Abstract
Ozone is associated with health impacts including respiratory outcomes; however, results differ across studies. Meta-analysis is an increasingly important approach to synthesizing evidence across studies. We conducted meta-analysis of short-term ozone exposure and respiratory hospitalizations to evaluate variation across studies and explore some of the challenges in meta-analysis. We identified 136 estimates from 96 studies and investigated how estimates differed by age, ozone metric, season, lag, region, disease category, and hospitalization type. Overall results indicate associations between ozone and various types of respiratory hospitalizations; however, study characteristics affected risk estimates. Estimates were similar, but higher, for the elderly compared to all ages and for previous day exposure compared to same day exposure. Comparison across studies was hindered by variation in definitions of disease categories, as some (e.g., asthma) were identified through ≥3 different sets of ICD codes. Although not all analyses exhibited evidence of publication bias, adjustment for publication bias generally lowered overall estimates. Emergency hospitalizations for total respiratory disease increased 4.47% (95% interval 2.48, 6.50%) per 10ppb 24-hr ozone among the elderly without adjustment for publication bias and 2.97% (1.05, 4.94%) with adjustment. Comparison of multi-city study results and meta-analysis based on single-city studies further suggested publication bias.
1. Introduction
Ozone is a highly reactive air pollutant that can irritate airways and interfere with host defense mechanisms[1] and is associated with risk of respiratory symptoms (e.g., coughing, wheezing), mortality, and hospital admissions.[2,3] Time-series and case-crossover studies have examined risk of respiratory hospitalizations or emergency room/department visits (emergency visits) as a function of short-term exposure to ambient ozone.
Many single-city studies observed associations between ozone and hospital admission for respiratory diseases,[4–7] including total respiratory diseases or general respiratory illness[8–23] and cause-specific respiratory diseases such as pneumonia,[10,24–26] chronic obstructive pulmonary disease (COPD),[10 25,27–32] and asthma.[31,33–50] Other studies reported no association or inconsistent results for total or general respiratory illnesses[51–59] or specific respiratory diseases.[58,60–70] Some studies found mixed results for different age groups or seasons.[71–73] Other potential confounders include co-pollutants, such as particulate matter (PM), with results differing by study [30,32,37,75,77]
Larger studies investigated multiple locations, reporting several individual-city estimates and/or a combined estimate across several locations. Many multi-city studies, such as the Air Pollution and Health: A European Approach (APHEA) project, found significant associations between ozone and hospital admissions for certain disease categories (e.g., total respiratory diseases, COPD), age group (e.g., elderly), or season (e.g., warm season).[78–83]
Although several studies identified links between ozone and risk of respiratory hospital admissions, several key questions remain, such as why study results differ, which would inform understanding of the overall scientific evidence for health risk and guide future research. Study and population characteristics such as location or age may impact effect estimates and thus hinder comparability across studies. For example, ozone was associated with increased respiratory hospitalizations among older people in Rotterdam but not Amsterdam,[84] and was associated with increased COPD and pneumonia admissions in Minneapolis-St. Paul, U.S., but significant associations were not observed in Birmingham, U.S.[85] Other study characteristics that may influence results include season, which can affect levels of ozone and other confounders, such as weather. Ozone levels are generally higher in summer due to photochemical formation.[86] Season can modify exposure patterns such as the use of open windows versus air conditioning, and these factors can differ by location. For instance, in analyses of 8-hr maximum ozone and total respiratory hospitalization of persons >64 years in London and Hong Kong, both cities had associations for all-year and the warm season; however, in cool seasons, only Hong Kong had an association.[87]
We investigated how various study characteristics impact results by using meta-analysis to integrate findings from previous studies with consideration of their uncertainty. Similar methods have been applied elsewhere, such as the study of short-term ozone exposure and mortality.[88–90] The goals of this project are to: assess the overall state of scientific evidence on ozone and respiratory hospital admissions; explore variation in effect estimates, such as by study location or age; and investigate some of the challenges inherent in meta-analysis such as publication bias, which is caused by the tendency for authors to submit or journals to publish statistically significant results as opposed to null or uncertain results.
2. Methods
We identified previously-conducted studies by searching PubMed for the following in the title and/or abstract: 1) “ozone” or “O3”, and 2) “hospital admission*,” “hospitalization*,” “emergency room,” “emergency department,” or “emergency visits,” where “*” reflects truncation indicating acceptance of any value. We selected studies meeting the following criteria: 1) investigated the association between short-term ozone exposure (single day or a few days) and hospital admissions or emergency visits for respiratory diseases through time-series or case cross-over approaches; 2) provided quantitative results with quantitative measure of the estimate’s uncertainty; 3) included a non-linear function for temperature in the regression model, except for season-specific results (e.g., warm season); and 4) were peer-reviewed and published in English from 1990 to 2008. Some early time-series analysis used linear regression models[12,33,51,91–96] and were excluded due to non-normally distributed health data.[97] We excluded a study that applied logarithmic transformation to ozone exposures.[98]
We recorded study characteristics including time frame and location of the study, disease categories (e.g., pneumonia, asthma), disease diagnosis codes (e.g., the International Classification of Disease ICD-9 codes), type of hospital visit (e.g., general hospital admissions, emergency visits), effect estimates with uncertainties in various formats (e.g., percentage change in risk of hospitalization and 95% confidence interval), ozone units (e.g., ppb, µg/m3), ozone temporal metric (e.g., 24-hr mean), age of subjects (e.g., elderly), lag (e.g., same day as lag0, previous day as lag1, average of same and previous days as lag0–1), season of analysis (e.g., summer), and co-pollutants included in models. Many studies reported multiple estimates as they explored several disease categories, age groups, seasons, or other factors. For studies presenting results from several cities, the meta-analysis included one result per city per study. For multi-city studies that only reported a combined estimate across cities, we analyzed these results separately and did not include them in the meta-analysis in order to compare single-city and multi-city results.
We used the standard chi-squared test, χ2 , to examine the homogeneity among effect estimates. Under homogeneity, the fixed-effect model was used to combine estimates; otherwise, the random-effect model was used.[99] We used statistical software R (version 2.9.2). We required at least four estimates to calculate an overall estimate in the meta-analysis. Results are presented as the percentage change in risk of hospital visit per 10ppb increase in 24-hr ozone. We also present key results based on the daily 8-hr maximum ozone metric. Stratification was used to explore whether meta-analysis estimates differ by use of ozone metric, age, lag for exposure, season, or region.
Studies used different metrics and units for ozone concentrations. We converted all results in µg/m3 to ppb for comparison using standard pressure and temperature. We converted results in all other metrics (i.e., 8-hr maximum, 8-hr mean, 1-hr maximum) to the 24-hr mean, with an assumption of a proportional relationship between different metrics. The 8-hr mean, corresponding to the 8-hr average of a specific time period when ozone concentrations are anticipated to be high (e.g., 9am–5pm[11]), was assumed to approximate the 8-hr maximum. We considered multiple conversion ratios of 1-hr maximum:8-hr maximum:24-hr mean ozone as: 1) 2:1.5:1 as previously applied by the U.S. Environmental Protection Agency (EPA),[100] 2) 1.76:1.53:1 from a national study of 78 U.S. communities,[101] and 3) a specific ratio for each community. The actual relationship among ozone metrics differs by community, ozone level, and season.[101] For the third approach, we used community-specific ratios based on data from a previously conducted study of 78 U.S. communities[101] and a database of air pollution concentrations for European communities.[102] For cities not in these databases, a ratio of 1.76:1.53:1 was applied.
Positive findings are more likely to be submitted to or published in a journal than null or negative results,[103] which can result in overestimation in meta-analysis. We investigated publication bias with funnel plots as an asymmetric distribution indicates potential publication bias among the combined estimates.[104] We used the linear regression test developed by Egger et al.[105] to examine publication bias.[106] Based on the Egger’s test results, we applied the “trim and fill” approach[107] to generate overall estimates adjusted for publication bias. We compared meta-analysis results, based on single-city estimates, to multi-city study results, which are less subject to publication bias.
3. Results
We identified 96 articles meeting our protocol. Among these, 86 studies presented only estimates for an individual city; 8 reported only combined estimates across multiple cities;[21,78–83,108] and 2 gave both estimates for an individual city and combined results across cities.[65,109] Results were categorized by age group, type of hospital visit (i.e., general hospital admissions, emergency hospital admissions, and emergency visits), and disease category (e.g., asthma). The most commonly reported disease categories were total or general respiratory diseases, pneumonia, COPD, and asthma.
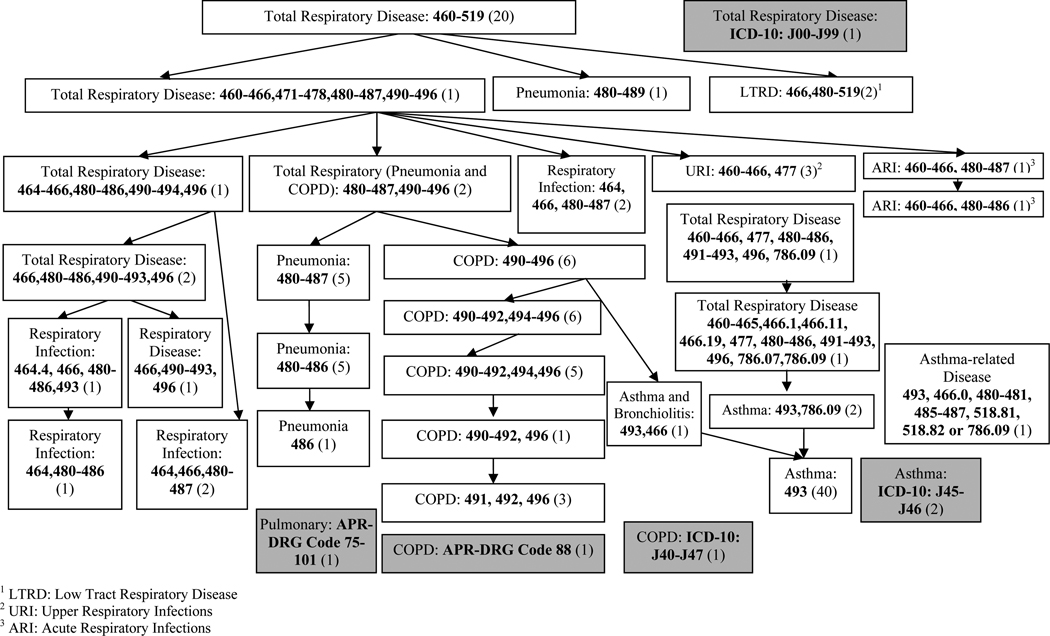
We identified a key challenge in meta-analysis or other synthesis of results in that studies used different diagnostic codes to define a disease (Figure 1). For example, total respiratory disease, respiratory infection, COPD, asthma, and pneumonia were each identified through three or more different sets of ICD codes. For the meta-analysis, we used the descriptions of diseases designated by the authors to categorize estimates by disease, although the somewhat different definitions present a difficulty in comparing across studies.
Figure 1. Disease categories and diagnosis codes in selected studies.
Note: The diagnosis codes in bold are ICD-9 unless specified. Numbers in parentheses indicate how many studies reported estimates for each specified disease category. The white-background boxes show the studies using ICD-9 codes to define disease categories. The gray-background boxes show the studies using other diagnosis codes (e.g. ICD-10 codes, APR-DRG codes). One study can be included in multiple boxes estimates are provided for multiple disease categories.
Within a study, for each individual city we selected one estimate for each hospital visit type (e.g., emergency visits), disease category (e.g., COPD), and age category, and grouped the main estimates by these categories. For cases in which researchers presented more than one such result, we selected the main result identified by the authors. This indicates another challenge in meta-analysis, as the authors’ choice of key result may be subject to publication bias. We generated overall estimates through meta-analysis for data groups with ≥4 estimates.
3.1 Ozone metrics
We used the 24-hr mean as the ozone metric for analysis and converted results in all other ozone metrics to the 24-hr mean. Separate meta-analyses were performed using three methods of converting ozone metrics, yielding similar results (Supplemental Table 1). Note that although 136 estimates were identified in our literature review, a far smaller number are available for a specific cause of hospitalization, age group, and hospital visit type (general, emergency admission, or emergency visit). Compared with the U.S. EPA metric conversion ratio,[100] the study based on U.S. communities[101] had a higher ratio of 8-hr maximum:24-hr average but a smaller value for 1-hr maximum:24-hr average. Results were also influenced by the magnitude of estimates in 8-hr maximum and 1-hr mean metrics. Combined estimates were more likely to be affected by choice of conversion ratio when study-specific central estimates were large.
Although the true relationship among ozone metrics is not constant, our overall results show little influence from the choice of metric conversion method. We applied the ratio from the U.S. study of 78 communities (1.76:1.53:1) for the remaining analyses, as that study was a systematic analysis particularly focused on approaches to converting ozone metrics, and location-specific conversion ratios were not available for all study locations. We also the same ratios to generate results for key findings in the 8-hr maximum ozone metric.
3.2 Summary effects of ozone and respiratory hospitalizations
Table 1 presents meta-analysis results in the form of 24-hr and 8-hr maximum ozone. Most estimates in Table 1 were calculated by the random-effect model, which indicates heterogeneity across studies’ results. We observed associations between ozone and hospitalization or emergency visits for all disease categories: total or general respiratory disease, pneumonia, COPD or asthma. All estimates for a 10ppb increase in the 24-hr ozone were as large as or larger than those for a 10ppb increase in the daily 8-hr maximum ozone, although a 10ppb increase in the 24-hr metric corresponds to approximately a 15ppb increase in the 8-hr maximum metric. All analyses for the elderly showed associations (total respiratory disease, pneumonia, or COPD general hospital admissions; total respiratory disease emergency hospital admissions) with effect estimates ranging from a 2.47% to 4.47% increase in risk per 10ppb 24-hr ozone. Other observed associations were for all ages for COPD (general or emergency hospital admissions) and total respiratory disease (emergency hospital admissions or emergency visits). Results did not indicate associations for total respiratory disease for general hospital admissions for all ages or children, emergency hospital admissions for adults (15–64 years), or emergency visits for children. Associations were observed for asthma for emergency hospital admissions for all ages, and emergency visits for all ages and children. Asthma emergency hospital admissions were not associated with ozone levels for children or adults (15–64 years).
Table 1.
Percentage increase (95% interval) in risk of hospital admissions or emergency visits per 10ppb ozone in 24-hr and 8-hr maximum metrics
| Disease Categories | 24-hr Mean Ozone Metric |
8-hr Max Ozone Metric |
Total # of Estimates |
Studies Included |
|---|---|---|---|---|
| General Hospital Admissions | ||||
| Total RDa (All ages)b | 2.03 (−0.21, 4.31) | 1.45 (−0.04, 2.95) | 6 | [53, 54, 59, 75, 117, 118] |
| Total RD (Elderly) | 2.47 (0.89, 4.07) | 1.60 (0.58, 2.63) | 8 | [9, 10, 52, 54, 85, 118, 119] |
| Total RD (Children) c | 0.69 (−2.03, 3.48) | 0.53 (−1.46, 2.56) | 4 | [53, 54, 59, 72] |
| Pneumonia (Elderly)c | 4.24 (2.85, 5.63) | 2.75 (1.86, 3.64) | 5 | [10, 24, 25, 60, 85] |
| COPD (All ages) | 5.74 (0.71, 10.96) | 4.23 (1.18, 7.36) | 4 | [30, 32, 53, 56, 118] |
| COPD (Elderly)d | 2.54 (1.29, 3.80) | 1.65 (0.84, 2.47) | 8 | [10, 25, 27, 60, 62, 85, 118] |
| Asthma (All ages) | 4.35 (−0.18, 9.10) | 2.83 (−0.12, 5.85) | 6 | [39, 53, 56, 120–122] |
| Asthma (Children) | −0.68 (−6.56, 5.57) | −0.68 (−6.56, 5.57) | 6 | [37, 53, 62, 69, 76, 123] |
| Emergency Hospital Admissions | ||||
| Total RD (All ages) | 1.90 (0.74, 3.07) | 1.24 (0.48, 1.99) | 10 | [5, 6, 11, 15, 19, 57, 74, 77, 124] |
| Total RD (Elderly) | 4.47 (2.48, 6.50) | 2.89 (1.60, 4.21) | 11 | [6, 11, 15, 20, 57, 66, 77, 84, 124] |
| Total RD (15–64 yrs) | 1.06 (−1.31, 3.47) | 0.69 (−0.86, 2.26) | 6 | [6, 11, 57, 84, 124] |
| COPD (All ages) | 5.06 (1.24, 9.05) | 3.29 (0.82, 5.82) | 6 | [15, 16, 29, 84, 125] |
| Asthma (All ages) | 6.64 (2.60, 10.85) | 4.29 (1.69, 6.96) | 8 | [6, 15, 16, 40, 57, 71, 84, 126] |
| Asthma (Children) | 2.83 (−3.45, 9.52) | 1.85 (−2.26, 6.12) | 6 | [6, 40, 43, 57, 71, 124] |
| Asthma (15–64 yrs) | 3.63 (−2.02, 9.60) | 2.46 (−1.41, 6.47) | 6 | [6, 40, 57, 77, 124] |
| Emergency Visits | ||||
| Total RD (All ages) | 1.23 (0.29, 2.17) | 0.80 (0.19, 1.42) | 5 | [17, 23, 127, 128] |
| Total RD (Children) | 2.55 (−1.71, 6.98) | 1.64 (−1.10, 4.48) | 4 | [22, 58, 128] |
| Asthma (All ages) | 4.50 (2.05, 6.99) | 2.90 (1.33, 4.50) | 8 | [38, 41, 42, 127–130] |
| Asthma (Children) | 3.67 (1.55, 5.81) | 2.51 (1.15, 3.88) | 13 | [36, 43, 44, 48, 49, 73, 128, 130–134] |
Note: Bold estimates are statistically significant.
RD = Respiratory Diseases
The combined estimates excluded one outlying study. [135]
Fixed-effect model used. Random-effect model used elsewhere.
Estimates converted in U.S. study ratio and specific ratios were combined in random-effect model, but estimates converted in EPA ratio were combined in fixed-effect model.
Some studies adjusted for PM, using a variety of particle size distributions. Results were generally similar results with and without PM adjustment. In some cases the central effect estimate for O3 was slightly higher with PM adjustment (e.g., [74], [30] for the age group ≥25 years); however, in many cases it was slightly attenuated (e.g., [9,32,37,75]), with results that were originally statistically significant remaining so. In a few cases, some results lost statistical significance with inclusion of PM (e.g., [30] for those <25 years [39], for days <25°C [76]). Effect estimates became statistically significant with inclusion of PM in a few cases (e.g., [77]).
3.3 Age of study subjects
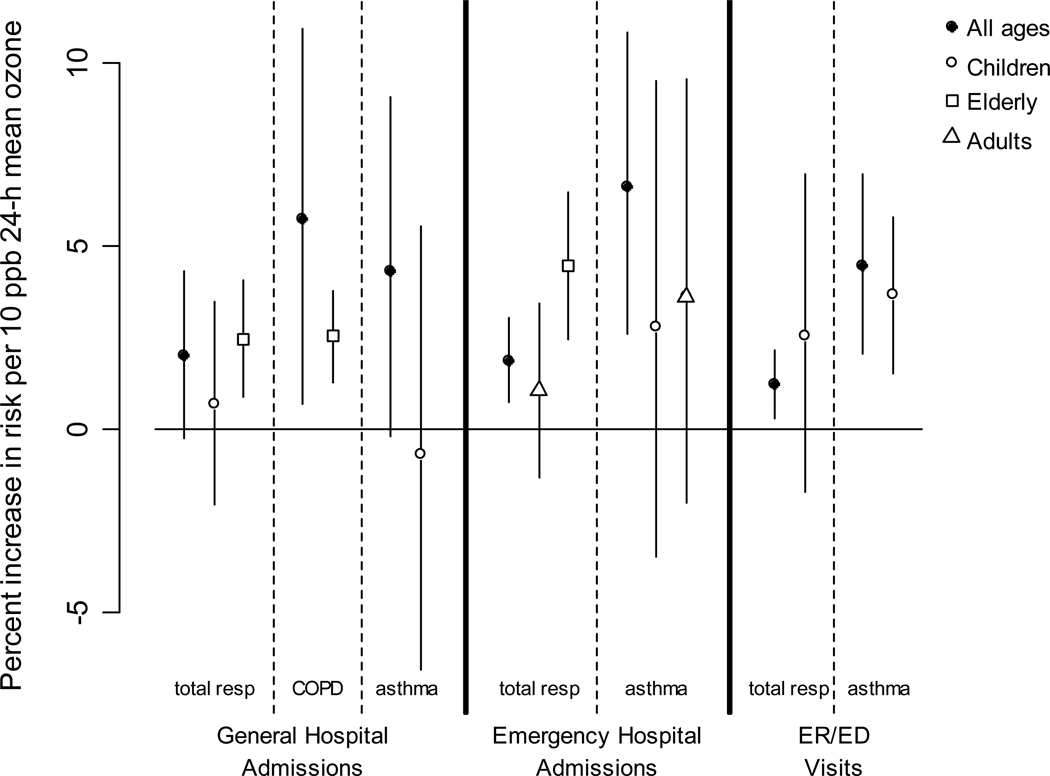
The relationship between ozone and hospital admissions or emergency visits was influenced by the subjects’ age. Figure 2 compares overall effect estimates by age group for total or general respiratory diseases by visit type. Sufficient data were not available to generate overall estimates for all hospital visit types, disease categories, and age groups. Effect estimates were slightly higher for the older age categories, with higher estimates for the elderly than children or adults for general or emergency admissions for total respiratory disease, and with higher estimates for adults than children for emergency hospitalizations for asthma.
Figure 2. Comparison of overall effect estimates for total or general respiratory disease by hospital visit type, disease, and age group.
3.4 Lag of exposure
Studies considered different lag times between exposure and hospitalization. Data were insufficient to calculate overall effects for every lag structure; however, we were able to stratify lag selection for certain disease categories, hospitalization type, and age group combinations. Although effects were similar, effects at lag1 were consistently higher than at lag0 for all comparisons. The increase in risk of hospital admissions for a 10ppb increase in 24-hr ozone for lag1 and lag0 was 2.51% (1.58, 3.45%) compared to 1.95% (1.08, 2.83%) for general hospital COPD admissions for the elderly; 4.14% (−1.50, 10.12%) compared to −4.06% (−11.84, 4.43%) for general hospital asthma admissions for children; and 4.96% (2.05, 7.96%) compared to 2.10% (−1.00, 5.31%) for emergency visits for asthma for children. Central estimates at lag1 and lag0–1 were similar at 2.02% (1.09, 2.93%) compared to 1.88% (0.90, 2.90%) for total or general respiratory disease emergency hospital admissions for the elderly. Central estimates were similar for lag1 and lag0–2 at 4.75% (3.71, 5.81%) compared to 5.15% (1.01, 9.45%) for emergency hospital admissions for asthma for all ages.
3.5 Exposure season
We classified estimates into three seasonal categories: 1) year round; 2) warm season (e.g., April–October, temperature >25°C); and 3) cold season (e.g., November–March, temperature ≤25°C). Studies in tropical or subtropical cities (e.g., Taipei) generally defined warm and cold time periods by temperature because of a lack of distinct seasons. We identified five estimates (4 from Europe, 1 from Hong Kong) with results for all three seasonal categories for the same disease category, hospitalization type and age group, which were total or general respiratory emergency hospital admissions for the elderly. Associations were observed in all seasonal categories. The largest effect of a 3.13% (2.04, 4.23%) increase in risk per 10ppb 24-hr ozone was found for the warm season, while 1.98% (1.17, 2.80%) and 1.67% (0.26, 3.11%) were observed for all-year and the cold season, respectively. For children’s asthma emergency visits the combined estimate for the warm season, 3.11% (1.08, 5.18%), was higher than that of all-year round, 1.08% (3.78, 3.94%).
3.6 Study region
As most studies were conducted in North America, Europe and particular Asian cities (e.g., Hong Kong), we could make only limited comparisons by region. We combined summary estimates for asthma emergency hospital admissions among all ages in Europe and non-European countries separately. The overall estimate for the 4 non-European locations (Canada, Australia, two in Hong Kong) was a 8.89% (3.64, 14.45%) increase in risk per 10ppb 24-hr ozone, compared to 4.04% (−1.74, 10.16%) for the 4 European studies (the Netherlands, Spain, two in the U.K.). U.S. and non-U.S. estimates for children’s asthma ER/ED visits were similar at 2.27% (1.17, 3.38%) based on 6 U.S. studies (Portland, Maine; District of Columbia; state of Maine; St. Louis; two in Atlanta) and 3.55% (−1.14, 8.46%) based on 7 non-U.S. studies (Australia, Ireland, France, Mexico, U.K., two in Canada). Stratifying these cities by North America versus non-North American locations yielded results of 2.64% (1.65, 3.66%) for North American locations compared to 3.06% (−6.36, 13.43%) for non-North American studies. Overall, our analysis indicates potential differences in some effects by region; however, our ability to investigate differences by region was hindered by a lack of studies from numerous locations.
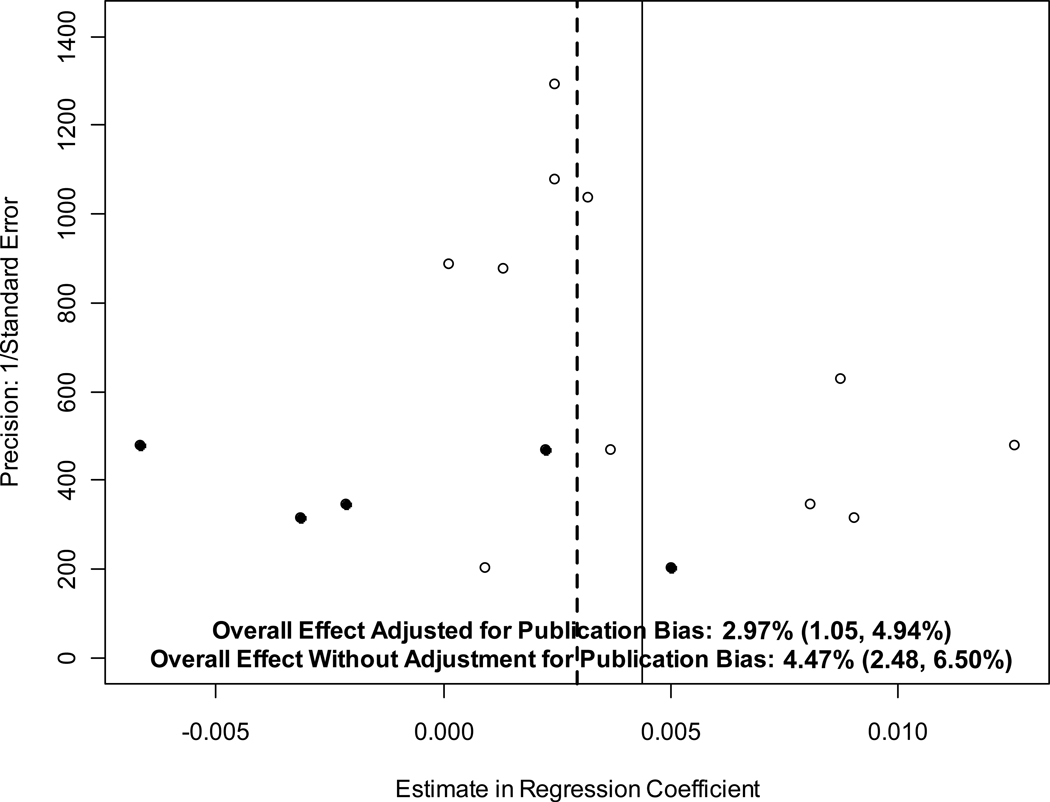
3.7 Publication bias
For the Egger’s linear regression test, a non-zero intercept indicates presence of publication bias. We found that most data groups from Table 1 did not indicate a statistically significant non-zero intercept, indicating lack of evidence for publication bias. Considering the small number of estimates in each data group, we used 0.10 as the significance level, and identified only three data groups with potential indication of publication bias (Table 2). Figure 3 shows an example funnel plot for the association between ozone and emergency hospital admissions for total or general respiratory disease, with and without adjustment for publication bias. If no publication bias occurred, the plot of regression coefficients versus standard error would be approximately symmetrical. The “trim and fill” approach estimates the number and results of hypothetical studies that would, if published, provide a more symmetrical distribution. In Figure 3, open circles represent original studies’ estimates. Filled circles represent hypothetical estimates added by the “trim and fill” method, and mirror a subset of the actual studies (open circles). The solid line reflects the central estimate by meta-analysis random model from the original estimates; the dashed line is the central estimate after the “trim and fill,” which is estimate adjusted for publication bias. The mirror axis is very close to the dashed line and thus not shown.
Table 2.
Percentage increase (95% interval) in risk of hospital admissions or emergency visits per 10ppb 24-hr ozone with and without adjustment for publication bias
| Hospitalization Type |
Disease Category | Age Group |
Total # of Estimates |
Without adjustment for publication bias |
With adjustment for publication bias |
|---|---|---|---|---|---|
| General Hospital Admissions |
Total or General Respiratory Disease |
Elderly | 9 | 2.47 (0.89, 4.07) | 2.26 (0.89, 3.64) |
| Emergency Hospital Admissions |
Total or General Respiratory Disease |
Elderly | 11 | 4.47 (2.48, 6.50) | 2.97 (1.05, 4.94) |
| Emergency Visits |
Total or General Respiratory Disease |
All Ages |
5 | 1.23 (0.29, 2.17) | 1.77 (0.66, 2.88) |
Note: Bold estimates are statistically significant.
Figure 3. Funnel plot of estimates of association between ozone and total or general respiratory disease emergency hospital admissions for the elderly with and without adjustment for publication bias.
Note: Effect estimates show the percentage increase in risk (95% confidence interval) for a 10ppb increase in daily ozone.
Table 2 shows overall results with and without adjustment for publication bias. After adjusting for publication bias, central estimates became smaller and confidence intervals narrowed; however, associations with ozone remained. For all ages total or general respiratory emergency visits, the linear regression test showed an inverse bias as the individual estimates were small or even negative. Thus after adjustment, the central estimate increased slightly.
Several multi-city studies investigated short-term ozone exposure and respiratory hospital admissions or emergency visits. Here we define multi-city studies as those that present an overall estimate across several cities, as opposed to those that only present multiple single-city estimates without an overall estimate. The multi-city study design is less subject to publication bias or between-study variation due to differences in model design, as a uniform framework is applied to all cities separately. Supplemental Table 2 summarizes main results from multi-city studies. We used the same conversion ratio[101] applied in the meta-analysis to convert multi-city estimates to a 24-hr mean metric. Multi-city studies were based in Canada, Australia, Europe, or the U.S. The largest was for 36 U.S. cities.[82]
We compared multi-city estimates to meta-analyses results by hospitalization type, disease category and age group, with close matches to lag selection and exposure season (Table 3). In five of the six comparisons, meta-analysis results exceeded multi-city studies’ estimates, which provides further evidence of publication bias in single-city studies. For general hospital admissions for total or general respiratory disease among the elderly, the estimate from multi-city studies, 2.33% (0.55, 4.13%), was closer to the meta-analysis estimate adjusted for publication bias, 2.26% (0.89, 3.64%), than the unadjusted meta-analysis estimate , 2.47% (0.89, 4.07%).
Table 3.
Percentage increase (95% interval) in risk of hospital admissions or emergency visits per 10ppb 24-hr ozone for meta-analysis and multi-city studies
| Disease | Type of Result | Location | Lag Selection |
Age Group |
Season | Estimate (95% Confidence Interval) |
|---|---|---|---|---|---|---|
| General Hospital Admissions | ||||||
| Total Respiratory Diseases |
Meta-analysis Result[53, 54, 59, 75, 117, 118] |
6 Single Cities from 6 Studies |
Short-term Lags* |
All Ages | All or Warm | 2.03 (−0.21, 4.31) |
| Multi-city Study[81] |
16 Canadian Cities |
Lag1 | All Ages | Warm | 2.50 (1.56, 3.45) | |
| Total Respiratory Diseases |
Meta-analysis Result[9, 10, 52, 54, 85, 118, 119] |
9 Single Cities from 7 Studies |
Short-term Lagsa |
Elderly (65+) |
All or Warm |
2.47, (0.89, 4.07) 2.26 (0.89, 3.64)b |
| Multi-city Study[81] |
16 Canadian Cities |
Lag1 | Elderly (65+) |
Warm | 2.33 (0.55, 4.13) | |
| Asthma | Meta-analysis Result[39, 53, 56, 120–122] |
6 Single Cities from 6 Studies |
Short-term Lagsa |
All Ages | All or Warm | 6.52 (1.38, 11.96) |
| Multi-city Study[83] |
10 Cities in Canada |
Not Specified |
All Ages | All | 2.17 (1.12, 3.22) | |
| Emergency Hospital Admissions | ||||||
| COPD | Meta-analysis Result[15, 16, 29, 84, 125] |
6 Single Cities from 5 Studies |
Short-term Lagsa |
All | All | 5.06 (1.24, 9.05) |
| Multi-city Study[78] |
5 Cities in Europe |
One-day Lag |
All | All | 2.60 (1.32, 3.90) | |
| Asthma | Meta-analysis Result[6, 40, 43, 57, 71, 124] |
6 Cities from 6 Studies |
Short-term Lagsa |
Children | All | 2.83 (−3.45, 9.52) |
| Multi-city Study[79] |
4 Cities in Europe |
Lag0 or Lag1 |
Children | All | −0.77 (−4.14, 2.71) | |
Note: Bold estimates are statistically significant.
Multiple short-term lags in different studies.
Adjusted for publication bias.
4. Discussion
Several studies applied meta-analytical approaches to ozone and mortality.[88–90] To our knowledge, no previous meta-analysis examined short-term ozone exposure and respiratory hospitalizations. Although multi-city studies have been conducted, our research aims to incorporate the value of previously conducted work by synthesizing evidence from single-city studies and investigating heterogeneity among study results.
We found that effects were similar by season, but higher for warm periods than year-round estimates, which were higher than cold season estimates. Individuals may have more outdoor activities in warm periods, resulting in higher exposure. Ozone’s impact on respiratory morbidity may be non-linear with different relative effects depending on ozone levels, which vary by season.[86] For instance, a U-shape relationship was reported for ozone and hospital admissions.[110,111] A threshold effect, with no or little effect at low levels, would result in different effects by season. One study found evidence of a threshold of ∼40–50ppb for 8-hr maximum ozone and hospitalizations.[11] However, others found increased risk of hospitalizations at 8-hr maximum ozone <50ppb, and the shape of the concentration-response function based on quintiles of ozone concentration did not suggest a threshold.[6] Few studies considered a non-linear relationship between ozone and hospitalizations, although lack of a threshold was observed for ozone and mortality.[112] Interaction with or confounding by temporally varying factors such as weather and co-pollutants could also result in different effects by season.
A meta-analysis of ozone and mortality found that the overall result from studies reporting a single lag was higher than the overall result from studies providing estimates from multiple lags,[90] implying that studies were more likely to report the lag with the largest effect. We were unable to explore lag structures in this manner due to data availability; however, we examined publication bias in other ways. Although funnel plot results for some groups of estimates have an asymmetrically distributed shape, suggestive of publication bias, the Egger’s linear regression test provides evidence of publication bias for only a few groups of estimates. Our results may be affected by the small number of estimates in data groups. Combined results from meta-analysis of single-city estimates were generally larger than corresponding results from multi-city analysis, and the difference between single-city and multi-city results narrowed after meta-analysis results were adjusted for publication bias. The discrepancy between the two types of results further suggests publication bias.
Our analysis revealed challenges in comparing across studies, in addition to publication bias. Many factors that could lead to heterogeneity across results were unreported or difficult to capture due to a small number of effect estimates, such as regional differences. Our protocol identified studies published over a time frame of almost 20 years. Associations between ozone and hospitalizations may have changed over this timeframe, such as from changes in socioeconomic factors, and these temporal trends may vary by region. For example, prevalence of residential air conditioning, which affects exposure, has a diverse geographic distribution, is related to socioeconomic status, and is increasing.[113] Several studies demonstrated that air conditioning prevalence can modify health effect estimates for ozone.[82,114,115]
Our ability to fully analyze differences by lag selection was limited as many studies did not report results of all lag structures. Studies tend to report results for the lag(s) with the most statistically significant result, which may bias estimates upward.[116] However, if associations are observed in a multiple-day lag selection but not in a single-day lag selection, studies investigating single-day lag(s) might underestimate the effect.[89]
Researchers applied different classifications of disease categories, even for identically worded categories (e.g., “pneumonia”). To generate overall estimates, we combined similar disease categories, although the actual diagnosis code(s) used in previous studies varied. Researchers also used different ozone metrics, thus results must be converted to a common metric for comparison, although the actual relationship among ozone metrics differs even within a community.[101] However, we found little difference among overall meta-analysis results based on the conversion ratio applied.
In summary, we found associations between short-term ozone exposure and respiratory hospital admissions or emergency visits for several disease categories, although estimates were sensitive to study characteristics and suggest publication bias for some data groups. Based on our analysis of previously conducted studies, we encourage application of the same or similar approaches to future analyses to aid comparison across results. As an example, researchers using different categorizations of disease categories could perform sensitivity analysis with diagnostic codes consistent with earlier work. Authors could report results from all lags used to avoid publication bias. The ability to compare and synthesize results across studies is important for regulatory agencies, such as the U.S. EPA and World Health Organization, that periodically review scientific evidence on how air pollution affects human health and establish regulations and guidelines accordingly. Our findings that suggest publication bias in single-city estimates indicate that the use of multi-city studies may be particularly useful to provide evidence for policy decisions, although an overall assessment of scientific evidence also should consider single-city studies, especially as locally important factors, such as differences in population vulnerability, may play a role in how ozone affects health.
Supplementary Material
Acknowledgements
Funding was provided by the Yale University Carpenter Sperry Award, the Yale F&ES Summer 2008 Globalization Internships and Research Fund, the U.S. Environmental Protection Agency STAR award (EPA R833665), and the National Institutes of Health (NIH) Outstanding New Environmental Scientist (ONES) Award (R01 ES 015028-02).
References
- 1.Yassi A, et al. Basic Environmental Health. New York: Oxford University Press; 2001. [Google Scholar]
- 2.Schwela D. Air pollution and health in urban areas. Rev Environ Health. 2000;15(1–2):13–42. doi: 10.1515/reveh.2000.15.1-2.13. [DOI] [PubMed] [Google Scholar]
- 3.Lippmann M. Health effects of tropospheric ozone: review of recent research findings and their implications to ambient air quality standards. J Expo Anal Environ Epidemiol. 1993;3(1):103–129. [PubMed] [Google Scholar]
- 4.Gourveia N, Fletcher T. Respiratory diseases in chidren and outdoor air pollution in San Paulo, Brazil: a time series analysis. Occup. Environ. Med. 2000;57:477–483. doi: 10.1136/oem.57.7.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gwynn RC, Burnett RT, Thurston GD. A time-series analysis of acidic particulate matter and daily mortality and morbidity in the Buffalo, New York region. Environ Health Perspect. 2000;108(2):125–133. doi: 10.1289/ehp.00108125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petroeschevsky A, et al. Associations between outdoor air pollution and hospital admissions in Brisbane, Australia. Arch Environ Health. 2001;56(1):37–52. doi: 10.1080/00039890109604053. [DOI] [PubMed] [Google Scholar]
- 7.Martins LC, et al. Air pollution and emergency room visits due to chronic lower respiratory diseases in the elderly: an ecological time-series study in Sao Paulo, Brazil. J Occup Environ Med. 2002;44(7):622–627. doi: 10.1097/00043764-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Burnett RT, et al. Effects of low ambient levels of ozone and sulfates on the frequency of respiratory admissions to Ontario hospitals. Environ Res. 1994;65(2):172–194. doi: 10.1006/enrs.1994.1030. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz J. Short term fluctuations in air pollution and hospital admissions of the elderly for respiratory disease. Thorax. 1995;50(5):531–538. doi: 10.1136/thx.50.5.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwartz J. Air pollution and hospital admissions for respiratory disease. Epidemiology. 1996;7(1):20–28. doi: 10.1097/00001648-199601000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Ponce de Leon A, et al. Effects of air pollution on daily hospital admissions for respiratory disease in London between 1987–88 and 1991–92. J Epidemiol Community Health. 1996;50 Suppl_1:s63–s70. doi: 10.1136/jech.50.suppl_1.s63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Delfino RJ, et al. Effects of air pollution on emergency room visits for respiratory illnesses in Montreal, Quebec. Am J Respir Crit Care Med. 1997;155(2):568–576. doi: 10.1164/ajrccm.155.2.9032196. [DOI] [PubMed] [Google Scholar]
- 13.Delfino RJ, Murphy-Moulton AM, Becklake MR. Emergency room visits for respiratory illnesses among the elderly in Montreal: association with low level ozone exposure. Environ Res. 1998;76(2):67–77. doi: 10.1006/enrs.1997.3794. [DOI] [PubMed] [Google Scholar]
- 14.Cakmak S, Burnett R, Krewski D. Adjusting for temporal variation in the analysis of parallel time series of health and environmental variables. J Expo Anal Environ Epidemiol. 1998;8(2):129–144. [PubMed] [Google Scholar]
- 15.Wong TW, et al. Air pollution and hospital admissions for respiratory and cardiovascular diseases in Hong Kong. Occup Environ Med. 1999;56(10):679–683. doi: 10.1136/oem.56.10.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burnett RT, et al. Effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Arch Environ Health. 1999;54(2):130–139. doi: 10.1080/00039899909602248. [DOI] [PubMed] [Google Scholar]
- 17.Stieb DM, et al. Air pollution, aeroallergens and cardiorespiratory emergency department visits in Saint John, Canada. J Expo Anal Environ Epidemiol. 2000;10(5):461–477. doi: 10.1038/sj.jea.7500112. [DOI] [PubMed] [Google Scholar]
- 18.Burnett RT, et al. Association between ozone and hospitalization for acute respiratory diseases in children less than 2 years of age. Am J Epidemiol. 2001;153(5):444–452. doi: 10.1093/aje/153.5.444. [DOI] [PubMed] [Google Scholar]
- 19.Oftedal B, et al. Traffic related air pollution and acute hospital admission for respiratory diseases in Drammen, Norway 1995–2000. Eur J Epidemiol. 2003;18(7):671–675. doi: 10.1023/a:1024884502114. [DOI] [PubMed] [Google Scholar]
- 20.Yang Q, et al. Association between ozone and respiratory admissions among children and the elderly in Vancouver, Canada. Inhal Toxicol. 2003;15(13):1297–1308. doi: 10.1080/08958370390241768. [DOI] [PubMed] [Google Scholar]
- 21.Dales RE, Cakmak S, Doiron MS. Gaseous air pollutants and hospitalization for respiratory disease in the neonatal period. Environ Health Perspect. 2006;114(11):1751–1754. doi: 10.1289/ehp.9044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin CA, et al. Air pollution and respiratory illness of children in Sao Paulo, Brazil. Paediatr Perinat Epidemiol. 1999;13(4):475–488. doi: 10.1046/j.1365-3016.1999.00210.x. [DOI] [PubMed] [Google Scholar]
- 23.Tolbert PE, et al. Multipollutant modeling issues in a study of ambient air quality and emergency department visits in Atlanta. J Expo Sci Environ Epidemiol. 2007;17 Suppl 2:s29–s35. doi: 10.1038/sj.jes.7500625. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz J. PM10, ozone, and hospital admissions for the elderly in Minneapolis-St. Paul, Minnesota. Arch Environ Health. 1994;49(5):366–374. doi: 10.1080/00039896.1994.9954989. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz J. Air pollution and hospital admissions for the elderly in Detroit, Michigan. Am J Respir Crit Care Med. 1994;150(3):648–655. doi: 10.1164/ajrccm.150.3.8087333. [DOI] [PubMed] [Google Scholar]
- 26.Farhat SC, et al. Effect of air pollution on pediatric respiratory emergency room visits and hospital admissions. Braz J Med Biol Res. 2005;38(2):227–235. doi: 10.1590/s0100-879x2005000200011. [DOI] [PubMed] [Google Scholar]
- 27.Moolgavkar SH. Air pollution and hospital admissions for chronic obstructive pulmonary disease in three metropolitan areas in the United States. Inhal Toxicol. 2000;12 Suppl 4:75–90. doi: 10.1080/089583700750019512. [DOI] [PubMed] [Google Scholar]
- 28.Erbas B, Hyndman RJ. Sensitivity of the estimated air pollution-respiratory admissions relationship to statistical model choice. Int J Environ Health Res. 2005;15(6):437–448. doi: 10.1080/09603120500289192. [DOI] [PubMed] [Google Scholar]
- 29.Ko FW, et al. Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong. Thorax. 2007;62(9):780–785. doi: 10.1136/thx.2006.076166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee IM, et al. Air pollution and hospital admissions for chronic obstructive pulmonary disease in a tropical city: Kaohsiung, Taiwan. Inhal Toxicol. 2007;19(5):393–398. doi: 10.1080/08958370601174818. [DOI] [PubMed] [Google Scholar]
- 31.Tolbert PE, et al. Interim results of the study of particulates and health in Atlanta (SOPHIA) J Expo Anal Environ Epidemiol. 2000;10(5):446–460. doi: 10.1038/sj.jea.7500106. [DOI] [PubMed] [Google Scholar]
- 32.Yang CY, Chen CJ. Air pollution and hospital admissions for chronic obstructive pulmonary disease in a subtropical city: Taipei, Taiwan. J Toxicol Environ Health A. 2007;70(14):1214–1219. doi: 10.1080/15287390701380880. [DOI] [PubMed] [Google Scholar]
- 33.Stieb DM, et al. Association between ozone and asthma emergency department visits in Saint John, New Brunswick, Canada. Environ Health Perspect. 1996;104(12):1354–1360. doi: 10.1289/ehp.961041354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sheppard L, et al. Effects of ambient air pollution on nonelderly asthma hospital admissions in Seattle, Washington, 1987–1994. Epidemiology. 1999;10(1):23–30. [PubMed] [Google Scholar]
- 35.Tobias A, Campbell MJ, Saez M. Modelling asthma epidemics on the relationship between air pollution and asthma emergency visits in Barcelona, Spain. Eur J Epidemiol. 1999;15(9):799–803. doi: 10.1023/a:1007657810096. [DOI] [PubMed] [Google Scholar]
- 36.Fauroux B, et al. Ozone: a trigger for hospital pediatric asthma emergency room visits. Pediatr Pulmonol. 2000;30(1):41–46. doi: 10.1002/1099-0496(200007)30:1<41::aid-ppul7>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 37.Lee J-T, et al. Air pollution and asthma among children in Seoul, Korea. Epidemiology. 2002;13(4):481–484. doi: 10.1097/00001648-200207000-00018. [DOI] [PubMed] [Google Scholar]
- 38.Galan I, et al. Short-term effects of air pollution on daily asthma emergency room admissions. Eur Respir J. 2003;22(5):802–808. doi: 10.1183/09031936.03.00013003. [DOI] [PubMed] [Google Scholar]
- 39.Tsai SS, et al. Air pollution and hospital admissions for asthma in a tropical city: Kaohsiung, Taiwan. Inhal Toxicol. 2006;18(8):549–554. doi: 10.1080/08958370600686176. [DOI] [PubMed] [Google Scholar]
- 40.Ko FW, et al. Effects of air pollution on asthma hospitalization rates in different age groups in Hong Kong. Clin Exp Allergy. 2007;37(9):1312–1319. doi: 10.1111/j.1365-2222.2007.02791.x. [DOI] [PubMed] [Google Scholar]
- 41.Kim SY, et al. Air pollution, socioeconomic position, and emergency hospital visits for asthma in Seoul, Korea. Int Arch Occup Environ Health. 2007;80(8):701–710. doi: 10.1007/s00420-007-0182-3. [DOI] [PubMed] [Google Scholar]
- 42.Villeneuve PJ, et al. Outdoor air pollution and emergency department visits for asthma among children and adults: a case-crossover study in northern Alberta, Canada. Environ Health. 2007;6:40. doi: 10.1186/1476-069X-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Babin SM, et al. Pediatric patient asthma-related emergency department visits and admissions in Washington, DC, from 2001–2004, and associations with air quality, socio-economic status and age group. Environ Health. 2007;6:9. doi: 10.1186/1476-069X-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Romieu I, et al. Effects of urban air pollutants on emergency visits for childhood asthma in Mexico City. Am J Epidemiol. 1995;141(6):546–553. doi: 10.1093/oxfordjournals.aje.a117470. [DOI] [PubMed] [Google Scholar]
- 45.Tenias JM, Ballester F, Rivera ML. Association between hospital emergency visits for asthma and air pollution in Valencia, Spain. Occup Environ Med. 1998;55(8):541–547. doi: 10.1136/oem.55.8.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cassino C, et al. Cigarette smoking and ozone-associated emergency department use for asthma by adults in New York City. Am J Respir Crit Care Med. 1999;159(6):1773–1779. doi: 10.1164/ajrccm.159.6.9809042. [DOI] [PubMed] [Google Scholar]
- 47.Carlin BP, Xia H. Assessing environmental justice using Bayesian hierarchical models: two case studies. J Expo Anal Environ Epidemiol. 1999;9(1):66–78. doi: 10.1038/sj.jea.7500027. [DOI] [PubMed] [Google Scholar]
- 48.Tolbert PE, et al. Air quality and pediatric emergency room visits for asthma in Atlanta, Georgia, USA. Am J Epidemiol. 2000;151(8):798–810. doi: 10.1093/oxfordjournals.aje.a010280. [DOI] [PubMed] [Google Scholar]
- 49.Szyszkowicz M. Ambient air pollution and daily emergency department visits for asthma in Edmonton, Canada. Int J Occup Med Environ Health. 2008;21(1):25–30. doi: 10.2478/v10001-008-0002-3. [DOI] [PubMed] [Google Scholar]
- 50.Paulu C, Smith AE. Tracking associations between ambient ozone and asthma-related emergency department visits using case-crossover analysis. J Public Health Manag Pract. 2008;14(6):581–591. doi: 10.1097/01.PHH.0000338371.53242.0e. [DOI] [PubMed] [Google Scholar]
- 51.Delfino RJ, Becklake MR, Hanley JA. The relationship of urgent hospital admissions for respiratory illnesses to photochemical air pollution levels in Montreal. Environ Res. 1994;67(1):1–19. doi: 10.1006/enrs.1994.1061. [DOI] [PubMed] [Google Scholar]
- 52.Fung KY, et al. Association between Air Pollution and Multiple Respiratory Hospitalizations among the Elderly in Vancouver, Canada. Inhalation Toxicology. 2006;18(13):1005–1011. doi: 10.1080/08958370600904538. [DOI] [PubMed] [Google Scholar]
- 53.Fusco D, et al. Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur Respir J. 2001;17(6):1143–1150. doi: 10.1183/09031936.01.00005501. [DOI] [PubMed] [Google Scholar]
- 54.Luginaah IN, et al. Association of ambient air pollution with respiratory hospitalization in a government-designated "area of concern": the case of Windsor, Ontario. Environ Health Perspect. 2005;113(3):290–296. doi: 10.1289/ehp.7300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lin M, Stieb DM, Chen Y. Coarse Particulate Matter and Hospitalization for Respiratory Infections in Children Younger Than 15 Years in Toronto: A Case-Crossover Analysis. Pediatrics. 2005;116(2):e235–e240. doi: 10.1542/peds.2004-2012. [DOI] [PubMed] [Google Scholar]
- 56.Dab W, et al. Short term respiratory health effects of ambient air pollution: results of the APHEA project in Paris. J Epedimiol Community Health. 1996;50 Suppl 1:s42–s46. doi: 10.1136/jech.50.suppl_1.s42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Atkinson RW, et al. Short-term associations between emergency hospital admissions for respiratory and cardiovascular disease and outdoor air pollution in London. Arch Environ Health. 1999;54(6):398–411. doi: 10.1080/00039899909603371. [DOI] [PubMed] [Google Scholar]
- 58.Ilabaca M, et al. Association between levels of fine particulate and emergency visits for pneumonia and other respiratory illnesses among children in Santiago, Chile. J Air Waste Manag Assoc. 1999;49:154–163. doi: 10.1080/10473289.1999.10463879. (9 Spec No) [DOI] [PubMed] [Google Scholar]
- 59.Middleton N, et al. A 10-year time-series analysis of respiratory and cardiovascular morbidity in Nicosia, Cyprus: the effect of short-term changes in air pollution and dust storms. Environ Health. 2008;7:39. doi: 10.1186/1476-069X-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schwartz J. Air pollution and hospital admissions for the elderly in Birmingham, Alabama. Am J Epidemiol. 1994;139(6):589–598. doi: 10.1093/oxfordjournals.aje.a117048. [DOI] [PubMed] [Google Scholar]
- 61.Castellsague J, et al. Short-term association between air pollution and emergency room visits for asthma in Barcelona. Thorax. 1995;50(10):1051–1056. doi: 10.1136/thx.50.10.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Morgan G, Corbett S, Wlodarczyk J. Air pollution and hospital admissions in Sydney, Australia, 1990 to 1994. Am J Public Health. 1998;88(12):1761–1766. doi: 10.2105/ajph.88.12.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nauenberg E, Basu K. Effect of insurance coverage on the relationship between asthma hospitalizations and exposure to air pollution. Public Health Rep. 1999;114(2):135–148. [PMC free article] [PubMed] [Google Scholar]
- 64.Linn WS, et al. Air pollution and daily hospital admissions in metropolitan Los Angeles. Environ Health Perspect. 2000;108(5):427–434. doi: 10.1289/ehp.00108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jaffe DH, Singer ME, Rimm AA. Air pollution and emergency department visits for asthma among Ohio Medicaid recipients, 1991–1996. Environ Res. 2003;91(1):21–28. doi: 10.1016/s0013-9351(02)00004-x. [DOI] [PubMed] [Google Scholar]
- 66.Prescott GJ, et al. Urban air pollution and cardiopulmonary ill health: a 14.5 year time series study. Occup Environ Med. 1998;55(10):697–704. doi: 10.1136/oem.55.10.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Voigt T, Bailey M, Abramson M. Air pollution in the Latrobe Valley and its impact upon respiratory morbidity. Aust N Z J Public Health. 1998;22(5):556–561. doi: 10.1111/j.1467-842x.1998.tb01438.x. [DOI] [PubMed] [Google Scholar]
- 68.Dales RE, et al. Influence of ambient fungal spores on emergency visits for asthma to a regional children's hospital. Am J Respir Crit Care Med. 2000;162(6):2087–2090. doi: 10.1164/ajrccm.162.6.2001020. [DOI] [PubMed] [Google Scholar]
- 69.Lin M, et al. Gaseous air pollutants and asthma hospitalization of children with low household income in Vancouver, British Columbia, Canada. Am J Epidemiol. 2004;159(3):294–303. doi: 10.1093/aje/kwh043. [DOI] [PubMed] [Google Scholar]
- 70.Yang Q, et al. Effect of short-term exposure to low levels of gaseous pollutants on chronic obstructive pulmonary disease hospitalizations. Environ Res. 2005;99(1):99–105. doi: 10.1016/j.envres.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 71.Anderson HR, et al. Air pollution, pollens, and daily admissions for asthma in London 1987–92. Thorax. 1998;53(10):842–848. doi: 10.1136/thx.53.10.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Braga AL, et al. Health effects of air pollution exposure on children and adolescents in Sao Paulo, Brazil. Pediatr Pulmonol. 2001;31(2):106–113. doi: 10.1002/1099-0496(200102)31:2<106::aid-ppul1017>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 73.Mohr LB, et al. Influence of season and temperature on the relationship of elemental carbon air pollution to pediatric asthma emergency room visits. J Asthma. 2008;45(10):936–943. doi: 10.1080/02770900802404082. [DOI] [PubMed] [Google Scholar]
- 74.Gwynn RC, Thurston GD. The burden of air pollution: impacts among racial minorities. Environ Health Perspect. 2001;109 Suppl 4:501–506. doi: 10.1289/ehp.01109s4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Burnett RT, et al. The role of particulate size and chemistry in the association between summertime ambient air pollution and hospitalization for cardiorespiratory diseases. Environ Health Perspect. 1997;105(6):614–620. doi: 10.1289/ehp.97105614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee SL, Wong WH, Lau WL. Association between air pollution and asthma admission among children in Hong Kong. Clin Exp Allergy. 2006;36(9):1138–1146. doi: 10.1111/j.1365-2222.2006.02555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wong CM, et al. A tale of two cities: effects of air pollution on hospital admissions in Hong Kong and London compared. Environ Health Perspect. 2002;110(1):67–77. doi: 10.1289/ehp.0211067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Anderson HR, et al. Air pollution and daily admissions for chronic obstructive pulmonary disease in 6 European cities: results from the APHEA project. Eur Respir J. 1997;10(5):1064–1071. doi: 10.1183/09031936.97.10051064. [DOI] [PubMed] [Google Scholar]
- 79.Sunyer J, et al. Urban air pollution and emergency admissions for asthma in four European cities: the APHEA Project. Thorax. 1997;52(9):760–765. doi: 10.1136/thx.52.9.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Spix C, et al. Short-term effects of air pollution on hospital admissions of respiratory diseases in Europe: a quantitative summary of APHEA study results. Air Pollution and Health: a European Approach. Arch Environ Health. 1998;53(1):54–64. doi: 10.1080/00039899809605689. [DOI] [PubMed] [Google Scholar]
- 81.Burnett RT, et al. Association between ozone and hospitalization for respiratory diseases in 16 Canadian cities. Environ Res. 1997;72(1):24–31. doi: 10.1006/enrs.1996.3685. [DOI] [PubMed] [Google Scholar]
- 82.Medina-Ramon M, Zanobetti A, Schwartz J. The effect of ozone and PM10 on hospital admissions for pneumonia and chronic obstructive pulmonary disease: a national multicity study. Am J Epidemiol. 2006;163(6):579–588. doi: 10.1093/aje/kwj078. [DOI] [PubMed] [Google Scholar]
- 83.Cakmak S, Dales RE, Judek S. Respiratory health effects of air pollution gases: modification by education and income. Arch Environ Occup Health. 2006;61(1):5–10. doi: 10.3200/AEOH.61.1.5-10. [DOI] [PubMed] [Google Scholar]
- 84.Schouten JP, Vonk JM, de Graaf A. Short term effects of air pollution on emergency hospital admissions for respiratory disease: results of the APHEA project in two major cities in The Netherlands, 1977–89. J Epidemiol Community Health. 1996;50 Suppl_1:s22–s29. doi: 10.1136/jech.50.suppl_1.s22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Moolgavkar SH, Luebeck EG, Anderson EL. Air pollution and hospital admissions for respiratory causes in Minneapolis-St. Paul and Birmingham. Epidemiology. 1997;8(4):364–370. doi: 10.1097/00001648-199707000-00003. [DOI] [PubMed] [Google Scholar]
- 86.Logan JA. Tropospheric ozone: seasonal behavior, trends, and anthropogenic influence. J Geophys Res. 1985;90(D6):10. 463–10,482. [Google Scholar]
- 87.Wong CW, et al. A tale of two cities: effects of air pollution on hospital admission in Hong Kong and London compared. Environ. Health Perspect. 2002;110:67–77. doi: 10.1289/ehp.0211067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Levy JI, Chemerynski SM, Sarnat JA. Ozone exposure and mortality: an empiric Bayes metaregression analysis. Epidemiology. 2005;16(4):458–468. doi: 10.1097/01.ede.0000165820.08301.b3. [DOI] [PubMed] [Google Scholar]
- 89.Ito K, De Leon SF, Lippmann M. Associations between ozone and daily mortality: analysis and meta-analysis. Epidemiology. 2005;16(4):446–457. doi: 10.1097/01.ede.0000165821.90114.7f. [DOI] [PubMed] [Google Scholar]
- 90.Bell ML, Dominici F, Samet JM. A meta-analysis of time-series studies of ozone and mortality with comparison to the National Morbidity, Mortality, and Air Pollution Study. Epidemiology. 2005;16(4):436–445. doi: 10.1097/01.ede.0000165817.40152.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tseng RY, Li CK, Spinks JA. Particulate air pollution and hospitalization for asthma. Ann Allergy. 1992;68(5):425–432. [PubMed] [Google Scholar]
- 92.Thurston GD, et al. Respiratory hospital admissions and summertime haze air pollution in Toronto, Ontario: consideration of the role of acid aerosols. Environ Res. 1994;65(2):271–290. doi: 10.1006/enrs.1994.1037. [DOI] [PubMed] [Google Scholar]
- 93.Burnett RT, et al. Associations between ambient particulate sulfate and admissions to Ontario hospitals for cardiac and respiratory diseases. Am J Epidemiol. 1995;142(1):15–22. doi: 10.1093/oxfordjournals.aje.a117540. [DOI] [PubMed] [Google Scholar]
- 94.Jones GN, et al. Ozone level effect on respiratory illness: an investigation of emergency department visits. South Med J. 1995;88(10):1049–1056. doi: 10.1097/00007611-199510000-00010. [DOI] [PubMed] [Google Scholar]
- 95.Weisel CP, Cody RP, Lioy PJ. Relationship between summertime ambient ozone levels and emergency department visits for asthma in central New Jersey. Environ Health Perspect. 1995;103 Suppl 2:97–102. doi: 10.1289/ehp.95103s297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hernandez-Garduno E, et al. Air pollution and respiratory health in Mexico City. J Occup Environ Med. 1997;39(4):299–307. doi: 10.1097/00043764-199704000-00006. [DOI] [PubMed] [Google Scholar]
- 97.Tobias A, et al. Sensitivity analysis of common statistical models used to study the short-term effects of air pollution on health. Int J Biometeorol. 2003;47(4):227–229. doi: 10.1007/s00484-003-0163-5. [DOI] [PubMed] [Google Scholar]
- 98.Ponka A, Virtanen M. Chronic bronchitis, emphysema, and low-level air pollution in Helsinki, 1987–1989. Environ Res. 1994;65(2):207–217. doi: 10.1006/enrs.1994.1032. [DOI] [PubMed] [Google Scholar]
- 99.Sutton AJ, et al. Wiley Series in Probability and Statistics - Applied Probability and Statistics Section. John Wiley & Sons, Ltd; 2000. Methods for meta-analysis in medical research. [Google Scholar]
- 100.U.S. EPA U.S.E.P. Agency, Editor. Air Quality Criteria for Ozone and Related Photochemical Oxidants (2006 Final) Washington DC: 2006. [Google Scholar]
- 101.Anderson G, Bell M. Does one size fit all? The suitability of standard ozone exposure metric conversion ratios and implications for epidemiology. J Exp Sci Environ Epidemiol. 2008 doi: 10.1038/jes.2008.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.European Environmental Agency. AirBase: The European Air Quality Database. http://www.eea.europa.eu/themes/air/airbase.
- 103.Easterbrook P, et al. Publication bias in clinical research. Lancet. 1991;337(8746):867–872. doi: 10.1016/0140-6736(91)90201-y. [DOI] [PubMed] [Google Scholar]
- 104.Light RJ, Pillemer DB. Summing Up: The Science of Reviewing Research. Cambridge, MA: Harvard University Press; 1984. p. 191. [Google Scholar]
- 105.Egger M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sterne JAC, Gavaghan D, Egger M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J Clinical Epidemiol. 2000;53(11):1119–1129. doi: 10.1016/s0895-4356(00)00242-0. [DOI] [PubMed] [Google Scholar]
- 107.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 108.Simpson R, et al. The short-term effects of air pollution on hospital admissions in four Australian cities. Aust N Z J Public Health. 2005;29(3):213–221. [PubMed] [Google Scholar]
- 109.Lin S, et al. Ambient ozone concentration and hospital admissions due to childhood respiratory diseases in New York State, 1991–2001. Environ Res. 2008;108(1):42–47. doi: 10.1016/j.envres.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 110.Buchdahl R, et al. Association between air pollution and acute childhood wheezy episodes: prospective observational study. BMJ. 1996;312(7032):661–665. doi: 10.1136/bmj.312.7032.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Buchdahl R, et al. Associations between ambient ozone, hydrocarbons, and childhood wheezy episodes: a prospective observational study in south east London. Occup Environ Med. 2000;57(2):86–93. doi: 10.1136/oem.57.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bell ML, Peng RD, Dominici F. The exposure-response curve for ozone and risk of mortality and the adequacy of current ozone regulations. Environ Health Perspect. 2006;114(4):532–536. doi: 10.1289/ehp.8816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kinney PL, et al. Approaches for estimating effects of climate change on heat-related deaths: challenges and opportunities. Environ Sci Policy. 2008;11:87–96. [Google Scholar]
- 114.Medina-Ramón M, Schwartz J. Who is more vulnerable to die from ozone air pollution? Epidemiology. 2008;19(5):672–679. doi: 10.1097/EDE.0b013e3181773476. [DOI] [PubMed] [Google Scholar]
- 115.Bell ML, Dominici F. Effect Modification by Community Characteristics on the Short-term Effects of Ozone Exposure and Mortality in 98 US Communities. Am J Epidemiol. 2008;167(8):986–997. doi: 10.1093/aje/kwm396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lumley T, Sheppard L. Assessing seasonal confounding and model selection bias in air pollution epidemiology using positive and negative control analyses. Environmetrics. 2000;11(6):705–717. [Google Scholar]
- 117.Hagen JA, et al. Associations between Outdoor Air Pollutants and Hospitalization for Respiratory Diseases. Epidemiology. 2000;11(2):136–140. doi: 10.1097/00001648-200003000-00009. [DOI] [PubMed] [Google Scholar]
- 118.Wong CM, et al. Modification by influenza on health effects of air pollution in Hong Kong. Environ Health Perspect. 2009;117(2):248–253. doi: 10.1289/ehp.11605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Schwartz J, et al. Methodological issues in studies of air pollution and daily counts of deaths or hospital admissions. J Epidemiol Community Health. 1996;50 Suppl 1:S3–S11. doi: 10.1136/jech.50.suppl_1.s3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yang CY, et al. Air pollution and hospital admissions for asthma in a subtropical city: Taipei, Taiwan. J Toxicol Environ Health A. 2007;70(2):111–117. doi: 10.1080/15287390600755059. [DOI] [PubMed] [Google Scholar]
- 121.Erbas B, et al. Do levels of airborne grass pollen influence asthma hospital admissions? Clin Exp Allergy. 2007;37(11):1641–1647. doi: 10.1111/j.1365-2222.2007.02818.x. [DOI] [PubMed] [Google Scholar]
- 122.Bell ML, Levy JK, Lin Z. The effect of sandstorms and air pollution on cause-specific hospital admissions in Taipei, Taiwan. Occup Environ Med. 2008;65(2):104–111. doi: 10.1136/oem.2006.031500. [DOI] [PubMed] [Google Scholar]
- 123.Lin M, et al. Effect of short-term exposure to gaseous pollution on asthma hospitalisation in children: a bi-directional case-crossover analysis. J Epidemiol Community Health. 2003;57(1):50–55. doi: 10.1136/jech.57.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Anderson HR, et al. Particulate matter and daily mortality and hospital admissions in the west midlands conurbation of the United Kingdom: associations with fine and coarse particles, black smoke and sulphate. Occup Environ Med. 2001;58(8):504–510. doi: 10.1136/oem.58.8.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hinwood AL, et al. The relationship between changes in daily air pollution and hospitalizations in Perth, Australia 1992–1998: a case-crossover study. Int J Environ Health Res. 2006;16(1):27–46. doi: 10.1080/09603120500397680. [DOI] [PubMed] [Google Scholar]
- 126.Tobías A, et al. Sensitivity analysis of common statistical models used to study the short-term effects of air pollution on health. International Journal of Biometeorology. 2003;47(4):227–229. doi: 10.1007/s00484-003-0163-5. [DOI] [PubMed] [Google Scholar]
- 127.Peel JL, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005;16(2):164–174. doi: 10.1097/01.ede.0000152905.42113.db. [DOI] [PubMed] [Google Scholar]
- 128.Wilson AM, et al. Air pollution, weather, and respiratory emergency room visits in two northern New England cities: an ecological time-series study. Environ Res. 2005;97(3):312–321. doi: 10.1016/j.envres.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 129.Boutin-Forzano S, et al. Visits to the emergency room for asthma attacks and short-term variations in air pollution. A case-crossover study. Respiration. 2004;71(2):134–137. doi: 10.1159/000076673. [DOI] [PubMed] [Google Scholar]
- 130.Paulu C, Smith AE. Tracking Associations Between Ambient Ozone and Asthma-Related Emergency Department Visits Using Case-Crossover Analysis. Journal of Public Health Management and Practice. 2008;14(6):581–591. doi: 10.1097/01.PHH.0000338371.53242.0e. 10.1097/01.PHH.0000338371.53242.0e. [DOI] [PubMed] [Google Scholar]
- 131.Carlin BP, Xia H. Assessing Environmental Justice Using Bayesian Hierarchical Models: Two Case Studies. Journal of Exposure Analysis and Environmental Epidemiology. 1999;9:66–78. doi: 10.1038/sj.jea.7500027. [DOI] [PubMed] [Google Scholar]
- 132.Dales RE, et al. Influence of Ambient Fungal Spores on Emergency Visits for Asthma to a Regional Children's Hospital. Am. J. Respir. Crit. Care Med. 2000;162(6):2087–2090. doi: 10.1164/ajrccm.162.6.2001020. [DOI] [PubMed] [Google Scholar]
- 133.Thompson AJ, Shields MD, Patterson CC. Acute asthma exacerbations and air pollutants in children living in Belfast, Northern Ireland. Arch Environ Health. 2001;56(3):234–241. doi: 10.1080/00039890109604447. [DOI] [PubMed] [Google Scholar]
- 134.Erbas B, et al. Air pollution and childhood asthma emergency hospital admissions: estimating intra-city regional variations. Int J Environ Health Res. 2005;15(1):11–20. doi: 10.1080/09603120400018717. [DOI] [PubMed] [Google Scholar]
- 135.Jayaraman G, Nidhi Air pollution and associated respiratory morbidity in Delhi. Health Care Manag Sci. 2008;11(2):132–138. doi: 10.1007/s10729-007-9050-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.