ABSTRACT
BACKGROUND
The National Heart, Lung and Blood Institute currently defines a blood pressure under 120/80 as “normal.”
OBJECTIVE
To examine the independent effects of diastolic (DBP) and systolic blood pressure (SBP) on mortality and to estimate the number of Americans affected by accounting for these effects in the definition of “normal.”
DESIGN, PARTICIPANTS AND MEASURES
Data on adults (age 25–75) collected in the early 1970s in the first National Health and Nutrition Examination Survey were linked to vital status data through 1992 (N = 13,792) to model the relationship between blood pressure and mortality rate adjusting for age, sex, race, smoking status, BMI, cholesterol, education and income. To estimate the number of Americans in each blood pressure category, nationally representative data collected in the early 1960s (as a proxy for the underlying distribution of untreated blood pressure) were combined with 2008 population estimates from the US Census.
RESULTS
The mortality rate for individuals over age 50 began to increase in a stepwise fashion with increasing DBP levels of over 90. However, adjusting for SBP made the relationship disappear. For individuals over 50, the mortality rate began to significantly increase at a SBP ≥140 independent of DBP. In individuals ≤50 years of age, the situation was reversed; DBP was the more important predictor of mortality. Using these data to redefine a normal blood pressure as one that does not confer an increased mortality risk would reduce the number of American adults currently labeled as abnormal by about 100 million.
CONCLUSIONS
DBP provides relatively little independent mortality risk information in adults over 50, but is an important predictor of mortality in younger adults. Conversely, SBP is more important in older adults than in younger adults. Accounting for these relationships in the definition of normal would avoid unnecessarily labeling millions of Americans as abnormal.
KEY WORDS: blood pressure, hypertension, guidelines, mortality
Physicians have traditionally been taught to think of elevated diastolic blood pressure (DBP) as abnormal. Over 4 decades ago, a VA Cooperative Study was published on the utility of treatment in asymptomatic diastolic hypertension.1 With less than 2 years of follow-up, the randomized trial demonstrated the tremendous value of lowering the pressure of men whose DBP was between 115 and 129 mmHg (1-year risk of death or end-organ damage: 26% control vs. <2% treatment). Subsequent trials demonstrated the smaller benefit of treating milder elevations of DBP.2,3
Almost 2 decades ago, another trial concluded there was also value in treating elevated systolic blood pressure (SBP).4 In 2003, the 7th Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) concluded, in fact, that SBP was more important than DBP in persons over 50 years old.5 JNC 7 went on to define a “normal” blood pressure as a SBP <120 mmHg and a DBP <80.
The definition of normal for any parameter of human health has important implications. Those who are not normal are, by implication, abnormal. Whether or not they are treated, simply labeling individuals as abnormal carries potentially important physical and psychological consequences.6–9 Furthermore, apparently small numerical alterations to narrow the definition of normal can affect literally millions of people.10 If this encourages more treatment, it does so in those individuals for whom clinical benefits are least likely to outweigh treatment harms. And if more people are turned into patients, the financial implications can be enormous: hugely positive for those with an interest in larger markets and hugely negative for those with an interest in containing health care expenditures. Consequently, the definition of normal blood pressure must be made with careful attention to the trade-off between the desire to identify those at substantially higher risk than average and the need to avoid overdiagnosis and overtreatment.
JNC 8 is expected to be released in Fall 2011.11 The panel is beginning to consider data now. In this paper we hope to contribute to that process and the public debate by examining two questions: (1) What is the independent contribution of DBP and SBP on mortality? and (2) How would accounting for these relationships in the definition of normal blood pressure affect the number of Americans currently defined as abnormal?
METHODS
Overview and Rationale for Source Data
To address our first question, we sought a nationally representative cohort study combining detailed intake data (including DBP and SBP) with long-term follow-up data on survival. To minimize the possible confounding effect of hypertension treatment, we were interested in finding the oldest data possible. The first National Health and Nutrition Examination Survey (NHANES I) met these criteria as it enrolled participants in 1971–1976, yet includes approximately 2 decades of follow-up data (via the NHANES I Epidemiologic Followup Study, which continued through 1992). Survival analyses in these data offer not only the opportunity to disentangle the effects of DBP and SBP on mortality, but also an operational definition of normal blood pressure: a range of pressures for which there is no statistically significant increase in long-term mortality risk. We believe that our use of this large, long-term study permits mortality to serve as an unbiased and largely complete estimate of “normality” because if a given DBP or SBP is also associated with major morbidity (e.g., development of new coronary, cerebrovascular or peripheral artery disease events or end-organ damage), a subsequent downstream impact on all-cause mortality should be observed.
To address our second question on the number of Americans affected by various definitions of normal required an inference about underlying (or natural) distribution of untreated blood pressures in American adults. Currently, it is not possible to make such an inference given the prevalence of hypertension treatment. We were able to find, however, a nationally representative survey of American's blood pressures: the first National Health Examination Survey (NHES) performed between 1959 and 1962—an era well before the first publications demonstrating the value of treating asymptomatic hypertension. While we acknowledge that the natural distribution may have shifted in the ensuing decades, we believe this serves as the best proxy of the underlying distribution of untreated blood pressure in American adults.
Blood Pressure and Mortality: NHANES I
A total of 14,407 adults age 25–74 completed NHANES I and were included in the NHANES I Epidemiologic Follow-up Study through 1992. Among these adults, 96.2% (n = 13,861) had complete vital status data. After excluding an additional 69 adults with missing data on SBP or DBP, we arrived at the final primary analytical cohort of 13,792.
Blood pressure was obtained by a physician at the beginning of the physical examination while the subject was in a sitting position.12 In addition, nurses obtained two repeated measurements at the end of the examination in a subset of subjects (n = 6,839). The nurse's measurement largely corroborated the physician's (nurse's systolic blood pressures were an average of 1.5 mmHg lower, whereas their diastolic blood pressures were on average 1 mmHg higher). Systolic blood pressure was then categorized into seven levels ranging from <100 to ≥200—with five 20-mmHg increments in between. Diastolic blood pressure was categorized into eight levels ranging from <60 to ≥120—with six 10-mmHg increments in between.
The outcome of interest was the observed all-cause mortality rate for a given blood pressure category relative to that for a so-called “normal” blood pressure: less than 120/80. To avoid the inclusion of abnormally low pressures, our referent category for SBP was 100–119 mmHg, whereas our referent category for DBP was 70–79 mmHg.
We also adjusted for a number of potential confounders. Age was coded as a continuous variable. Smoking was categorized as current, never and former. Weight and height were used to calculate BMI (kg/m2), and BMI was categorized into 11 levels from ≤18 to >34 with eight 2-kg/m2 increments in between and one level for those with missing weight or height data. Total cholesterol was categorized into 13 levels from <120 to ≥320 with ten 20-mg/dl increments in between and one level for those with missing cholesterol data. Education was categorized into 19 levels for years of education including a level for those missing education data. Income was categorized into 12 levels including a level for those missing income data. Race was categorized as Native American, Asian/Pacific Islander, Black, White or Other.
We estimated the rate of death using Cox regression for systolic or diastolic blood pressure categories both adjusted and unadjusted for each other. Based on the findings of the JNC 7 report, separate analyses were performed in persons above and below age 50.5 All models were adjusted for age, sex, smoking status, BMI, total cholesterol, education, income and race. An additional sensitivity analysis stratified results by baseline income.
Population Distribution of Blood Pressure: NHES
A total of 7,710 adults were included in the National Health Examination Survey (NHES), 6,672 of whom were examined during the period from October 1959 to December 1962. Data from this cohort was used to estimate the proportion of the population in various blood pressure categories prior to the advent of widespread therapy. We estimated the blood pressure distribution for each of six 10-year age strata (20–29 through 70–79). To incorporate the NHES sampling strategy, the accompanying survey weights were used to estimate these proportions. We then obtained 2008 population estimates from the US Census13 for each age stratum to estimate the number of Americans currently within each blood pressure category. All analyses were conducted using SAS version 9.1 (SAS Institute Inc., Cary, NC).
RESULTS
Table 1 shows the distribution of the 13,792 participants in each age-blood pressure cell. The table also shows the distribution for the 4,572 deaths. The smallest number of deaths among the elevated blood pressure categories was 96 in those over age 50 (DBP ≥120) and 19 in those age 50 and younger (SBP ≥200).
Table 1.
Number of Participants and Deaths in Each Age-Blood Pressure Cell in NHANES I
| Category | Number of participants | Number of deaths | ||
|---|---|---|---|---|
| Age >50 | Age ≤50 | Age >50 | Age ≤50 | |
| Diastolic BP | ||||
| <60 | 50 | 112 | 39 | 8 |
| 60–69 | 309 | 832 | 204 | 31 |
| 70–79 | 1,277 | 2,110 | 731 | 122 |
| 80–89 | 2,148 | 2,514 | 1,236 | 211 |
| 90–99 | 1,600 | 1,158 | 956 | 130 |
| 100–109 | 703 | 370 | 466 | 75 |
| 110–119 | 263 | 147 | 197 | 35 |
| ≥120 | 124 | 75 | 96 | 35 |
| Total | 6,474 | 7,318 | 3,925 | 647 |
| Systolic BP | ||||
| <100 | 42 | 295 | 25 | 14 |
| 100–119 | 683 | 2,647 | 317 | 139 |
| 120–139 | 1,850 | 3,062 | 953 | 269 |
| 140–159 | 2,015 | 961 | 1,263 | 126 |
| 160–179 | 1,167 | 248 | 792 | 59 |
| 180–199 | 466 | 74 | 370 | 21 |
| ≥200 | 251 | 31 | 205 | 19 |
| Total | 6,474 | 7,318 | 3,925 | 647 |
| 13,792 | 4,572 | |||
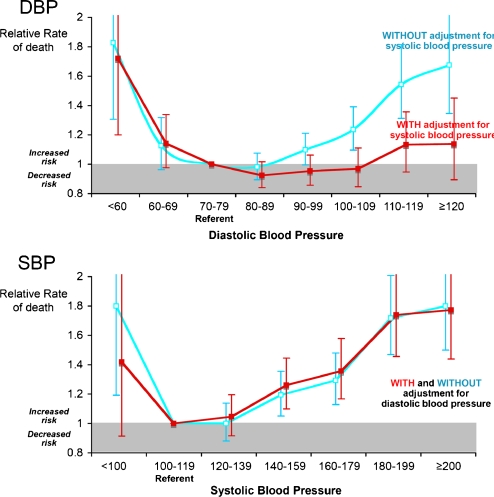
Persons over Age 50
Figure 1 shows the relative mortality rate associated with various blood pressure categories in those over age 50. Overall, there appeared to be a J-shaped association, such that the lowest and highest blood pressures were associated with the greatest rates of death. Without adjusting for SBP, the rate of death (relative to a DBP of 70–79) began to increase at a DBP of 90–99 (RR = 1.10; 95% CI 1.00–1.21) and subsequently increased in a step-wise fashion: DBP 100–109 (RR = 1.24; 95% CI 1.10–1.39), DBP 110–119 (RR = 1.54; 95% CI 1.31–1.82) and DBP ≥120 (RR = 1.68; 95% CI 1.35–2.09). The relationship between elevated DBP and mortality almost completely disappeared, however, when we adjusted for SBP.
Figure 1.
Blood pressure and mortality risk in persons over age 50. DBP/SBPs are from a single, sitting measurement; the outcome is the RR for all-cause mortality relative to a person with a DBP 70–79 or SBP 100–119. All analyses are controlled for age, sex, race, current and former smoking, BMI, cholesterol, education and income.
While the relationship between DBP and mortality was dramatically dampened by adjusting for SBP, the relationship between SBP and mortality was virtually unaffected by adjusting for DBP. With or without adjustment for DBP, SBPs above 140 were associated with significant increases in mortality.
A secondary analysis examined the question: Among persons over age 50 whose SBP is less than 140, what is the effect of having abnormal diastolic blood pressure (as currently defined)? In this subgroup, there was no significant difference in the relative rate of death in persons with DBP ≥80 relative to those with DBP <80 (RR = 0.91; 95% CI 0.81–1.02).
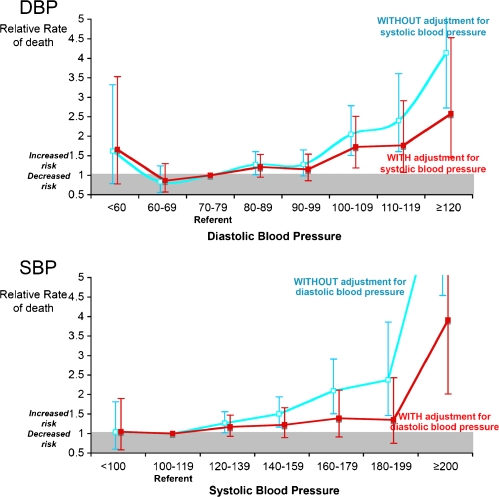
Persons Age 50 and Younger
Figure 2 shows the mortality risk associated with various blood pressure categories in those age 50 and younger. Note that the y-axis (relative rate of death) scale has changed—because, in this younger age group, extreme blood pressure elevations have a more dramatic relative effect on a low absolute risk of death. Although adjustment for SBP had some effect on the point estimates for the relative rate of death, it had no effect on the threshold for increased risk. With or without adjustment for SBP, DBPs above 100 were associated with significant increases in mortality.
Figure 2.
Blood pressure and mortality risk in persons age 50 and younger. DBP/SBPs are from a single, sitting measurement; the outcome is the RR for all-cause mortality relative to a person with a DBP 70–79 or SBP 100–119. All analyses are controlled for age, sex, race, current and former smoking, BMI, cholesterol, education and income.
Adjustment for DBP, however, did influence the assessment of SBP in this younger age group. Without adjusting for DBP, the rate of death increased with increasing levels of SBP. The rate of death (relative to a SBP of 110–119) began to increase at a SBP of 120–139 (RR = 1.26; 95% CI 1.02–1.56) and subsequently increased in a step-wise fashion: SBP 140–159 (RR = 1.50; 95% CI 1.16–1.94), SBP 160–179 (RR = 2.09; 95% CI 1.51–2.91), SBP 180–199 (RR = 2.38; 95% CI 1.46–3.86) and SBP ≥200 (RR = 7.67; 95% CI 4.54–12.98). Adjusting for DBP, however, made all but the most extreme relationship disappear: SBP ≥200 (RR = 3.91; 95% CI 2.02–7.58).
A secondary analysis examined the question: Among persons age 50 and younger whose DBP was less than 100, what is the effect of having a systolic blood pressure elevation between 140 and 200? In this subgroup, there was no significant difference in the relative rate of death in persons with SBP 140–200 relative to those with SBP <140 (RR = 1.26; 95% CI 0.99–1.58).
Estimates of the Number Affected by Various Definitions
Table 2 provides estimates of the number of adult Americans affected by various definitions of abnormal blood pressure. Using the current definition of normal blood pressure (less than 120/80) about 60 million are labeled normal and about 160 million are labeled abnormal. Using an operational definition of normal—one that does not confer an increased long-term mortality risk (in these NHANES data)—the situation would be reversed: about 160 million would be labeled normal and about 60 million would be labeled abnormal. In other words, the choice about the approach used to define normal blood pressure could affect about 100 million Americans.
Table 2.
Estimates of the Number of Adult Americans Affected by Varying Definitions of “Normal” Blood Pressure (Based on the Natural Distribution of Blood Pressures in 1959)
| Proportion of 1959 population | Estimated number in category in 2008 | |
|---|---|---|
| Over age 50 | ||
| Current definition of normal | 11.3% | 10,100,000 |
| (SBP <120, DBP <80) | ||
| Arguably normal | 33.9% | 30,700,000 |
| No evidence of statistically significant increase in morality risk | ||
| (120≤ SBP <140, any DBP) | ||
| Unambiguous increased risk | 54.8% | 53,300,000 |
| (SBP ≥140) | ||
| Age 50 and younger | ||
| Current definition of normal | 42.1% | 52,000,000 |
| (SBP <120, DBP <80) | ||
| Arguably normal | 54.4% | 70,500,000 |
| No evidence of statistically significant increase in morality risk | ||
| (120≤ SBP <200, 80≤ DBP <100) | ||
| Unambiguous increased risk | 3.5% | 4,800,000 |
| (SBP ≥200, DBP ≥100) | ||
| Total | ||
| Current definition of normal | 31.9% | 62,100,000 |
| Arguably normal | 47.6% | 101,200,000 |
| Unambiguous increased risk | 20.5% | 58,100,000 |
The percentage distribution in the second column does not exactly match the count distribution in the third column as the age structure of the population has changed. The counts in the third column are the sum of counts calculated using the 1959 distribution and 2008 population estimates within 10-year age groups
COMMENT
Our examination of the independent effects of diastolic and systolic blood pressure on mortality confirms a central tenet of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC 7): systolic blood pressure elevations are more important than diastolic blood pressure elevations in persons over age 50. In fact, in our data, diastolic blood pressures are largely irrelevant in this age group. The situation was reversed in persons age 50 and younger: in whom diastolic blood pressure was the more important predictor of mortality.
Our analysis was also directed at a broader question that we hope JNC 8 will consider in its ongoing deliberations: What is the impact of various definitions of normal blood pressure? The current definition of normal is less than 120/80. Our analysis offers one possible alternative definition: a blood pressure that does not confer an increased mortality risk in a cohort of over 10,000 individuals followed for nearly 20 years. From our data this would mean that abnormal for individuals over age 50 would be a SBP of ≥140 (independent of DBP), and for individuals less than 50, a DBP ≥100 or a SBP ≥200. While it should not be viewed as the final word on this topic, we hope it serves as an example of an alternative approach. If nothing else, our findings highlight that the choice about the approach used to define normal blood pressure will impact literally millions of Americans.
Limitations
Our analysis has a number of limitations. The most obvious is that we have no data about treatment. It is possible that subsequent treatment might attenuate the relationship between elevated blood pressure and mortality. Given this concern, we sought the oldest data possible—when blood pressure treatment was less widespread. And within our data there is evidence that suggests treatment explains little of what we observed.
Because patients were enrolled in the early 1970s, any treatment that occurred would have been directed at elevations in diastolic blood pressure. Nevertheless our analysis of the effect of diastolic blood pressure (without adjustment for systolic blood pressure) shows a strong dose-response relationship. Were higher diastolic blood pressures more likely to have been successfully treated, one would have expected this relationship to be much flatter. Furthermore, we performed an additional analysis focusing on the best available proxy for the absence of treatment: that of having little income. When we restricted our analysis to those with family incomes of less than $10,000 per year (approximately $50,000 or less in today's dollars), we identified exactly the same blood pressure categories as being associated with significant increases in mortality.
Our findings do not include reductions in quality of life due to cardiovascular morbidity not directly associated with a decrease in years of life. The exact magnitude or proportion is not well known, nor is the corresponding impact this would have on treatment decision making (i.e., the decision to treat a patient to reduce cardiovascular complications even if there was no reduction in mortality). Practically speaking, however, it is important to point out that all-cause mortality and cardiovascular mortality are highly correlated—a finding confirmed in data from over 300,000 men enrolled in the Multiple Risk Factor Intervention Trial (MRFIT).14 Furthermore, the largest meta-analysis of 1 million adults from 61 prospective observational studies also found that non-vascular causes of death were positively related to blood pressure.15 Given that our data are based on exceptionally long-term follow-up, that approximately one-third of individuals died, including almost two-thirds of those over age 50, and the known close association of cardiovascular events with all-cause mortality, we believe that clinically meaningful cardiovascular morbidity (and the corresponding decrement in quality of life) and mortality should have been largely captured in our measurement of all-cause mortality.
Furthermore, we believe there is a strong theoretical argument for using all-cause mortality as the primary outcome. First, it is the least ambiguous outcome measure. Because the fact of death can be unambiguously ascertained, it is the outcome least subject to measurement bias. Second, all-cause mortality is the most comprehensive measure of the mortality impact of a condition. Because it is comprehensive, it avoids having to assume no relationship between one form of death and another—and thus avoids the potential problem of either underestimating risk (e.g., failing to recognize that elevated blood pressure might be associated with non-cardiovascular deaths) or overestimating it (e.g., failing to recognize that there might be a trade-off between cardiovascular deaths and non-cardiovascular deaths).16
Policy Implications
Because they are based on one dataset, our findings by themselves are insufficient to develop policy. We would hope others would reconsider the question of what constitutes normal blood pressure using other datasets. We also recognize that our approach for defining normal adds an additional complexity to the current approach because it is modified by age (SBP less than 140 for those over age 50 and a blood pressure under 200/100 for those age 50 and younger). But even a small simple expansion in the definition of normal—from under 120/80 to under 140/90—would have a tremendous impact: affecting about 80 million Americans.
The current approach to define normal as less than 120/80 is presumably based on detectable increases in risk above that level. But there are always bound to be small, detectable effects if we study enough people. And the threshold to label individuals as “abnormal” ought to require more than simply any detectable effect, in any outcome, in any size sample.
The reason is because there are costs associated with labeling people as abnormal. There are human costs: both for the people who have been turned into patients (and who have been informed that they are now more vulnerable to disease) and for the clinicians who are increasingly overwhelmed by the number of diagnoses they face (arguably distracting them from the patients who need them most). There are also the tremendous logistical and financial costs associated with millions of new diagnoses—a cost that may be even larger in this country to the extent it impedes progress toward universal access.
Finally, there is the problem of excessive treatment. Regardless of what is recommended, the tendency of clinicians will increasingly be to treat lower blood pressures to make them “normal.” When abnormal is defined to include values in which the risk itself is ambiguous, the ability of treatment to change that risk becomes even less certain. In the absence of randomized trials demonstrating the benefit of intervening in this grey area, we urge caution in suggesting that individuals are abnormal (and, in doing so, inadvertently encouraging more intervention). But the most important concern may be the potential for harm. Careful readers have likely already noted the increased mortality associated with very low blood pressures in those over age 50. Much of this effect undoubtedly reflects individuals with low blood pressure because of underlying cardiovascular disease or poor health status. However, given the recent finding that increased all-cause mortality may be higher with tight blood pressure control in hypertensive patients with diabetes,17 it may also reflect the risk some individuals may face if they are excessively treated. The finding of increased mortality following intensive glucose lowering18 is another example that refutes the previously held notion that achieving lower (whether it is glucose levels or blood pressure measurements) will necessarily improve mortality and should, at least, encourage clinicians to consider the possibility that intensive blood pressure lowering may not be helpful or necessary, and in fact could be hazardous for patients in general. The potential harm would seem to be greatest in patients whose baseline blood pressure is near normal.
At some point, it becomes incumbent on consensus panels (like JNC 8) to consider these trade-offs in their definition of normal. The fundamental question is how much of an effect is worth worrying the population about and experiencing the associated costs? To do this, they may well need to consider unfamiliar questions, such as: If we cannot reliably see a mortality effect in a large group of individuals followed for nearly 20 years, should we define the condition as abnormal? We believe considering this kind of approach represents a critical step in ensuring that diagnoses are given only to those with a meaningful elevation in risk and that interventions are targeted towards individuals most likely to benefit.
ACKNOWLEDGEMENTS
This material received no direct funding, but is the result of work supported with resources and the use of facilities at the Minneapolis and White River Junction VA Medical Centers. The views expressed herein do not necessarily represent the views of the Department of Veterans Affairs or the United States Government.
Conflicts of Interest None disclosed.
REFERENCES
- 1.Veterans Administration Cooperative Study Group on Antihypertensive Agents Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202(11):1028–1034. doi: 10.1001/jama.202.11.1028. [DOI] [PubMed] [Google Scholar]
- 2.Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mmHg. JAMA 1970; 213(7):1143–1152. [PubMed]
- 3.Neaton JD, Grimm RH, Jr, Prineas RJ, Stamler J, Grandits GA, Elmer PJ, Cutler JA, Flack JM, Schoenberger JA, McDonald R. Treatment of mild hypertension study. Final results. Treatment of Mild Hypertension Study Research Group. JAMA. 1993;270(6):713–724. doi: 10.1001/jama.270.6.713. [DOI] [PubMed] [Google Scholar]
- 4.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991; 265(24):3255–3264. [PubMed]
- 5.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 6.Bergman AB, Stamm SJ. The morbidity of cardiac nondisease in schoolchildren. N Engl J Med. 1967;276(18):1008–1013. doi: 10.1056/NEJM196705042761804. [DOI] [PubMed] [Google Scholar]
- 7.Macdonald LA, Sackett DL, Haynes RB, Taylor DW. Labelling in hypertension: a review of the behavioural and psychological consequences. J Chronic Dis. 1984;37(12):933–942. doi: 10.1016/0021-9681(84)90070-5. [DOI] [PubMed] [Google Scholar]
- 8.Cadman D, Chambers LW, Walter SD, Ferguson R, Johnston N, McNamee J. Evaluation of public health preschool child developmental screening: the process and outcomes of a community program. Am J Public Health. 1987;77(1):45–51. doi: 10.2105/ajph.77.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feldman W. How serious are the adverse effects of screening? J Gen Intern Med. 1990;5(5 Suppl):S50–S53. doi: 10.1007/BF02600842. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz LM, Woloshin S. Changing disease definitions: implications for disease prevalence. Analysis of the Third National Health and Nutrition Examination Survey, 1988-1994. Eff Clin Pract. 1999;2(2):76–85. [PubMed] [Google Scholar]
- 11.National Heart, Lung, and Blood Institute (NHLBI) National Institutes of Health. The Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8). Available at: http://www.nhlbi.nih.gov/guidelines/hypertension/jnc8/index.htm. Accessed January 14, 2011. [PubMed]
- 12.CDC National Center for Health Statistics' website. Public Use Data Tape Documentation: Medical Examination: National Health and Nutrition Examination Survey, 1971–75. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanesi/4233.pdf. Accessed January 14, 2011.
- 13.U.S.Census Bureau. Annual Estimates of the Resident Population by Sex and Five-Year Age Groups for the United States: April 1, 2000 to July 1, 2008. Available at: http://www.census.gov/popest/national/asrh/NC-EST2008-sa.html. Accessed January 14, 2011.
- 14.Rutan GH, Kuller LH, Neaton JD, Wentworth DN, McDonald RH, Smith WM. Mortality associated with diastolic hypertension and isolated systolic hypertension among men screened for the Multiple Risk Factor Intervention Trial. Circulation. 1988;77(3):504–514. doi: 10.1161/01.cir.77.3.504. [DOI] [PubMed] [Google Scholar]
- 15.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. doi: 10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 16.Hulley SB, Walsh JM, Newman TB. Health policy on blood cholesterol. Time to change directions. Circulation. 1992;86(3):1026–1029. doi: 10.1161/01.cir.86.3.1026. [DOI] [PubMed] [Google Scholar]
- 17.Cooper-Dehoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, Pepine CJ. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304(1):61–68. doi: 10.1001/jama.2010.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gerstein HC, Miller ME, Byington RP, Goff DC, Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH, Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–2559. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]