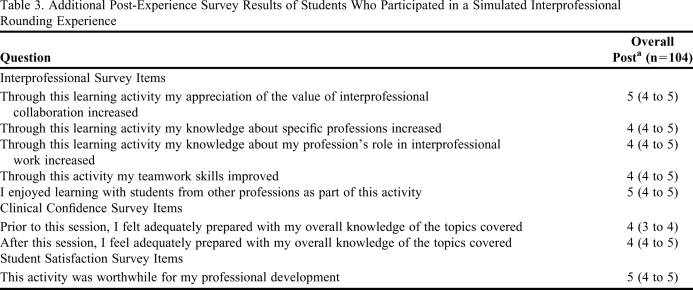
Additional survey results were assessed after participation in a simulated interprofessional rounding experience. The students had better appreciation of the value of interprofessional collaboration, increased knowledge about other professions, increased knowledge about their professions’ role, and self-perceived improvement in teamwork skills. The majority of students who participated in the simulated interprofessional rounding experience enjoyed learning with other professions and were satisfied with the simulation as a learning experience (Table 3).
Table 3.
Additional Post-Experience Survey Results of Students Who Participated in a Simulated Interprofessional Rounding Experience
Median score (and interquartile range) using 5-point likert scale: 1-strongly disagree to 5-strongly agree
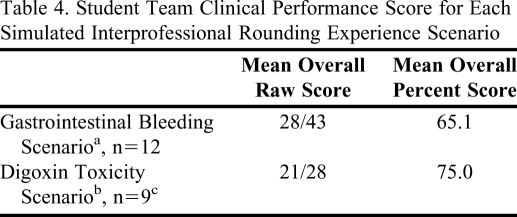
The clinical performance of the interprofessional teams completing the simulation was assessed using a clinical performance checklist. For each of the scenarios, a raw score and a percent score based on a 100% scale were used. A percent score of 70% or greater was deemed a competent clinical performance by the interprofessional team. The mean clinical performance scores for the interprofessional teams were 65% for the gastrointestinal bleed scenario and 75% for the digoxin toxicity scenario (Table 4).
Table 4.
Student Team Clinical Performance Score for Each Simulated Interprofessional Rounding Experience Scenario
Score out of 43 points
Score out of 28 points
One team missing data
Other assessment data included qualitative comments from the students, which revealed a positive response to the pilot simulation program. The majority of students felt the simulated interprofessional rounding experience was beneficial to their overall learning. The main themes identified from the qualitative comments were that the students: (1) enjoyed working with students from other healthcare professions, (2) appreciated “hands-on” interactive learning, (3) enjoyed being put into an acute scenario with “lots of pressure,” (4) would like to participate in more simulated interprofessional rounding experiences.
DISCUSSION
Our pilot simulated interprofessional rounding experience using human patient simulators was viewed as a positive learning experience by the majority of students involved. There was a significant improvement in interprofessional attitudes after students completed the experience. This finding was primarily seen within the pharmacy student group, while the medical/physician assistant student group demonstrated minimal improvement. The mean interprofessional team clinical performance scores were slightly below average or average depending on the specific simulation scenario completed. However, there was a significant improvement in clinical confidence after students completed the simulation. Overall, students felt that the simulated interprofessional rounding experience was a worthwhile learning activity, and they enjoyed working in interprofessional teams and the interactive simulation scenario.
These findings are similar to those of other studies regarding the use of simulation in pharmacy education. Seybert and colleagues found that pharmacy students’ satisfaction, knowledge, and confidence increased after participation in a human patient simulation exercise in a pharmacotherapy course.12,14 Also, use of human patient simulators to teach pharmacy students ACLS demonstrated improved understanding of pharmacist responsibilities during an ACLS event; however, students performed poorly on ACLS knowledge-based questions after the simulation.15 Fernandez and colleagues reported high student satisfaction regarding a learning activity in which human patient simulators were used to teach interprofessional team skills to pharmacy students; however, actors were used to play the roles of nurses and physicians.16 The study did not include nonpharmacy health professions students in the interprofessional interaction, nor did it assess student responses to interprofessional teamwork or interaction.
Our study findings add to the literature regarding interprofessional teamwork and active-learning methods using human patient simulators. A large number of students were included in the simulated interprofessional rounding experience and response rates to the surveys were high. The simulation used actual interprofessional student teams to provide patient care in a simulated clinical environment, compared to previous studies that did not use health professions’ students. In addition to serving as a tool to apply clinical skills and pharmacotherapy knowledge, the simulated rounding experience allowed students to learn about interprofessional roles and practice providing care in a team environment. Assessment of the simulation went beyond collection of student satisfaction data regarding the learning technique and included student satisfaction, student attitudes related to interprofessional roles, team interactions, and clinical confidence.
Colleges and schools of pharmacy could implement a program similar to this simulated interprofessional rounding experience and fulfill many ACPE and CAPE outcomes related to active-learning and IPE. Colleges and schools that are associated with an academic medical center or based on a health-sciences campus with a college/school of medicine and/or nursing may have access to a simulation center. Collaborations and partnerships can be formed to provide simulation experiences to all health professions students, as the recommendation for interprofessional educational experiences becomes more common in all health professions’ educational curriculum.
While there are significant benefits to providing interprofessional simulations such as this, consideration of cost, scheduling, and faculty time is important. Many simulation centers may have a cost associated with use of their facilities. However, partnerships that include health professions who have ownership in the simulation center may provide a mechanism to reduce or waive these fees. Scheduling of interprofessional simulations may be a challenge as different health professions’ colleges/schools cover interprofessional course content at different points in their curriculum; advanced planning and flexibility will help to resolve this issue. Lastly, faculty time is a major barrier to consider when implementing a program such as a simulated interprofessional rounding experience. Significant time is devoted to developing clinical scenarios that appeal to a variety of health professions and programming clinical checklists into the simulators. Recruiting and training additional faculty pairs to run the simulation and debrief the small groups is also challenging. Many faculty members are needed to provide high-quality, organized simulation experiences for the students.
While our findings add to the literature, they are not without limitations. Data collected was attitudinal and self-reported by students. Further research regarding team performance and associated clinical outcomes, including quantitative measures, should be collected. There were not equal groups of each of the health professions’ students represented in the sample and the imbalance may have influenced the results. Specifically, when analyzing the pre- and post-experience results within specific professions, significant improvements in interprofessional attitudes and clinical confidence were reported by pharmacy students. In contrast the medical/physician assistant students did not report significant improvements. This could be due to several factors. Most likely, the pharmacy students’ advantage in numbers (3 pharmacy students to 2 nonpharmacy students) influenced their learning experience. Working alongside classmates on the same educational level may provide better peer support and collaboration among classmates. Less likely explanations include that the scenario in some way favored pharmacy students or that pharmacy students were more willing to learn in interprofessional groups. Future research may benefit from selecting more balanced interprofessional teams. Additionally, medical and physician assistant students were not separated for data collection purposes due to different numbers participating in the interprofessional teams. Finally, because the simulated interprofessional rounding experience was part of a required course, there was no control group used in the study design.
SUMMARY
Incorporating a simulated interprofessional rounding experience into a required clinical assessment course was successful at fulfilling ACPE and CAPE curricular outcomes. Student response to the simulation was positive. Overall there was a significant improvement in interprofessional attitudes and confidence in clinical skills after completing the simulation. Student response to the interprofessional simulation was encouraging and the program will continue at SCCP. Implementation of similar interprofessional simulations should be considered by other colleges and schools of pharmacy.
ACKNOWLEDGEMENTS
This project was supported by the South Carolina Clinical & Translational Research Institute, Medical University of South Carolina's CTSA, NIH/NCRR Grant Number UL1RR029882. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or NCRR.
REFERENCES
- 1.Center for Advancement of Interprofessional Education (CAIPE) http://www.caipe.org.uk/about-us/defining-ipe/. Accessed April 12, 2011.
- 2. The Institute of Medicine: Bridge to Quality Report endorses the movement toward an interprofessional approach to patient care [Institute of Medicine, Crossing the Quality Chasm: A New Health System for the 21st Century, National Academy Press, Washington, DC; 2001.
- 3.American Association of Colleges of Pharmacy. Annual report of the Task Force on Interprofessional Education 2006-2007. http://www.aacp.org/governance/councilfaculties/ Accessed April 12, 2011. Documents/COF_InterprofEd2007.pdf. Accessed November 22, 2010.
- 4.Kirch DG. A Word from the President: “Interprofessional Collaboration: We Are Willing- Can We Find A Way?”. Available at http://www.aamc.org/newsroom/reporter/may08/88258/may08_word.html. Accessed April 12, 2011.
- 5.Association of American Medical Colleges. Interprofessional Education: Current Rationale, Resources, and Relevance. Available at https://www.aamc.org/download/183128/data/inter-professional_education_current_rationale_resources.pdf Accessed April 12, 2011.
- 6.Buring S, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. 2009;73(3):Article 59. doi: 10.5688/aj730459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40(3):254–262. doi: 10.1111/j.1365-2929.2006.02394.x. [DOI] [PubMed] [Google Scholar]
- 8.Kuduvalli PM, Jervis A, Tighe SQM, et al. Unanticipated difficult airway management in anesthetized patients: a prospective study of the effect of mannequin training on management strategies and skill retention. Anesthesia. 2008;63(4):364–369. doi: 10.1111/j.1365-2044.2007.05353.x. [DOI] [PubMed] [Google Scholar]
- 9.Wayne DB, Siddall VJ, Butler J, et al. A longitudinal study of internal medicine residents' retention of advanced cardiac life support skills. Acad Med. 2006;81(10):S9–S12. doi: 10.1097/00001888-200610001-00004. [DOI] [PubMed] [Google Scholar]
- 10.Accreditation Council for Pharmacy Education. Accreditation standards. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed April 12, 2011.
- 11. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed April 12, 2011.
- 12.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3):Article 48. doi: 10.5688/aj700348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3):Article 48. doi: 10.5688/aj710348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2):Article 37. doi: 10.5688/aj720237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mieure KD, Vincent WR, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2):Article 22. doi: 10.5688/aj740222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernandez R, Parker D, Kalus J, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary teams skills to pharmacy students. Am J Pharm Educ. 2007;71(3):Article 51. doi: 10.5688/aj710351. [DOI] [PMC free article] [PubMed] [Google Scholar]