Abstract
Objective
To evaluate the effectiveness of a community intervention in promoting adoption of behaviors to reduce the take-home pathway of pesticide exposure in farmworker households.
Methods
Using two cross-sectional samples of farmworker households in 11 intervention and 12 comparison communities in Washington State, we examined whether differences over time in reported pesticide safety practices varied by community intervention status.
Results
Pesticide safety practices increased in both intervention and comparison communities over time. Changes were significantly greater in intervention communities for removing work shoes before entering the home (p=0.003) and marginally significantly greater for changing out of work clothes within one hour of arriving home (p=0.05).
Conclusions
The intervention was associated with modest effects in certain behaviors among farmworkers. Further research is needed to identify successful strategies for reducing the take-home pathway of pesticide exposure.
Introduction
In the last decade, research and prevention efforts related to pesticide exposure and farmworkers have increased their focus on the take-home pathway (1-10). A number of studies suggest that in addition to exposure routes involving diet, residential pesticide use, and drift, household members of farmworkers may be exposed to pesticide residue brought into the home on farmworkers’ clothing, boots, skin, and from their work vehicles. For example, studies have shown that the levels of pesticide metabolites in children of farmworkers are significantly higher than in children of non-farmworkers (8) and are correlated with pesticide concentrations in house dust samples (10) as well as with the metabolite levels of adult farmworkers in the same household (2, 10). Direct correlations have also been observed between levels of pesticides in house dust and the number of farmworkers residing in a household (5).
The increased emphasis on the take-home pathway has been motivated, at least in part, by concerns regarding the health and development of children of farmworkers. While the effects of chronic exposure to organophosphate pesticides in young children are not well understood, animal and epidemiologic studies have identified childhood cancer, neurobehavioral deficits, and respiratory problems as possible risks of exposure to pesticides during early life (11-14). Moreover, young children are particularly vulnerable to indoor pesticide exposure because of their close proximity to the floor (where pesticide residues may accumulate) and their hand-to-mouth behaviors. A study of farmworker children in North Carolina observed strong associations between finding detectable levels of pesticides in house floor dust samples and on children’s hands and toys (6).
Specific precautions are believed to reduce the take-home pathway by minimizing the introduction of pesticides into the home environment and preventing contact between household members and contaminated items. These behaviors include washing hands immediately after work, storing and washing work clothes separately from household laundry and after one use, showering and changing out of work clothes immediately after work, and removing work shoes before entering the home (15). Laundering contaminated work clothes in hot water after one use and hand washing have been shown to be effective in reducing pesticide exposure (16, 17). Although the effectiveness of other precautions has not been evaluated thoroughly, one study suggests that waiting more than two hours before changing out of work clothes is associated with higher concentrations of pesticide residue in house dust (18). Another study, however, found no association between specific home protective practices and levels of pesticide metabolites in children of farmworkers (8).
Pesticide exposure in farmworkers and their families is an issue that lends itself well to community-based participatory research (CBPR). CBPR refers to a partnership between researchers, community members, community-based organizations, and other stakeholders that involves all members equitably throughout the research process (19). Conducting research with farmworker populations is often met with a number of challenges, such as high mobility of farmworkers due to transient work, low levels of education, limited English proficiency, and documentation issues. In some communities, concerns about pesticides can result in contentious relationships between groups. By involving farmworkers, farmworker advocates, and/or other stakeholders in the research process, CBPR approaches are uniquely positioned to address issues of concern to the community in ways that are culturally appropriate and have community support.
We report on the behavioral outcomes of a five-year study that used a community-based participatory research approach to reduce the take-home pathway of pesticide exposure in farmworker households in Eastern Washington. In 1998 the Center for Child Environmental Health Risks Research at the University of Washington received funding to conduct community-based participatory research in Eastern Washington on pesticide exposure and children’s health. The community-based research involved a collaboration with researchers at the Fred Hutchinson Cancer Research Center. The specific aims of the five-year project, known as ¡Para Niños Saludables! (For Healthy Kids!), were to: 1) develop a culturally appropriate intervention to break the take-home pathway of pesticides; 2) conduct a randomized, controlled community trial to evaluate the effectiveness of the intervention in reducing urinary organophosphate pesticide metabolites in children ages two to six years in farmworker households; and 3) assess the secondary effects of the intervention, including changes in pesticide concentrations in dust samples from farmworkers’ homes and vehicles, changes in urinary organophosphate pesticide metabolites in adult farmworkers, and changes in farmworkers’ self-reported pesticide safety practices.
Previous work evaluating changes in adult and child urinary pesticide metabolite concentrations and pesticide residue concentrations in house and vehicle dust in a subset of farmworker households included in this study observed no significant decreases over time associated with the intervention (20). However, given that the focus of the intervention was to raise awareness in the community of the risks of pesticide exposure and to promote behavior change in farmworker households that would ultimately reduce the take-home pathway, these negative findings do not necessarily indicate that the intervention was ineffective. Factors that vary over time, such as the amount and type of pesticides applied each year and the timing of application, may influence exposure levels in farmworkers and their families and may be difficult to control for in analyses. Behavioral outcomes provide an additional measure with which to evaluate the intervention, and in this paper we describe the effectiveness of the intervention in relation to the secondary outcome of farmworkers’ reported pesticide safety practices.
Materials and Methods
Setting
This study took place in the Lower Yakima Valley in Washington State, an area comprised of many small agricultural communities. The primary crops in this region include apples, pears, peaches, cherries, grapes, and hops (21). In 2002, the U.S. Census estimated the percentage of Hispanics to be over 50 percent (22), and many Hispanics in the area are involved in the harvesting, pruning, thinning, and other care of the crops grown in this region.
Community Organization
During an earlier community-based study on cancer prevention in the Valley (23), community members made requests for research on pesticide exposure. This led to a community analysis, in which interviews and small discussions were conducted with various stakeholder groups, to better understand the diversity of views around pesticides (24). In response to these interviews, a community planning committee agreed that health promotion efforts should focus on protecting children and not target the elimination of pesticides in order to achieve widespread community support and to be inclusive of all stakeholders. The community analysis facilitated the formation of a community advisory board (CAB) reflecting these diverse views. The CAB consisted of 18 members representing 16 different organizations and included farmworkers, growers and their associations, representatives from regulatory agencies, the health department, the Department of Agriculture, the Department of Labor and Industries, farmworkers’ clinics, the farmworker union, the local Spanish radio station, local legal services, and the local office of the Environmental Protection Agency.
In partnership with the CAB, Thompson and colleagues (4) designed and implemented the study described here to test an approach aimed at breaking the take-home pathway of pesticide exposure through community-based intervention activities. The CAB was responsible for hiring project staff, contributing to the study design, generating ideas for intervention activities, determining which activities to implement and at which times during the growing season, ensuring that intervention materials and survey procedures were culturally appropriate, and identifying approaches for sharing project information with the community. The CAB met monthly in the beginning, bi-monthly as the project was underway, and quarterly as intervention activities began to wind down.
Study Design
This study conducted a randomized community trial involving two cross-sectional samples of 24 communities in the Lower Yakima Valley. Group randomized trials are designed to reach large numbers of people, and as such, are used as tools to motivate health behavior change in group settings such as communities. This design allows for messages to be communicated among diverse groups of individuals with the potential to influence community norms and health behaviors (25). In addition, the randomization of communities helps to minimize differences between intervention and comparison sites that may be unmeasured or difficult to measure, thereby enhancing the likelihood that differences in outcomes are related to the intervention rather than other factors (26). A cross-sectional design was chosen over a cohort design to avoid problems associated with attrition, maturation of the cohort, and repeated testing and, to avoid expenses associated with tracking participants over time (27, 28).
The study design and survey procedures have been described in detail elsewhere (4). Briefly, farmworker households for the baseline sample were identified in the summer of 1999 through three strategies: 1) sampling potential respondents in 19 communities from households identified for a previous study on cancer prevention, which was a population-based study that oversampled Hispanics (23); 2) randomly sampling additional households in 16 of these communities which had large numbers of farmworkers; and 3) randomly sampling households in eight labor camps identified by local informants (see Figure 1). Of 1,264 households identified through these strategies at baseline, 651 were ineligible because they did not have farmworkers in the household (n=627) or could not be reached (n=24). Approximately 93 percent (571) of the remaining 613 households agreed to participate. Following the baseline assessment, three of the 19 communities were excluded because there were not enough farmworkers in those areas, resulting in a sample of 546. Thus, 16 communities and eight labor camps were matched according to community size, percent Hispanic, and treatment arm of the cancer study, and then randomized within each pair to treatment assignment for the present study.
Figure 1.
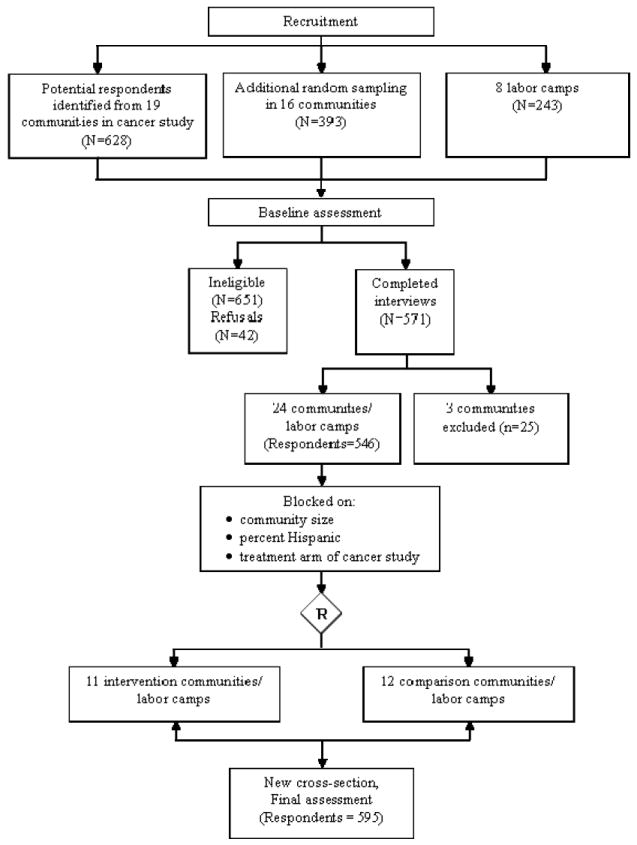
Study Design of the For Healthy Kids! Study
Intervention activities were initiated following the baseline assessment and continued for two years. One labor camp randomized to the intervention group closed down during the intervention, resulting in 11 intervention and 12 comparison communities. At the end of the intervention period, a follow-up cross-sectional sample of 595 households from participating communities and labor camps was enrolled in the summer of 2002. The sampling methods used for the baseline sample were employed at follow-up. Of 1,158 households approached, 486 were ineligible because a farmworker did not reside in the household, and 39 households could not be reached. Of the remaining 633 households, 595 (94%) agreed to participate. Upon completion of the final assessment, intervention materials developed for local organizations were disseminated in the control communities.
Survey Procedures
Prior to the interviews, each household received a letter in English and Spanish describing the study and providing contact information for the local project office if individuals had questions or did not want to participate. Locally hired and trained bi-lingual staff obtained informed consent and conducted in-person interviews with adult farmworkers at their homes in the summers of 1999 and 2002. When more than one adult farmworker resided in the household, birthdates were used to select a respondent. The baseline survey instrument contained 73 items and inquired about agricultural tasks, general pesticide exposure in job tasks, personal perceived health effects of exposure, farmworker protective practices at work, employer practices at work, family protective practices, and demographics. The follow-up instrument contained 87 items that covered the topics above and addressed respondents’ awareness of and participation in study activities in their communities in the past two to three years. Study design and data collection procedures were approved by the Human Subjects Board at the University of Washington and the Institutional Review Board at the Fred Hutchinson Cancer Research Center.
In addition to survey data, a process tracking system was created to monitor the types of activities in each community, the number held, and the number of individuals who participated in each event.
Intervention
Intervention messages sought to communicate information on the risks of pesticide exposure, particularly for children, symptoms of pesticide exposure, ways in which farmworkers and their families could be exposed, precautions to reduce pesticide exposure, and an overview of the project. Intervention activities were implemented at the community level, the organizational environment, within social and family groups, and one-on-one with individuals. Community-wide events included activities sponsored by For Healthy Kids! (FHK), such as neighborhood block parties, participation in community-wide events, such as health fairs, Cinco de Mayo activities, and others, and messages communicated through local media outlets. At community events, project staff set up a road-ready booth that showcased interactive displays, including videos that featured fluorescent whitening agents to show how pesticide residue can remain on the skin, demonstrations of how pesticides can be transported into the house from residue on farmworkers’ skin and clothing, and precautionary measures to reduce the take-home pathway. A puppet show designed by a local university focused on educating children how they could protect themselves from pesticides (for example, not entering fields where pesticides have been used). Materials were primarily visual and bilingual and included educational items for children such as coloring books and balloons with pesticide safety messages. Small incentives were provided at these events and included new caps, gloves, crates for outdoor storage of work boots, and similar items.
Organizational-level interventions included collaborations with ongoing activities and local organizations, such as Head Start, grade schools, ESL classes, local churches, farmworker clinics, worksites, and parents’ meetings, among others. For example, project staff developed a curriculum around pesticide safety for use with children in Head Start programs and provided training for Head Start teachers. Interventionists also made presentations at local grade schools that coincided with and promoted an annual student calendar contest addressing pesticide safety. Among participating worksites, interventionists held meetings with farmworkers to discuss pesticide safety and distribute an agricultural worker manual that was developed by the study. At each of the organizations, interventionists distributed handouts on pesticide safety in English and Spanish as well as detergent packets, bags for sorting clothes, shoe crates, and shower kits.
Outreach played an important role in the individual and small group activities. These approaches relied heavily on promotoras, or lay health workers, to lead activities and direct discussions around pesticide safety. The promotoras received extensive training in the purpose of the research study, pesticide exposure, the take-home pathway, and protective measures. For the home health parties promotoras recruited individuals who invited friends and relatives to their homes, and the promotoras led a guided discussion on pesticides and protecting oneself and one’s family. Promotoras also interacted individually and in small groups with community members at community-wide events, through door-to-door home visits, and at grocery stores and other places frequented by farmworkers. As part of their outreach, promotoras handed out various items such as clothes-washing kits, hand-washing kits, showering kits, and other items.
Intervention activities varied across sites according to their size and organizational infrastructure. For example, because labor camps did not have public institutions, intervention activities were primarily in the form of block parties, home health parties, and one-on-one outreach.
Measures
The primary outcomes of interest for this analysis were recent behaviors taken by farmworkers to reduce the take-home pathway of pesticide exposure. Respondents were asked how often in the past three months they washed their hands immediately after work, removed their work boots before entering the home, and washed work clothes separately from household laundry. Response categories were “always, usually, sometimes, rarely, or never.” For the analysis, we collapsed these categories to “always/usually” and “sometimes/rarely/never” to allow comparisons in the analysis between farmworkers who engaged in these practices consistently with those who did not. Respondents were also asked how soon after returning home from work they removed their work clothes and showered or bathed (“less than 1 hour, 1 to 2 hours, more than 2 hours”), and after how many wearings they washed their work clothes (“after wearing one time, after wearing two times, after wearing three or more times”). We collapsed these variables into “less than one hour” versus “one or more hours” and “after wearing one time” versus “wearing two or more times,” respectively. Although the intervention focused primarily on behaviors related to the take-home pathway, some intervention activities also addressed precautions to reduce pesticide exposure at work. Thus, we also examined farmworkers’ reported use of personal protective equipment (PPE) at work as secondary outcomes, namely how often when not working as an applicator or sprayer of pesticides they wore gloves, boots, protective lenses, and a hat at work in the past three months. These responses were collapsed to “always/usually” and “sometimes/rarely/never.”
We created separate indices for work and home protective practices by adding one point for each precaution that respondents reported performing consistently. For example, respondents who reported “always” or “usually” changing out of their work clothes within one hour of arriving home from work were assigned one point towards this index. The resulting indices included a 4-point scale for work protective practices and a 6-point scale for home protective practices.
Data Analysis
Because farmworker households were nested within communities, we controlled for potentially correlated responses by modeling communities as random effects. To evaluate the effectiveness of the intervention in improving adoption of specific pesticide safety practices over time, we performed mixed-effects logistic regression models using the SAS procedure GLIMMIX (29). To test whether the intervention was effective in increasing the overall number of precautions taken, we regressed the behavior indices, modeled as continuous responses, on independent variables in linear mixed models using the MIXED procedure (30). Intervention status, time of assessment, and the interaction of intervention by time were treated as fixed effects in both types of models. A test of the interaction term determined whether differences in reported behaviors over time varied between the intervention and control communities. We used the linear predictors of the regression models to calculate expected frequencies of reported behaviors and means of the behavior indices by intervention status and time of assessment. Although communities were randomized to treatment assignment, we added covariates to subsequent regression models to control for potential confounding and increase precision. Covariates included gender, age, education (less than 5th grade, 5th to 8th grade, some high school, high school graduate or higher), ethnicity (Hispanic/ non-Hispanic White), community type (community/labor camp), job task (handler of pesticides/ non-handler), receipt of training in the previous five years (yes/no), and the number of years working in agriculture. We also evaluated whether community type and gender were effect modifiers by including additional interaction terms in the regression models.
Missing Data
The baseline sample was missing age in approximately 15 percent of respondents because some of the interviewers failed to collect respondents’ age. Respondents with missing age at baseline were more likely to be Hispanic (p=0.01) and report fewer years of education (p=0.05) than respondents with complete age data. Described in detail elsewhere (31), we used multiple imputation to prevent systematic bias and loss of power with a complete case analysis (32, 33). We generated a set of five plausible values for each missing observation by regressing age on predictors that were included in the analytic model, significantly associated with missingness, and significantly correlated with age. We used a bootstrap sample with the program ICE in Stata 8.0, which performs multiple imputation with chained equations (34, 35). We then created five copies of the follow-up sample and merged the baseline and follow-up datasets. Using the procedure MIANALYZE in SAS 9.1 (30, 36), we performed the mixed model regression analyses described above on each of the five datasets and obtained estimated coefficients and standard errors that incorporated within- and between-imputation variability (33).
Secondary Analysis
We conducted a secondary analysis of the follow-up data to evaluate the extent to which participation in specific intervention activities was associated with the number of precautions performed. At the follow-up assessment, respondents indicated (yes/no) whether they had participated in specific programs or activities in their communities in the past two or three years. We regressed the work and home behavior indices on each participation measure in separate models and controlled for gender, age, education, ethnicity, community intervention status, community type, job task, receipt of training in the previous five years, and the number of years in agriculture. Models for two participation measures (home health parties, programs about protection from pesticides at work) were run separately for men and women due to effect modification by gender.
Results
For this analysis, we excluded respondents who were of an ethnicity other than Hispanic or non-Hispanic White (n= 4 at baseline) and who reported not working in the fields in the previous three months (n= 13 at baseline; n=32 at follow-up). Our final dataset contained a baseline sample of 529 farmworkers and a follow-up sample of 562 farmworkers.
In general, respondents at both baseline and follow-up were predominantly male, Hispanic, married, and had children under 18 living in their homes (Table 1). Nearly half were under the age of 35. Approximately two-thirds completed eight years of education or less, and approximately 80 percent reported an annual household income of $25,000 or less. Nearly one-third of respondents reported handling pesticides directly in the previous three months at baseline, and less than a quarter reported doing so at follow-up. Notably, less than one-third of farmworkers at both time points reported being trained in pesticide safety through their employer in the past five years. There were no significant differences at baseline or follow-up in demographic characteristics by intervention status.
Table 1.
Characteristics of the Baseline and Follow-up Cross-sectional Samples, by Randomization Group*
| Baseline, % | Follow-up, % | |||
|---|---|---|---|---|
| Control N=284 | Intervention N=245 | Control N=303 | Intervention N=259 | |
| Gender | ||||
| Male | 73.6 | 71.4 | 65.7 | 71.4 |
| Female | 26.4 | 28.6 | 34.3 | 28.6 |
| Ethnicity | ||||
| Hispanic | 88.7 | 89.4 | 96.4 | 92.3 |
| White, non-Hispanic | 11.3 | 10.6 | 3.6 | 7.7 |
| Age (years) | ||||
| 18 to 24 | 11.1 | 14.6 | 15.5 | 17.4 |
| 25 to 34 | 32.8 | 31.6 | 35.0 | 31.7 |
| 35 to 49 | 35.8 | 33.3 | 33.3 | 31.6 |
| 50 and older | 20.3 | 20.5 | 16.2 | 19.3 |
| Education | ||||
| <5th grade | 33.8 | 32.2 | 31.7 | 33.6 |
| 5th to 8th grade | 32.4 | 35.5 | 31.0 | 34.0 |
| Some high school | 21.5 | 20.4 | 25.1 | 20.5 |
| ≥ High school graduate | 12.3 | 11.8 | 12.2 | 12.0 |
| Annual household income (n=1,038) | ||||
| ≤$15,000 | 49.4 | 53.6 | 52.3 | 58.4 |
| $15,001 to $25,000 | 30.3 | 31.5 | 31.1 | 28.4 |
| >$25,000 | 20.3 | 14.9 | 16.6 | 13.2 |
| Marital status | ||||
| Married/living as married | 81.0 | 82.5 | 78.9 | 77.6 |
| Other | 19.0 | 17.5 | 21.1 | 22.4 |
| Children under 18 living in home | ||||
| Yes | 72.9 | 80.0 | 74.2 | 71.7 |
| No | 27.1 | 20.0 | 25.8 | 28.3 |
| Handler of pesticides past 3 months | ||||
| Yes | 33.8 | 28.6 | 23.1 | 19.7 |
| No | 66.2 | 71.4 | 76.9 | 80.3 |
| Pesticide safety training past 5 years | ||||
| Yes | 30.6 | 27.4 | 27.8 | 27.0 |
| No | 69.4 | 72.7 | 72.2 | 73.0 |
| Provided PPE | ||||
| Yes | 44.4 | 39.6 | N/A | N/A |
| No | 55.6 | 60.4 | N/A | N/A |
| Years in agriculture (Mean, SD) (n=1,072) | 16.6 (13.0) | 14.8 (12.2) | 12.8 (10.9) | 12.7 (11.5) |
Percentages based on the number of valid responses for each item.
We present expected frequencies of reported pesticide safety practices and expected mean number of safety behaviors performed in Table 2. In general, between baseline and follow-up, the percentage of farmworkers who reported regularly engaging in specific pesticide safety practices increased in both intervention and control communities. Notably, we observed an increase of nearly 30 percentage points in both intervention and control communities in the proportion of farmworkers who wore protective boots to work. Washing hands immediately after work and wearing a hat showed increases ranging from eight to 14 percentage points between baseline and follow-up assessments. Similarly, the total number of behaviors performed regularly in the past three months increased with time in both treatment groups, as shown by the work behavior and home behavior indices. For home behaviors in particular, the average number of behaviors performed increased from 3.8 and 3.6 in the control and intervention communities, respectively, to approximately 5 among all respondents. This represents a change of approximately 32 percent and 41 percent, respectively.
Table 2.
Expected Frequency of Pesticide Safety Practices and Expected Mean Number of Behaviors Performed in the Past 3 Months, by Intervention Group and Time
| Control | Intervention | Differencea | Pb | Pc | |||
|---|---|---|---|---|---|---|---|
| Base-line N=284 | Follow-up N=303 | Base-line N=245 | Follow-up N=259 | ||||
| % | % | % | % | ||||
| Work Protective Practices | |||||||
| Gloves | 39.2 | 46.5 | 38.2 | 43.6 | |||
| Change | 7.3 | 5.4 | -1.9 | 0.74 | 0.73 | ||
| Boots | 40.4 | 69.3 | 43.8 | 74.2 | |||
| Change | 28.9 | 30.4 | 1.5 | 0.67 | 0.84 | ||
| Protective lenses | 22.1 | 24.7 | 24.5 | 25.6 | |||
| Change | 2.6 | 1.1 | -1.5 | 0.76 | 0.54 | ||
| Hat | 84.3 | 94.2 | 80.5 | 94.2 | |||
| Change | 9.9 | 13.7 | 3.8 | 0.54 | 0.57 | ||
| Home Protective Practices | |||||||
| Wash hands right after work | 58.9 | 69.6 | 57.7 | 65.9 | |||
| Change | 10.7 | 8.2 | -2.5 | 0.64 | 0.52 | ||
| Take off shoes/boots before entering home | 60.6 | 60.3 | 53.1 | 70.0 | |||
| Change | -0.3 | 16.9 | 17.2 | 0.004 | 0.003 | ||
| Change out of work clothes within 1 hour of arriving home | 61.3 | 66.6 | 53.4 | 70.0 | |||
| Change | 5.3 | 16.6 | 11.3 | 0.06 | 0.05 | ||
| Shower within 1 hour of arriving home | 49.8 | 59.3 | 45.8 | 51.9 | |||
| Change | 9.5 | 6.1 | -3.4 | 0.58 | 0.41 | ||
| Wash work clothes after one wearing | 67.0 | 75.2 | 64.3 | 70.7 | |||
| Change | 8.2 | 6.6 | -1.6 | 0.70 | 0.99 | ||
| Wash work clothes separately from household laundry | 84.0 | 89.8 | 82.4 | 89.5 | |||
| Change | 5.8 | 7.1 | 1.3 | 0.82 | 0.68 | ||
| Mean | Mean | Mean | Mean | ||||
| Work behavior index (range=0-4) | 1.86 | 2.35 | 1.86 | 2.37 | |||
| Change | 0.49 | 0.51 | 0.02 | 0.85 | 0.95 | ||
| Home behavior index (range=0-6) | 3.82 | 5.08 | 3.58 | 5.04 | |||
| Change | 1.26 | 1.46 | 0.20 | 0.28 | 0.19 | ||
Difference between change in intervention communities and change in control communities
P value is for the test of the intervention × time (baseline vs. follow-up) interaction
P value is for the test of the intervention × time (baseline vs. follow-up) interaction, controlling for gender, ethnicity, education, age, community type, receipt of training in past 5 years, job task, and years working in agriculture
For most behaviors, the extent to which these changes over time varied by intervention status was not statistically significant. We did find, however, that the changes were significantly greater in the intervention communities for removing work boots before entering the house and marginally significantly greater for changing out of work clothes within one hour of arriving home. Adjusting for demographics and potential confounders did not considerably alter our estimates. Additionally, the interaction terms used to evaluate whether community type and gender modified the effect of the intervention were not significant, indicating that the intervention had a similar effect over time in communities and labor camps and among men and women.
The secondary analysis revealed that participation in some intervention programs was associated with reporting more precautions at the follow-up assessment, particularly among women (Table 3). The only specific intervention activity associated with increased precautions was participation in home health parties; women who participated in these events reported performing significantly more precautions at work than women who did not participate. We found no significant associations between participation in home health parties and increased precautions at work among men, and increased precautions at home among men and women. Having participated in general programs about keeping pesticides from entering the home and about protection from pesticides at work was also associated with reporting more precautions.
Table 3.
Adjusted regression coefficientsa for work and home behavior indices of pesticide safety practices and participation in program activities, among farmworkers surveyed at follow-up (N=558)
| Intervention Activity | Work Behavior Indexb | Home Behavior Indexc | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | p-value | β | 95% CI | p-value | |
| General | ||||||
| Programs about keeping pesticides from entering home | 0.22 | (0.003, 0.44) | 0.05 | 0.24 | (-0.12, 0.61) | 0.19 |
| Programs about protection from pesticides at work | 0.44 | (0.06, 0.81) | 0.02 | |||
| Men (N=384) | -0.01 | (-0.26, 0.23) | 0.93 | |||
| Women (N=176) | 0.63 | (0.14, 1.12) | 0.01 | |||
| Programs or activities | ||||||
| Health fairs or block parties | 0.10 | (-0.16, 0.36) | 0.44 | 0.05 | (-0.39, 0.49) | 0.82 |
| Presentations at schools or adult education classes | -0.13 | (-0.38, 0.12) | 0.30 | 0.03 | (-0.38, 0.45) | 0.87 |
| Someone coming to your door | 0.14 | (-0.07, 0.35) | 0.19 | 0.14 | (-0.21, 0.49) | 0.43 |
| Church events | 0.29 | (-0.04, 0.62) | 0.09 | 0.44 | (-0.10, 0.98) | 0.11 |
| Home health parties | 0.38 | (-0.08, 0.83) | 0.10 | |||
| Men (N=384) | -0.01 | (-0.34, 0.31) | 0.94 | |||
| Women (N=176) | 0.83 | (0.32, 1.35) | 0.002 | |||
| Presentations at organizations | 0.05 | (-0.23, 0.32) | 0.75 | 0.19 | (-0.27, 0.65) | 0.42 |
Adjusted for gender (where applicable), age, ethnicity, community intervention status, education, pesticide safety training, occupation task, and years in agriculture
Values for the work behavior index ranged from 0 to 4
Values for the home behavior index ranged from 0 to 6
Respondents in intervention communities consistently reported greater awareness of and participation in intervention activities compared to respondents in control communities (Table 4). For example, 29 percent of respondents residing in intervention communities at the follow-up assessment had heard of health fairs or block parties related to pesticide safety taking place in their communities compared with 19 percent of respondents in control communities. We observed a similar pattern for participation in intervention activities. Nonetheless, the finding that farmworkers in control communities reported participating in intervention events indicates that some contamination occurred.
Table 4.
Awareness of and participationa in health programs or activities in intervention and control communities, assessed at follow-up*
| Awareness N (%) | Participation N (%) | |||
|---|---|---|---|---|
| Control (N=303) | Intervention (N=259) | Control (N=303) | Intervention (N=259) | |
| Any intervention program or activity | 152 (50.2) | 174 (67.2) | 90 (29.7) | 130 (50.2) |
| General | ||||
| Programs about keeping pesticides from entering home | 88 (29.0) | 122 (47.1) | 39 (12.8) | 71 (27.4) |
| Programs about protection from pesticides at work | 96 (31.7) | 121 (46.7) | 36 (11.8) | 62 (23.9) |
| Programs or activities | ||||
| Health fairs or block parties | 56 (18.5) | 76 (29.3) | 24 (7.9) | 39 (15.1) |
| Presentations at schools or adult education classes | 52 (17.2) | 74 (28.6) | 24 (7.9) | 43 (16.6) |
| Someone coming to your door | 48 (15.8) | 101 (39.0) | 35 (11.6) | 84 (32.4) |
| Church events | 34 (11.2) | 56 (21.6) | 11 (3.6) | 27 (10.4) |
| Home health parties | 33 (10.9) | 67 (25.9) | 14 (4.6) | 44 (17.0) |
| Presentations at organizations | 48 (15.8) | 79 (30.5) | 17 (5.6) | 40 (15.4) |
Respondents were asked if they had heard about and had participated in these programs or activities taking place in their communities in the past two or three years
Percentages based on the number of valid responses for each item.
Table 5 presents the number and type of activities implemented throughout the two year intervention period. In total, nearly 2,000 events were held in the intervention communities. Although there is considerable variation in the number of events held per community, this is expected considering the range in population size of the communities and labor camps.
Table 5.
Process results from the 11 intervention communities in the For Healthy Kids! Study
| Total Number of Events | Number of Events per Community | Total Number of Participants | Number of Participants per Event | |||
|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | |||
| Community-level | ||||||
| Community-wide eventsa | 93 | 8 | 1-27 | 6,009 | 44 | 6-102 |
| Media | 165 | 17 | 1-48 | NA | NA | NA |
| Intermediate | ||||||
| Presentations at schools (6 communities) | 210 | 35 | 1-81 | 5,016 | 22 | 16-25 |
| Church events (6 communities) | 26 | 4 | 2-7 | 1,414 | 54 | 14-80 |
| Otherb | 128 | 12 | 1-59 | 1,483 | 13 | 3-26 |
| Small group | ||||||
| Home parties | 979 | 89 | 7-333 | 3,721 | 4 | 3-6 |
| Otherc | 332 | 30 | 4-81 | 856 | 3 | 2-6 |
Includes FHK-sponsored events, such as health fairs and block parties, and community events in which FHK participated
Includes presentations at work-sites, farmworkers’ clinics, parents’ meetings, ESL/GED/Citizenship classes, etc.
Includes other small group activities, such as home visits and outreach
Discussion
In this study we report the self-reported behavioral outcomes of a randomized community intervention trial designed to break the take-home pathway of pesticide exposure through a culturally appropriate community intervention. Overall, we observed modest effects, with two of the six behaviors showing increased adoption associated with the intervention. These behaviors included removing work boots before entering the home and changing out of work clothes within one hour of arriving home. The increase in reported frequency over time was 17 percentage points and 11 percentage points higher in the intervention than the control communities for the two behaviors, respectively. For other home-related behaviors, the frequency with which farmworkers reported engaging in them was considerably higher at follow-up compared to baseline for respondents in both intervention and control communities. Work-related behaviors showed similar changes among respondents in intervention and control communities.
There are several possible reasons why the intervention was associated with positive change in some behaviors and not others. First, we would expect work practices to be less amenable to change associated with the intervention (compared with home practices) given that farmworkers’ use of these items is related to the work environment, whether such items are provided, their job tasks, and training histories (31). The observed increase of approximately 30 percentage points in the proportion of farmworkers who reported wearing boots at work may suggest a change in employer practices, workplace norms, or the availability of boots to farmworkers over time. Second, some behaviors, such as washing work clothes separately from household laundry, were already performed by the majority of farmworkers at baseline, reducing the likelihood of detecting additional change. Third, some behaviors may be more amenable to change than others for practical or cultural reasons. For example, previous research has underscored the importance of humoral beliefs in this population such that farmworkers often report delaying showering for over an hour after work in order to allow their bodies to cool fully for fear of developing arthritis or other health problems (37, 38). Finally, it is possible that the intervention promoted certain behaviors more effectively than others.
Concurrent events likely contributed to some of the changes in behavior observed between the two assessments. As shown by the behavior indices, there was an overall increase in the number of home behaviors performed between baseline and follow-up of approximately 30 percent and 40 percent among respondents in control and intervention communities, respectively. The observed increases in behavior are indeed encouraging; however, we are unable to discern the role of the intervention in producing changes when there are equivalent increases in the intervention and control communities over time. Pesticide exposure has long been a concern in agricultural communities, and it is likely that local or other efforts to address these issues reached farmworkers in control communities. Detecting intervention effects independent of changes over time has been an important challenge in community trials (39, 40).
It is also likely that some contamination occurred among respondents living in the control communities. Although geographically distinct, the communities in the Lower Yakima Valley are relatively small and in close proximity. Farmworkers may live and work in different communities, and in the smaller areas or labor camps, it may be necessary to travel to a nearby community for shopping or recreation. In addition, farmworkers from different communities may have been exposed to intervention activities and messages at worksites located in intervention communities. Evidence for contamination is provided by our finding that respondents in control communities did report having participated in intervention activities; however, the frequency of awareness and participation was consistently higher among respondents in intervention communities. It is not clear to what extent this level of contamination may have affected our results.
Despite the large number of activities that were carried out, the intervention dose may not have been sufficient to effect widespread change among farmworkers residing in the intervention communities. One limitation of community interventions is that the dose is spread across a large population base. The multilevel approach used here was intended to reach farmworkers through multiple channels and capitalize on participants’ social networks. Our results indicate that approximately two-thirds and one-half of all farmworkers living in intervention communities at the follow-up reported being aware of and having participated in at least one intervention activity, respectively. This suggests that the intervention reached approximately half of the farmworker population, on average, across the eleven intervention communities, a penetration rate that is higher than that reported for other community trials (41, 42). Nonetheless, this level of exposure did not translate into extensive improvements in the adoption of precautions associated with the intervention. This could be because the intervention activities were not effective or because the dose was not strong enough to elicit change.
Results from the secondary analysis provide some suggestive evidence regarding intervention activities that were associated with positive behavioral outcomes. Our findings indicate that women who participated in home health parties reported a greater number of precautions at work at the follow-up assessment than women who did not participate in these events. Participation in general programs on reducing pesticide exposure at work and at home was also significantly associated with taking more precautions; however, it is possible that these programs were not a part of the For Healthy Kids! intervention. It is not clear why participation in the home health parties would be associated with greater precautions at work and not at home. Previous work among farmworker women has identified competing responsibilities, perceived lack of control, and cultural, family, and community factors as barriers to engaging in behaviors to reduce the take-home pathway (38). The secondary analysis also suggests that intervention activities, particularly home health parties, reached the women more effectively than the men.
Findings from a previous process evaluation provide support for the effectiveness and appeal of the home health parties, which accounted for nearly half of intervention activities. Although it is possible that home health party participants may have self-selected to participate as a result of greater interest in learning about pesticide safety, the evaluation found that a random sample of home party participants surveyed approximately 3 months following participation were consistently more likely than respondents at baseline to report engaging in pesticide safety practices (e.g. 86% of party attendees reported changing out of work clothes within one hour compared to 58% of respondents at baseline; unpublished data). Evaluations also indicated that participants found the parties useful and informative. Activities such as home health parties are more resource- and time-intensive and have a narrower reach than events such as health fairs, but our findings suggest that participants responded favorably to this format. Events such as home health parties utilize participants’ existing social networks and provide information in an environment that is safe and familiar. The use of lay health workers to disseminate information is a popular strategy in studies involving low-income Hispanics and has been associated with positive outcomes (43-47).
The intervention activities developed in partnership with the CAB comprised a ‘kitchen sink’ approach with multiple components implemented simultaneously throughout the intervention communities. This approach had the potential to be synergistic such that exposure to combinations of activities and messages may have been important for behavior change, but these relationships are difficult to evaluate. The secondary analysis provided some suggestive evidence of the effectiveness of the individual components, but these findings should be interpreted with caution given the potential for self-selection among program participants, the inability to control for baseline behavior rates, and the lack of adherence to the randomized design in the secondary analysis. A more thorough evaluation of specific intervention activities that includes, for example, inquiries regarding the appeal and value of the different activities and precautions performed by program participants, would have helped delineate which activities participants found useful, informative, and interesting and would inform the design of future intervention efforts. Such an evaluation was conducted with home health party participants but not with participants of other intervention activities.
In this analysis we examined a number of outcome variables, which raises the possibility that associations may be significant due to chance alone. Because this was a community intervention, where messages were spread across a wide population base, and where survey respondents were not necessarily program participants but rather were intended to constitute a representative sample of community members, observed effects associated with the intervention were anticipated to be small (25). Thus, we chose not to adjust for multiple comparisons. In addition, although we observed significant changes associated with the intervention in certain behaviors, we did not evaluate the extent to which these behaviors reduced pesticide exposure. Previous work indicated that the intervention was not associated with reduced exposure over time as measured by concentrations of urinary pesticide metabolites in adult farmworkers and their children and pesticide residue in house and vehicle dust (20). Our data may also be limited by the self-reported nature of our outcome measures. Finally, the multiple imputation performed on age at baseline may have introduced a degree of uncertainty into the analysis. However, we used age to control for confounding only, and performing a complete case analysis would have reduced power and increased the potential for biased estimates.
This study also has a number of strengths. The community-based participatory research approach promoted community ownership of the project, ensured cultural appropriateness of intervention materials, and invariably contributed to the high response rate obtained at both assessments, which resulted in a very large sample of farmworkers. The intervention was multilevel and disseminated messages through various channels. Such a comprehensive approach has been recommended for promoting behavior change among Hispanic populations (48). In addition, the intervention was designed to promote the sustainability of certain components, all of which addressed pesticide safety in relation to agricultural work and the family. These include the Head Start curriculum for young children, the manual for workers, the elementary school calendar contest on pesticide safety, and local media messages.
The use of a randomized community intervention trial within the framework of community-based participatory research represents an innovative approach for the design and evaluation of strategies to reduce the take-home pathway of pesticide exposure in farmworker households. Further research is needed to identify successful strategies for reducing the take-home pathway of pesticide exposure. The long-term reduction of pesticide exposure in farmworkers and their families ultimately requires work environments that facilitate greater use of protective clothing and equipment and that provide options for changing out of and storing work clothes, and enhanced safety standards that limit opportunities for exposure, in addition to individual behavior change (49). Mobilizing the community to promote increased awareness of the risks of pesticide exposure among farmworkers, their families, and communities as a whole, including growers, marks an important step towards that aim.
Acknowledgments
The authors thank members of the community advisory board, the staff at the community field office, and the participants in this survey for their time and energy in this research, and Dale McLerran for his assistance with data analysis.
This research was supported by grants from The National Institute of Environmental Health Sciences (PO1 ES09601), the United States Environmental Protection Agency (R826886), and the National Institute for Occupational Safety and Health (T42 CCT010418). The opinions expressed here are those of the authors and do not necessarily reflect those of the funding agencies.
Footnotes
No competing financial interests exist for any of the authors.
References
- 1.Fenske RA, Lu C, Simcox NJ, et al. Strategies for assessing children’s organophosphorus pesticide exposures in agricultural communities. J Expo Anal Environ Epidemiol. 2000;10:662–671. doi: 10.1038/sj.jea.7500116. [DOI] [PubMed] [Google Scholar]
- 2.Curl CL, Fenske RA, Kissel JC, et al. Evaluation of take-home organophosphorus pesticide exposure among agricultural workers and their children. Environ Health Perspect. 2002;110:A787–792. doi: 10.1289/ehp.021100787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rao P, Quandt SA, Doran AM, Snively BM, Arcury TA. Pesticides in the homes of farmworkers: Latino mothers’ perceptions of risk to their children’s health. Health Educ Behav. 2007;34:335–353. doi: 10.1177/1090198106288045. [DOI] [PubMed] [Google Scholar]
- 4.Thompson B, Coronado GD, Grossman JE, et al. Pesticide take-home pathway among children of agricultural workers: study design, methods, and baseline findings. J Occup Environ Med. 2003;45:42–53. doi: 10.1097/00043764-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 5.McCauley LA, Lasarev MR, Higgins G, et al. Work characteristics and pesticide exposures among migrant agricultural families: a community-based research approach. Environ Health Perspect. 2001;109:533–538. doi: 10.1289/ehp.01109533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quandt SA, Arcury TA, Rao P, et al. Agricultural and residential pesticides in wipe samples from farmworker family residences in North Carolina and Virginia. Environ Health Perspect. 2004;112:382–387. doi: 10.1289/ehp.6554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldman L, Eskenazi B, Bradman A, Jewell NP. Risk behaviors for pesticide exposure among pregnant women living in farmworker households in Salinas, California. Am J Ind Med. 2004;45:491–499. doi: 10.1002/ajim.20012. [DOI] [PubMed] [Google Scholar]
- 8.Lu C, Fenske RA, Simcox NJ, Kalman D. Pesticide exposure of children in an agricultural community: evidence of household proximity to farmland and take home exposure pathways. Environ Res. 2000;84:290–302. doi: 10.1006/enrs.2000.4076. [DOI] [PubMed] [Google Scholar]
- 9.Simcox NJ, Fenske RA, Wolz SA, Lee IC, Kalman DA. Pesticides in household dust and soil: exposure pathways for children of agricultural families. Environ Health Perspect. 1995;103:1126–1134. doi: 10.1289/ehp.951031126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coronado GD, Vigoren EM, Thompson B, Griffith WC, Faustman EM. Organophosphate pesticide exposure and work in pome fruit: evidence for the take-home pesticide pathway. Environ Health Perspect. 2006;114:999–1006. doi: 10.1289/ehp.8620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daniels JL, Olshan AF, Savitz DA. Pesticides and childhood cancers. Environ Health Perspect. 1997;105:1068–1077. doi: 10.1289/ehp.971051068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eskenazi B, Bradman A, Castorina R. Exposures of children to organophosphate pesticides and their potential adverse health effects. Environ Health Perspect. 1999;107:409–419. doi: 10.1289/ehp.99107s3409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Landrigan PJ. Pesticides and polychlorinated biphenyls (PCBs): an analysis of the evidence that they impair children’s neurobehavioral development. Mol Genet Metab. 2001;73:11–17. doi: 10.1006/mgme.2001.3177. [DOI] [PubMed] [Google Scholar]
- 14.Weiss B, Amler S, Amler RW. Pesticides. Pediatrics. 2004;113:1030–1036. [PubMed] [Google Scholar]
- 15.United States Environmental Protection Agency. Steps to protect yourself from pesticides (Spanish). Prevention, pesticides, and toxic substances (7506C) 1995 EPA 735-F-95-002. [Google Scholar]
- 16.Curwin BD, Hein MJ, Sanderson WT, Nishioka M, Buhler W. Acephate exposure and decontamination on tobacco harvesters’ hands. J Expo Anal Environ Epidemiol. 2003;13:203–210. doi: 10.1038/sj.jea.7500271. [DOI] [PubMed] [Google Scholar]
- 17.National Institutes of Occupational Safety and Health. Report to Congress on Workers’ Home Contamination Study conducted under the Workers’ Family Protection Act. U.S. Department of Health and Human Services, CDC/NIOSH; 1995. [Google Scholar]
- 18.McCauley LA, Michaels S, Rothlein J, Muniz J, Lasarev M, Ebbert C. Pesticide exposure and self reported home hygiene: practices in agricultural families. AAOHN J. 2003;51:113–119. [PubMed] [Google Scholar]
- 19.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 20.Thompson B, Coronado GD, Vigoren EM, et al. Para Niños Saludables: A communtiy intervention trial to reduce organophosphate pesticide exposure in children of farmworkers. Environ Health Perspect. 2008;116 doi: 10.1289/ehp.10882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.United States Department of Agriculture. 2002 Census of Agriculture, volume 1 Chapter 2: Washington County Level Data. Washington, D.C.: United States Department of Agriculture, National Agricultural Statistics Service; 2002. [Google Scholar]
- 22.U.S. Census Bureau. U.S. Census Bureau, Detailed Tables: Yakima County, Washington American FactFinder. Washington, D.C.: U.S. Census Bureau; 2002. [Google Scholar]
- 23.Thompson B, Coronado G, Solomon C, McLerran DF, Neuhauser ML, Feng Z. Cancer prevention behaviors and socioeconomic status among Hispanics and non-Hispanic Whites in a rural population in the United States. Cancer Causes Control. 2002;13:719–728. doi: 10.1023/a:1020280427712. [DOI] [PubMed] [Google Scholar]
- 24.Thompson B, Coronado G, Puschel K, Allen E. Identifying constituents to participate in a project to control pesticide exposure in children of farmworkers. Environ Health Perspect. 2001;109(Suppl 3):443–448. doi: 10.1289/ehp.01109s3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thompson B, Coronado G, Snipes SA, Puschel K. Methodologic advances and ongoing challenges in designing community-based health promotion programs. Annu Rev Public Health. 2003;24 doi: 10.1146/annurev.publhealth.24.100901.140819. [DOI] [PubMed] [Google Scholar]
- 26.Koepsell TD, Diehr PH, Cheadle A, Kristal A. Invited commentary: symposium on community intervention trials. Am J Epidemiol. 1995;142:594–599. doi: 10.1093/oxfordjournals.aje.a117680. [DOI] [PubMed] [Google Scholar]
- 27.Koepsell TD, Wagner EH, Cheadle AC, et al. Selected methodological issues in evaluating community-based health promotion and disease prevention programs. Annu Rev Public Health. 1992;13:31–57. doi: 10.1146/annurev.pu.13.050192.000335. [DOI] [PubMed] [Google Scholar]
- 28.Feng Z, Thompson B. Some design issues in a community intervention trial. Control Clin Trials. 2002;23:431–449. doi: 10.1016/s0197-2456(02)00206-4. [DOI] [PubMed] [Google Scholar]
- 29.SAS Institute Inc. The GLIMMIX Procedure, Nov 2005. Cary, NC: SAS Institute Inc.; 2005. [Google Scholar]
- 30.SAS Institute Inc. SAS/STAT User’s Guide, Version 9.1. Cary, NC: SAS Institute Inc.; 2004. [Google Scholar]
- 31.Strong LL, Thompson B, Koepsell TD, Meischke H. Factors associated with pesticide safety practices in farmworkers. Am J Ind Med. 2008;51:69–81. doi: 10.1002/ajim.20519. [DOI] [PubMed] [Google Scholar]
- 32.Raghunathan TE. What do we do with missing data? Some options for analysis of incomplete data. Annu Rev Public Health. 2004;25:99–117. doi: 10.1146/annurev.publhealth.25.102802.124410. [DOI] [PubMed] [Google Scholar]
- 33.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: Wiley; 1987. [Google Scholar]
- 34.Royston P. Multiple imputation of missing values. The Stata Journal. 2004;4:227–241. [Google Scholar]
- 35.Royston P. Multiple imputation of missing values: update. The Stata Journal. 2005;5:188–201. [Google Scholar]
- 36.Yuan YC. Multiple Imputation for Missing Data: Concepts and New Development. Proceedings of the 25th Annual SAS Users Group International Conference; Indianapolis. 2000. Abstract P267-25. [Google Scholar]
- 37.Arcury TA, Quandt SA, Cravey AJ, Elmore RC, Russell GB. Farmworker reports of pesticide safety and sanitation in the work environment. Am J Ind Med. 2001;39:487–498. doi: 10.1002/ajim.1042. [DOI] [PubMed] [Google Scholar]
- 38.Strong LL, Starks HE, Meischke H, Thompson B. Perspectives of Mothers in Farmworker Households on Reducing the Take-Home Pathway of Pesticide Exposure. Health Educ Behav. 2009 January 9; doi: 10.1177/1090198108328911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sorensen G, Emmons K, Hunt MK, Johnston D. Implications of the results of community intervention trials. Annu Rev Public Health. 1998;19:379–416. doi: 10.1146/annurev.publhealth.19.1.379. [DOI] [PubMed] [Google Scholar]
- 40.Susser M. The tribulations of trials--intervention in communities. Am J Public Health. 1995;85:156–158. doi: 10.2105/ajph.85.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Community Intervention Trial for Smoking Cessation (COMMIT): I. cohort results from a four-year community intervention. Am J Public Health. 1995;85:183–192. doi: 10.2105/ajph.85.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thompson B, Coronado G, Chen L, Islas I. Celebremos la salud! a community randomized trial of cancer prevention (United States) Cancer Causes Control. 2006;17:733–746. doi: 10.1007/s10552-006-0006-x. [DOI] [PubMed] [Google Scholar]
- 43.Fernandez-Esquer ME, Espinoza P, Torres I, Ramirez AG, McAlister AL. A su salud: a quasi-experimental study among Mexican American women. Am J Health Behav. 2003;27:536–545. doi: 10.5993/ajhb.27.5.5. [DOI] [PubMed] [Google Scholar]
- 44.Hunter JB, de Zapien JG, Papenfuss M, Fernandez ML, Meister J, Giuliano AR. The impact of a promotora on increasing routine chronic disease prevention among women aged 40 and older at the U.S.-Mexico border. Health Educ Behav. 2004;31:18S–28S. doi: 10.1177/1090198104266004. [DOI] [PubMed] [Google Scholar]
- 45.Navarro AM, Senn KL, McNicholas LJ, Kaplan RM, Roppe B, Campo MC. Por La Vida model intervention enhances use of cancer screening tests among Latinas. Am J Prev Med. 1998;15:32–41. doi: 10.1016/s0749-3797(98)00023-3. [DOI] [PubMed] [Google Scholar]
- 46.Teufel-Shone NI, Drummond R, Rawiel U. Developing and adapting a family-based diabetes program at the U.S.-Mexico border. Prev Chronic Dis. 2005;2:A20. [PMC free article] [PubMed] [Google Scholar]
- 47.Liebman AK, Juarez PM, Leyva C, Corona A. A pilot program using promotoras de salud to educate farmworker families about the risk from pesticide exposure. J Agromedicine. 2007;12:33–43. doi: 10.1300/J096v12n02_04. [DOI] [PubMed] [Google Scholar]
- 48.Flores ET, Castro FG, Fernandez-Esquer ME. Social theory, social action, and intervention research: implications for cancer prevention among Latinos. J Natl Cancer Inst Monogr. 1995:101–108. [PubMed] [Google Scholar]
- 49.Arcury TA, Quandt SA, McCauley L. Farmworkers and pesticides: community-based research. Environ Health Perspect. 2000;108:787–792. doi: 10.1289/ehp.00108787. [DOI] [PMC free article] [PubMed] [Google Scholar]


