Abstract
Background
Quality of antidepressant treatment remains disturbingly poor. Rates of medication adherence and follow-up contact are especially low in primary care, where most depression treatment begins. Telephone care management programs can address these gaps, but reliance on live contact makes such programs less available, less timely, and more expensive.
Objective
Evaluate the feasibility, acceptability, and effectiveness of a depression care management program delivered by online messaging through an electronic medical record.
Design
Randomized controlled trial comparing usual primary care treatment to primary care supported by online care management
Setting
Nine primary care clinics of an integrated health system in Washington state
Participants
Two hundred and eight patients starting antidepressant treatment for depression.
Intervention
Three online care management contacts with a trained psychiatric nurse. Each contact included a structured assessment (severity of depression, medication adherence, side effects), algorithm-based feedback to the patient and treating physician, and as-needed facilitation of follow-up care. All communication occurred through secure, asynchronous messages within an electronic medical record.
Main Measures
An online survey approximately five months after randomization assessed the primary outcome (depression severity according to the Symptom Checklist scale) and satisfaction with care, a secondary outcome. Additional secondary outcomes (antidepressant adherence and use of health services) were assessed using computerized medical records.
Key Results
Patients offered the program had higher rates of antidepressant adherence (81% continued treatment more than 3 months vs. 61%, p = 0.001), lower Symptom Checklist depression scores after 5 months (0.95 vs. 1.17, p = 0.043), and greater satisfaction with depression treatment (53% “very satisfied” vs. 33%, p = 0.004).
Limitations
The trial was conducted in one integrated health care system with a single care management nurse. Results apply only to patients using online messaging.
Conclusions
Our findings suggest that organized follow-up care for depression can be delivered effectively and efficiently through online messaging.
KEY WORDS: depression, randomized, follow-up, online messaging
INTRODUCTION
Depression care remains one of the poorest scores on the US healthcare report card.1,2 While antidepressant use has grown dramatically over the last 15 years,3 quality of antidepressant treatment has failed to improve.2,4 Rates of medication adherence and follow-up contact are especially low in primary care, where most depression treatment begins.5
Consistent evidence supports the effectiveness of organized depression care programs.6–8 Key elements of these programs include systematic outreach, structured outcome assessment, and algorithms to prompt evidence-based practice.9,10 Such programs have improved adherence, satisfaction, and clinical outcomes across diverse practice settings and patient populations.11–19 Telephone outreach is a central component of these programs.
Reliance on live contact between patients and providers, however, makes telephone follow-up less convenient, less timely, and more expensive. Patients must receive calls when providers are available. Repeated missed contacts are the norm.11,13 Each contact requires up to an hour of clinician time, with half of that spent on unsuccessful attempts.20 Inconvenience and cost are significant barriers to adoption of these programs.
Online patient–provider communication has the potential to increase the availability and reduce the cost of effective depression care. Our previous research supports use of online messaging to improve care of chronic medical conditions21,22 and suggests that patients treated for depression are especially likely to use online communication with healthcare providers.23
Depression care through online messaging, however, might prove less acceptable to patients or less clinically effective than care provided in-person or by telephone. Asynchronous text communication may limit a clinician’s ability to understand patients’ concerns or to communicate support and encouragement. Live voice contact may be essential for satisfying or effective depression care.
This randomized trial evaluated a depression care management program delivered entirely by asynchronous online messaging. The study design and intervention were intended to parallel those of previous telephone programs. We examined the acceptability of the program (indicated by the enrollment in the trial and participation in monitoring contacts) and examined whether the program led to improvements in severity of depression (the primary outcome) as well as improvements in patient satisfaction and quality of antidepressant treatment (secondary outcomes) compared to usual care.
METHODS
Setting and Participants
Participants were enrolled between April and October of 2009 from nine primary care clinics of Group Health Cooperative, an integrated health system serving approximately 600,000 members in the Pacific Northwest. Clinics were located in urban and suburban areas of the Washington cities of Bellevue, Burien, Everett, Olympia, Renton, Seattle, and Spokane. Group Health members are demographically similar to the area population. Group Health’s performance on measures of antidepressant medication adherence and follow-up visit frequency are between the 50th and 75th percentiles for US health plans.2
Participating clinics were experienced users of the EpicCare electronic medical record system (Epic Systems, Verona, WI). A patient website linked to this medical record includes online tools for refilling prescriptions, viewing laboratory results and exchanging online messages with providers. Automated e-mail reminders alert members to new messages or laboratory results. Members are encouraged to register for online messaging, and approximately 52% of all adult members had done so by April 2009.
Inclusion Criteria
Each week, electronic records identified potential participants meeting the following criteria: age 18 or older, filled a new antidepressant prescription from a participating primary care physician; did not fill any prescription for antidepressant medication in the prior 270 days; had a diagnosis of a depressive disorder associated with the prescription; was registered to use online messaging; and received no diagnosis of bipolar disorder or psychotic disorder nor any prescription for mood stabilizer or antipsychotic medication in the prior 2 years.
Randomization and Interventions
Each potential participant was sent an online invitation from the principal investigator (a Group Health psychiatrist). This message briefly described the study and included a link to an online consent form describing study procedures and potential risks. Each participant electronically signed this form prior to enrollment.
Consenting participants completed an online survey including a 20-item depression scale from the Hopkins Symptom Checklist,24 a standard measure of depression severity used in previous trials of telephone care management.11,12,15 Following the survey, each participant was randomly assigned to continued usual care or to the intervention program and was immediately notified of her/his assignment. Assignments were automatically generated by the survey database using a random number generator with no blocking or stratification. Treating physicians were not notified regarding study participation or group assignment, but (as described below) physicians of intervention group patients were later contacted by the care manager.
For those assigned to the usual care control group, no additional services were provided, but no services normally available (including follow-up in primary care or specialty referral for psychotherapy or medication management) were withheld. Online patient–provider messaging was available to all participants in the usual care group.
The care management intervention was a supplement to usual care by the treating physician. Structure and content followed the telephone programs tested in earlier studies11,12 with all communications by online messaging.
Immediately after randomization, each participant assigned to the intervention received a welcome message from the nurse care manager describing the program and providing general advice regarding antidepressant medication and self-care for depression. Monitoring contacts were scheduled two, six, and ten weeks later.
Each monitoring contact began with an outreach message from the nurse containing a link to an online assessment. The assessment included the PHQ depression questionnaire25,26 and questions regarding use of antidepressant medication, side effects, and reasons for medication discontinuation. Those not responding were sent up to two reminder messages.
For each assessment completed, an algorithm generated a suggested response based on PHQ depression score, current antidepressant use, and side effects (Table 1). The care manager could tailor this suggested response using information in the medical record or in messages since the last contact.
Table 1.
Sample Care Manager Responses to Online Antidepressant Monitoring Assessments. Complete Table of Suggested Responses Available on Request
| PHQ Depression Score | Antidepressant Use and Dose | Antidepressant Side Effects | Suggested Online Response | Follow-Up Communication |
|---|---|---|---|---|
| 0 to 4 | till using, any dose | None or mild | It seems that you are not having significant symptoms of depression now. I'd like to check with you again in a few weeks to make sure you are still doing well. I'll send you a message then. Please do contact me sooner if you need to | Re-assess at next monitoring point |
| O to 4 | till using, any dose | Moderate or severe | It seems that you are not having significant symptoms of depression now. But the medication is causing significant side effects. Do you think you can keep taking a while to see if the side effects get better? Or do we need to talk with your doctor about trying some other treatment? | Await response from patient. If side effects not tolerable, contact physician regarding need for alternative treatment. If tolerable, re-assess at next monitoring point |
| 10 or more | Stopped antidepressant (Reports it didn’t help) | N/A | It seems like you are still having significant problems with symptoms of depression. Does that sound right to you? You said the medication didn't help. Could you tell me how long you took it? And what dose (or how many pills a day) you took? Did you notice any positive effect? | Await response from patient. If initial trial not adequate, suggest re-starting. If initial trial adequate, contact physician to discuss alternative treatment |
| 10 or more | Still using, low or moderate dose | None or mild | It seems that you are still having significant symptoms of depression. But the medication is not causing significant side effects. I'll check with your doctor about whether we should continue the same for now or try increasing the dose. I'll get back to you soon | Contact physician to discuss increasing antidepressant dose, then follow up with patient |
| 15 or more | Still using, high dose | None or nild | It seems that you are still having significant symptoms of depression. I'll contact your doctor about whether we should try some other treatment. I'll get back to you soon | Contact physician to discuss alternative treatment, then follow up with patient |
The care manager communicated with the treating physician using an electronic messaging system within the electronic medical record. In consultation with the physician, the care manager might facilitate follow-up visits, support changes in medication, or facilitate referral for specialty care (including urgent referrals in case of suicidal ideation or severe symptoms). Each of the three care management contacts included this cycle: outreach message from the care manager, patient completion of online assessment, structured response from the care manager, and follow-up communication with the patient and physician as needed (see Table 1). The care manager’s messages to patients included brief support but no formal psychotherapy. Patients were free to send additional messages or telephone the care manager if needed. The care manager was expected to make outreach telephone calls in case of suicidal ideation or other urgent clinical need. All outgoing messages were in English.
The care manager in this trial was a registered nurse with added certification in psychiatry and 15 years of experience in mental health. Training for this program included two hours of practice with the care management software. Supervision meetings with the study psychiatrist (approximately 15 minutes weekly for 3 months and 15 minutes monthly thereafter) reviewed adherence to the contact schedule and discussed cases showing persistently high depression scores. The supervising psychiatrist had no direct communication with treating physicians.
Outcomes and Follow-up
Approximately five months after randomization each participant in the care management and usual care groups received a message inviting participation in a research follow-up survey. This online survey included measures used in previous trials of telephone care management: the SCL depression score and a single-item rating of satisfaction with depression care on a 7-point scale ranging from “very dissatisfied” to “very satisfied”. Consistent with previous trials, comparison of satisfaction ratings considered the proportion “very satisfied”.
For all potential participants, computerized membership and medical records were used to examine demographic characteristics (including neighborhood demographics based on census block of residence),27 and overall medical morbidity.28
For all actual participants, electronic medical records were used to examine use of specific health services during the six months after randomization: filled antidepressant prescriptions, outpatient visits, telephone contacts, and online messages. Prescription refill data were used to assess two measures of antidepressant use: the total days dispensed AND receipt of a second antidepressant (indicating medication switch or combination).
Statistical Analysis
Analyses compared the intervention and usual care groups according to initial assignment, regardless of participation in care management. The primary outcome measure was mean SCL depression score after adjustment for baseline score. Comparison of depression scores and satisfaction with care included all completing the research outcome survey. Comparison of health service use included all those randomized. A priori power calculations indicated that a sample of 100 per group would have 80% power to detect a between-group difference of 0.25 in mean SCL depression score and a difference of 20% in the proportion continuing antidepressant medication more than 90 days (differences approximately equal to those seen with earlier telephone programs).
All study procedures were approved by the Group Health Cooperative Human Subjects Review Committee.
RESULTS
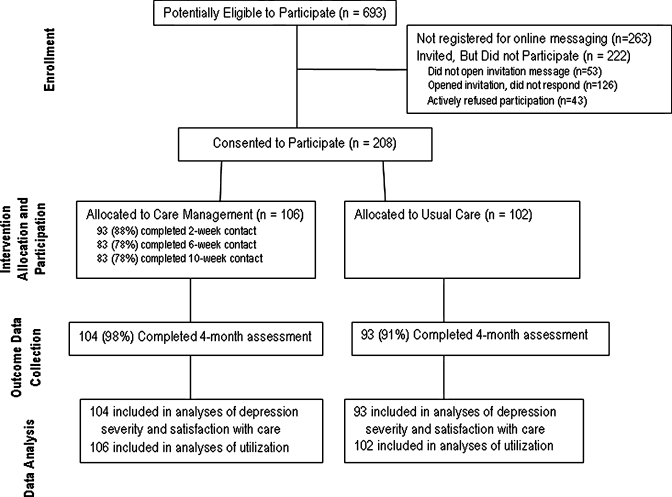
The progress of participants through the trial is shown in Figure 1. Of patients at participating clinics starting antidepressant treatment, 62% were registered for online messaging and therefore eligible to enroll in the trial. As shown in the left portion of Table 2, registration was significantly associated with female sex and lower probability of residing in neighborhoods with lower educational attainment. Of eligible patients invited to participate, 12% did not open the invitation message, 29% opened the invitation but did not respond, and 10% responded by declining to participate. Consequently, the rate of participation was 48% (208/430) among all invited and 55% (208/377) among those opening the invitation. The right portion of Table 2 includes those meeting all eligibility criteria and compares those enrolling and not enrolling. Participants did not differ significantly from non-participants in any measure examined.
Figure 1.
Trial flow chart.
Table 2.
Patient Characteristics Related to Study Participation. Left Half of Table Includes all Patients at Study Clinics Starting Antidepressant Treatment and Compares Those Registered and Those not Registered to use Online Messaging. Right Half of Table Includes Patients Meeting all Eligibility Criteria (Including Registration for Website) and Compares Those Enrolled in the Trial with Those not Participating
| Among patients starting antidepressant | Among patients eligible to participate | |||||
|---|---|---|---|---|---|---|
| Registered for Messaging (n = 430) | Not Registered (n = 263) | Registered vs. Not Registered (df = 1 for all) | Enrolled in Trial (n = 208) | Did Not Participate (n = 222) | Enrolled vs. Not Enrolled (df = 1 for all) | |
| % Age 60 or older | 25% (n = 108) | 28% (n = 74) | X2 = 0.77, p = 0.38 | 14% (n = 28) | 20% (n = 44) | X2 = 3.11, p = 0.078 |
| % Female | 75% (n = 322) | 67% (n = 176) | X2 = 5.12, p = 0.024 | 72% (n = 150) | 75% (n = 166) | X2 = 0.39, p = 0.53 |
| % With high medical comorbidity | 28% (n = 120) | 22% (n = 58) | X2 = 2.93, p = 0.087 | 24% (n = 50) | 26% (n = 58) | X2 = 0.25, p = 0.62 |
| % From lower income neighborhood* | 24% (n = 103) | 29% (n = 76) | X2 = 2.08, p = 0.15 | 22% (n = 45) | 26% (n = 58) | X2 = 1.19, p = 0.28 |
| % From lower education neighborhood† | 34% (n = 146) | 43% (n = 114) | X2 = 6.14, p = 0.013 | 35% (n = 72) | 37% (n = 82) | X2 = 0.25, p = 0.62 |
*- % from census block with median income <$40,000/yr
†−% from census block with <25% college graduates
The 208 participants were treated by 78 primary care physicians. As shown in Table 3, participants were predominantly female with average age in the 40 s and average baseline depression score in the moderate range. At the baseline survey (typically 7 to 10 days after starting treatment), 13% (27/208) reported mild depression (SCL score less than 1.0) and 20% (41/208) reported severe depression (SCL score 2.5 or greater).
Table 3.
Comparison of Participants Assigned to Care Management and Usual Care Groups
| Care Management (n = 106) | Usual Care (n = 102) | |
|---|---|---|
| Mean age (st. dev.) | 46 (13) | 45 (14) |
| % Female (n) | 69% (n = 73) | 75% (n = 77) |
| % Minority race/ethnicity (n) | 17% (n = 18) | 15% (n = 15) |
| % using online messaging in prior 6 months | 86% (n = 91) | 82% (n = 84) |
| Mean SCL depression score (st dev) | 1.84 (0.74) | 1.83 (0.69) |
Participants assigned to the intervention completed 82% of all care management contacts; 95% of participants completed at least one contact. Completion of care management contacts was not related to baseline depression severity. Of completed care management contacts, 57% (151/263) included one or two follow-up messages between patient and nurse, 29% (76/263) included three or four, and 14% (36/263) included five or more follow-up messages.
Approximately 95% of participants completed the research outcome assessment, and average time from randomization to completion was 155 days. Completion was not related to severity of depression at baseline.
Mean SCL depression scale scores at the outcome assessment were 0.95 (st. dev. 0.71) in the care management group compared to 1.17 (st. dev. 0.81) in the usual care control group (t = 2.05, df = 195, p = 0.043, effect size =0.29). In a linear model adjusting for baseline SCL depression score and including a random effect for treating primary care physician, depression severity was significantly lower in those assigned to the care management program (Adjusted difference = 0.29, 95% CI 0.06–0.51). The proportion of participants experiencing a 50% or greater decrease in SCL depression score between the baseline and five month assessments (a standard criterion for satisfactory treatment response) was 55% (57/104) in the care management group compared to 41% (38/93) in the usual care group (Odds Ratio = 1.8, 95% CI = 1.0 to 3.1). The proportion of participants “very satisfied” with depression treatment was 53% (56/104) in the care management group compared to 33% (31/93) in usual care (X2 = 8.38, df = 1, p = 0.004). No harms or unintended effects of the intervention were observed, and there were no psychiatric hospitalizations or suicide attempts in either group.
Use of antidepressant medication and other outpatient services during the six months following randomization is shown in Table 4. Patients assigned to the intervention were more likely to continue medication beyond 90 days and were slightly (but not significantly) more likely to receive a second antidepressant (indicating medication change or combination). Utilization rates for outpatient medical and mental health visits, telephone encounters, and non-study online messages (i.e. excluding messages to or from the care manager) did not differ significantly between the two groups.
Table 4.
Use of Health Services During Six Months After Randomization
| Care Management (n = 106) | Usual Care (n = 102) | Test Statistic | |
|---|---|---|---|
| Number (%) using antidepressant for over 90 days* | 86 (81%) | 62 (61%) | X2 = 10.5, df = 1, p = 0.001 |
| Number (%) receiving an additional antidepressant* | 23 (22%) | 16 (16%) | X2 = 1.23, df = 1, p = 0.27 |
| Number (%) making any specialty mental health visits | 34 (32%) | 32 (31%) | X2 = 0.01, df = 1, p = 0.91 |
| Mean (st dev) mental health visits for psychotherapy | 0.8 (1.9) | 0.9 (2.1) | Z‡ = 0.93, p = 0.35 |
| Mean (st dev) mental health visits for medication mgmt. | 0.4 (1.4) | 0.3 (1.5) | Z‡ = 1.35, p = 0.18 |
| Mean (st dev) primary care visits | 4.1 (4.4) | 3.5 (3.9) | Z‡ = 1.14, p = 0.25 |
| Mean (st dev) online message exchanges† | 7.3 (9.5) | 5.9 (6.8) | Z‡ = 1.20, p = 0.23 |
| Mean (st dev) telephone contacts | 2.3 (3.5) | 2.3 (4.5) | Z‡ = 0.28, p = 0.78 |
* - Based on prescription refill records
† − Count of message “threads” includes series of messages on a single subject. This count excludes messages between intervention group patients and care management nurse.
‡ − Mann-Whitney nonparametric test for comparison of ranks
Total care manager time allocated to delivering the intervention was 104 hours (approximately 1 hour per patient offered the program or 0.4 hours per completed contact). No telephone contacts (either outreach calls by the care manager or incoming calls from patients) were necessary.
DISCUSSION
Among primary care patients starting antidepressant treatment, care management through online messaging significantly reduced severity of depression compared to usual primary care. Participation in care management contacts was high, and the program significantly improved patients’ satisfaction with depression treatment. These findings add to previous research demonstrating the effectiveness of online health communication in the management of chronic conditions such as hypertension and diabetes.21,22
The 0.29 effect size for improvement in depressive symptoms in this trial is larger than the effect sizes of 0.23 and 0.19 in two previous telephone programs at these same clinics11,12 and approximately equal to the effect sizes of 0.25 to 0.30 seen with telephone depression programs in other primary care settings.15,16 The increase in proportion of patients experiencing a satisfactory clinical response was also similar to that seen with earlier telephone care management programs. Clinical effects were, however, smaller than those seen with more intensive programs including telephone psychotherapy or in-person contact.11,14 These indirect comparisons between online and telephone or in-person programs should be interpreted cautiously, and definite conclusions must await a direct comparison.
The staff time required to provide depression follow-up by online messaging was less than half of that required for telephone programs.20 Some of the work of the care manager (welcome messages, invitation messages, reminders to those not completing assessments) could be automated, further increasing efficiency.
Limitations
We should emphasize that these findings only apply to patients able and willing to communicate by online messaging. Nearly 80% of Americans have home internet access,29 and surveys find high interest in e-mail communication with health care providers.30 Financial incentives authorized by the 2009 Recovery Act may further increase availability of online health communication, especially if those incentives define meaningful use of electronic records to include online patient–provider communication.31 Nevertheless, disadvantaged populations may have less access to online health services. In our sample of patients starting antidepressant treatment, those not registered for online services more often lived in disadvantaged neighborhoods.
Approximately half of those registered to use online services enrolled in this trial, compared to 60% to 65% participation in similar trials of telephone care management.11,12 Non-participation may have reflected reservations about online depression follow-up or reservations about participation in a clinical trial. Participation may have been greater if (as in previous trials of telephone interventions) the initial invitation had come from the patient’s health care team rather than a researcher and was followed by vigorous telephone outreach.
The overall completion rate for care management contacts was approximately 85% compared to 95% in previous telephone programs.11,12 Despite these lower completion rates, clinical benefits (considering all patients randomized) were similar.
This study was conducted in an integrated health care system with shared records of medical and mental health care as well as established collaborative relationships between primary care and mental health providers. The efficiency and clinical benefit of this program might be difficult to replicate outside of an integrated system.
Follow-up in the usual care group was more intensive than in typical primary care practice, probably reflecting both above-average follow-up rates in this setting2,5 and a greater likelihood of research participants to return for follow-up. Testing this intervention among patients receiving above-average follow-up care could create a conservative bias (i.e. reduce the likelihood of showing a benefit).
Implications for Research and Policy
Our findings suggest additional questions regarding the effectiveness and value of online care management. We cannot determine whether increased medication adherence was the cause of improved outcomes or simply a corollary. We do not know whether more vigorous outreach (as in previous telephone programs11,12) might have increased either participation in care management or the effectiveness of the program. While we observed no significant effects of the intervention on use of health services for depression treatment, this trial was too small and too brief in duration to assess effects on economic outcomes such as health care spending or work productivity.
Future research might also examine acceptability and effectiveness of online care management outside of an electronic medical record. Communication by standard email, text messaging, or social networking sites would be less integrated into health system workflow and information systems, but it would certainly be more convenient for patients. Text messaging communication would also reach many disadvantaged patients without conventional internet access. Health care lags behind other industries in taking advantage of these more widespread communication technologies.
Unfortunately, online health communication, whether with physician or non-physician providers, would not be reimbursed by most US health insurance systems. Even if the cost of online care management is low, implementation is unlikely without reimbursement reform. Increasing attention to the patient-centered medical home32,33 may facilitate reimbursement for services other than in-person physician visits.
Conclusions
We did not evaluate the benefits of simply allowing online patient–provider communication; online messaging was available to the intervention and usual care groups. Instead we evaluated a structured care program among people already using online communication. Availability of online messaging (like availability of the telephone) does not guarantee effective clinical communication or improved quality of care. Organized care for depression, whether by telephone or online, includes systematic outreach, standardized assessment of adherence and outcomes, application of evidence-based guidelines, and persistent tailoring of treatment to maximize response.9,10 Our findings suggest that those key elements of depression care can be delivered effectively and efficiently through online messaging.
ACKNOWLEDGEMENTS
Authorship contributions:
• Study concept and design: Simon, Ralston, Operskalski, Pabiniak, Savarino, Wentzel
• Acquisition of data: Wentzel, Pabiniak, Savarino
• Analysis and interpretation of data: Simon, Ralston, Wentzel
• Drafting of manuscript: Simon
• Critical revision of manuscript for important intellectual content: Ralston, Savarino, Pabiniak, Wentzel, Operskalski
• Statistical analysis: Simon
• Obtained funding: Simon
• Administrative, technical, or material support: Operskalski, Savarino, Pabiniak
• Study supervision: Simon, Operskalski
Financial Interests: Drs. Simon and Ralston are both employees of the Group Health Permanente Medical Group; the remaining authors are all employees of Group Health Cooperative. The authors have no other relevant financial interests to disclose.
Funded by NIMH grant R21 MH082924. The funder had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Dr. Simon had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest None disclosed.
Footnotes
Trial Registration
Clinicaltrials.gov ID NCT00755235
REFERENCES
- 1.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 2.The state of health care quality 2009. Washington: National Committee for Quality Assurance; 2009. [Google Scholar]
- 3.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–856. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- 4.Morrato EH, Libby AM, Orton HD, et al. Frequency of provider contact after FDA advisory on risk of pediatric suicidality with SSRIs. Am J Psychiatry. 2008;165(1):42–50. doi: 10.1176/appi.ajp.2007.07010205. [DOI] [PubMed] [Google Scholar]
- 5.Simon GE, Korff M, Rutter CM, Peterson DA. Treatment process and outcomes for managed care patients receiving new antidepressant prescriptions from psychiatrists and primary care physicians. Arch Gen Psychiatry. 2001;58(4):395–401. doi: 10.1001/archpsyc.58.4.395. [DOI] [PubMed] [Google Scholar]
- 6.Bower P, Gilbody S, Richards D, Fletcher J, Sutton A. Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]
- 7.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 8.Williams JW, Jr, Gerrity M, Holsinger T, Dobscha S, Gaynes B, Dietrich A. Systematic review of multifaceted interventions to improve depression care. Gen Hosp Psych. 2007;29(2):91–116. doi: 10.1016/j.genhosppsych.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 9.VonKorff M, Gruman J, Schaefer J, Curry S, Wagner E. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–1102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 10.Wagner E, Austin B, VonKorff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–544. doi: 10.2307/3350391. [DOI] [PubMed] [Google Scholar]
- 11.Simon GE, Ludman EJ, Tutty S, Operskalski B, Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292(8):935–942. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 12.Simon GE, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ. 2000;320(7234):550–554. doi: 10.1136/bmj.320.7234.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang P, Simon G, Avorn J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298:1401–1411. doi: 10.1001/jama.298.12.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Unutzer J, Katon W, Callahan C, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 15.Dietrich A, Oxman T, Williams J, et al. Re-engineering systems for the treatment of depression in primary care: a cluster randomised controlled trial. BMJ. 2004;329:602–610. doi: 10.1136/bmj.38219.481250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hunkeler E, Meresman J, Hargreaves W, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Arch Fam Med. 2000;9:700–708. doi: 10.1001/archfami.9.8.700. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Bair MJ, Damush TM, et al. Optimized antidepressant therapy and pain self-management in primary care patients with depression and musculoskeletal pain: a randomized controlled trial. JAMA. 2009;301(20):2099–2110. doi: 10.1001/jama.2009.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richards DA, Lovell K, Gilbody S, et al. Collaborative care for depression in UK primary care: a randomized controlled trial. Psychol Med. 2008;38(2):279–287. doi: 10.1017/S0033291707001365. [DOI] [PubMed] [Google Scholar]
- 19.Fortney JC, Pyne JM, Edlund MJ, et al. A randomized trial of telemedicine-based collaborative care for depression. J Gen Intern Med. 2007;22(8):1086–1093. doi: 10.1007/s11606-007-0201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu CF, Fortney J, Vivell S, et al. Time allocation and caseload capacity in telephone depression care management. Am J Manag Care. 2007;13(12):652–660. [PubMed] [Google Scholar]
- 21.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299(24):2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diab Care. 2009;32(2):234–239. doi: 10.2337/dc08-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ralston JD, Rutter CM, Carrell D, Hecht J, Rubanowice D, Simon GE. Patient use of secure electronic messaging within a shared medical record: a cross-sectional study. J Gen Intern Med. 2009;24(3):349–355. doi: 10.1007/s11606-008-0899-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Derogatis L, Rickels K, Uhlenhuth E, Covi L. The Hopkins symptom checklist: a measure of primary symptom dimensions. In: Pichot P, editor. Psychological measurements in psychopharmacology: problems in psychopharmacology. Basel: Kargerman; 1974. pp. 79–110. [Google Scholar]
- 25.Kroenke K, Spitzer R, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spitzer R, Kroenke K, Williams J. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 27.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–710. doi: 10.2105/AJPH.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Starfield B, Weiner JP, Mumford L, Steinwaches DM. Ambulatory care groups: a categorization of diagnosis for research and management. Health Serv Res. 1991;26:54–74. [PMC free article] [PubMed] [Google Scholar]
- 29.Smith A. Home broadband 2010. Washington: Pew Research Center's Internet & American Life Project; 2010. [Google Scholar]
- 30.Cummings J. The benefits of electronic medical records sound good, but privacy could become a difficult issue. Rochester: Harris Interactive; 2007. [Google Scholar]
- 31.Ralston JD, Coleman K, Reid RJ, Handley MR, Larson EB. Patient experience should be part of meaningful-use criteria. Health Aff (Millwood) 2010;29(4):607–613. doi: 10.1377/hlthaff.2010.0113. [DOI] [PubMed] [Google Scholar]
- 32.Ralston JD, Martin DP, Anderson ML, et al. Group health cooperative's transformation toward patient-centered access. Med Care Res Rev. 2009;66(6):703–724. doi: 10.1177/1077558709338486. [DOI] [PubMed] [Google Scholar]
- 33.Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29(5):835–843. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]