Abstract
Introduction
This study aims to identify whether patient-level or provider-level characteristics are most influential on a patient’s length of stay in the acute care hospital.
Materials and Methods
A dataset containing a nationally representative sample of inpatient discharge abstracts was used. Multi-level linear regression models were used to evaluate the associations between patient- and provider-level characteristics on patients’ lengths of stay.
Results
The target population included 322,894 discharges with a primary procedure code for primary total knee arthroplasty and 193,553 discharges for total hip arthroplasty. The variables associated with the greatest increases in length of stay were a higher co-morbidity level among patient level attributes (+17.4%) and low surgeon volume among provider-level characteristics (+18.8%).
Discussion
Provider-level characteristics, particularly provider volume, had a greater impact on length of stay.
INTRODUCTION
The prevalence of arthritis and joint pain has risen in the overall US population, from 11.0% in 1996 to 12.9% in 2004.1 Lower extremity total joint arthroplasties have been repeatedly demonstrated to be efficacious and cost-effective methods for treating end-stage arthritis.2-5 Between 1993 and 2002, the rates of primary hip and knee arthroplasty procedures increased by 35% and 70%, respectively, however by 2030, the rates are expected to be nearly 174% and 673% times higher than the 2005 rates.4, 6 Understanding the influence of specific baseline demographic characteristics on outcomes including hospital length of stay in patients undergoing arthroplasty may inform pre-operative planning to optimize discharge planning, rehabilitative resources and outcomes. By anticipating shorter or longer lengths of stay, patients may be more accurately counseled pre-operatively to appropriately manage patient and family expectations of their hospital stay.
A number of recent studies have demonstrated a relationship between patient, surgeon, and hospital characteristics and the patient’s risk for developing post-operative complications. Higher volume surgeons and hospitals experience lower mortality rates than lower volume surgeons and centers.7-9 Previous research has demonstrated the importance of both surgeon and hospital volume in determining the outcome of total joint arthroplasty.8, 10, 11 Higher provider volumes have been similarly linked to improved surgical outcomes in other specialties as well.7 Additionally, it has been shown that patient characteristics have a greater influence on the development of post-operative complications than hospital characteristics.12 African-Americans have higher rates of morbidity, mortality and readmission compared to Caucasians following total hip arthroplasty (THA) and total knee arthroplasty (TKA).13, 14 The development of complications is associated with prolonged lengths of stay and increased hospital costs.15 This study directly compares the effects of the patient and provider characteristics to determine which is more important in influencing length of stay while adjusting for the effects of other covariates. Identifying sources of prolonged lengths of stay in total joint arthroplasties could provide targets for cost-saving opportunities.
MATERIALS AND METHODS
The study was a cross-sectional secondary data analysis of a national administrative database. Parallel studies employing an identical methodological approach were conducted separately for TKA and THA cases. This study was approved by the hospital’s Institutional Review Board.
Sponsored by the Agency for Healthcare Research and Quality, the 2002 Health Care Utilization Project-Nationwide Inpatient Sample (HCUP-NIS) is an annual nationally representative stratified sample of community hospitals in states contributing to the HCUP. The sampling strategy was designed to select hospitals representing 20% of the discharges in each hospital characteristic stratum (i.e. region, urban/rural location, number of beds, teaching status, and ownership/control). Once a hospital was selected for inclusion in the database, 100% of that hospital’s discharges were included. The database includes over seven-million discharges from hospitals in thirty-five states and provides sampling weights allowing the data to be representative of national trends.
Study population
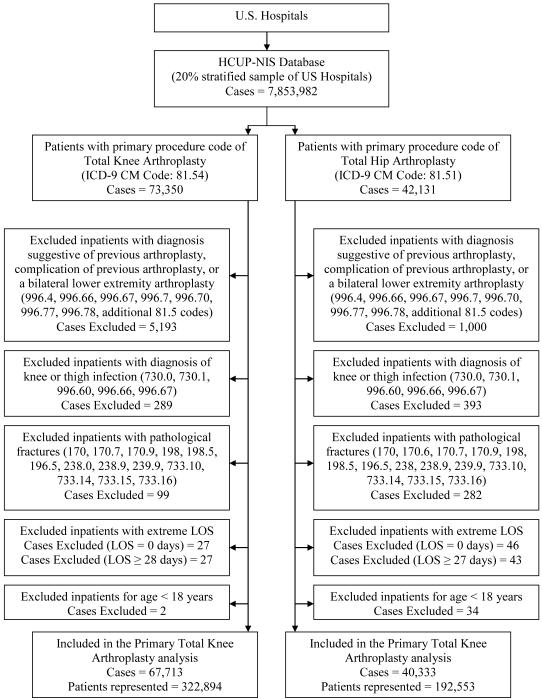
Cases were selected from the entire HCUP-NIS database based on having a primary procedure code of either primary TKA or THA according to the International Classification of Diseases, 9th Clinical Modification procedure of 81.54 and 81.51 respectively. This resulted in 73,350 TKA discharges and 42,131 THA discharges (Figure 1).
Figure 1.
Schema of Case Inclusion and Exclusion
The figure is a schematic representation of how the HCUP-NIS data file was pruned to two separate data files consisting of the primary TKR and THR cases. Arrows represent the step by step progression of exclusion, noting the number of cases excluded at each step, prior to obtaining the final set of cases meeting all inclusion and exclusion criteria.
Exclusion criteria included: the patient was undergoing a concurrent lower-extremity joint arthroplasty procedure (bilateral knee arthroplasty, hip and knee arthroplasty, or bilateral total hip arthroplasty); the discharge record carried diagnosis codes suggestive of knee or thigh infections, of a previous arthroplasty, complication from a previous arthroplasty, or of a pathological fracture8; the length of stay for a particular discharge fell in the outlier range (representing 0.04% and 0.11% from each tail of the distribution of the knee arthroplasty and the hip arthroplasty cases respectively); the patient was less than 18 years old. These exclusion criteria yielded 67,713 primary TKA discharges and 40,333 primary THA discharges, representing 322,894 primary TKA cases and 192,553 primary THA cases after applying the discharge weights (Figure 1).
Main Outcome Measures
The primary dependent variable of interest was a patient’s length of stay, in days, in the acute care hospital, from the date of admission to the date of discharge. Due to its right-skewed distribution, a logarithmic transformation of the patient’s length of stay was used as the primary outcome of interest. This log transformation resulted in a normal distribution imperative for the linear modeling.16
In a secondary analysis, the hospital charges associated with the discharges were evaluated to estimate the amount associated with each additional day in a patient’s hospital stay. Cases incurring charges amounting in the top and bottom 1% of charges were excluded from this secondary analysis. In order to obtain a normal distribution, a logarithmic transformation of the hospital charges was performed and then used as the outcome in the regression model. The transformed outcome variable in the model required a re-transformation according to the peer-reviewed methods to produce the mean change in hospital charges associated with each additional day in the hospital stay.17
Main Effects
Independent variables evaluated for an association with length of stay included patient-level and provider-level characteristics. The patient-level characteristics evaluated included age, gender, race, Deyo18 adjusted Charlson comorbidity index, household income at the ZIP code level, and insurance status. A reference case was constructed for comparison. The reference case was a young (under 60) white male13, with a Charlson comorbidity score of zero19, with private insurance, and having a household income of $45,000 or more per year. Age was categorized according to quartiles as shown in Table 1. Race was missing from a substantial portion of the records due to 11 of the 35 states in the dataset not reporting race at all. As a result, the records without a value for race did not appear to represent a distinct racial group that was underrepresented but a factor of the states not reporting race. For the cases missing a race value, a dummy value for race was created to distinguish these patients and prevent their being dropped from the analysis. As a result, the race variable was categorized into four groups: white, black, other (Hispanic, Asian, Native American and other), and missing in an attempt to increase the statistical power of minority patient groups. Charlson comorbidity scores were split into 3 categories, a score of 0, 1 and greater than or equal to 2. A score of 0 does not indicate that the patient did not have any comorbidity; rather that none of the documented diagnosis codes could count towards the Charlson index. The insurance payer analyzed was only the primary payer listed for the discharge except for dual Medicare/Medicaid enrollees who were identified by looking at both the primary and secondary insurers. The “Other” insurance status included patients listed as “self-pay” or “no-charge.”
Table 1.
Baseline Characteristics of patients with a primary procedure code for either lower extremity total joint arthroplasty
| Baseline Characteristics: Values given are frequencies with (%) unless noted. |
Primary Total Knee Arthroplasty N = 322,894 |
Primary Total Hip Arthroplasty N = 192,553 |
|---|---|---|
| Patient-level variables | ||
|
| ||
| Age – median (IQR) | 68 (60, 75) | 68 (57, 76) |
| - 18-59 | 76,399 (23.66%) | 58,542 (30.40%) |
| - 60-67 | 75,509 (23.38%) | 36,373 (18.89%) |
| - 68-74 | 80,308 (24.87%) | 40,549 (21.06%) |
| - 75+ | 90,679 (28.08%) | 57,088 (29.65%) |
|
| ||
| Gender | ||
| - Male | 114,333 (35.41%) | 81,404 (42.28%) |
| - Female | 208,556 (64.59%) | 111,140 (57.72%) |
|
| ||
| Race | ||
| - White | 186,669 (57.81%) | 116,106 (60.30%) |
| - Black | 16,786 (5.20%) | 8,676 (4.51%) |
| - Hispanic | 12,945 (4.01%) | 4,356 (2.26%) |
| - Asian/Pacific Islander | 2,210 (0.68%) | 1,021 (0.53%) |
| - Native American | 458 (0.14%) | 216 (0.11%) |
| - Other | 3,840 (1.19%) | 2,058 (1.07%) |
| - Missing | 99,986 (30.97%) | 60,120 (31.22%) |
|
| ||
| Charlson Score | ||
| - 0 | 216,431 (67.03%) | 135,660 (70.45%) |
| - 1 | 81,679 (25.30%) | 43,046 (22.36%) |
| - 2+ | 24,784 (7.68%) | 13,848 (7.19%) |
|
| ||
| Income level | ||
| - $1-24,999 | 9,668 (2.99%) | 5,056 (2.63%) |
| - $25,000-34,999 | 59,780 (18.51%) | 29,596 (15.37%) |
| - $35,000-44,999 | 85,242 (26.40%) | 46,519 (24.16%) |
| - ≥$45,000 | 161,058 (49.88%) | 107,238 (55.69%) |
| - Missing | 7,146 (2.21%) | 4,144 (2.15%) |
|
| ||
| Insurance Status (Primary payer): | ||
| - Private | 106,892 (33.12%) | 73,194 (38.03%) |
| - Medicare | 196,317 (60.83%) | 108,971 (56.62%) |
| - Medicaid | 7,632 (2.37%) | 5,242 (2.72%) |
| - Dual Medicare/Medicaid* | 15,665 (4.85%) | 9,056 (4.70%) |
| - Other (incl. Self-pay) | 11,908 (3.69%) | 5,076 (2.62%) |
|
| ||
| Provider-level variables | ||
|
| ||
| Hospital Region | ||
| - Northeast | 59,306 (18.37%) | 42,108 (21.87%) |
| - Midwest | 86,930 (26.92%) | 49,437 (25.67%) |
| - South | 117,440 (36.37%) | 61,486 (31.93%) |
| - West | 59,219 (18.34%) | 39,522 (20.53%) |
|
| ||
| Hospital Setting | ||
| - Urban | 276,641 (85.68%) | 169,438 (88.00%) |
| - Rural | 46,253 (14.32%) | 23,115 (12.00%) |
|
| ||
| Hospital teaching status | ||
| - Non-teaching | 182,023 (56.37%) | 95,428 (49.56%) |
| - Teaching | 140,872 (43.63%) | 97,126 (50.44%) |
|
| ||
| Hospital Bed Size | ||
| - Small | 46,690 (14.46%) | 28,212 (14.65%) |
| - Medium | 79,576 (24.64%) | 44,228 (22.97%) |
| - Large | 196,629 (60.90%) | 120,113 (62.38%) |
|
| ||
| Surgeon Volume (Cases/year) | ||
| - TKA: 1-17; THA:1-10 | 49,080 (15.20%) | 30,925 (16.06%) |
| - TKA: 18-35; THA:11-21 | 50,974 (15.79%) | 26,599 (13.81%) |
| - TKA: 36-66; THA: 22-52 | 47,610 (14.74%) | 28,450 (14.78%) |
| - TKA: ≥67; THA: ≥53 | 48,962 (15.16%) | 28,572 (14.84%) |
| - Missing | 126,269 (39.11%) | 78,008 (40.51%) |
|
| ||
| Hospital Volume (Cases/year) | ||
| - TKA: 1-100; THA: 1-64 | 83,060 (25.72%) | 50,248 (26.10%) |
| - TKA: 101-197; THA: 65-123 | 83,791 (25.95%) | 47,925 (24.89%) |
| - TKA: 198-293; THA:124-224 | 76,898 (23.82%) | 48,628 (25.25%) |
| - TKA: ≥293; THA: ≥225 | 79,146 (24.51%) | 45,751 (23.76%) |
|
| ||
| Hospital Ownership | ||
| - Government or Private | 190,951 (59.14%) | 124,914 (64.87%) |
| - Public | 17,722 (5.49%) | 9,005 (4.68%) |
| - Private Non-profit | 65,964 (20.43%) | 33,837 (17.57%) |
| - Private For-profit | 29,701 (9.20%) | 14,852 (7.71%) |
| - Private (Unspecified) | 18,556 (5.75%) | 9,945 (5.16%) |
|
| ||
| Unadjusted average Length of Stay (LOS) | 3.74 (±1.43) | 3.90 (±1.43) |
Provider-level characteristics analyzed included geographic region (Northeast, South, Midwest, West), location (Urban/Rural), teaching status (Teaching/Non-teaching), bed size (Small, Medium, Large), hospital ownership structure (public, private non-profit, private for-profit), surgeon volume of knee or hip arthroplasty procedures, and hospital volume of knee or hip arthroplasty procedures. The actual number of beds required to be classified as small, medium, or large varied according to the region and setting of the hospital, but these values were standardized in the HCUP-NIS dataset. The reference provider selected was an urban, non-teaching hospital in the northeastern US, with a low number of beds (small) but a high volume surgeon in a high volume non-profit center.
Two variables of interest, surgeon and hospital volumes of THA and TKA, were derived by using the synthetic physician and hospital identifiers associated with each discharge. Surgeon and hospital volumes were determined by counting the number of times a specific physician or hospital was identified in the dataset for having performed one of the total joint arthroplasty operations. Since the dataset is a 20% sample stratified at the hospital level, but contains 100% of the discharges from the sampled hospitals, this approach was believed a valid method of capturing surgeon and hospital volumes. This means that the dataset contains only a select number of hospitals within a state to obtain one-fifth of all discharges within that state, but every single discharge from an included hospital was listed in the dataset. As with the patient’s race variable, surgeon codes were missing from 39.1% of TKA cases and 40.5% THA cases due to 12 of the 35 states not reporting the provider identification. The surgeon and hospital variables were then categorized based on quartiles in order to give meaningful cut-points to variations in volume. A fifth category of ‘Missing’ was added to the surgeon volume variable in order to retain cases in the analysis from the 12 states which did not associate discharges with a surgeon identifier.
Statistical Methods
Associations between the patient-level and provider-level variables were evaluated using chi-square and ANOVA tests for categorical and continuous variables, respectively. Univariate analyses were then conducted evaluating unadjusted variations in length of stay associated with each of the patient- and hospital-level characteristics. These analyses were conducted using SAS version 9.1 (SAS Institute Inc., Cary, NC) which allowed for the sampling weights from the data collection to be taken into account.
The effects of patient-level and provider-level characteristics were evaluated simultaneously in a 2-level hierarchical linear model in order to distinguish the independent effects from each level of variables on the continuous outcome, length of stay. The first level was the patient-level variables and the second level was comprised of the provider-level variables. In these multivariable models, the effects of each independent variable were evaluated while adjusting for all of the patient-level and provider-level variables
In a separate 2-level hierarchical linear model, length of stay was added to the model as an independent variable along with all of the previously included variables, while the outcome of interest was hospital charges associated with the discharges. The effect of each additional day in a patient’s length of stay on the hospital charges was then ascertained while adjusting for all of the patient-level and provider-level variables. These various multi-level analyses were conducted using HLM version 6 (SSI Inc., Lincolnwood, IL).
RESULTS
The patients were predominantly white (over 80%) and female (over 55%) in each of the procedure groups (Table 1). The mean age of patients undergoing TKA was slightly higher (67.4 years) than patients undergoing THA (65.8 years). While women outnumbered men in both procedures, this was especially evident among TKA patients (64.59% versus 57.72%). The populations undergoing primary joint arthroplasty operations did not have a significant comorbidity burden reflected by approximately 70% of patients for either procedure having Charlson Comorbidity Index scores of zero. The mean length of stay was slightly greater when undergoing a THA compared to TKA (3.90 days versus 3.74 days).
Many of the patient characteristics were associated with certain provider-level variables (Tables 2 and 3). The percentages given in Tables 2 and 3 represent the proportion of that patient characteristic seen within the hospital characteristic level, as a result, the proportions do not add to 100%. There was substantial variation in the patient populations treated by different strata of providers. In particular, providers differed in their patient population’s composition of race, income level, and comorbidity score. Among both TKA and THA providers, low volume surgeons had higher proportions of black patients. Black patients also comprised higher proportions of the populations for urban and teaching hospitals. Poorer patients comprised a larger proportion of the patients treated for TKA and THA in rural, non-teaching hospitals and by low volume surgeons. Patients with higher comorbidity scores were more likely to be treated at hospitals with a higher number of beds. Surprisingly, low volume surgeons for both TKA and THA had patient populations with slightly higher comorbidity burdens (Tables 2 and 3).
Table 2.
Associations between Patient-level and Provider-level variables – Total Knee Arthroplasty
| REGION | SETTING | TEACHING | BED SIZE | SURGEON VOLUME |
HOSPITAL VOLUME |
HOSPITAL OWNERSHIP |
|
|---|---|---|---|---|---|---|---|
|
Age:
Mean (SD) |
NE: 67.9 (10.6) MW: 67.5 (10.7) S: 66.9 (10.6) W: 67.8 (10.6) p < 0.0001 |
Urban: 67.3 (10.7) Rural: 67.6 (10.5) p < 0.0001 |
Non-teaching: 67.8 (10.5) Teaching: 66.9 (10.7) p < 0.0001 |
Small: 67.5 (10.5) Medium: 66.9 (10.8) Large: 67.5 (10.6) p < 0.0001 |
1-17: 67.2 (10.7) 18-35: 67.2 (10.7) 36-66: 67.7 (10.4) ≥ 67: 67.9 (10.5) Missing: 67.2 (10.7) p < 0.0001 |
1-100: 67.6 (10.7) 101-197: 67.5 (10.7) 198-293: 67.2 (10.6) ≥ 294: 67.1 (10.5) p < 0.0001 |
Government: 67.4 (10.9) Non-profit: 67.7 (10.6) For-profit: 67.5 (10.3) p = 0.2005 |
|
Gender
(% female) |
NE: 65.37% MW: 64.76% S: 65.12% W: 62.52% p < 0.0001 |
Urban: 64.51% Rural: 65.09% p = 0.2740 |
Non-teaching: 64.14% Teaching: 65.18% p = 0.0053 |
Small: 65.02% Medium: 64.56% Large: 64.50% p = 0.6190 |
1-17: 64.99% 18-35: 65.33% 36-66: 64.05% ≥ 67: 63.50% Missing: 64.65% p = 0.0183 |
1-100: 66.31% 101-197: 64.30% 198-293: 64.01% ≥ 294: 63.65% p < 0.0001 |
Government: 65.95% Non-profit: 63.95% For-profit: 63.54% p = 0.0385 |
|
Race
(% Black) |
NE: 5.74% MW: 5.68% S: 12.06% W: 5.00% p <0.0001 |
Urban: 8.78% Rural: 4.66% p < 0.0001 |
Non-teaching: 5.60% Teaching: 12.20% p < 0.0001 |
Small: 6.20% Medium: 9.91% Large: 7.99% p < 0.0001 |
1-17: 10.32% 18-35: 9.22% 36-66: 8.35% ≥ 67: 6.09% Missing: 5.62% p < 0.0001 |
1-100: 6.79% 101-197: 9.03% 198-293: 7.28% ≥ 294: 7.24% p < 0.0001 |
Government: 10.29% Non-profit: 6.39% For-profit: 7.47% p <0.0001 |
|
Charlson
Score: mean (SD) |
NE: 0.33 (0.64) MW: 0.46 (0.73) S: 0.47 (0.73) W: 0.40 (0.70) p < 0.0001 |
Urban: 0.43 (0.71) Rural: 0.41 (0.71) p = 0.3389 |
Non-teaching: 0.42 (0.71) Teaching: 0.43 (0.72) p = 0.0054 |
Small: 0.38 (0.61) Medium: 0.41 (0.63) Large: 0.42 (0.63) p < 0.0001 |
1-17: 0.42 (0.64) 18-35: 0.40 (0.62) 36-66: 0.41 (0.63) ≥ 67: 0.39 (0.62) Missing: 0.41 (0.63) p = 0.0058 |
1-100: 0.41 (0.63) 101-197: 0.40 (0.62) 198-293: 0.41 (0.63) ≥ 294: 0.41 (0.63) p = 0.7777 |
Government: 0.45 (0.71) Non-profit: 0.46 (0.73) For-profit: 0.42 (0.70) p = 0.0098 |
|
Income
(% <$35,000) |
NE: 17.12% MW: 19.00% S: 33.42% W: 15.28% p <0.0001 |
Urban: 18.30% Rural: 44.33% p < 0.0001 |
Non-teaching: 25.37% Teaching: 17.68% p < 0.0001 |
Small: 20.00% Medium: 21.16% Large: 22.80% p < 0.0001 |
1-17: 10.32% 18-35: 9.22% 36-66: 8.35% ≥ 67: 6.09% Missing: 5.62% p < 0.0001 |
1-100: 7.24% 101-197: 7.28% 198-293: 9.03% ≥ 294: 6.79% p < 0.0001 |
Government: 29.85% Non-profit: 28.16% For-profit: 26.99% p = 0.0055 |
|
Insurance
Status (% Medicaid or dual) |
NE: 6.33% MW: 3.84% S: 5.70% W: 3.17% p < 0.001 |
Urban: 4.38% Rural: 7.67% p < 0.0001 |
Non-teaching: 4.84% Teaching: 4.87% p = 0.8371 |
Small: 6.12% Medium: 4.63% Large: 4.64% p < 0.0001 |
1-17: 9.20% 18-35: 9.76% 36-66: 9.39% ≥ 67: 7.52% Missing: 6.19% p < 0.0001 |
1-100: 7.61% 101-197:7.79% 198-293: 8.89% ≥ 294: 7.29% p < 0.0001 |
Government: 6.91% Non-profit: 4.16% For-profit: 6.12% p < 0.0001 |
Table 3.
Associations between Patient-level and Provider-level variables – Total Hip Arthroplasty
| REGION | SETTING | TEACHING | BED SIZE | SURGEON VOLUME |
HOSPITAL VOLUME |
HOSPITAL OWNERSHIP |
|
|---|---|---|---|---|---|---|---|
|
Age:
Mean (SD) |
NE: 66.4 (13.0) MW: 66.2 (13.0) S: 65.1 (13.8) W: 65.9 (13.1) p < 0.0001 |
Urban: 65.51 (13.4) Rural: 68.0 (12.5) p < 0.0001 |
Non-teaching: 67.4 (12.8) Teaching: 64.1 (13.6) p < 0.0001 |
Small: 64.9 (13.4) Medium: 65.9 (13.2) Large: 66.0 (13.3) p < 0.0001 |
1-10: 68.0 (13.3) 11-21: 66.7 (12.9) 22-52: 65.3 (13.4) ≥ 53: 64.0 (13.0) Missing: 65.4 (13.4) p < 0.0001 |
1-64: 67.2 (13.1) 65-123: 66.5 (13.1) 124-224: 65.7 (13.3) ≥ 225: 63.7 (13.4) p < 0.0001 |
Government: 67.3 (12.9) Non-profit: 67.0 (12.9) For-profit: 66.3 (13.5) p = 0.0054 |
|
Gender
(% female) |
NE: 57.33% MW: 58.48% S: 57.33% W: 57.80% p = 0.2854 |
Urban: 57.62% Rural: 58.47% p = 0.2689 |
Non-teaching: 58.65% Teaching: 56.81% p = 0.0002 |
Small: 58.21% Medium: 58.04% Large: 57.50% p = 0.4951 |
1-10: 60.22% 11-21: 58.52% 22-52: 58.69% ≥ 53: 55.47% Missing: 56.59% p < 0.0001 |
1-64: 59.16% 65-123: 58.67% 124-224: 56.91% ≥ 225: 56.00% p < 0.0001 |
Government: 58.18% Non-profit: 58.47% For-profit: 58.62% p = 0.9540 |
|
Race
(% Black) |
NE: 4.45% MW: 5.49% S: 10.80% W: 4.60% p <0.0001 |
Urban: 7.23% Rural: 4.57% p < 0.0001 |
Non-teaching: 5.05% Teaching: 9.06% p < 0.0001 |
Small: 4.91% Medium: 7.50% Large: 7.25% p <0.0001 |
1-10: 9.76% 11-21: 5.89% 22-52: 7.67% ≥ 53: 5.49% Missing: 5.19% p < 0.0001 |
1-64: 7.12% 65-123: 6.70% 124-224: 5.18% ≥ 225: 7.38% p < 0.0001 |
Government: 9.85% Non-profit: 5.76% For-profit: 6.42% p <0.0001 |
|
Charlson
Score: mean (SD) |
NE: 0.33 (0.70) MW: 0.42 (0.76) S: 0.45 (0.81) W: 0.38 (0.77) p < 0.0001 |
Urban: 0.40 (0.77) Rural: 0.41 (0.76) p = 0.0503 |
Non-teaching: 0.42 (0.77) Teaching: 0.39 (0.77) p = 0.0006 |
Small: 0.32 (0.57) Medium: 0.38 (0.63) Large: 0.38 (0.62) p < 0.0001 |
1-10: 0.42 (0.65) 11-21: 0.36 (0.60) 22-52: 0.35 (0.60) ≥ 53: 0.34 (0.59) Missing: 0.37 (0.61) p < 0.0001 |
1-64: 0.39 (0.63) 65-123: 0.38 (0.62) 124-224: 0.36 (0.61) ≥ 225: 0.34 (0.59) p < 0.0001 |
Government: 0.45 (0.83) Non-profit: 0.43 (0.77) For-profit: 0.42 (0.79) p = 0.2878 |
|
Income
(% <$35,000) |
NE: 14.17% MW: 18.58% S: 28.63% W: 15.28% p <0.0001 |
Urban: 15.20% Rural: 42.08% p < 0.0001 |
Non-teaching: 22.38% Teaching: 14.49% p < 0.0001 |
Small: 16.50% Medium: 18.44% Large: 18.82% p < 0.0001 |
1-10: 9.76% 11-21: 5.89% 22-52: 7.67% ≥ 53: 5.49% Missing: 5.19% p < 0.0001 |
1-64: 7.12% 65-123: 6.70% 124-224: 5.18% ≥ 225: 7.38% p < 0.0001 |
Government: 24.27% Non-profit: 24.34% For-profit: 21.51% p = 0.0038 |
|
Insurance
Status (% Medicaid or dual) |
NE: 5.56% MW: 4.06% S: 5.36% W: 3.56% p < 0.001 |
Urban: 4.28% Rural: 7.82% p < 0.0001 |
Non-teaching: 4.56% Teaching: 4.84% p = 0.1852 |
Small: 6.26% Medium: 4.49% Large: 4.42% p < 0.0001 |
1-10: 8.85% 11-21: 8.40% 22-52: 8.89% ≥ 53: 5.46% Missing: 6.24% p < 0.0001 |
1-64: 8.08% 65-123: 7.76% 124-224: 6.56% ≥ 225: 6.47% p < 0.0001 |
Government: 6.97% Non-profit: 4.27% For-profit: 4.32% p < 0.0001 |
According to the unadjusted analyses, almost every patient and provider characteristic evaluated was associated with statistically significant extended lengths of stay, with similar results for both TKA and THA (Table 4).
Table 4.
Unadjusted Length of Stay Associated with Patient and Provider Characteristics
| Values given are transformed mean LOS (95% CI) |
Total Knee Arthroplasty | Total Hip Arthroplasty | |||
|---|---|---|---|---|---|
| Patient Characteristics | |||||
| Gender | MALE | 3.68 (3.66, 3.70) | p < 0.0001 | 3.82 (3.80, 3.84) | p < 0.0001 |
| FEMALE | 3.78 (3.76, 3.79) | 3.98 (3.96, 3.99) | |||
| Age | 18-44 | 3.41 (3.48, 3.63) | p < 0.0001 | 3.70 (3.65, 3.75) | p < 0.0001 |
| 45-64 | 3.63 (3.62, 3.65) | 3.75 (3.73, 3.77) | |||
| 65-84 | 3.79 (3.78, 3.81) | 3.98 (3.96, 4.00) | |||
| 85+ | 4.06 (4.00, 4.13) | 4.69 (4.59, 4.79) | |||
| Race | WHITE | 3.69 (3.67, 3.70) | p < 0.0001 | 3.92 (3.90, 3.94) | p < 0.0001 |
| BLACK | 3.90 (3.85, 3.95) | 4.11 (4.03, 4.18) | |||
| OTHER* | 3.89 (2.62, 5.76) | 3.94 (2.66, 5.85) | |||
| MISSING | 3.77 (2.70, 5.26) | 3.84 (2.67, 5.53) | |||
| Charlson Score |
0 | 3.65 (3.64, 3.66) | p < 0.0001 | 3.80 (3.78, 3.81) | p < 0.0001 |
| 1 | 3.85 (3.83, 3.88) | 4.08 (4.04, 4.11) | |||
| 2+ | 4.18 (4.14, 4.23) | 4.56 (4.49, 4.64) | |||
| Income | $1-24,999 | 3.94 (3.87, 4.00) | p < 0.0001 | 4.26 (4.16, 4.36) | p < 0.0001 |
| $25-34,999 | 3.77 (3.75, 3.80) | 3.99 (3.95, 4.02) | |||
| $35-44,999 | 3.78 (3.75, 3.80) | 3.96 (3.93, 3.98) | |||
| $45+ | 3.70 (3.68, 3.71) | 3.85 (3.83, 3.87) | |||
| Insurance | PRIVATE | 3.58 (3.56, 3.60) | p < 0.0001 | 3.68 (3.66, 3.70) | p < 0.0001 |
| MEDICARE | 3.81 (3.80, 3.82) | 4.05 (4.03, 4.07) | |||
| MEDICAID | 4.12 (4.03, 4.20) | 4.31 (4.20, 4.41) | |||
| OTHER | 3.83 (3.78, 3.89) | 4.02 (3.91, 4.12) | |||
| Provider Characteristics | |||||
| Region | Northeast | 3.63 (2.53, 5.21) | p < 0.0001 | 3.86 (2.68, 5.55) | p < 0.0001 |
| Midwest | 3.76 (2.72, 5.19) | 3.91 (2.80, 5.48) | |||
| South | 3.79 (2.60, 5.51) | 4.00 (2.74, 5.82) | |||
| West | 3.75 (2.61, 5.38) | 3.84 (2.64, 5.57) | |||
| Setting | Urban | 3.73 (2.62, 5.30) | p < 0.0001 | 3.88 (2.70, 5.58) | p < 0.0001 |
| Rural | 3.85 (2.60, 5.69) | 4.13 (2.85, 6.00) | |||
| Teaching Status |
Non-teaching | 3.75 (2.60, 5.40) | p = 0.3000 | 3.97 (2.77, 5.69) | p < 0.0001 |
| Teaching | 3.74 (2.64, 5.29) | 3.86 (2.67, 5.57) | |||
| Bed size | Small | 3.83 (2.73, 5.38) | p < 0.0001 | 4.04 (2.90, 5.63) | p < 0.0001 |
| Medium | 3.71 (2.62, 5.25) | 3.89 (2.73, 5.54) | |||
| Large | 3.74 (2.59, 5.39) | 3.89 (2.67, 5.65) | |||
| Surgeon Volume |
TKA: 1-17; THA: 1-10 | 3.95 (2.48, 5.42) | p < 0.0001 | 4.30 (2.77, 5.82) | p < 0.0001 |
| TKA: 18-35; THA: 11-21 | 3.80 (2.37, 5.22) | 3.96 (2.55, 5.37) | |||
| TKA: 36-66; THA: 22-52 | 3.61 (2.20, 5.01) | 3.79 (2.41, 5.17) | |||
| TKA: ≥ 67; THA: ≥53 | 3.45 (2.02, 4.88) | 3.50 (2.07, 4.94) | |||
| VOLUME MISSING | 3.82 (2.71, 5.38) | 3.95 (2.79, 5.60) | |||
| Hospital Volume |
TKA: 1-100; THA: 1-64 | 3.95 (2.49, 5.40) | p < 0.0001 | 4.17 (2.69, 5.64) | p < 0.0001 |
| TKA: 101-197; THA: 65-123 | 3.66 (2.21, 5.11) | 3.91 (2.47, 5.34) | |||
| TKA: 198-293; THA: 124-224 | 3.77 (2.37, 5.16) | 3.86 (2.47, 5.24) | |||
| TKA: ≥ 294; THA: ≥ 225 | 3.61 (2.20, 5.02) | 3.72 (2.27, 5.16) | |||
| Ownership | ALL HOSPITALS | 3.74 (2.64, 5.28) | p < 0.0001 | 3.88 (2.69, 5.89) | p < 0.0001 |
| PUBLIC | 3.97 (2.72, 5.81) | 4.17 (2.85, 6.10) | |||
| NON-PROFIT | 3.73 (2.64, 5.28) | 3.88 (2.71, 5.56) | |||
| FOR-PROFIT | 3.69 (2.46, 5.53) | 4.02 (2.82, 5.75) | |||
Other race includes: Hispanic, Native American, Asian or Pacific Islander, or Other
In the adjusted multi-level regression models, many of the patient and provider characteristics were no longer significantly associated with extended lengths of stay (Table 5). Females stayed longer than their male peers (TKA: +2.0%; THA: +2.6%). Individuals over 75 years old stayed longer than their younger counterparts (TKA: +5.3%; THA: +8.4%). Black patients stay slightly longer than whites (TKA: +3.5%; THA: +5.6%). Not surprisingly, sicker patients stay longer in the hospital. Compared to patients with a comorbidity score of zero, patients with a comorbidity score of 1 stayed slightly longer (TKA: +4.5%; THA: +5.6%) while patients with comorbidity scores of 2 or more stayed considerably longer (TKA: +12.4%; THA: +17.4%). Income levels were not consistently associated with prolonged lengths of stay. Among THA patients, individuals in the lowest income level stayed the longest (+3.8%). Individuals with private insurance had the shortest stays in the hospital. Medicaid patients had the longest stays (TKA: +8.8%; THA: +10.3%).
Table 5.
Relative Differences to Length of Stay
| Patient Factors | |||||
|---|---|---|---|---|---|
| Total Knee Arthroplasty | Total Hip Arthroplasty | ||||
| Gender | MALE | 1.000 | -- | 1.000 | -- |
| FEMALE | 1.020 | p = 0.000 | 1.026 | p = 0.000 | |
| Age | 18-59 | 1.000 | -- | 1.000 | -- |
| 60-68 | 1.020 | p = 0.000 | 1.011 | p = 0.036 | |
| 68-75 | 1.014 | p = 0.048 | 1.006 | p = 0.560 | |
| 75+ | 1.053 | p = 0.000 | 1.084 | p = 0.000 | |
| Race | WHITE | 1.000 | -- | 1.000 | -- |
| BLACK | 1.035 | p = 0.000 | 1.056 | p = 0.000 | |
| OTHER* | 1.011 | p = 0.117 | 0.988 | p = 0.250 | |
| MISSING | 1.005 | p = 0.628 | 0.999 | p = 0.897 | |
| Charlson score |
0 | 1.000 | -- | 1.000 | -- |
| 1 | 1.045 | p = 0.000 | 1.056 | p = 0.000 | |
| 2+ | 1.124 | p = 0.000 | 1.174 | p = 0.000 | |
| Income | $1-24,999K | 1.011 | p = 0.322 | 1.038 | p = 0.008 |
| $25,000-34,999 | 1.012 | p = 0.012 | 0.992 | p = 0.288 | |
| $35,000-44,999 | 1.010 | p = 0.013 | 1.003 | p = 0.629 | |
| $45,000+ | 1.000 | -- | 1.000 | -- | |
| Insurance | PRIVATE | 1.000 | -- | 1.000 | -- |
| MEDICARE | 1.031 | p = 0.000 | 1.027 | p = 0.006 | |
| MEDICAID | 1.088 | p = 0.000 | 1.103 | p = 0.000 | |
| DUAL ENROLL | 1.025 | p = 0.049 | 1.078 | p = 0.000 | |
| OTHER | 1.039 | p = 0.000 | 1.061 | p = 0.000 | |
| Provider Factors | |||||
|---|---|---|---|---|---|
| Hospital Region |
NORTHEAST | 1.000 | -- | 1.00 | -- |
| MIDWEST | 0.986 | p = 0.539 | 0.964 | p = 0.122 | |
| SOUTH | 1.092 | p = 0.003 | 1.077 | p = 0.013 | |
| WEST | 1.037 | p = 0.309 | 0.999 | p = 0.978 | |
| Setting | URBAN | 1.000 | -- | 1.000 | -- |
| RURAL | 1.021 | p = 0.257 | 1.038 | p = 0.040 | |
| Teaching Status |
NON-TEACHING | 1.000 | -- | 1.000 | -- |
| TEACHING | 1.003 | p = 0.861 | 1.012 | p = 0.583 | |
| Bed Size | SMALL | 1.000 | -- | 1.000 | -- |
| MEDIUM | 1.004 | p = 0.856 | 1.007 | p = 0.733 | |
| LARGE | 1.007 | p = 0.700 | 1.013 | p = 0.517 | |
| Surgeon Volume (Cases/year) |
TKA: 1-17; THA: 1-10 | 1.108 | p = 0.000 | 1.188 | p = 0.000 |
| TKA: 18-35; THA: 11-21 | 1.052 | p = 0.007 | 1.073 | p = 0.005 | |
| TKA: 36-66; THA: 22-52 | 0.977 | p = 0.250 | 1.052 | p = 0.038 | |
| TKA: ≥ 67; THA: ≥53 | 1.000 | -- | 1.000 | -- | |
| MISSING | 1.040 | 0.446 | 1.090 | p = 0.019 | |
| Hospital Volume (Cases/year) |
TKA: 1-100; THA: 1-64 | 1.113 | p = 0.000 | 1.146 | p = 0.001 |
| TKA: 101-197; THA: 65-123 | 0.999 | p = 0.982 | 1.055 | p = 0.152 | |
| TKA: 198-293; THA: 124-224 | 1.031 | p = 0.288 | 1.030 | p = 0.368 | |
| TKA: ≥ 294; THA: ≥ 225 | 1.000 | -- | 1.000 | -- | |
| Hospital Ownership |
NON-PROFIT | 1.000 | -- | 1.000 | -- |
| PUBLIC | 1.023 | p = 0.422 | 1.025 | p = 0.390 | |
| FOR-PROFIT | 1.002 | p = 0.923 | 1.033 | p = 0.187 | |
| PRIVATE (NOT SPECIFIED) | 0.961 | p = 0.052 | 0.963 | p = 0.047 | |
Other race includes: Hispanic, Native American, Asian or Pacific Islander, or Other
Fewer provider characteristics significantly impacted the patient’s length of stay (Table 3). Factors that were not significant included most geographic regions, a rural versus urban setting, teaching status, size, and ownership status (i.e. whether the hospital is public, private for-profit, or private non-profit). Two variables that were highly significant predictors of length of stay were the annual volume of that procedure performed by the surgeon and the center. The centers in the lowest volume quartile (TKA: <100 cases per year; THA: <64 cases per year) had patients stay longer (TKA: +11.3%; THA: +14.6%) than the centers in the highest volume quartile (TKA: ≥294 cases per year; THA: ≥225 cases per year). Surgeon volumes also had a great effect on the patient’s length of stay. Patients treated by surgeons in the lowest volume quartile (TKA: <17 cases per year; THA: <10 cases per year) stayed longer (TKA: +10.8%; THA: 18.8%) than the patients of surgeons in the highest volume quartile (TKA: ≥67 cases per year; THA: ≥53 cases per year).
The regression model evaluating the effect of each additional day of a patient’s length of stay on marginal charges by the hospital showed each additional day was responsible for roughly an 8% increase in hospital charges (TKA: +8.9%; THA: +7.8%, p<0.001).
DISCUSSION
Our findings suggest that surgeon volume had as great, if not a greater effect, on a patient’s length of stay as their co-morbidity score. In addition, the institution’s volume of that procedure had a considerable impact on the patients’ length of stay. When combining the surgeon with the hospital, the provider’s volume of the procedure has the largest effect on a patient’s length of stay. For example, a TKA patient who might otherwise have an anticipated length of stay of 4 days, when treated by a low-volume surgeon in a low-volume hospital could anticipate a length of stay of 4.88 days. For a THA patient, the effect of low-volume surgeons and hospitals is even more pronounced, when an anticipated length of stay of 4 days would be extended to 5.34 days.
It has been shown that a prolonged length of stay is often the result of developing complications.15 Studies have demonstrated that age, gender, race, Charlson comorbidity index, income level, insurance type, and hospital volume are all associated with the development of complications following TKA and THA.12, 20 This study demonstrates that the annual volume of that procedure performed by the surgeon and hospital has as great or a greater impact on the patient’s length of stay than the patient’s characteristics. The finding that high volume providers having shorter lengths of stay is not surprising considering the literature supporting these surgeons and hospitals have superior outcomes.8, 10-12
A disparity in access to and utilization of total joint arthroplasty in the US has been described. African-Americans and women are more reluctant than Caucasians and men to choose a TKA.21 Despite this reluctance, women remain the predominant recipients of total knee and hip replacements since osteoarthritis is more prevalent in women. African-Americans and Hispanics have a similar prevalence of osteoarthritis to Caucasians, however minorities undergo total joint arthroplasty at lower rates than Caucasians.4, 22, 23 Patients of lower socioeconomic also undergo total joint replacements at lower rates than their wealthier peers.24 Our results demonstrate that once a minority or a low income individual elects to undergo a joint replacement, she is more likely to be treated by a low volume surgeon. This is notable since these minority and low income patients are at greater risk for developing complications and appear to be more frequently treated by the providers with inferior outcomes. Since total joint arthroplasty operations are typically an elective, non-emergent procedure, future research may be necessary to identify why these patients tend to receive treatment from low volume providers if we hope to decrease disparities in length of stay.
Other factors influencing the patient’s length of stay may have very little to do with the patient herself, including insurance status and geographic region. Administrative factors may be the underlying reason a patient’s insurance status impacts the patient’s length of stay. Many insurers pay lump sums for a procedure regardless of the duration of a patient’s hospital stay, thus encouraging hospitals to discharge the patient sooner for cost-savings. In contrast, Medicare requires minimum lengths of stay in the hospital, including a three day minimum stay prior to being discharged to a rehabilitation facility in order to avoid the hospital facing a reimbursement penalty.25 These administrative characteristics of the insurance plans may play a greater role in the length of stay differences between public and private insurance than the characteristics of the patients enrolled in each plan. It has been documented for several years that regional variations in length of stay exist.26, 27
One potential explanation for the study’s findings may be that the higher volume centers are simply more efficient at cost-shifting by discharging their patients to inpatient rehabilitation facilities earlier. Between 1997 and 2007, the average length of stay following a total hip or knee arthroplasty decreased (4.7 days to 3.7 days) while simultaneously there was a corresponding increase in the percentage of total hip or knee arthroplasty patients discharged to extended care facilities or home health care (69.3% to 75.9%) as opposed to being discharged home with outpatient physical therapy.28 It has been demonstrated with other diagnoses and surgical procedures that hospitals with higher volume and hospitals affiliated with an inpatient extended care facility or a home health network are more likely to discharge patients to those care facilities.29, 30 In a 2006 article though, Bozic et al. found that older, sicker, and Medicare insured patients were more likely to be discharged to an extended care facility following a total joint arthroplasty procedure.31 While cost-shifting is a reasonable concern when evaluating earlier discharges, the patient characteristics associated with an increased likelihood of being discharged to an extended care facility were also associated with prolonged lengths of stay in our analysis.
This study found that each additional day in a patient’s length of stay was associated with an 8% increase in hospital charges. Some researchers have suggested that reducing length of stay is not economically significant for the patient since the final day of hospitalization is only associated with 6.8% of the total cost for a patient whose length of stay is four days.32 Considering the nation spent $11.9 billion on TKAs in 2003, a reduction of even 6.8% poses a significant cost-savings opportunity for the health care system.33
Hospitals face a financial burden associated with unnecessarily long patient stays and have gradually discharged patients at earlier time points in recent years.25, 28 Reducing lengths of stay is a primary driver of reducing hospital costs associated with total joint arthroplasty procedures.34, 35 The results of this study can be used to develop an appropriate timeline for anticipated discharge based upon the patient and provider’s characteristics. This timeline can be used to facilitate making appropriate arrangements for post-acute care in advance of the patient actually being prepared for discharge, thus avoiding last minute administrative obstacles to discharge. The results of this study can also be used by hospitals for quality assurance measures to evaluate whether their patients’ lengths of stay are simply due to the demographics of the hospital’s patient population or if the lengths of stay are artificially high due to systemic issues.
The primary limitation in this study is that HCUP-NIS is a cross-sectional database without patient identifiers, thus it is impossible to determine adverse events post-discharge. The same patient may have been readmitted to the hospital immediately after discharge, but it would appear as two separate entries and interpreted as two separate individuals in the database. This limited the ability to accurately determine if patients discharged prematurely may have been readmitted, as this would have been undetected within the database. In addition, while the lengths of stay are reported as integers in the database, treating length of stay as a continuous variable allowed for greater sensitivity for detecting variations between patient groups. However, a 10% longer length of stay is more pertinent to the health care system than the individual patient. Whether a patient’s prolonged length of stay is a result of the development of complications or difficulty in post-acute care accommodation arrangements is not possible to discern in the dataset. The variations could represent certain segments of the population reluctant to leave the safety of the hospital despite being physically capable of being discharged.
While these variations in lengths of stay may be difficult for the clinician to readily appreciate in their daily practice, clinicians can appreciate inefficiencies in the health care system. Centralizing sites for patients undergoing THA or TKA may provide an opportunity for cost-savings by minimizing the financial burden on the health care system due to prolonged hospital stays. While from a health care system perspective, it may be most cost-effective to limit arthroplasty procedures to high volume centers, from the patient’s perspective, this may involve having to travel large distances away from friends and family to undergo the procedure by an unfamiliar surgeon. Since our system continues to utilize third-party payers, insurers may require patients to do more than use convenience as a reason to justify their selection of a surgeon. As our healthcare system comes under greater price scrutiny, administrators will be more reluctant to pay higher prices for less efficient care. In order for lower volume surgeons to continue competing with high volume centers, they will likely need to adopt the high volume centers’ methods for more efficient discharges of patients post-operatively.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Joseph F. Styron, Department of Epidemiology and Biostatistics, School of Medicine, Wood Building WG-57, Case Western Reserve University, 10900 Euclid Avenue, Cleveland, OH 44106-4945.
Siran Koroukian, Department of Epidemiology and Biostatistics, School of Medicine, Wood Building WG-57, Case Western Reserve University, 10900 Euclid Avenue, Cleveland, OH 44106-4945, sxk15@case.edu.
Alison Klika, Department of Orthopaedic Surgery, Mail Code: A-41, 9500 Euclid Avenue, Cleveland, OH 44195, klikaa@ccf.org.
Wael K. Barsoum, Department of Orthopaedic Surgery, Mail Code: A-41, 9500 Euclid Avenue, Cleveland, OH 44195, barsouw@ccf.org.
References
- 1.Jacobs JJ. Burden of musculoskeletal diseases in the United States. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2008. [Google Scholar]
- 2.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster J-Y. Health-Related Quality of Life in Total Hip and Total Knee Arthroplasty. J Bone Joint Surg Am. 2004;86-A(5):963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The Functional Outcomes of Total Knee Arthroplasty. J Bone Joint Surg Am. 2005;87-A(8):1719–1724. doi: 10.2106/JBJS.D.02714. [DOI] [PubMed] [Google Scholar]
- 4.Katz JN. Total joint replacement in osteoarthritis. Best Pract Res Clin Rheumatol. 2006;20(1):145–153. doi: 10.1016/j.berh.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Lavernia CJ, Guzman JF, Gachupin-Garcia A. Cost Effectiveness and Quality of Life in Knee Arthroplasty. Clin Orthop Relat Res. 1997;345:134–139. [PubMed] [Google Scholar]
- 6.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 7.Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital Volume and Surgical Mortality in the United States. N Engl J Med. 2002;346(15):1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 8.Hervey SL, Purves HR, Guller U, Toth AP, Vail TP, Pietrobon R. Provider Volume of Total Knee Arthroplasties and Patient Outcomes in the HCUP-Nationwide Inpatient Sample. J Bone Joint Surg Am. 2003;85:1775–1783. doi: 10.2106/00004623-200309000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Doro C, Dimick J, Wainess R, Upchurch G, Urquhart A. Hospital Volume and Inpatient Mortality Outcomes of Total Hip Arthroplasty in the United States. J Arthroplasty. 2006;21(6 Suppl. 2):10–16. doi: 10.1016/j.arth.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Katz JN, Mahomed NN, Baron JA, et al. Association of Hospital and Surgeon Procedure Volume With Patient-Centered Outcomes of Total Knee Replacement in a Population-Based Cohort of Patients Age 65 Years and Older. Arthritis Rheum. 2007;56(2):568–574. doi: 10.1002/art.22333. [DOI] [PubMed] [Google Scholar]
- 11.Kreder HJ, Grosso P, Williams JI, et al. Provider volume and other predictors of outcome after total knee arthroplasty: a population study in Ontario. Can J Surg. 2003;46(1):15–22. [PMC free article] [PubMed] [Google Scholar]
- 12.SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors Predicting Complication Rates Following Total Knee Replacement. J Bone Joint Surg Am. 2006;88(3):480–485. doi: 10.2106/JBJS.E.00629. [DOI] [PubMed] [Google Scholar]
- 13.Ibrahim SA, Stone RA, Han X, et al. Racial/Ethnic Differences in Surgical Outcomes in Veterans Following Knee or Hip Arthroplasty. Arthritis Rheum. 2005;52(10):3143–3151. doi: 10.1002/art.21304. [DOI] [PubMed] [Google Scholar]
- 14.Mahomed NN, Barrett JA, Katz JN, Baron JA, Wright JR, Losina E. Epidemiology of Total Knee Replacement in the United States Medicare Population. J Bone Joint Surg Am. 2005;87-A(6):1222–1228. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 15.Dimick J, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA. Hospital Costs Associated with Surgical Complications: A Report from the Private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199(4):531–537. doi: 10.1016/j.jamcollsurg.2004.05.276. [DOI] [PubMed] [Google Scholar]
- 16.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 17.Duan N. Smearing Estimate: A Nonparametric Retransformation Method. J Am Stat Assoc. 1983;78(383):605–610. [Google Scholar]
- 18.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 19.Heck DA, Robinson RL, Partridge CM, Lubitz RM, Freund DA. Patient Outcomes After Knee Replacement. Clin Orthop Relat Res. 1998;(356):93–110. doi: 10.1097/00003086-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Mahomed NN, Barrett JA, Katz JN, et al. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2003;85(1):27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Byrne MM, Soucheck J, Richardson M, Suarez-Almazor ME. Racial/ethnic differences in preferences for total knee replacement surgery. J Clin Epidemiol. 2006;59:1078–1086. doi: 10.1016/j.jclinepi.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 22.Katz BP, Freund DA, Heck DA, Dittus RS, Paul JE, Wright J. Demographic variation in the rate of knee replacement: a multi-year analysis. Health Serv Res. 1996;31:125–140. [PMC free article] [PubMed] [Google Scholar]
- 23.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349:1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 24.Bourne R, DeBoer D, Hawker GA, et al. Chapter 5: Total hip and knee replacement. In: Tu J, Pinfold S, McColgan P, Laupacis A, editors. Access to Health Services in Ontario: ICES Atlas. 2005. pp. 91–118. Institute for Clinical Evaluative Sciences Web site. [Google Scholar]
- 25.Fitzgerald JD, Boscardin WJ, Hahn BH, Ettner SL. Impact of the Medicare Short Stay Transfer Policy on Patients Undergoing Major Orthopedic Surgery. Health Serv Res. 2007;42(1):25–44. doi: 10.1111/j.1475-6773.2006.00606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chassin MR, Brook RH, Park RE, et al. Variations in the Use of Medical and Surgical Services by the Medicare Population. N Engl J Med. 1986;314:285–290. doi: 10.1056/NEJM198601303140505. [DOI] [PubMed] [Google Scholar]
- 27.Chassin MR, Kosecoff J, Park RE, et al. Does Inappropriate Use Explain Geographic Variations in the Use of Health Care Services? A Study of Three Procedures. JAMA. 1987;258:2533–2537. [PubMed] [Google Scholar]
- 28.HCUPnet [Accessed December 16, 2009];Healthcare Cost and Utilization Project (HCUP) 1997-2007 http://www.ahrq.gov/HCUPnet/
- 29.Buntin MB, Gartin AD, Paddock S, Saliba D, Totten M, Escarce JJ. How Much Is Postacute Care Use Affected by Its Availability? Health Serv Res. 2005;40(2):413–434. doi: 10.1111/j.1475-6773.2005.00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blewett LA, Kane RL, Finch M. Hospital Ownership of Post-Acute Care: Does It Increase Access to Post-Acute Care Services? Inquiry. 1995;32(4):457–467. [PubMed] [Google Scholar]
- 31.Bozic KJ, Wagie A, Naessens JM, Berry DJ, Rubash HE. Predictors of Discharge to an Inpatient Extended Care Facility After Total Hip or Knee Arthroplasty. J Arthroplasty. 2006;21(6 Suppl. 2):151–156. doi: 10.1016/j.arth.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 32.Taheri PA, Butz DA, Greenfield LJ. Length of Stay Has Minimal Impact on the Cost of Hospital Admission. J Am Coll Surg. 2000;191(2):123–130. doi: 10.1016/s1072-7515(00)00352-5. [DOI] [PubMed] [Google Scholar]
- 33.Health, United States, 2006 With Chartbook on Trends in the Health of Americans. National Center for Health Statistics; Hyattsville, MD: 2006. [PubMed] [Google Scholar]
- 34.Healy WL, Iorio R, Ko J, Appleby D, Lemos DW. Impact of Cost Reduction Programs on Short-Term Patient Outcome and Hospital Cost of Total Knee Arthroplasty. J Bone Joint Surg Am. 2002;84-A(3):348–353. doi: 10.2106/00004623-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Healy WL, Ayers ME, Iorio R, Patch DA, Appleby D, Pfeifer BA. Impact of a clinical pathway and implant standardization on total hip arthroplasty: a clinical and economic study of short-term patient outcome. J Arthroplasty. 1998;13:266–276. doi: 10.1016/s0883-5403(98)90171-1. [DOI] [PubMed] [Google Scholar]