Abstract
OBJECTIVE
The shortage of radiologists in breast imaging may be related to heightened malpractice lawsuit concerns. Our objective was to examine radiologists' reported experiences and perceptions of future lawsuit risk and explore personal and professional factors that may be associated with elevated perceptions of risk.
MATERIALS AND METHODS
Radiologists who routinely interpret mammography examinations in diverse regions of the United States (Washington, Colorado, and New Hampshire) completed a mailed survey in 2002 and 2006, including questions on demographics, practice characteristics, and medicolegal experience and perceptions as well as a validated scale measuring reactions to uncertainty in clinical situations. A survey assessing the radiologists' work facilities was also completed in 2002.
RESULTS
Participation by eligible radiologists was 77% (139 of 181) in 2002 and 71% (84 of 118) in 2006. The percentage of radiologists reporting malpractice claims related to mammography in the previous 5 years was 8% on the 2002 survey and 10% on the 2006 survey. Radiologists' mean estimate of the probability of being sued for malpractice in the next 5 years (41% in 2002 and 35% in 2006) was markedly higher than the actual reported risk. Radiologists' age, sex, clinical experience, and workload were not associated with a higher perceived risk of being sued. Radiologists who reported higher perceived risk of lawsuits were more likely to have experienced a prior malpractice claim, to report knowing colleagues with prior lawsuits, and to score higher on a scale measuring anxiety caused by uncertainty in clinical situations. Radiologists working at facilities that did not use double reading reported higher perceived risk, but the difference was not statistically significant.
CONCLUSION
Radiologists working in breast imaging substantially overestimate their risk of a future malpractice lawsuit. Radiologists with higher risk perceptions show more negative reactions to uncertainty in a clinical setting. Understanding that their actual risk of malpractice lawsuits may be substantially lower than anticipated may help reduce radiologists' fears and alleviate the manpower shortage in mammography. Programs to address the shortage of breast imagers could be targeted toward radiologists with heightened malpractice lawsuit concerns.
Keywords: mammography, medical malpractice risk
The interpretation of mammograms has been especially vulnerable to medical malpractice litigation. Because more than two thirds of radiologists do at least some breast imaging, the number of radiologists at risk is immense [1]. In 1990, a study by the Physicians Insurers Association of America (PIAA), a large consortium of physician-owned liability carriers, indicated that delay in diagnosis of breast cancer was the second most common reason that physicians were subject to malpractice lawsuits [2]. The PIAA repeated the study in 1995 and 2002, noting that delay in breast cancer diagnosis had become the most common reason for medical malpractice lawsuits filed in the United States [2, 3]. In the PIAA's 2002 study, the most commonly named defendant in such lawsuits was the interpreting radiologist. Although legal cases involving neurologically impaired newborns have the highest aggregate indemnity awards, payments related to breast cancer are the second highest, with an average payment of $438,047 in the 2002 report [2].
Concerns about malpractice litigation may have a detrimental effect on health care delivery. Fear of litigation was among the leading reasons cited by radiologists for their declining interest in specializing in mammography [4, 5]. This fear has also caused more than one third of practicing radiologists to consider leaving the field of breast imaging [6]. Over a recent 3-year period, the number of physicians interpreting mammograms decreased by 5% despite an increase in the number of women undergoing mammography [7].
In previous work using survey data from 2002, we assessed the relationship between radiologists' perception of the likelihood they would be sued for medical malpractice and their interpretive performance in mammography. Although radiologists are understandably concerned about mammography-related litigation, their perception of the risk of future lawsuits in the next 5 years was noted to be quite high in the 2002 survey [6]. We surveyed these same radiologists again in 2006 and thus can now compare their 2002 risk estimates with actual rates of malpractice suits filed against them. When radiologists' perceived risk of lawsuits sufficiently exceeds their real risk, an opportunity arises to better educate them about the medicolegal environment and potentially diminish the worsening manpower shortage. Such education depends in part on being able to characterize those radiologists with the highest perceived risk of litigation. For example, emerging research suggests that radiologists' attitudes about uncertainty in clinical medicine may be associated with their interpretive performance [8–10]. Yet few studies have explored the connection between physician characteristics such as sociodemographics or attitudes about malpractice and their perceived risk of litigation, and none of these prior studies have focused exclusively on radiologists [11, 12]. In addition, no prior studies, to our knowledge, have explored longitudinal trends in physicians' malpractice attitudes.
In this article, we link the 2002 survey results with results of the follow-up survey of radiologists performed in 2006. We describe the prevalence in 2002 and 2006 of legal claims and attitudes about litigation among radiologists working in breast imaging and explore radiologists' characteristics and practice patterns associated with elevated perceptions of malpractice lawsuit risk.
Materials and Methods
Study Design
This community-based, multicenter, observational study involves collaboration among radiologists in diverse regions in the United States participating in the Breast Cancer Surveillance Consortium (BCSC) [13]. Data were obtained from radiologists working in these BCSC registries via a mailed survey and obtained from the BCSC facilities at which these radiologists interpret mammograms [6, 14].
All radiologists interpreting mammograms at facilities that participate in one of three mammography registries in Colorado, New Hampshire, and Western Washington were mailed a survey in 2002 and 2006. The survey included questions on demographic characteristics (e.g., age, sex), clinical practice (e.g., experience with mammography, experience with procedures), and perception of and experience with medical malpractice. Specifically, radiologists were asked to rate the following question on a 100-point scale: “What do you think is the probability of a medical malpractice lawsuit being filed in the next 5 years against you if you were to interpret mammograms full time?” Radiologists were also asked to report medical malpractice lawsuits related to mammography and provide a date in which the lawsuit was filed.
The radiologist survey in 2002 also included an instrument assessing reactions to uncertainty in clinical decision making that has been validated among several specialties, including radiologists [8, 15]. The instrument included 10 questions that characterize physicians' reactions to the uncertainty associated with clinical care in three areas: reluctance to disclose mistakes to other physicians, stress from uncertainty in clinical decision making, and concerns about bad outcomes. The questions were each scored using a Likert scale from 1 (strongly disagree) to 6 (strongly agree). The 10 individual questions were modified to make them more relevant to the practice of mammography interpretation, and the psychometric properties remained unchanged [8] (see Appendix 1 for the adapted instrument). The 2006 survey did not contain this instrument on reaction to uncertainty.
After extensive pilot testing, a survey of the BCSC facilities at which the radiologists interpret mammograms was conducted at the time of the 2002 radiologist survey. Information regarding mammography practice collected in the facilities survey included use of double reading by a second radiologist, application of computer-aided detection (CAD) programs, use of an audit report system providing feedback to individual radiologists regarding mammography performance, and for-profit status of the facility [16]. A second facility survey was not conducted in 2006.
Institutional review board (IRB) approval for all surveys was obtained from the University of Washington School of Medicine, Group Health Center for Health Studies (Washington), Dartmouth College (New Hampshire), and the Cooper Institute (Colorado). Each registry and the Statistical Coordinating Center have received IRB approval for either active or passive consenting processes or a waiver of consent to enroll participants, link data, and perform analytic studies. All registries and the Statistical Coordinating Center have received a Federal Certificate of Confidentiality that protects the identities of research subjects. Federal, state, and local confidentiality and data security protections to safeguard these research data are described elsewhere [17].
Statistical Analysis
We calculated Student's t tests and Pearson's correlation coefficients to determine whether perceived risk of being sued for medical malpractice was associated with radiologists' characteristics or reactions to uncertainty in clinical decision making using the radiologist survey data from 2002 and 2006 and the facility survey data from 2002. We used multiple linear regression to determine the relationship between radiologists' perceived malpractice risk and different radiologist and facility characteristics while adjusting for BCSC registry. Predictors included radiologists' age, sex, score on the instrument for assessing reaction to uncertainty in clinical medicine, and prior medical malpractice claims (self or colleague). Facility characteristics assessed as predictors included use of double reading, frequency of audit reports, and use of CAD programs. A regression model was also fit without the reaction to uncertainty score included as a predictor.
Results
Characteristics of Respondents: 2002 and 2006 Surveys
The response rate to the radiologist surveys in 2002 and 2006 were 77% (139/181) and 71% (84/118), respectively. The interpretive performance (sensitivity, specificity, and positive predictive value) of responders in 2002 was the same as the nonresponders. Demographic, clinical practice, malpractice experience characteristics, and facility-level characteristics are shown in Table 1. The majority of respondents in 2002 and 2006 were 45 years old or older, male, had more than 10 years of experience in interpreting mammograms, spent more than 20% of their work time on breast imaging, and were not affiliated with an academic medical center.
TABLE 1.
Radiologists' Estimation of Risk of Mammography-Related Medical Malpractice Lawsuit Within Next 5 Years
| Radiologist and Facility Characteristics | 2002 Survey | 2006 Survey | ||
|---|---|---|---|---|
| No. (%) of Radiologists | Mean (SD) of Radiologists' Perceived Risk of Future Malpractice Lawsuita | No. (%) of Radiologists | Mean (SD) of Radiologists' Perceived Risk of Future Malpractice Lawsuita | |
|
| ||||
| Demographic characteristics | ||||
| Age (y) | ||||
| 34–44 | 44 (32) | 37.4 (26.8) | 17 (20) | 27.7 (32.0) |
| 45–54 | 51 (37) | 46.4 (30.4) | 34 (40) | 38.0 (24.0) |
| ≥ 55 | 44 (32) | 39.3 (30.7) | 33 (39) | 36.1 (26.4) |
| Sex | ||||
| M | 107 (78) | 41.6 (29.8) | 59 (70) | 33.0 (26.4) |
| F | 31 (22) | 38.2 (27.1) | 25 (30) | 40.3 (27.1) |
| Clinical experience of radiologists | ||||
| Mammogram interpretation experience (y) | ||||
| < 5 | 13 (9) | 41.6 (26.9) | 3 (4) | 30.0 (20.0) |
| 5–9 | 20 (15) | 34.4 (24.9) | 11 (13) | 40.0 (39.5) |
| 10–19 | 61 (45) | 47.6 (30.9) | 31 (37) | 34.0 (24.0) |
| ≥ 20 | 43 (31) | 36.4 (29.2) | 39 (46) | 35.1 (25.6) |
| Clinical time spent on breast imaging (%) | ||||
| < 20 | 63 (46) | 38.9 (27.6) | 18 (24) | 28.7 (27.7) |
| 20–39 | 57 (42) | 45.6 (31.4) | 19 (26) | 30.7 (24.4) |
| ≥ 40 | 16 (12) | 39.6 (29.5) | 37 (50) | 43.1 (28.1) |
| Total annual mammograms interpreted | ||||
| < 1,000 | 36 (26) | 38.0 (25.5) | 13 (17) | 34.6 (27.2) |
| 1,001–2,000 | 53 (39) | 43.0 (31.6) | 26 (33) | 30.3 (26.3) |
| > 2,000 | 48 (35) | 41.9 (29.9) | 39 (50) | 37.8 (25.0) |
| Affiliated with academic medical center | ||||
| Yes (primary/adjunct) | 23 (17) | 45.9 (31.1) | 12 (14) | 37.0 (32.8) |
| No | 116 (83) | 40.3 (29.2) | 72 (86) | 34.9 (25.7) |
| Malpractice experience | ||||
| Any malpractice claim filed against self? | ||||
| Yes | 71 (52) | 47.1 (32.2) | 45 (54) | 35.1 (24.5) |
| No | 66 (48) | 35.0 (25.0)c | 39 (46) | 35.3 (29.2) |
| Malpractice claim filed against colleague?b | ||||
| Yes | 119 (87) | 43.7 (30.0) | ||
| No | 18 (13) | 23.2 (17.5)d | ||
| Facility-level characteristics e | ||||
| Works at a facility that uses double reading? | ||||
| Yes | 80 (70) | 37.9 (30.3)f | ||
| No | 35 (30) | 48.6 (27.6)f | ||
| No. of times per year performance data are received | ||||
| 1 or 2 | 88 (77) | 39.1 (30.5) | ||
| 4 | 26 (23) | 48.9 (26.6) | ||
| Works at a for-profit mammography facility? | ||||
| Yes | 75 (65) | 39.1 (28.4) | ||
| No | 40 (35) | 44.8 (32.2) | ||
| Ever read a screen at a facility that uses computer-aided detection? | ||||
| Yes | 16 (14) | 52.3 (28.8) | ||
| No | 99 (86) | 39.4 (29.7) | ||
Note—Percentages do not add up to 100 because of rounding.
Total number of responses was 135; four radiologists did not have response data for risk estimates.
Results from the 2002 radiologist survey are linked with the 2002 facility survey. No facility survey was performed in 2006, and the radiologists were not asked about malpractice claims filed against colleagues.
p < 0.05.
p < 0.01.
Total number of responses was 115 for all facility-level questions with the exception of number of times per year performance data are received (n= 114).
p = 0.08.
Linkage with the 2002 facility survey revealed that most radiologists worked at a facility that used double reading (70%), received a performance audit report one or two times a year (77%), and worked at a for-profit mammography facility (65%). Fourteen percent of radiologists worked at facilities that used CAD programs. A facility survey was not performed in 2006.
Malpractice Attitudes and Experiences: 2002 and 2006 Surveys
As previously reported for the 2002 survey [6], the majority (87%) of participants reported knowing a colleague who had been sued for malpractice, and approximately half (n = 71) of the radiologists reported having had a malpractice claim filed against them. Fourteen percent (n = 19) of radiologists reported a prior mammography-specific claim at any point in the past (data not shown). Eight percent of radiologists (n = 11 of 130 responders to this question) reported a mammography-specific claim that was initiated in the 5 years before the initial survey (1997–2001).
Data from our 2006 survey revealed that only eight of 84 responders (approximately 10%) reported a mammography-specific claim in the previous 5 years (2002–2006), whereas four did not respond to this question. If the four nonrespondents either all had or all did not have a mammography-specific claim in the previous 5 years, the mammography malpractice experience would range from 9% (8/88) to 14% (12/88). Of the 60 responders who completed both surveys, six radiologists reported a mammography-specific legal claim in the previous 5 years (2002–2006) and four were missing data on this question.
Radiologists' perception of their risk of malpractice lawsuits related to mammography in the next 5 years on the 2002 survey ranged from 2.5% to 100% with a mean of 41.3% and a median of 30% (Fig. 1). One of four radiologists reported a perception of risk of 70% or higher. Data from our 2006 survey show the mean perceived risk in the future 5 years is similar to that estimated by radiologists in our initial survey (mean, 35.2%; median, 25%). This 2006 survey shows that radiologists continue to have a heightened estimate of medical malpractice risk, whereas the percentage of radiologists reporting actual lawsuits filed against them has been stable over the past decade. The Pearson's correlation coefficient between the 2002 perceived risk and the 2006 perceived risk was 0.1758 (p = 0.1869).
Fig. 1.
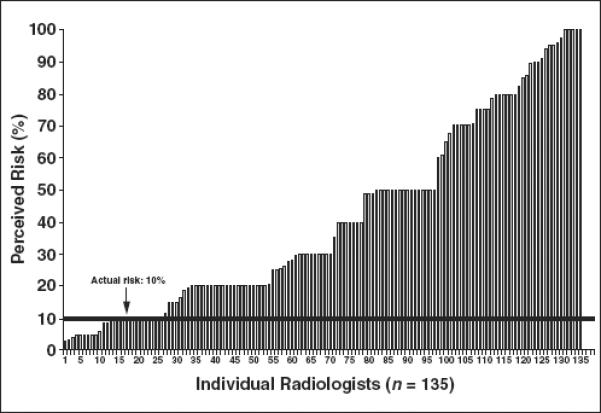
Graph shows individual radiologists' estimates on 2002 survey of their own 5-year malpractice risk (mean perceived risk, 41.3%; median, 30%). Actual risk noted on follow-up survey 5 years later in 2006 was ~10%.
Factors Associated with Radiologists' Malpractice Risk Perceptions
No clear associations were found between risk perception and radiologists' demographic or clinical characteristics such as age, sex, and clinical experience in either 2002 or 2006 (Table 1). Radiologists who spent more time in breast imaging or who had interpreted a high volume of mammograms (based on self-report) did not have a significantly higher perception of the risk of a mammography-related lawsuit. Radiologists who in 2002 reported a malpractice claim filed against a colleague or themselves reported a significantly higher perceived future malpractice lawsuit risk than those who did not (p < 0.05 in both cases). Radiologists in 2006 reporting a prior malpractice claim filed against them did not have a significantly different perception of malpractice risk compared with radiologists without malpractice claims. However, the sample size of radiologists responding to this question was small in 2006 compared with 2002 (n = 84 vs 137). We also did not ask radiologists in 2006 about malpractice claims filed against colleagues, and this was the most significant variable in 2002 that was associated with malpractice risk estimates. Radiologists working at a facility that did not use double reading tended to perceive higher risk than those who worked at a facility using double reading, but the difference was not statistically significant (average perceived risk of 48.6% and 37.9%, respectively; nonsignificant).
Radiologists' mean score on the validated scale measuring reactions to uncertainty in clinical decision making was 33.5 (range, 13–53 of 60 total possible points; SD, 8.6), where higher scores indicate more negative reactions to uncertainty (i.e., more reluctance to disclose errors, stress from clinical uncertainty, and concern about bad outcomes). In general, the more uncomfortable radiologists were with uncertainty in clinical decision making, the higher their perceptions of the risk of being sued (Pearson's correlation coefficient, 0.34; p < 0.001) (Fig. 2). This finding remained stable even when the concern about bad outcomes subscale (a subscale that included items assessing radiologists' malpractice concerns) was not included (Pearson's correlation coefficient, 0.29; p < 0.001).
Fig. 2.
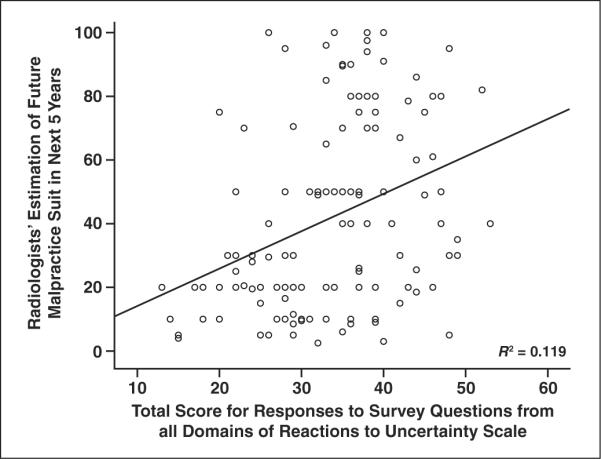
Graph shows radiologists' estimate of mammography-related medical malpractice lawsuit in the next 5 years and total score on an instrument measuring reactions to uncertainty in clinical situations. Reaction scale can range from 10 to 60. Higher score on reaction to uncertainty scale indicates radiologist is not comfortable with ambiguity in clinical situations [15]. Results are from 2002 survey.
In the multiple linear regression analysis of variables listed in Table 1, age, sex, site, having colleagues with a claim, and prior claim history were not significant predictors of the radiologists' perceived risk of malpractice. Double reading and the frequency of receiving audit data were also not significant predictors. The only significant predictor of a heightened perception of malpractice lawsuit risk was the score on the reactions to uncertainty scale (p < 0.001). The average malpractice risk perceptions of those in the lowest and highest quartile of stress because of clinical uncertainty were 26% and 48%, respectively. When the reaction to uncertainty score was not included in the regression equation, having a colleague with a prior malpractice claim was the only significant predictor of a heightened perception of malpractice risk (p = 0.04).
Discussion
A shortage of qualified radiologists in breast imaging in the United States could diminish the ability to provide women with their recommended regular screening mammograms. Fears of the medicolegal risks of breast imaging may be an important influence on whether radiologists decide to interpret mammograms [6, 14]. Our study found that radiologists' perceptions of the risk of malpractice lawsuits related to breast imaging were significantly higher than their actual reported experience of being sued, and these perceptions remained high over a 5-year period. Interestingly, those radiologists who found uncertainty in clinical medicine more troubling reported higher estimates for their likelihood of being sued.
Our data show that the average perceived risk for a lawsuit related to mammography is about four times higher than the reported rate of malpractice claims: 41% average perceived risk from the first survey for the time period from 2001 to 2005 versus 10% actual risk reported from the follow-up survey in 2006. This overestimation is higher than that shown in a study by Lawthers et al. [11] in which high-risk specialists, including neurosurgeons and general surgeons, only overestimated their risk of being sued by a factor of 1.6, whereas low-risk specialists such as internists overestimated their risk by a factor of 1.3. However, the data were gathered by Lawthers et al. more than 15 years ago, which may explain the lower perceived risk in their study.
The radiologists' 5-year estimates for the likelihood of being sued varied enormously, with 19% estimating their risk at 10% or lower and 25% estimating their risk at 70% or higher. This variation suggests a considerable need for education to help radiologists better understand their actual risk of being sued. Radiologists responding to the 2002 survey with the highest estimates for the likelihood of being sued were those who had previously been sued or knew colleagues who had been sued. Although physicians with prior claims may have an increased likelihood of experiencing a future claim [18], there is no known relationship between knowing a colleague who has been sued and actually being sued. Yet seeing a colleague experience the trauma of being sued may lead radiologists to mistakenly conclude that their own risk of being sued is higher by association, as might be anticipated. In addition, physicians are generally advised by risk managers not to discuss malpractice lawsuits that have been filed against them with colleagues because of concern that the colleague could be subpoenaed to testify in the case [19]. Thus, the information physicians may learn about lawsuits against colleagues may be incomplete or inaccurate, leading physicians to mistakenly inflate their chances of being sued.
Radiologists' malpractice risk perceptions remained high over the 5 years between the two surveys despite the fact that only 10% were actually sued during this time period, suggesting that understanding the sources of radiologists' malpractice risk perceptions will be important in bridging the gap between these risk perceptions and reality. For example, radiologists whose survey responses showed greater discomfort with uncertainty in clinical settings also perceived that the risk of being sued was higher—an association that persisted when adjusted for clinical and sociodemographic characteristics. Being sued for malpractice is fraught with uncertainty, including which clinical events will initially lead to lawsuits, whether a lawsuit will proceed to trial, and the outcome of that trial [20, 21].
In a malpractice situation, this uncertainty is deeply unsettling for physicians—a successful lawsuit can dramatically increase insurance premiums or, occasionally, render a physician uninsurable [22]. One study of Swiss physicians has shown that stress due to clinical uncertainty is associated with lower work-related satisfaction; this is an especially important issue in breast imaging, given the workforce strain in mammography [23]. Radiologists' discomfort with clinical uncertainty is also associated with higher recall rates, lower specificity, and lower positive predictive value when interpreting diagnostic mammograms [9]. Thus, developing interventions to reduce radiologists' discomfort with uncertainty could reduce their fears of malpractice and enhance the quality of mammographic interpretations.
Many other sources likely contribute to physicians' elevated perception of the risk of litigation. The mass media actively report errors in medicine and often emphasize breast cancer cases [24, 25], potentially heightening radiologists' awareness and anxiety regarding malpractice issues. Many medical societies and other physician interest groups have vigorously publicized the challenges in the current malpractice environment in hopes of encouraging tort reform [26]. The medical community should strive to help physicians better understand their actual risk of litigation by providing malpractice education that is accurate and balanced. Radiologists may also be less anxious about malpractice if they know that many lawsuits are dropped or never go to trial and that plaintiffs prevail in only a small fraction of cases that do proceed to trial [27–31].
Interventions, such as the use of CAD programs, did not influence physicians' perceptions of the risk of being sued. The practice of having a second set of human eyes looking at each examination may provide more reassurance that cancers are less likely to be missed. Radiologists may not have the same sense of trust in the second reading by a CAD program [32]. Considerable legal uncertainty exists regarding the impact of new technologies, such as CAD, on malpractice litigation. In one recent lawsuit, an appellate court upheld negative CAD results as reliable supportive evidence in the radiologist's defense [10]. It is also possible that CAD markings on a lesion that radiologists decided not to recall could be used to assist a plaintiff. However, positive CAD marks may be less helpful to plaintiffs in light of the low reliability of a CAD mark given the large number of false-positive findings [33]. Thus, the actual impact of these technologies on radiologists' risks of being sued for malpractice and the outcomes of these lawsuits remain uncertain.
This study addresses an urgent topic given that delay in breast cancer diagnosis remains the leading reason for medical malpractice claims in the United States and an important factor for declining interest in specializing in the field of breast imaging. The strength of this study is inclusion of community radiologists from three regions across the country. The participating radiologists from the state of Colorado might have lower perceptions of malpractice risk compared with other U.S. radiologists because these physicians are self-insured, and there are caps on malpractice lawsuits in Colorado. Limitations of this study include the reliance on self-reported data about malpractice litigation and experience. It is not known if these data are relevant to fields other than breast imaging. Radiologists who work part time and full time were asked to provide risk estimates for full-time practice in mammography; the risk estimates were similar for those whose practice at the time of the survey was part-time compared with the full-time radiologists. Although we had an unusually high response rate to mailed surveys for physicians (> 70%), we do not know if there was a bias induced by the type of radiologists who responded to our survey. The interpretive performance of responders to the 2002 survey was similar to that of the nonresponders, which is reassuring [34].
Recruiting and maintaining radiologists in breast imaging has become problematic due in part to malpractice litigation threats and resulting fear of litigation [4, 5]. Our study is the first to evaluate trends over a 5-year period in malpractice lawsuit experience and perception of risk among radiologists who interpret breast imaging. Our study is different from prior studies in that we compared perception of malpractice lawsuit risk not only to physician demographics and experience but also to practice characteristics (such as double reading and use of CAD) and physicians' reactions to uncertainty in clinical situations. Our data allow radiologists to review their peers' experience with malpractice litigation in breast imaging. Developing an accurate perception of malpractice lawsuit risk and understanding the characteristics of individual radiologists that are associated with an increased concern may help to lessen anxiety. Ultimately, radiologists who can put malpractice lawsuit risks in a realistic context may be more likely to choose the field of breast imaging and maintain their interest in remaining in the field. Given potential manpower shortages in breast imaging, maintaining radiologists in this field is an essential goal.
Acknowledgments
We thank the BCSC investigators, participating mammography facilities, and radiologists for the data they have provided for this study. A list of the BCSC investigators and procedures for requesting BCSC data for research purposes is provided at breastscreening.cancer.gov/.
Data collection for this work was supported by a National Cancer Institute (NCI)-funded Breast Cancer Surveillance Consortium cooperative agreement (U01 CA 86076; U01 CA63731; U01 CA86082; U01 CA63736).
J. G. Elmore was supported by public health service grant R01 HS-010591 from the Agency for Healthcare Research and Quality and NCI grants R01 CA107623 and K05 CA104699.
APPENDIX 1: Reaction to Uncertainty Domain and Individual Survey Items
| Modified instrument to assess reactions to uncertainty in medical decision making, adapted from the instrument developed by Gerrity and White [15] and validated in other physician populations. The original order has been modified to highlight the content of the three sub-scales. |
| Domain 1: Reluctance to Disclose Mistakes to Physicians |
| I never tell other physicians about mammographic interpretation errors I have made. |
| I almost never tell other physicians about cancer diagnoses I have missed. |
| Domain 2: Stress Due to Uncertainty |
| Uncertainty in mammography makes me uneasy. |
| I am quite comfortable with the uncertainty in mammography practice. |
| I find the uncertainty involved in mammography disconcerting. |
| I usually feel anxious when I am not sure of a mammographic interpretation. |
| The uncertainty in mammography often troubles me. |
| Domain 3: Concerns About Bad Outcomes |
| I worry about malpractice when I am not sure of a mammographic interpretation. |
| When I am uncertain of a mammographic interpretation, I imagine all sorts of bad scenarios—patient dies, patient sues, etc. |
| I fear being held accountable for the limits of my knowledge. |
Note—Reprinted with permission from Springer [15].
References
- 1.Lewis RS, Sunshine JH, Bhargavan M. A portrait of breast imaging specialists and of the interpretation of mammography in the United States. AJR. 2006;187:1167, W456–W468. doi: 10.2214/AJR.05.1858. web. [DOI] [PubMed] [Google Scholar]
- 2.Physician Insurers Association of America . PIAA 2002 breast cancer study. Physician Insurers Association of America; Rockville, MD: 2002. [Google Scholar]
- 3.Physician Insurers Association of America . PIAA 2003 breast cancer study. Physician Insurers Association of America; Rockville, MD: 2003. [Google Scholar]
- 4.Bassett LW, Monsees BS, Smith RA, et al. Survey of radiology residents: breast imaging training and attitudes. Radiology. 2003;227:862–869. doi: 10.1148/radiol.2273020046. [DOI] [PubMed] [Google Scholar]
- 5.Farria DM, Schmidt ME, Monsees BS, et al. Professional and economic factors affecting access to mammography: a crisis today, or tomorrow? Results from a national survey. Cancer. 2005;104:491–498. doi: 10.1002/cncr.21304. [DOI] [PubMed] [Google Scholar]
- 6.Elmore JG, Carney PA, Taplin S, D'Orsi CJ, Cutter G, Hendrick E. Does litigation influence medical practice? The influence of community radiologists, medical malpractice perceptions, and experience on screening mammography. Radiology. 2005;236:37–46. doi: 10.1148/radiol.2361040512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Government Accountability Office (GAO) Mammography: current nationwide capacity is adequate but access problems may exist in certain locations. GAO; Washington, DC: 2006. Publication no. GAO-06-724. [Google Scholar]
- 8.Carney PA, Elmore JG, Abraham LA, et al. Radiologist uncertainty and the interpretation of screening. Med Decis Making. 2004;24:255–264. doi: 10.1177/0272989X04265480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carney PA, Yi JP, Abraham LA, et al. Reactions to uncertainty and the accuracy of diagnostic mammography. J Gen Intern Med. 2007;22:234–241. doi: 10.1007/s11606-006-0036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brenner RJ, Ulissey MJ, Wilt RM. Computer-aided detection as evidence in the courtroom: potential implications of an appellate court's ruling. AJR. 2006;186:48–51. doi: 10.2214/AJR.05.0215. [DOI] [PubMed] [Google Scholar]
- 11.Lawthers AG, Localio AR, Laird NM, Lipsitz S, Herbert L, Brennan TA. Physicians' perceptions of the risk of being sued. J Health Polit Policy Law. 1992;17:463–482. doi: 10.1215/03616878-17-3-463. [DOI] [PubMed] [Google Scholar]
- 12.Schumacher JE, Ritchey FJ, Nelson LJ, Murray S, Martin J. Malpractice litigation fear and risk management beliefs among teaching hospital physicians. South Med J. 1995;88:1204–1211. doi: 10.1097/00007611-199512000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Ballard-Barbash R, Taplin SH, Yankaskas BC, et al. Breast Cancer Surveillance Consortium: a national mammography screening and outcomes database. AJR. 1997;169:1001–1008. doi: 10.2214/ajr.169.4.9308451. [DOI] [PubMed] [Google Scholar]
- 14.D'Orsi C, Tu SP, Nakano C, et al. Current realities of delivering mammography services in the community: do challenges with staffing and scheduling exist? Radiology. 2005;235:391–395. doi: 10.1148/radiol.2352040132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gerrity MS, White K. Physicians' reactions to uncertainty: refining the constructs and scales. Motiv Emot. 1995;19:175–191. [Google Scholar]
- 16.Hendrick RE, Cutter GR, Berns EA, et al. Community-based mammography practice: services, charges, and interpretation methods. AJR. 2005;184:433–438. doi: 10.2214/ajr.184.2.01840433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carney PA, Geller BM, Moffett H, et al. Current medicolegal and confidentiality issues in large, multicenter research programs. Am J Epidmiol. 2000;152:371–378. doi: 10.1093/aje/152.4.371. [DOI] [PubMed] [Google Scholar]
- 18.Bovbjerg RR, Petronis KR. The relationship between physicians' malpractice claims history and later claims: does the past predict the future? JAMA. 1994;272:1421–1426. [PubMed] [Google Scholar]
- 19.Brenner RJ. Mammography and malpractice litigation: current status, lessons, and admonitions. AJR. 1993;161:931–935. doi: 10.2214/ajr.161.5.8273628. [DOI] [PubMed] [Google Scholar]
- 20.Rowe M. Doctors' responses to medical errors. Crit Rev Oncol Hematol. 2004;52:147–163. doi: 10.1016/j.critrevonc.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Christensen JF, Levinson W, Dunn PM. The heart of darkness: the impact of perceived mistakes on physicians. J Gen Intern Med. 1992;7:424–431. doi: 10.1007/BF02599161. [DOI] [PubMed] [Google Scholar]
- 22.Studdert DM, Mello MM, Brennan TA. Medical malpractice. N Engl J Med. 2004;350:283–292. doi: 10.1056/NEJMhpr035470. [DOI] [PubMed] [Google Scholar]
- 23.Bovier PA, Perneger TV. Stress from uncertainty from graduation to retirement: a population-based study of Swiss physicians. J Gen Intern Med. 2007;22:632–638. doi: 10.1007/s11606-007-0159-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burke W, Daly M, Garber J, et al. Recommendations for follow-up care of individuals with an inherited predisposition to cancer. JAMA. 1997;277:997–1003. [PubMed] [Google Scholar]
- 25.Berlin L. Breast cancer, mammography, and malpractice litigation: the controversies continue. AJR. 2003;180:1229–1237. doi: 10.2214/ajr.180.5.1801229. [DOI] [PubMed] [Google Scholar]
- 26.Mello MM, Studdert DM, Brennan TA. The new medical malpractice crisis. N Engl J Med. 2003;34:2281–2284. doi: 10.1056/NEJMp030064. [DOI] [PubMed] [Google Scholar]
- 27.Brennan TA, Sox CM, Burstin HR. Relation between negligent adverse events and the outcomes of medical-malpractice litigation. N Engl J Med. 1996;335:1963–1967. doi: 10.1056/NEJM199612263352606. [DOI] [PubMed] [Google Scholar]
- 28.Brennan TA, Mello MM. Patient safety and medical malpractice: a case study. Ann Intern Med. 2003;139:267–273. doi: 10.7326/0003-4819-139-4-200308190-00009. [DOI] [PubMed] [Google Scholar]
- 29.Sage WM. The forgotten third: liability insurance and the medical malpractice crisis. Health Aff (Millwood) 2004;23:10–21. doi: 10.1377/hlthaff.23.4.10. [DOI] [PubMed] [Google Scholar]
- 30.Mello MM, Studdert DM, DesRoches CM, et al. Caring for patients in a malpractice crisis: physician satisfaction and quality of care. Health Aff (Millwood) 2004;23:42–53. doi: 10.1377/hlthaff.23.4.42. [DOI] [PubMed] [Google Scholar]
- 31.Studdert DM, Thomas EJ, Burstin HR, Zbar BI, Orav EJ, Brennan TA. Negligent care and malpractice claiming behavior in Utah and Colorado. Med Care. 2000;38:250–260. doi: 10.1097/00005650-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Gromet M. Comparison of computer-aided detection to double reading of screening mammograms: review of 231,221 mammograms. AJR. 2008;190:854–859. doi: 10.2214/AJR.07.2812. [DOI] [PubMed] [Google Scholar]
- 33.Greenberg JS. An appellate court ruling and potential implications for CAD technology in the courtroom. AJR. 2006;186:52–53. doi: 10.2214/ajr.06.5014. [DOI] [PubMed] [Google Scholar]
- 34.Barlow WE, Chi C, Carney PA, et al. Accuracy of screening mammography interpretation by characteristics of radiologists. J Natl Cancer Inst. 2004;96:1840–1850. doi: 10.1093/jnci/djh333. [DOI] [PMC free article] [PubMed] [Google Scholar]


