ABSTRACT
BACKGROUND
African Americans (AA) and rural communities often suffer disproportionately from poorer health. Theory-guided research examining how individual- and community-level factors influence health behaviors and contribute to disparities is needed.
OBJECTIVE
To understand how a social network model that captures the interplay between individual and community factors might inform community-based interventions to reduce HIV risk in rural AA communities.
DESIGN
Qualitative study.
SETTING AND PARTICIPANTS
Eleven focus groups with 38 AA 16–24 year olds, 42 adults over age 25, and 13 formerly incarcerated individuals held in community settings in two rural, predominantly AA counties in North Carolina. Thirty-seven semi-structured interviews with multiethnic key informants.
APPROACH
Semi-structured interviews and focus groups with open-ended questions assessed a) perceptions of multi-level HIV risk determinants from a social network model (individual, interpersonal, social, economic, political and structural) identified through literature review and b) community needs and assets affecting local HIV rates. Qualitative data was analyzed using directive content analysis guided by a social network model.
RESULTS
We identified four themes regarding the interaction between individuals and their communities that mediate HIV risk: interpersonal processes, community structural environment, social disorder, and civic engagement. Communities were characterized as having a high degree of cohesiveness, tension, and HIV-related stigma. The community structural environment—characterized by neighborhood poverty, lack of skilled jobs, segregation, political disenfranchisement and institutional racism—was felt to reduce the availability and accessibility of resources to combat HIV. Adults noted an inability to combat social problems due to social disorder, which fuels HIV risk behaviors. Civic engagement as a means of identifying community concerns and developing solutions is limited by churches’ reluctance to address HIV-related issues.
CONCLUSION
To combat HIV-related stigma, physicians should follow recommendations for universal HIV testing. Besides asking about individual health behaviors, physicians should ask about the availability of support and local community resources. Physicians might consider tailoring their treatment recommendations based on available community resources. This strategy may potentially improve patient adherence and clinical outcomes.
KEY WORDS: social capital, HIV prevention, rural communities, African Americans, community-based participatory research
INTRODUCTION
Racial disparities in health are well-documented.1 African Americans and individuals living in rural communities are often disproportionately affected by poor health and suboptimal health care. Extant literature largely focuses on individual-level factors which contribute to health disparities, with less emphasis on the contextual factors within communities that often underlie and perpetuate disparities.2,3
Social capital is a potentially useful construct for understanding health disparities because it acknowledges the contribution of individual- and community-level factors that impact health care and outcomes. Social capital has various definitions, ranging from the strength of connections within and between groups (i.e. social cohesion) to the resources (e.g., economic, political, or material) available to groups.4–6 Social capital theories suggest that individuals embedded in social networks can access and benefit from group resources.7 Thus, individuals belonging to groups possessing a greater amount of social capital are expected to exhibit lower disease rates.2
Social capital has been examined in relation to a variety of health-related outcomes, including mortality,8 health status,9 sexually transmitted diseases,10,11 mental health,12–15 health care access,16 and health behaviors.17,18 Findings from studies examining social capital as a contributor to racial disparities have been inconclusive.19 The ambiguity stems from variations in the definitions and measures used to assess social capital.4–6 Measures of social capital that fail to understand the dynamic interplay between individuals and their communities produce only partial accounts of individuals’ lived experiences and little insight into why disparities persist or how to eliminate them.20,21
Therefore, the goals of our study were twofold: 1) to understand, using qualitative methods, how a social network model that emphasizes the impact of differential social capital on health disparities and outcomes can be used to understand disparities in HIV risk by examining the reciprocal relationship between rural AAs and their communities, and 2) to use this information to develop a community-based HIV risk reduction intervention.
METHODS
Description of Social Network Model
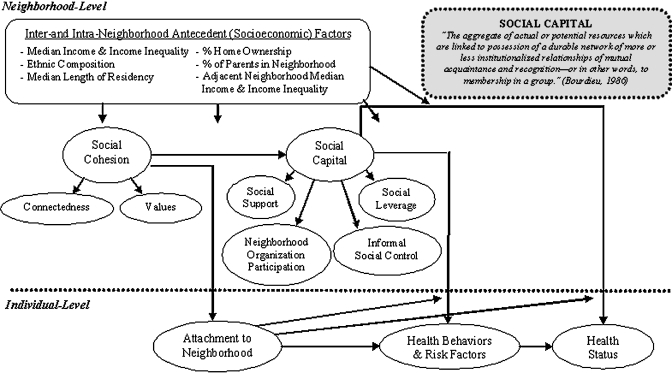
This model (Fig. 1) incorporates aspects of an individual’s interpersonal environment, as well as broader neighborhood factors that influence health behaviors, health outcomes, and health disparities.22 It is based on a definition of social capital as “the aggregate of actual or potential resources linked to possession of a durable network available to group members for pursuing action in the absence of, or in conjunction with their own economic capital.”4 This model proposes three critical conceptual domains: (1) social cohesion which leads to social capital, (2) social capital, or the actual or potential group resources that can be leveraged by individuals for their benefit, and (3) the influence of the broader neighborhood environment on the exercise of capital. Social cohesion represents trust, familiarity, and shared values among neighborhood residents. Social capital takes four forms: support (assistance coping with daily life issues and stressors), leverage (providing access to information and social advancement), control (collective maintenance of order and neighborhood safety), and civic participation (engagement in organized groups or structured activities to address community issues).22 The neighborhood environment influences both the degree of cohesion that can develop between individuals and the availability and accessibility of community resources.
Figure 1.
Proposed Conceptual Model of Neighborhood Social Capital Processes on Individual Health Outcomes. Reprinted with permission SOURCE: Richard M. Carpiano (2006). Toward a Neighborhood Resource-based Theory of Social Capital for Health: Can Bourdieu and Sociology Help? Social Science and Medicine, 62(1), 165-175.
Study Design and Setting
Our work was conducted through an academic-community partnership which uses community-based participatory research (CBPR) approaches to develop HIV prevention interventions.23 Data were collected through focus groups (FG) and key informant (KI) interviews conducted in 2006–2007 as part of a community needs and assets assessment to guide intervention development. The study took place in two counties in northeast North Carolina (NC) with some of the highest rates and most significant disparities in HIV/AIDS in the state (Table 1).24,25 These counties rank 3rd and 16th among NC’s 100 counties in the three-year average rate of new HIV cases for 2005–2007. In 2006, the majority of each county’s HIV/AIDS cases were among AAs (86% and 82%). Participants aged 18 and older provided verbal informed consent; those under age 18 provided verbal assent and their parents provided written informed consent. This study was approved by the Institutional Review Board at The University of North Carolina at Chapel Hill.
Table 1.
Descriptive Statistics by County
| Characteristic | County A | County B |
|---|---|---|
| Population size | 55,606 | 87,420 |
| % African American | 58 | 34 |
| State ranking in 3-year average rate of new HIV cases* | 3 rd | 16th |
| % of HIV/AIDS cases per county among African Americans† | 86 | 82 |
| $ Median Household Income | 30, 983 | 37,147 |
| % with less than a High School Education | 34.4 | 24.4 |
| % with a High School Diploma | 36.9 | 33.9 |
| % with a Bachelor’s Degree or higher | 8.5 | 17.2 |
*For years 2005–2007
†For year 2006
Focus Groups
We recruited individuals from three populations that our community partners felt were at greatest risk for HIV infection: youth/young adults aged 16–24, formerly incarcerated (FI) individuals, and adults over age 25. Together with community-based organizations in both counties, our team posted flyers, used print and radio advertising, and person-to-person sampling. Eleven gender-stratified FG were held: four with youth/young adults, five with general adults, and two with FI individuals. Groups were held at local youth centers, a church, and a community administration facility. Each lasted approximately two hours and was led by an experienced moderator, matched to participants’ race and gender.
The semi-structured discussion guide assessed three topic areas: 1) perceptions about local HIV determinants based on literature review, 2) community needs, assets and resources affecting local HIV rates and 3) key considerations for intervention development. We asked two general questions about factors contributing to the spread of HIV locally: 1) "Why do you think rates are higher among AAs than Whites in this community?", and 2) "If our goal is to reduce high rates of HIV/AIDS among AA around here, list everything that gets in the way of achieving that goal"; interviewees were asked to consider individual, interpersonal, social, economic, political, and structural barriers, as well as physical surroundings. To ensure that all FG and KI interviews covered these topics, probes were used if participants’ responses did not fit within at least one of the aforementioned categories. To identify community needs, assets, resources, and key considerations for intervention development, we asked, “What can you and your community do to address these (e.g. cultural) issues to help reduce HIV/AIDS among AA in this community?” Each participant completed a demographic questionnaire and received a $20 incentive for their participation.
Key Informant Interviews
Community partners were asked to identify influential individuals in each county whose opinions about HIV risk, disparities, and potential solutions would be valuable. We sought individuals from the following sectors: political, economic, health, law enforcement, media, recreation, community groups, education, religious, social welfare, and leaders of grassroots organizations. Project staff contacted nominees about participating. Nominees were asked to identify other KI using these same criteria. Semi-structured interviews were conducted in private offices, lasted approximately 2 hours, and used a 12-question discussion guide that paralleled the FG guide.
Analysis
FG and KI interviews were audio-recorded, transcribed and entered into Atlas.ti version 5.2, a qualitative data management program. Since we used an existing framework to guide the data coding process, we conducted directive content analysis (DCA). DCA is performed when the analytic goal is to validate or extend prior theoretical frameworks.26 Coders reviewed transcripts line-by-line to identify passages supporting the three domains from the social network model.22 Coders considered whether a comment explicitly addressed a domain in a general sense (e.g., descriptions of social cohesion), as well as whether narratives linked one of the models’ domains specifically to HIV risk or prevention (e.g., how dilapidated houses foster engagement in HIV risk behaviors). Finally, coders considered the relevance of participants’ comments for developing an HIV prevention intervention.
Transcripts were coded by two independent coders. The team organized coded passages into major and sub-themes and explored theoretical links between themes. When there was ambiguity or coders differed in their assignment of a thematic category, coders met with a third party to discuss the issue and reach consensus. We compared thematic content within and across FG and interviews. For FG, we also compared themes across participant gender and type. Reported themes were consistent across study participant types, unless otherwise specified, and consistent across coders.
RESULTS
Sample Characteristics
We interviewed 93 FG participants and 37 KIs. All FG participants and 23 (62%) of KI were AA. Eighteen (47%) of the youth/young adult, 24 (57%) of general adults, and 4 (31%) of the FI FG participants were female. Mean ages for youth/young adult, general adult, and FI participants was 18, 35, and 37 years, respectively. The mean age of KIs was 49 years. More KIs reported having a graduate degree (n = 14, 38%) than general adult FG participants (n = 1, 2%) (Table 2).
Table 2.
Characteristics of Study Sample
| Focus Group Participants | ||||
|---|---|---|---|---|
| Characteristic | Youth/Youths (N = 38) | General Adults (n = 42) | Formerly Incarcerated (n = 37) | Key Informants (n = 13) |
| African American, N (%) | 38 (100) | 42 (100) | 13 (100) | 23 (62) |
| Female gender, N (%) | 18 (47) | 24 (57) | 4 (31) | 16 (43) |
| Mean age, years (range) | 18 (16-24) | 35 (22-46) | 37 (25-53) | 49 (32-64) |
| Education, N (%)* | ||||
| Less than high school grad | 32 (84) | 8 (19) | 7 (54) | 0 (0) |
| Graduate high school/ GED | 3 (8) | 8 (19) | 5 (15) | 2 (5) |
| Some college | 2 (5) | 8 (19) | 1 (8) | 6 (16) |
| Graduate degree | 1 (3) | 1 (2) | 0 (0) | 14 (38) |
| Family receiving Public Assistance, % | 13 (34) | 5 (12) | 3 (23) | N/A |
*Numbers may not add up to 100% since not all possible categories are represented
N/A = not asked
Thematic Overview
We identified 4 main themes as important for understanding racial disparities in local HIV rates: Interpersonal processes, community structural environment, social disorder, and civic engagement (Table 3).
Table 3.
Four main themes, subthemes and representative quotes
| Interpersonal Processes* | |
| Social cohesion | “I like the ability that we have to work on various problems in the community. I like the cohesiveness that exists among our community… Wanting to make sure that what I do is in the best interest of everybody in the community.” |
| –AA female KI | |
| Social tensions | “We are so in that ‘crab attitude’. We’re so scared one will get higher than the other that instead of trying to take both of them and move up, we’d rather pull somebody down instead of try to lift them up.” |
| –AA adult male FG | |
| HIV-related stigma | “Everybody is so secretive about it. [HIV] is like a disease that you don't want to talk about. It’s a disease that you don't want in your neighborhood.” |
| –AA female KI | |
| People don’t know about HIV and the people don’t want to talk about it… it’s a fear of stigma for one of the reasons that stand in the way for HIV AIDS. | |
| –AA adult female FG | |
| Community Structural Forces | |
| Availability of resources | “If I don’t have a job to go to and I’m sitting around all day, the only thing that I’m thinking about doing is something to make me feel better. I’m going to get high or I’m gonna have sex.” |
| –AA adult male FG | |
| “[County Name] is one of the poorest counties… having one of the highest… AIDS rates and highest drugs and alcohol activity it makes you wonder why… It’s not that we don't have jobs, we don't have resources. Folk are depressed and oppressed and, and therefore we’re turning to other things…“ | |
| –AA male KI | |
| Accessibility of resources | “A lot of people have a hard time getting to different functions and community things because they don’t have transportation or a way to get there…” |
| –AA youth/young adult female FG | |
| “Most men that could be role models are either working and do not have that time, accessibility to come out and be role models for the children. And those that do, the few that has the ability to do that are overworked…” | |
| –AA male KI | |
| Segregation, political forces and institutional racism | “We still have some racial tension here in this county… I think a lot of it is in government, not so much the people in the community… Some of that carries over to the school where students sometimes are not treated fairly I think. Also it carries over to the job market where certain people of certain races may not be promoted in this county because of the close-mindedness.” |
| –AA female KI | |
| Social Disorder | |
| “Either you don't have enough police presence there or if you do have the police presence there, you have a lot of community people who don’t trust them … And to me that, that prevents them [police and community members] from working together and trying to control the neighborhood.” –AA male KI | |
| Civic Engagement | |
| “When a person is more involved in their church, they have often times a greater sense of purpose and they have a support network that helps with their mental health and helps with so many other things.” –White male KI “I'm not sure that there is a support network through the churches because… I think that religion… often times people who are in that ‘at risk’ category for HIV AIDS are probably not viewed positively in a religious setting…” –White female KI | |
Interpersonal Processes
Adults described strong cohesion and a deep-seated sense of community resulting from small population size, population stability, long-standing intergenerational connections, and shared values between residents. In contrast, youth and FI individuals believed that social tension (i.e. lack of cohesion), largely related to segregation and poverty, overshadowed their sense of belonging and restricted access to beneficial resources outside their personal networks. They described racial tensions between AA and Whites, conflicts based on neighborhood boundaries, and socio-economic class differences among AAs as fostering this tension.
Features of these communities, which made them desirable for some participants (e.g., small size and familiarity between individuals) also served to foster HIV-related stigma. Individuals living with or presumed to be at risk for HIV were unable to draw upon support of others in the community. As illustrated by an AA female KI, “individuals who test positive are outcasts…no longer a part of the community.” HIV-related stigma also adversely affected outreach and prevention efforts. Community members were less willing to be tested for HIV for fear that doing so may cause others to assume they were homosexual or engaging in high-risk behaviors.
Community Structural Environment
Availability of resources Adult respondents remarked that tight connections between individuals engendered a high degree of perceived support. Yet, the ability of social networks to provide tangible support was reportedly reduced by a combination of neighborhood poverty, lack of skilled jobs, lack of transportation, and segregation by race and socio-economic status. These factors concentrated AAs into communities lacking crucial resources necessary for self-sufficiency. For some, this adversity led to engagement in criminal activities, such as selling drugs or prostitution. Others responded by leaving the community to seek better opportunities for economic and social advancement. Those remaining often worked multiple jobs or long shifts and had little time for civic engagement. Thus, individuals capable of providing tangible support or mentorship were often inaccessible or overextended. Material and psychological effects of poverty fostered feelings of hopelessness and isolation. Participants’ narratives suggested that many AAs in these communities have a sense of ‘fatalism’ about their futures, which reportedly led to engagement in high-risk behaviors as an escape mechanism.
Accessibility to resources Our respondents reported an inability to fully utilize information and other health-promoting community resources. Concentrated poverty in these communities meant AAs primarily utilized public health departments or “free clinics” as primary sources of care. Participants perceived that shame surrounding the use of these facilities combined with fear of confidentiality breeches, common in small communities, led many to avoid seeking health care or HIV testing services. Such avoidance was thought to indirectly facilitate HIV transmission. Youth and adult participants articulated barriers to accessing certain health services to reduce HIV transmission. A female FI participant noted:
“…the people who use drugs they don’t go to the health department…speaking from being on that life, living in that life. You won’t come up and take care of yourself like you should. And at any given time, you don't have condoms. You won’t use condoms.”
Segregation, Political Forces and Institutional Racism Participants attributed AAs collective inability to capitalize on resources external to their personal networks to historical and continued racial segregation at the county level and a lack of AA representation in social welfare and political institutions. As one female KI noted: [African Americans] are outnumbered … on [the] school board…These decision makers at the hospital level, at the political level, at where something can be done about this issue [HIV], is generally led and financed by Whites. And they are more concerned about their race than they are [about] Blacks.
Despite the HIV burden in the target counties, participants felt county-level funding for prevention remained inadequate. Participants blamed institutional racism for AAs inability to translate their growing political power into lower HIV risk. One white male KI commented: If this was an epidemic in the White, middle-class high school students, all the resources of the town and county would be diverted immediately to address it. But it’s predominantly seen as an African-American issue and I think that racism, the institutional racism of our community, is what keeps us inactive.
Social Disorder
Many respondents noted a lack of informal control over the criminal activity and violence perpetuated by local gangs. Some participants attributed this inability to maintain control as both a product and consequence of a lack of community cohesiveness and downward spiraling community norms. Many feared retaliation from perpetrators if they spoke out. This fear was compounded by their perception that police ignored criminal activity in AA communities and, therefore, were not a resource that could be utilized to help maintain order. In addition, dilapidated and abandoned houses and buildings, remnants of a hurricane seven years prior, served as visible symbols of community disorder. These structures became venues where individuals could engage unabated in drug use and prostitution—behaviors which increased HIV risk.
Civic Engagement
Participants noted that the expression of community concerns and the utilization of informal networks to address important issues traditionally occur in religious settings, particularly AA churches. However, participants perceived that churches are not good sources of support or activism for HIV prevention due to their reluctance to talk about or participate in HIV-related activities. HIV is considered to be a ‘gay disease’ by many religious leaders who preach against homosexuality and pre-marital sex. Such sentiments served to alienate some individuals and make it harder to access the myriad resources inherent within churches.
DISCUSSION
In this study, FG participants and KIs described four main themes relevant to how a social network model emphasizing the impact of differential social capital on health disparities and outcomes can be used when considering community-based interventions to address disparities in HIV risk—interpersonal processes, community structural environment, social disorder and civic engagement. Our findings have several implications for how social network models and community participation in research might inform HIV risk reduction interventions in rural AA communities.
Emergent themes from our data suggest several considerations and targets for community-based interventions to reduce HIV risk in rural AA communities. Small rural communities may offer the advantage of strong networks between individuals, which may facilitate sharing of knowledge and other health-related resources. However, these same networks may serve to marginalize and exclude certain individuals (i.e. those considered ‘at risk’ for HIV). Insufficient numbers of positive role models and constructive social outlets were felt to increase HIV risk indirectly through engagement in risky behaviors to combat feelings of isolation. These dynamics suggest that interventions to reduce HIV risk behaviors which capitalize on network cohesion and include peer education and mentoring may be efficacious.
HIV-related stigma in rural predominantly AA communities is rampant and perpetuated by some religious organizations and leaders. This finding has implications for whom researchers can partner and the approach that must be taken when designing interventions to improve access to HIV-related services. Novel strategies are needed to lessen the stigma associated with attending certain types of health facilities in order to reduce access-related barriers. For example, mobile units which provide various health- and non-health-related services (e.g., HIV testing and counseling, education and testing for other health conditions, and information on social services) may be beneficial.
Our findings related to the effect of community structural forces on the development and exercise of social capital is illustrative of the dynamic interplay between individuals and their communities. Neighborhood poverty, lack of skilled jobs, poor housing conditions, segregation, and political disenfranchisement were perceived by respondents to contribute to higher rates of HIV among AAs through their influence on individuals’ health behaviors and on the availability and accessibility of community resources. Consistent with other studies, these suggest that variability in social determinants of health is a significant source of health disparities among AAs and inequities in contextual factors must be eliminated if health disparities are to be effectively addressed.27–29 Therefore, interventions to reduce HIV risk in AAs should target factors operant outside the health care system. Concentrated and sustained efforts may be required to address neighborhood segregation and institutionalized racism that fuel HIV risk. Individuals designing HIV prevention interventions should consider using CBPR approaches whereby community and academic partners work together to identify problems and design solutions. Interventions employing these approaches might be more successful and sustainable because they are informed by those most affected and are more likely to address context-specific influences on risk.
We focused on how social capital influences HIV risk in two rural U.S. counties. Previous studies examined the role of social capital in HIV.10,30–32 However, these studies relied on social capital measures that reflect only social cohesion, civic participation, norms of reciprocity, and trust between individuals. These measures have limited relevance for understanding how the social environment influences health disparities because they only tap relational aspects of social capital without considering the material and political aspects. Furthermore, few of these studies emphasize how social capital unfolds to influence risk in U.S. rural communities. Although we applied a specific model to explain disparities in HIV, this model and our qualitative approach can be successfully applied to understand disparities in other conditions and inform community-based intervention development.
Our study illustrates how different conceptualizations of social capital examined in isolation can yield contradictory results. Had we only considered social cohesion as our measure of social capital, we might surmise that high social capital was related to HIV risk. Likewise, had we only examined social capital resources, we would have found that low levels of social capital were associated with HIV risk. However, by simultaneously considering the influence of community structural features, we see that complex forces act synergistically to negate the positive effects of social cohesion and limit individuals’ ability to develop or exercise social capital. Our findings are consistent with theory and empiric research suggesting that social capital can have negative as well as positive consequences.4,33
Our findings have implications for clinical practice and patient education. In clinical settings, providers generally focus on individual-level HIV risk behaviors, such as not using condoms, intravenous drug use, or having concurrent sexual partners. In taking a “social history,” physicians should question the availability of support and local community resources, since communities may differ in their capacity to support individuals in avoiding high-risk behaviors. Physicians should consider using this information to tailor patients’ treatment recommendations. Such an approach may potentially improve patient adherence and clinical outcomes. Integration of case management services into primary care practices may help patients identify and access various health-promoting community resources, thereby potentially improving care delivery and health outcomes. To combat HIV-related stigma, physicians should follow the Centers for Disease Control recommendations for universal HIV testing of all individuals aged 13–64 who visit health care settings.34 Patient education about HIV prevention should extend to non-traditional settings, such as prisons and jails, and continue through re-entry into the community since immediate release from these facilities represents one of the greatest risk periods for injection drug use and risky sexual behavior.35,36
This study has notable limitations. We sampled participants from two rural counties in one state and only included AAs in our FGs, thereby limiting external validity to other groups and settings. We did not query respondents about their specific HIV risk behaviors or objectively measure their HIV status.
Our study has several strengths. A large sample size and triangulation of data from FG participants and KIs provide a rich understanding of how social capital influences HIV risk in the target communities. Use of a qualitative approach guided by a strong theoretical model for examining this issue is novel. We examined the interface between communities which provide the structure that positively or negatively influences disease risk and individuals who are bound by and help shape that structure. Consequently, we have a better understanding of how individual and community level factors interact to influence health behaviors which fuel HIV-related disparities. This work can inform the development of effective interventions which target multi-level HIV determinants to lower HIV risk among AAs in rural communities.
CONCLUSION
We used qualitative methods to understand how a specific social network model, which captures the dynamic interplay between individual and community factors, might inform community-based interventions to reduce HIV risk in rural AA communities. Cohesiveness between individuals may help mitigate HIV risk (e.g. through sharing of resources). However, it may not be sufficient for lowering HIV risk when coupled with community-level disadvantage, neighborhood segregation and institutionalized racism—factors which may constrain individuals’ rational choices and facilitate engagement in high risk behaviors. Although clinicians may have little direct control over the community-level factors that influence an individual patient's HIV risk, they should have a multi-faceted understanding of factors which influence HIV risk from the patient’s perspective. Such understanding may result in the delivery of more “patient-centered care”—care which considers patients’ illness experiences within a broader biopsychosocial framework.
Acknowledgements
We would like to acknowledge the contributions of all steering committee members in the development of Project GRACE Consortium: Larry Auld, Reuben Blackwell, Hank Boyd, III, John Braswell, Angela Bryant, Cheryl Bryant, Don Cavellini, Trinette Cooper, Dana Courtney, Eugenia Eng, Jerome Garner, Vernetta Gupton, Davita Harrell, Shannon Hayes-Peaden, Stacey Henderson, Doris Howington, Clara Knight, Gwendolyn Knight, Taro Knight, Patricia Oxendine-Pitt, Donald Parker, Reginald Silver, Doris Stith, Jevita Terry, and Cynthia Worthy. We would also like to thank the three anonymous reviewers, Dr. Amina Chaudhry, Dr. Karran Phillips, and Mr. R.H. Wright for their helpful comments on this manuscript. We would especially like to thank the assigned Deputy Editor for her very detailed and thoughtful comments which strengthened this manuscript tremendously.
This work was funded by grants from the National Center on Minority Health and Health Disparities (R24MD001671) and The University of North Carolina Center for AIDS Research (UNC CFAR P30 AI50410). Dr. Corbie-Smith is a Health Disparities Scholar with the National Center on Minority Health and Health Disparities. Drs. Cené and Akers received support as funded scholars through the Clinical Translational Science Award-K12 Scholars Program (KL2). The CTSA is a national consortium with the goal of transforming how clinical and translational research is conducted, ultimately enabling researchers to provide new treatments more efficiently and quickly to patients. Drs. Cené and Aker’s work on this project was supported by award number KL2RR025746 and KL2 RR024154-0, respectively from the National Center for Research Resources, a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Dr. Powell Hammond is supported by the National Center for Minority Health and Health Disparities (Award # 1L60MD002605-01), National Cancer Institute (Grant # 3U01CA114629-04 S2) and a developmental award from the UNC Center for Aids Research Award (CFAR P30 AI50410).
The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding agencies. This paper was presented at the 32th Annual Meeting of the Society of General Internal Medicine, May 14, 2009, Miami, Florida.
Conflicts of Interest None disclosed.
REFERENCES
- 1.Institute of Medicine, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. 2002.
- 2.Shaw M, Dorling D, Smith GD. Poverty, social exclusion, and minorities. In: Marmot M, Wilkinson RG, editors. Social determinants of health. 2. Oxford: Oxford University Press; 2006. pp. 196–223. [Google Scholar]
- 3.Nazroo JY, Williams DR. The social determination of ethnic/racial inequalities in health. In: Marmot M, Wilkinson RG, editors. Social determinants of health. 2. Great Britain: Oxford University Press; 2006. pp. 238–266. [Google Scholar]
- 4.Bourdieu P. The handbook of theory and research for the sociology of education. In: Richardson JG, editor. The forms of capital. New York: Greenwood Press; 1986. pp. 241–258. [Google Scholar]
- 5.Coleman JS. Social Capital in the Creation of Human Capital. AJS. 1988;94(Supplement):S95-S120.
- 6.Putnam RD. Bowling alone: America’s declining social capital. JOD. 1995;6(1):65–78. [Google Scholar]
- 7.Hsieh CH. A concept analysis of social capital within a health context. Nurs Forum. 2008;43(3):151–159. doi: 10.1111/j.1744-6198.2008.00107.x. [DOI] [PubMed] [Google Scholar]
- 8.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–1498. doi: 10.2105/AJPH.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawachi I, Kennedy BP, Glass R. Social capital and self-rated health: a contextual analysis. Am J Public Health. 1999;89(8):1187–1193. doi: 10.2105/AJPH.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holtgrave DR, Crosby RA. Social capital, poverty, and income inequality as predictors of gonorrhea, syphilis, chlamydia and AIDS case rates in the United States. Sex Transm Infect. 2003;79(1):62–64. doi: 10.1136/sti.79.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Semaan S, Sternberg M, Zaidi A, Aral SO. Social capital and rates of gonorrhea and syphilis in the United States: spatial regression analyses of state-level associations. Soc Sci Med. 2007;64(11):2324–2341. doi: 10.1016/j.socscimed.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 12.Almedom AM. Social capital and mental health: an interdisciplinary review of primary evidence. Soc Sci Med. 2005;61(5):943–964. doi: 10.1016/j.socscimed.2004.12.025. [DOI] [PubMed] [Google Scholar]
- 13.Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental illness: a systematic review. J Epidemiol Community Health. 2005;59(8):619–627. doi: 10.1136/jech.2004.029678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Islam MK, Merlo J, Kawachi I, Lindstrom M, Gerdtham UG. Social capital and health: does egalitarianism matter? A literature review. Int J Equity Health. 2006;5:3. doi: 10.1186/1475-9276-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Macinko J, Starfield B. The utility of social capital in research on health determinants. Milbank Q. 2001;79(3):387-427, IV. [DOI] [PMC free article] [PubMed]
- 16.Pitkin Derose K, Varda DM. Social capital and health care access: a systematic review. Med Care Res Rev. 2009;66(3):272-306. [DOI] [PMC free article] [PubMed]
- 17.Holtgrave DR, Crosby R. Is social capital a protective factor against obesity and diabetes? Findings from an exploratory study. Ann Epidemiol. 2006;16(5):406–408. doi: 10.1016/j.annepidem.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 18.Crosby RA, Holtgrave DR, DiClemente RJ, Wingood GM, Gayle JA. Social capital as a predictor of adolescents' sexual risk behavior: a state-level exploratory study. AIDS Behav. 2003;7(3):245–252. doi: 10.1023/A:1025439618581. [DOI] [PubMed] [Google Scholar]
- 19.Carlson ED, Chamberlain RM. Social capital, health, and health disparities. J Nurs Scholarsh. 2003;35(4):325–331. doi: 10.1111/j.1547-5069.2003.00325.x. [DOI] [PubMed] [Google Scholar]
- 20.Carpiano RM. Neighborhood social capital and adult health: an empirical test of a Bourdieu-based model. Health Place. 2007;13(3):639–655. doi: 10.1016/j.healthplace.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Baum F, Palmer C. 'Opportunity structures': urban landscape, social capital and health promotion in Australia. Health Promot Int. 2002;17(4):351–361. doi: 10.1093/heapro/17.4.351. [DOI] [PubMed] [Google Scholar]
- 22.Carpiano RM. Toward a neighborhood resource-based theory of social capital for health: can Bourdieu and sociology help? Soc Sci Med. 2006;62(1):165–175. doi: 10.1016/j.socscimed.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 23.Corbie-Smith G, Adimora A, Youmans S, Muhammad M, Blumenthal C, Ellison A, Akers A, Council B, Thigpen Y, Wynn M, Lloyd S. "Project GRACE: A Staged Approach to Development of a Community-Academic Partnership to address HIV in Rural African American Communities." Health Promotion and Practice. [DOI] [PMC free article] [PubMed]
- 24.Edgecombe County Health Department/Nash County Health Department. Edgecombe county Health Department/Nash County Statistical Analysis Query Report. Retrieved on April 1, 2007.
- 25.NC Rural Economic Development Center. North Carolina Rural Data Bank. http://www.ncruralcenter.org/databank/index.html. Updated 2009. Accessed July, 2010.
- 26.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 27.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med. 1997;44(6):809–819. doi: 10.1016/S0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- 28.American College of Physicians. Racial and ethnic disparities in health care, updated 2010.
- 29.Buffardi AL, Thomas KK, Holmes KK, Manhart LE. Moving upstream: ecosocial and psychosocial correlates of sexually transmitted infections among young adults in the United States. Am J Public Health. 2008;98(6):1128–1136. doi: 10.2105/AJPH.2007.120451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gregson S, Terceira N, Mushati P, Nyamukapa C, Campbell C. Community group participation: can it help young women to avoid HIV? An exploratory study of social capital and school education in rural Zimbabwe. Soc Sci Med. 2004;58(11):2119–2132. doi: 10.1016/j.socscimed.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Pronyk PM, Harpham T, Morison LA, et al. Is social capital associated with HIV risk in rural South Africa? Soc Sci Med. 2008;66(9):1999–2010. doi: 10.1016/j.socscimed.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 32.Campbell C, Williams B, Gilgen D. Is social capital a useful conceptual tool for exploring community level influences on HIV infection? An exploratory case study from South Africa. AIDS Care. 2002;14(1):41–54. doi: 10.1080/09540120220097928. [DOI] [PubMed] [Google Scholar]
- 33.Takahashi LM, Magalong MG. Disruptive social capital: (un)healthy socio-spatial interactions among Filipino men living with HIV/AIDS. Health Place. 2008;14(2):182–197. doi: 10.1016/j.healthplace.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, Clark JE. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. 2006:592–7. [PubMed]
- 35.Khan MR, Wohl DA, Weir SS, et al. Incarceration and risky sexual partnerships in a southern US city. J Urban Health. 2008;85(1):100–113. doi: 10.1007/s11524-007-9237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.MacGowan RJ, Margolis A, Gaiter J, et al. Predictors of risky sex of young men after release from prison. Int J STD AIDS. 2003;14(8):519–523. doi: 10.1258/095646203767869110. [DOI] [PubMed] [Google Scholar]