Abstract
Purpose
The National Cancer Screening Program (NCSP) began in 1999. The objective of this report is to evaluate the results of the NCSP in 2008 and provide essential evidence associated with the gastric cancer screening program in Korea.
Materials and Methods
Data was obtained from the National Cancer Screening Information System; participation rates in gastric cancer screening were calculated. According to screening modalities, recall rates were estimated with 95% confidence intervals (CIs).
Results
The target population of the gastric cancer screening program in 2008 was 7,132,820 Korean men and women aged 40 and over, 2,076,544 of whom underwent upper endoscopy or upper gastrointestinal (UGI) series as screening tools (participation rate, 29.1%). Disparities in participation rates were observed relating to gender and health insurance type. Overall, recall rates of upper endoscopy and UGI series were 3.1% (95% CI, 3.0 to 3.1) and 33.3% (95% CI, 33.3 to 33.4), respectively.
Conclusion
According to our research, efforts to facilitate participation and to reduce disparities in gastric cancer screening among Korean men and women are needed. These results will provide essential data for evidence-based strategies in gastric cancer control in Korea.
Keywords: Korea, Mass screening, Stomach neoplasms
Introduction
Gastric cancer mortality has been decreasing continuously in Korea. It is, however, still a clinically important disease due to its high incidence and mortality [1,2]. To reduce high gastric cancer mortality, as part of a comprehensive 10-year plan for cancer control, the National Cancer Screening Program (NCSP) for Medical Aid Program (MAP) recipients was initiated in 1999. The NCSP recommends that men and women aged 40 or over undergo upper endoscopy or upper gastrointestinal (UGI) series every other year [3]. When a UGI series is chosen as a screening method, upper endoscopy can also be conducted if gastric cancer is suspected. If necessary, a biopsy is conducted during upper endoscopy.
The target population of NCSP was expanded to include National Health Insurance (NHI) beneficiaries within the lower 20% of the income bracket in 2002. This cut-off was increased to 30% in 2003 and then to 50% in 2005. Currently, MAP recipients and NHI beneficiaries in the lower 50% income bracket are eligible to be included in the NCSP and can have gastric cancer screening free of charge (including additional upper endoscopy and biopsy). The NHI Corporation has also provided gastric cancer screening to its beneficiaries who are not included in the NCSP and covers part of the cost of the screening services through the NHI screening program. It subsidized 50% of the cost of screening services until 2005. It subsequently increased its subsidization to 80% in 2006 and then to 90% in 2010.
The aim of this study was to evaluate results of the NCSP for gastric cancer in 2008, to investigate the participation rate of gastric cancer screening, and to assess the results.
Materials and Methods
Participants of the NCSP in 2008 were men and women who were NHI beneficiaries within the lower 50% of the income bracket and MAP recipients aged 40 or over, who were born in 1968 or before. For those who were included in the NCSP among the NHI beneficiaries, their insurance premium was US$56.5 (1 US$=1,000 won) per month or below (based on November, 2007) for the employee insured and US$67 per month or below for the self-employed insured.
Participation in the NCSP was confirmed from the claims and results of gastric cancer screening submitted to the NHI Corporation before December 31, 2009. Screening was performed between January 1, 2008 and December 31, 2008. Some subjects underwent the same screening procedure multiple times; for these individuals only the first screening was counted (n=2,239). Some subjects underwent UGI series followed by endoscopy because gastric cancer was suspected from the UGI series (n=5,719). These patients were only counted once to give the participation rate. The participation rate of gastric cancer screening was calculated by dividing the number of participants by the target population of NCSP for gastric cancer, and denoted as a percentile [4].
The results of the screening program were classified into six categories: 'normal,' 'benign,' 'needing further evaluation,' 'suspicious of cancer,' 'gastric cancer,' and 'confirmed gastric cancer.' 'Needing further evaluation' was defined as needed additional examination due to suspected gastric cancer, or the case where follow-up was required within a short period. 'Gastric cancer' was defined as a case where gastric cancer was confirmed in the biopsy during upper endoscopy. 'Confirmed gastric cancer' was defined as cases wherein the patient already has a previous medical history of gastric cancer prior to screening. In this study, participants falling within the categories 'needing further evaluation,' 'suspicious of cancer,' and 'gastric cancer' were deemed to be recall cases. Subjects who underwent both UGI series and upper endoscopy were defined as recall cases in UGI series regardless of the final result. Recall rates for gastric cancer screening were defined as the proportion of recall cases among the cancer-screened participants. The 95% confidence intervals were calculated for all outcome variables.
Results
In the target population of 7,132,820 subjects for gastric cancer screening, there were 3,407,649 (47.8%) males and 3,725,171 (52.2%) females. Based on health insurance, 929,428 (13.0%) were covered by MAP and 6,203,392 (87.0%) were covered by NHI. There were 330,870 over the age of 70 covered by MAP, accounting for 35.6% of total MAP recipients. This was much higher than the 11% of NHI beneficiaries falling in the same age group.
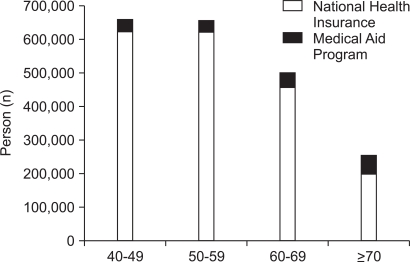
Of the target population, 2,076,544 participants underwent gastric cancer screening, giving 29.1% participation. Of them, 58.6% (1,216,690) were women and 41.4% (859,854) were men. For men, there were 268,419 (31.2%) participants in their 50s, accounting for the largest male group, whereas, for women, the largest group was women in their 40s where there were 420,094 (34.5%) participants. For the NHI beneficiaries, participation decreased as their age increased, whereas, for MAP beneficiaries, participation increased as their age increased. Thus, there were 55,036 participants in their 70s, accounting for 32.1% of the total (Fig. 1).
Fig. 1.
Number of participants by health insurance type and age from the National Cancer Screening Program, 2008.
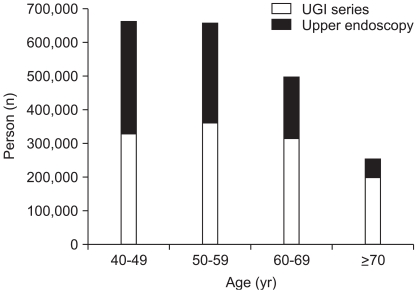
According to screening method, 1,198,061 (57.7%) participants selected UGI series as a primary gastric cancer screening method, whereas 878,483 (42.3%) participants selected upper endoscopy. However, 385,062 subjects, (32.1%) who initially underwent UGI series, also underwent upper endoscopy. Of the participants in their 50s, 34.2% of the individuals who underwent UGI series also underwent upper endoscopy, accounting for the largest portion, whereas 28.9% of the participants in their 70s or over additionally underwent upper endoscopy, accounting for the smallest portion. For participants in their 40s, 335,087 (50.5%) underwent upper endoscopy, whereas 328,417 (49.5%) underwent UGI series. As age increased, the participation rate decreased so that 56,845 participants in their 70s underwent upper endoscopy, accounting for 22.4% of the total participants in their 70s who participated in the gastric cancer screening (Fig. 2).
Fig. 2.
Number of participants by screening modalities and age from the National Cancer Screening Program, 2008. UGI, upper gastrointestinal.
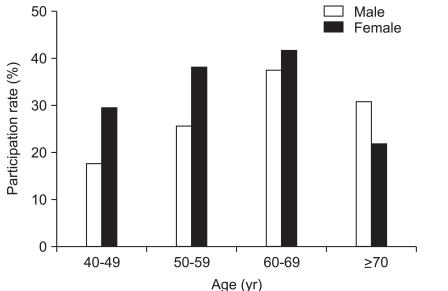
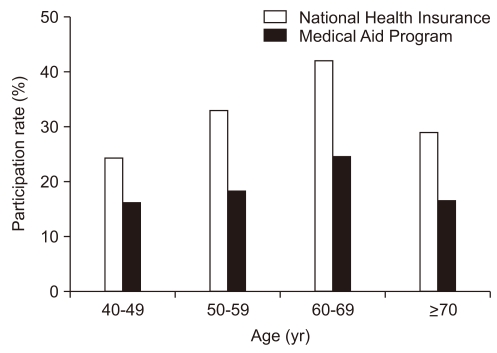
The participation rate in gastric cancer screening in the 2008 NCSP was 29.1%. In the target population, the female participation rate was 32.7%, which was higher than the males with a rate of 25.2%. As participant age increased, so did the participation rate, to 39.7% in their 60s, which was the highest rate for both male and females (Fig. 3). This figure decreased to 25.0% in those in their 70s and over. When the participation rate was classified by insurance type, the participation rate was 18.5% in MAP recipients, which was lower than 30.7% in NHI beneficiaries (Fig. 4).
Fig. 3.
Participation rates by gender and age from the National Cancer Screening Program, 2008.
Fig. 4.
Participation rates by health insurance type and age from the National Cancer Screening Program, 2008.
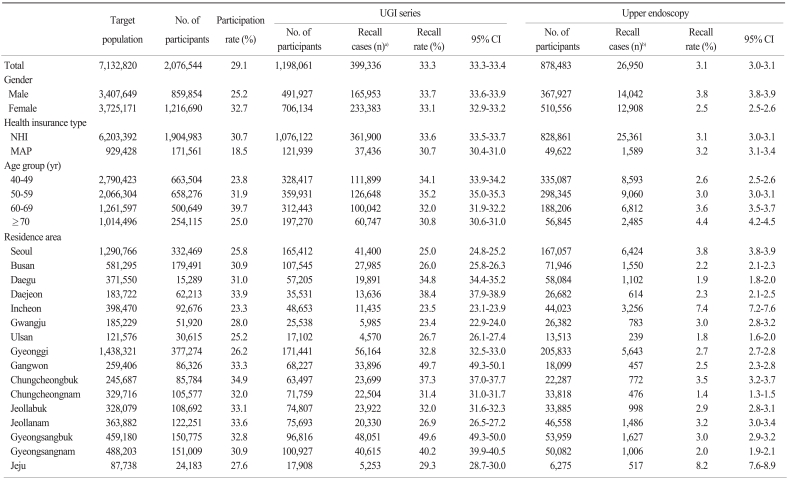
Of the 1,198,061 participants who underwent UGI series, 561,377 (46.9%) subjects were normal and 237,049 (19.8%) subjects were benign. The recall cases were classified as 12,575 (1.0%) 'needing further evaluation,' 386,634 (32.3%) 'suspicious of cancer,' and 127 (0.0%) as 'gastric cancer.' Of the total 878,483 participants who underwent upper endoscopy, 113,829 (13.0%) were normal and 737,427 (83.9%) were benign. The recall cases were classified as 24,014 (2.7%) 'needing further evaluation,' 1,138 (0.1%) 'suspicious of cancer,' and 1,798 (0.2%) as 'gastric cancer.' The recall rate for UGI series was 33.3%, with the highest rate of 34.1% for participants in their 40s. As participant age increased, the recall rate decreased, to 30.8%, the lowest rate being in participants aged 70 and over. The recall rate of upper endoscopy was 3.1%, which was lower than that of UGI series. As participant age increased, the recall rate increased (Table 1).
Table 1.
Screening outcomes by gender, health insurance type, age, and area of residence from the National Cancer Screening Program, 2008
UGI, upper gastrointestinal; CI, confidence interval; NHI, National Health Insurance; MAP, Medical Aid Program. a)Participants who received 'needing further evaluation,' 'suspicious of cancer,' or 'gastric cancer' or received additional upper endoscopy for further evaluation after undergoing UGI series were deemed to be recall cases, b)Participants who received 'needing further evaluation,' 'suspicious of cancer,' or 'gastric cancer' were deemed to be recall cases.
Discussion
The participation rate in the NCSP for gastric cancer in 2008 was 29.1%. Trends for participation rates have been increasing continuously, from 12.7% in 2002 when the participation rate of gastric cancer screening in the NCSP was first estimated. However, it is still below the overall screening rate for gastric cancer in Korea (53.5%), including opportunistic screenings as well as the organized screening program conducted by the NHI Corporation [5].
In 1960, mass gastric screening by barium X-ray was started in Miyagi Prefecture, Japan. In conformity with the Law of Health and Medical Services for the Elderly, which came into effect in 1983, gastric cancer screening has been conducted nationwide as a Japanese government policy. Japanese men and women aged 40 or over were recommended to participate annually in cancer screening programs for gastric cancer with photofluorography using X-ray devices. Although the Japanese government set a goal of an annual participation rate of 30% among the target population, the participation rate in gastric cancer screening was 12.1% in 2006 [6-8].
In Korea, the participation rate in NCSP is higher than that of Japan, but is lower than the participation rate of 60-70% in European countries [9,10]. One reason that gastric cancer screening has not had a higher take-up in the NCSP was the negative perception that the quality of screening services was poor [11]. To facilitate participation in NCSP, many hospitals and clinics were allowed to become a gastric cancer screening facility if they met minimal requirements. This policy increased the participation rate in NCSP, but also caused an issue with the quality of the management of the cancer screening service.
To address this issue and improve the quality of cancer screening systematically, the government legislated for assessing and regulating cancer screening facilities via an amendment to the Cancer Control Act in 2006. The Quality Evaluation of National Cancer Screening (QENCS) program, which has been conducted by the National Cancer Center (NCC) since 2008, evaluates all aspect of cancer screening including the structure, process, and outcome. In particular, for outcome assessment, both participant satisfaction and the accuracy of cancer screening are reviewed. Prior to the assessment, the NCC developed and distributed 'Quality guidelines of gastric cancer screening' with the help of professional associations to improve the quality of gastric cancer screening. When the first term of the QENCS program, which is in progress, is completed for 2010, more objective and improved assessment items and standards will be developed.
The use of a photofluorographic device with 100 mm film will be prohibited in UGI series starting from 2010 to improve imaging quality. The standardized method of taking a series of films including 'supine positioned double contrast image,' 'prone positioned single contrast image,' 'erect compression image,' 'distal esophagus and gastroesophageal junction image,' and 'right posterior and left posterior oblique images (45°)' has been recommended since 2010. Although this lags the Japanese standardized method with the seven standard images [12], the standardization of UGI series and an improvement in screening performance can be expected as a result of this recommendation.
Despite the increasing trend in participation in NCSP for gastric cancer, there are some issues to be resolved. First, the incidence and mortality of gastric cancer are known to be relatively high in the lower socio-economic class in Korea [13]. Thus, the participation rate in gastric cancer screening needs to be improved in these people. However, the participation rate of MAP recipients increased from 12.6% in 2002 to 18.6% in 2008, which is lower than the rate of NHI beneficiaries (12.7% in 2002; 30.7% in 2008). Despite gastric cancer screening being free of charge, the poor participation rate of the socio-economic lower class in gastric cancer screening indicates other factors inhibit participation in gastric cancer screening apart from the economic burden of screening costs. Thus, identification of factors that inhibit participation in gastric cancer screening and suitable measures to overcome these are required.
Second, incidence rates of gastric cancer based on gender are 61.2 males/100,000 persons and 23.9 females/100,000 persons, 2.6-fold higher in males than females. Gastric cancer mortality is also 2.7-fold higher in males than females (age-adjusted mortality rate per 100,000, 25.3 in males and 9.3 in females) [2]. Despite the high incidence and mortality of gastric cancer in males, the male participation rate in gastric cancer screening is lower than for females (age-adjusted participation rate, 25.4% in males; 33.2% in females). Thus, to decrease high gastric cancer mortality, efforts should be made to increase the participation rate of gastric cancer screening in Korean men.
Third, compared with the recall rate of 3.1% in upper endoscopy, the recall rate was 33.3% in UGI series. This is attributable to the fact that 32.1% of the examinees who selected UGI series also underwent upper endoscopy. In the NCSP, if UGI series is chosen as a gastric cancer screening method, upper endoscopy can also be conducted free of charge. However, due to the ambiguous indication of additional upper endoscopy and free screening costs, unnecessary additional upper endoscopy is likely to be conducted.
In Japan, the recall rate of gastric cancer screening in Osaka was 11.7% in the 1970s [14], with a minimum of 10.1% and maximum of 18.9% in the 1980s [15-19]. Since the 1990s, the recall rate was recently reported to be approximately 10% [8,20]. At the beginning of gastric cancer screening programs in Japan, recall rates were as high as 20%, but decreased continuously to 10%, which has now stabilized. The category 'suspicious of cancer' will be clearly stated in the requirement of conducting additional upper endoscopy starting from 2010 in the NCSP, which should reduce unnecessary additional upper endoscopy.
The recall rate of upper endoscopy was 3.1%, maintaining the lower level, but disparities, depending on geographical location, were observed (age-adjusted recall rate range, 1.4 to 8.2%). In Korea, the qualification of doctors who can conduct endoscopy including the NCSP is not separately defined. In various foreign countries, to conduct endoscopy, doctors are required to take supervised training to reach a certain level of competence [21]. Additionally, to meet increased endoscopy demand and provide qualified services due to the introduction of a nationwide screening program using endoscopy, development of a new educational and training program is required [22]. The development of educational programs for endoscopists in the NCSP is required to minimize variations and to provide upper endoscopy at a consistent level.
Finally, there is the regional disparity of up to 11.6% in the participation rate, ranging from 23.3% to 34.9%. There was no change in the regional disparity even if the age was adjusted based on the region (age-adjusted participation rate range, 23.5 to 35.1%). According to the 2008 report, from a total of 249 regions across the country, 10 areas were reported to be without gastric cancer screening facilities (4.0%) [23]. In these areas, participants underwent gastric cancer screening in other areas or via mobile screening units.
In 2008, essentially required medical devices for gastric cancer screening were changed from 'endoscope' and 'photoflorographic apparatus' to 'endoscope' to improve access to gastric cancer screening. Through this modification, gastric cancer screening was available in clinics and hospitals equipped only with devices for upper endoscopy. Of the participants who underwent gastric cancer screening in 2008, 42.3% selected upper endoscopy as a screening tool. Considering additional upper endoscopy, more than half of the total participants underwent this procedure. However, 54.6% of the participants in Gyeonggi province underwent upper endoscopy for gastric cancer screening, whereas only 21.0% of the participants in Gangwon province underwent the same procedure. Regional disparities exist not only in the number of gastric cancer screening facilities but also in the number of hospitals and clinics that provide upper endoscopy. Thus, continuing efforts are required for more medical centers to participate in the NCSP, as well as investment in public hospitals to resolve areas with no screening unit.
Conclusion
In 2008, 29.1% of the target population of NCSP participated in gastric cancer screening. Differences in participation rate occurred between regions, age, and socioeconomic status. Additionally, differences existed in the selection of gastric cancer screening methods. Thus, along with improving the participation rate in gastric cancer screening, continuing efforts are required to minimize these differences.
Acknowledgments
This study was supported by a Grant-in-Aid for Cancer Research and Control from the National Cancer Center of Korea (#1010201-1).
Footnotes
Conflict of interest relevant to this article was not reported.
References
- 1.Won YJ, Sung J, Jung KW, Kong HJ, Park S, Shin HR, et al. Nationwide cancer incidence in Korea, 2003-2005. Cancer Res Treat. 2009;41:122–131. doi: 10.4143/crt.2009.41.3.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, et al. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010;25:1113–1121. doi: 10.3346/jkms.2010.25.8.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park CH. Proposal of a screening program for gastric cancer in Korea. J Korean Med Assoc. 2002;45:964–971. [Google Scholar]
- 4.Perry N, Broeders M, de Wolf C, Tornberg S, Hölland R, von Karsa L. European guidelines for quality assurance in breast cancer screening and diagnosis. 4th ed. Brussels: European Communities; 2006. pp. 53–54. [DOI] [PubMed] [Google Scholar]
- 5.National Cancer Center; Ministry for Health Welfare and Family Affairs. Cancer facts and figures 2009. Goyang: National Cancer Center; 2009. pp. 47–56. [Google Scholar]
- 6.Ministry of Health, Labour and Welfare [Internet] Tokyo: Ministry of Health, Labour and Welfare; [cited 2010 May 28]. Available from: http://www.mhlw.go.jp/shingi/2004/04/s0427-2.html. [Google Scholar]
- 7.Health Statistics in Japan, 2007 [Internet] Tokyo: Ministry of Health, Labour and Welfare; [cited 2010 May 28]. Available from: http://www.mhlw.go.jp/english/database/db-hss/dl/hs2007a.pdf. [Google Scholar]
- 8.Ministry of Health, Labour and Welfare [Internet] Tokyo: Ministry of Health, Labour and Welfare; [cited 2010 May 28]. Available from: http://www.mhlw.go.jp/toukei/saikin/hw/c-hoken/06/r8.html. [Google Scholar]
- 9.Day NE, Williams DR, Khaw KT. Breast cancer screening programmes: the development of a monitoring and evaluation system. Br J Cancer. 1989;59:954–958. doi: 10.1038/bjc.1989.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tabar L, Fagerberg G, Chen HH, Duffy SW, Smart CR, Gad A, et al. Efficacy of breast cancer screening by age: new results from the Swedish Two-County Trial. Cancer. 1995;75:2507–2517. doi: 10.1002/1097-0142(19950515)75:10<2507::aid-cncr2820751017>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 11.Yoon NH, Lee HY, Kwak MS, Choi KS, Jun JK, Kim MK, et al. Comparison of satisfaction with cancer screening at mobile van and static sites: National Cancer Screening Program in Korea. Jpn J Clin Oncol. 2009;39:169–174. doi: 10.1093/jjco/hyn156. [DOI] [PubMed] [Google Scholar]
- 12.Hisamichi S. Screening for gastric cancer. World J Surg. 1989;13:31–37. doi: 10.1007/BF01671151. [DOI] [PubMed] [Google Scholar]
- 13.Kim CW, Lee SY, Moon OR. Inequalities in cancer incidence and mortality across income groups and policy implications in South Korea. Public Health. 2008;122:229–236. doi: 10.1016/j.puhe.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Murakami R, Tsukuma H, Ubukata T, Nakanishi K, Fujimoto I, Kawashima T, et al. Estimation of validity of mass screening program for gastric cancer in Osaka, Japan. Cancer. 1990;65:1255–1260. doi: 10.1002/1097-0142(19900301)65:5<1255::aid-cncr2820650536>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 15.Sugawara N, Hirasawa Y, Morimoto T, Sibuki S, Kogane T, Sato H, et al. An investigative report about health state of old age groups at first screening for gastric mass survey. J Gastroenterol Mass Surv. 1992;95:184–186. [Google Scholar]
- 16.Fukao A, Hisamichi S, Takano A, Sugawara N. Accuracies of mass screening for gastric cancer-test sensitivity and program sensitivity. J Gatstroenterol Mass Surv. 1992;97:59–63. [Google Scholar]
- 17.Sugahara N, Sibuki S, Hirasawa Y, Morimoto T. Characteristics of false negative cases. Stomach Intestine. 1991;26:1357–1362. [Google Scholar]
- 18.Ishida T, Suematsu T, Oomayashi K, Takada Y, Kimura S, Suematsu C. Measurement of accuracy of stomach mass screening by population-based cancer registration. J Gastroenterol Mass Surv. 1994;32:9–16. [Google Scholar]
- 19.Hattori M, Fujita M, Hosokawa O, Yamazaki S. A clinico-pathological evaluation of false negative cases in gastric cancer mass survey. J Gastroenterol Mass Surv. 1998;36:468–475. [Google Scholar]
- 20.Abe S, Shibuya D, Noguchi T, Shimada T. An estimate of the false-negative rate of mass-screening for gastric carcinoma. J Gastroenterol Mass Surv. 2000;38:475–482. [Google Scholar]
- 21.American Society for Gastrointestinal Endoscopy. Principles of training in gastrointestinal endoscopy. From the ASGE. Gastrointest Endosc. 1999;49:845–853. [PubMed] [Google Scholar]
- 22.Pentti M, Muller J, Janda M, Newman B. Views of supervisors of colonoscopy training on quality issues for the national bowel cancer screening program in Australia. J Gastroenterol Hepatol. 2009;24:209–213. doi: 10.1111/j.1440-1746.2008.05603.x. [DOI] [PubMed] [Google Scholar]
- 23.National Cancer Center. Development on evaluation of a comprehensive regional cancer center and operational framework for the specified regional cancer center. 0720620. Goyang: National Cancer Center; 2008. pp. 160–163. [Google Scholar]