Abstract
The effect of heart rate and variation during cardiac computed tomography (CT) on the examination quality. The purpose of this study is to investigate whether it is possible to predict heart rate and range during enhanced cardiac computed CT scan from previous non-enhanced cardiac CT scan. Electrocardiograph (ECG) files from 112 patients on three types of cardiac 64-slice CT (non-enhanced, prospective ECG-triggered and retrospective ECG-gated enhanced scans) were recorded. The mean heart rate, range (defined as difference between maximal and minimal heart rates) and the range ratio (defined as maximal heart rate divided by minimal heart rate) during the scans were compared. Scan time was 4.8, 4.6, and 7.3 s on non-enhanced, prospective ECG-triggered and retrospective ECG-gated scans, respectively (p < 0.0001). The heart rates were not significantly different (60 ± 9 beats per minute (bpm), 60 ± 9 and 61 ± 10 bpm; p = 0.64). Heart rate on the enhanced scan markedly correlated with that of the non-enhanced scan (r = 0.78 and 0.74). In contrast, the ranges of heart rate were 2 ± 5, 4 ± 8, and 8 ± 21 bpm, with different range ratios (1.04, 1.07, and 1.14; p < 0.0001). Correlation of heart rate ranges between non-enhanced scan versus prospective ECG-triggered scan was low (r = 0.27) and that between non-enhanced scan versus retrospective ECG-gated scan negligible (r = −0.027).Heart rate on enhanced cardiac CT, in most cases, can be predicted from a non-enhanced scan. Heart rate range on enhanced cardiac CT, however, is hard to predict from the non-enhanced scan.
Key words: Cardiac, computed tomography, heart rate, heart rate range
Introduction
Image quality and detection of stenosis in coronary computed tomography (CT) angiography (CTA) is affected by heart rate and the range during acquisition.1–6 With single-source 64-slice CTA, most investigators recommend lowering the patient’s heart rate to <65 beats per minute (bpm) to achieve stable image quality.7–10 In this range, diagnostic image quality can be obtained for all coronary arteries at a single reconstruction interval at mid-diastole.11 When higher heart rates are included however, additional reconstructions at late systole may be required for optimal visualization of the right coronary artery.12 The variation of heart rate alters the data acquisition window of the cardiac cycle, which may result in the inclusion of systole. In order to reduce and stabilize the heart rate, β-blocker is often used on cardiac CT, administered orally at 1 to 2 h(s) prior to the examination or/and intravenously just before the examination.
Practitioners have to decide the acquisition protocol depending on the heart rate. electrocardiograph (ECG) editing; i.e., by arbitrarily modifying the position of the temporal windows within the cardiac cycle, to correct and compensate for part or all of the artifacts,13 is not perfect but is the most robust imaging technique for instable heart rates. As it needs retrospective ECG-gated CTA without ECG-correlated tube current modulation however, it involves a high radiation dose. In patients with a relatively stable heart rate, ECG-correlated tube current modulation, reducing radiation exposure by 30% to 50%, is used.14,15 In this technique, the practitioner has to determine the peak current interval relative to the cardiac phase and the minimal current value relative to the maximal current. Recently devised prospective ECG-triggered coronary 64-slice CTA16 needs low and stable heart rate.17
In these circumstances, prediction of heart rate and variation is important on 64-slice CTA for deciding use of β-blockers and the determination of scanning protocol. The purpose of this study is to investigate whether it is possible to predict heart rate and range during enhanced cardiac CT from non-enhanced cardiac CT.
Materials and Methods
Patients
The comparative study between prospective ECG-triggered and retrospective ECG-gated cardiac 64-slice CTA18 was approved by the local hospital ethics committee and all patients provided written informed consent. This study analyzed heart rate and heart rate range of 112 patients (63 males and 49 females, 64 ± 11 years old: ranged, 35–87 years) undergoing coronary artery calcium scoring and two types of coronary CTA. The mean body mass index was 24 ± 13 kg/m2. Of 112 patients, 87 (78%) were symptomatic and 71 (64%) had coronary risk factors. Using a 64-slice CT scanner (Lightspeed VCT, GE Healthcare, Waukesha, WI), 86 patients were scanned with retrospective ECG-gated CTA first, followed by prospective ECG-triggered CTA and the remaining 26 patients were scanned in reverse order. The time interval between the two scans was 5 min. To minimize motion artifacts, patients with an initial heart rate ≥60 bpm (n = 83) were given with oral β-blocker (metoprolol 40 mg) to achieve a target heart rate of 50–60 bpm. No additional intravenous β-blocker, at the time of the examination, was used. Except for two patients with contraindications, nitroglycerin spray (one push, Mycor spray, Astellas pharma, Tokyo, Japan) was used 5 min before coronary CTA scan to dilate the diameters of the coronary arteries.19
Data Acquisition
Each scan was performed 5 s after breath-hold at mild-inspiration in order to minimize range of heart rate, which was investigated on non-enhanced cardiac CT.20 The ECG files were obtained using three lead ECG during the CT scan, and the data were transferred to an external PC for further analysis.
The use of contrast media included 10 ml Iopamiron® 370 (Bayer-Schering Pharma, Berlin, Germany), followed by 25 ml saline chaser for test bolus scan and contrast media (volume = body weight (in kg) × 0.6 ml), followed by 25 ml saline chaser for each type of coronary CTA. The injection rate of contrast media and saline was 0.06 × body weight ml/s (the contrast media was administered during 10 s).
Patients with atrial fibrillation and having beat-to-beat variability exceeding 20 bpm during pre-examination baseline breathing were excluded from analysis.21 This was because such types of heartbeat might disturb the analysis of the effect of contrast media or scan time on heart rate.
Electrocardiograph Data Evaluation and Statistical Analysis
Mean heart rate, the range (defined as difference between maximal and minimal heart rates) and the range ratio (defined as maximal heart rate divided by minimal heart rate) during scanning were compared between the three scans. Depending on the data distribution, one-factor analysis of variance (ANOVA) or Kruskal–Wallis was used. Mean heart rate and the range on prospective ECG-triggered and retrospective ECG-gated enhanced scans in relation to the non-enhanced scan were tested using Pearson’s correlation coefficient and Bland–Altman analysis with a 95% confidence interval (CI). The degree of Pearson’s product moment correlation coefficient (r) was regarded as follows: 0 to 0.2, no or negligible; 0.2 to 0.4, low; 0.4 to 0.6, moderate; 0.6 to 0.8, marked and 0.8 to 1.0, high. Student’s t test was used to determine the difference in acquisition time, heart rate, and the range between two groups divided by scan order. P values <0.05 were considered to identify significant differences.
Results
All patients were able to hold their breath on the three scans. All scans were performed without any significant adverse effect of contrast material. The data acquisition time was 4.8 ± 1.1 s (median, 4.7 s; 95% CI, 4.5 and 4.9 s) in non-enhanced scan, 4.6 ± 1.2 s (median, 4.5 s; 95% CI, 4.2 and 4.8 s) in prospective ECG-triggered scan and 7.3 ± 1.0 s (median, 7.2 s; 95% CI, 7.0 and 7.3 s) in retrospective ECG-gated scan (Kruskal–Wallis test; p < 0.01). The data acquisition time was not different between two groups divided by scan order in non-enhanced, prospective ECG-triggered and retrospective ECG-gated scans (p = 0.23, 0.64, and 0.47). The body weight was 62 ± 14 (38–103) kg, and the total contrast volumes (test bolus scan, prospective ECG-triggered, and retrospective ECG-gated CTA) administered was 85 ± 16 (56–134) ml. The effective radiation dose, estimated based on the dose-length product, was 0.9 ± 0.2, 4.1 ± 1.8, and 19.8 ± 3.5 mSv in non-enhanced, prospective ECG-triggered and retrospective ECG-gated scans, respectively.
Heart Rate
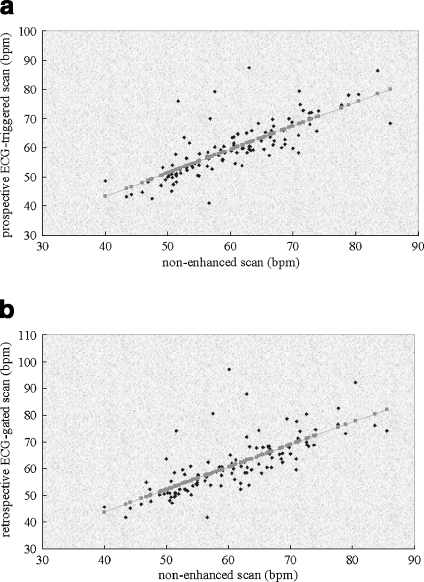
Heart rates were not significantly different between non-enhanced scan (60 ± 9 bpm), prospective ECG-triggered scan (60 ± 9 bpm), and retrospective ECG-gated scan (61 ± 10 bpm; one-factor ANOVA; p = 0.64). Heart rates markedly correlated between non-enhanced scan versus prospective ECG-triggered scan (r = 0.78 (95% CI, 0.70 and 0.85); p < 0.01) and non-enhanced scan versus retrospective ECG-gated scan (r = 0.74 (95% CI; 0.64 and 0.81); p < 0.01) (Fig. 1). Results in the Bland–Altman analysis are shown Table 1.
Fig 1.
Scatterplots of heart rate between non-enhanced scan and enhanced scan a HR (prospective ECG-triggered scan) = 0.804 × HR (non-enhanced scan) + 11.2 (p < 0.00001; r = 0.78 (95% CI, 0.70 and 0.85)); b HR (retrospective ECG-gated scan) = 0.840 × HR (non-enhanced scan) + 10.2 (p < 0.00001; r = 0.74 (95% CI, 0.64 and 0.81)) HR = heart rate.
Table 1.
Non-enhanced Scan versus Prospective Scan and Non-enhanced Scan Versus Retrospective Scan
| Non-enhanced | Prospective | Retrospective | Non-enhanced versus prospective | Non-enhanced versus retrospective | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Bias | Limits of agreement | Bias | Limits of agreement | |
| Heart rate (bpm) | 60.5 ± 9.1 | 59.8 ± 9.3 | 0.6 | −11.3 to 12.6 | |||
| Heart rate range (bpm) | 2.3 ± 4.7 | 3.9 ± 7.9 | −0.5 | −14.5 to 13.4 | |||
| Heart rate (bpm) | 60.5 ± 9.1 | 61.0 ± 10.3 | −1.6 | −17.4 to 14.2 | |||
| Heart rate range (bpm) | 2.3 ± 4.7 | 8.2 ± 21.0 | −5.9 | −48.5 to 36.4 | |||
Non-enhanced and enhanced scans were compared using Bland–Altman analysis
SD standard deviation
The heart rate was not different between two groups divided by scan order in non-enhanced, prospective ECG-triggered and retrospective ECG-gated scans (p = 0.46, 0.25, and 0.17).
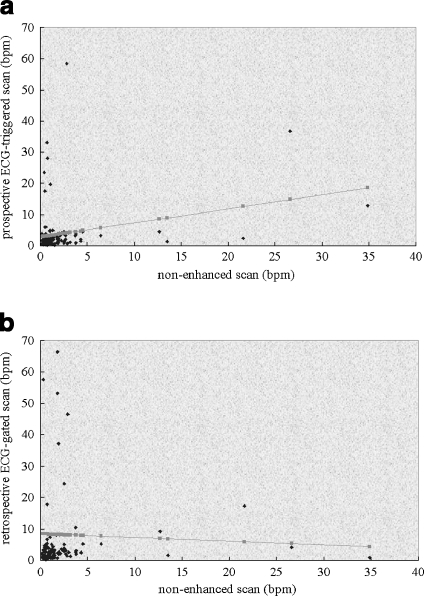
Heart Rate Range
Heart rate ranges were non-enhanced scan: 2 ± 5 bpm (median, 1.3 bpm; 95% CI, 1.1 and 1.6 bpm), prospective ECG-triggered scan: 4 ± 8 bpm (median, 2.1 bpm; 95% CI, 1.7 and 2.5 bpm), and retrospective ECG-gated scans: 8 ± 21 bpm (median, 2.7 bpm; 95% CI, 2.2 and 3.2 bpm), with different heart rate range ratios (1.04, 1.07, and 1.14, Kruskal–Wallis test; p < 0.00001). The heart rate range >5 bpm occurred in 5.4% (6/112), 8.9% (10/112) and 20.5% (23/112) in non-enhanced, prospective ECG-triggered and retrospective ECG-gated scans, respectively. Similarly, the heart rate range >10 bpm occurred in 4.5% (5/112), 7.1% (8/112), and 11.6% (13/112). Correlation of heart rate ranges between non-enhanced scan versus prospective ECG-triggered scan was low (r = 0.27 (95% CI, 0.09 and 0.43)) and that between non-enhanced scan versus retrospective ECG-gated scan negligible (r = −0.027 (95% CI, −0.21 and 0.16)) (Fig. 2). Results in the Bland–Altman analysis are shown Table 1. In summary, marked degree of range occurred in both enhanced and non-enhanced scans. Marked range in non-enhanced scan does not predict the same during enhanced scanning and vice versa. The heart rate range was not different between the two groups divided by scan order in non-enhanced, prospective ECG-triggered and retrospective ECG-gated scans (p = 0.18, 0.70, and 0.24).
Fig 2.
Scatterplots of heart rate range between non-enhanced scan and enhanced scan a HR range (prospectiveECG-triggered scan) = 0.285 × HR range (non-enhanced scan) + 2.8 (p < 0.01; r = 0.27 (95% CI, 0.09 and 0.43)); b HR range (retrospective ECG-gated scan) = −0.118 × HR range (non-enhanced scan) + 8.48 (p = 0.781; r = −0.027 (95% CI, −0.21 and 0.16)) HR = heart rate.
Discussion
This study compares heart rate and range between non-enhanced scan and enhanced scans with two data acquisition times. The results of our study suggest that (1) heart rate on enhanced cardiac CT, in most cases, can be predicted from a non-enhanced scan, (2) heart rate range on enhanced cardiac CT is not relevant to non-enhanced scan and is greater than non-enhanced scan, (3) a shorter scan time is advantageous for reducing heart rate range.
We found one previous study by Zhang et al., using relatively longer scan times (13–14 s for non-enhanced and enhanced scans), examining heart rate and range.21 They showed that injection of contrast media had no significant effect on heart rate, which is in line with our study. They showed that percentage of beats outside a ±5 bpm about the mean was not different between non-enhanced (3.0%) and enhanced (3.3%) scans. In contrast to this, our results showed greater heart rate range on the enhanced scan compared with the non-enhanced scan. The reason for the difference is not clear; however, we consider that greater heart rate range on the enhanced scan may be explained by the influence of increased venous return associated with bolus injection, the effect of iodine and psychological reaction.
Possible greater heart rate range with a longer scan time seems to be understandable. For 64-slice CT, a typical scan time required to image the heart is approximately 5–15 s, depending on CT scanner model.21 A relatively shorter scan time of the CT scanner we used, is likely to offer small heart rate range. Recently, next-generation 320-detector row CT, enabling full heart coverage in one cardiac cycle, has been announced. This technology has a definite advantage in terms of heart rate range.
We would like to emphasize the importance of non-enhanced CT. Compared with non-enhanced scan for calcium scoring, coronary CTA uses higher radiation dose, especially with retrospective ECG-gating algorithm. The scan coverage is set up visually on the topogram; however, the position of the scanning start can vary according to individual anatomy.22 To avoid repeated scan, there is a tendency to expose tissues beyond the boundaries of the volume to be imaged. Therefore, optimization of scan coverage from non-enhanced CT scan data is important. In addition, one must be aware that the quality of the CTA is likely to be impaired or non-diagnostic if large quantities of coronary calcium are found on non-enhanced CT.23,24 Thus as mentioned above, apart from ECG information, we need get the most out of non-enhanced prior to coronary CTA.
We acknowledge the following limitation to our study. Enhanced scans were performed twice, and the numbers of patient were not the same level between two types of scan order. The effect of previously injected contrast is not negligible although this is likely to be minimized after the scan interval of 5 min. The fact that the patient was aware of what is going to happen to them for the second of the contrast studies might lead them less anxious.
In conclusion, the results suggest that heart rate on enhanced cardiac CT, in most cases, can be predicted from the non-enhanced scan. This is useful for determining protocol, i.e., helical or axial scan and the pitch in case of helical scan. In contrast, heart rate range in enhanced scan is greater than non-enhanced scan and is hard to predict from non-enhanced scan. In this respect, a shorter scan time has a definite advantage.
Acknowledgements
This study was financially supported by Tsuchiya Foundation (http://www.tsuchiya-foundation.or.jp), Hiroshima, Japan.
Contributor Information
Jun Horiguchi, Phone: +81-82-8791111, Email: horiguchi@hiroshimairyo.or.jp.
Hideya Yamamoto, Email: hideyayama@hiroshima-u.ac.jp.
Ryuichi Arie, Email: rarie1979@yahoo.co.jp.
Masao Kiguchi, Email: kiguchi@hiroshima-u.ac.jp.
Chikako Fujioka, Email: fujioka@hiroshima-u.ac.jp.
Megu Ohtaki, Email: ohtaki@hiroshima-u.ac.jp.
Yasuki Kihara, Email: ykihara@hiroshima-u.ac.jp.
Kazuo Awai, Email: awai@hiroshima-u.ac.jp.
References
- 1.Kroft LJM, Roos A, Geleijns J. Artifacts in ECG-synchronized MDCT coronary angiography. AJR. 2007;189:581–591. doi: 10.2214/AJR.07.2138. [DOI] [PubMed] [Google Scholar]
- 2.Herzog C, Arning-Erb M, Zangos S, et al. Multi-detector row CT coronary angiography: influence of reconstruction technique and heart rate on image quality. Radiology. 2006;238:75–86. doi: 10.1148/radiol.2381041595. [DOI] [PubMed] [Google Scholar]
- 3.Giesler T, Baum U, Ropers D, et al. Noninvasive visualization of coronary arteries using contrast-enhanced multidetector CT: influence of heart rate on image quality and stenosis detection. AJR. 2002;179:911–916. doi: 10.2214/ajr.179.4.1790911. [DOI] [PubMed] [Google Scholar]
- 4.Wintersperger BJ, Nikolaou K, Ziegler F, et al. Image quality, motion artifacts and reconstruction timing of 64-slice coronary computed tomography angiography with 0.33-second rotation speed. Invest Radiol. 2006;41:436–442. doi: 10.1097/01.rli.0000202639.99949.c6. [DOI] [PubMed] [Google Scholar]
- 5.Caussin C, Larchez C, Ghostine S, et al. Comparison of coronary minimal lumen area quantification by 64-slice computed tomography versus intravascular ultrasound for intermediate stenosis. Am J Cardiol. 2006;98:871–876. doi: 10.1016/j.amjcard.2006.04.026. [DOI] [PubMed] [Google Scholar]
- 6.Leschka S, Scheffel H, Husmann L, et al. Effect of decrease in heart rate variability on the diagnostic accuracy of 64-MDCT coronary angiography. AJR. 2008;190:1583–1590. doi: 10.2214/AJR.07.2000. [DOI] [PubMed] [Google Scholar]
- 7.Fine JJ, Hopkins CB, Ruff N, Newton FC. Comparison of accuracy of 64-slice cardiovascular computed tomography with coronary angiography in patients with suspected coronary artery disease. Am J Cardiol. 2006;97:173–174. doi: 10.1016/j.amjcard.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 8.Leber AW, Knez A, Ziegler F, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005;46:147–154. doi: 10.1016/j.jacc.2005.03.071. [DOI] [PubMed] [Google Scholar]
- 9.Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552–557. doi: 10.1016/j.jacc.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 10.Achenbach S. Computed tomography coronary angiography. J Am Coll Cardiol. 2006;48:1919–1928. doi: 10.1016/j.jacc.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 11.Leshka S, Husmann L, Desbiolles LM, et al. Optimal image reconstruction intervals for non-invasive coronary angiography with 64-slice CT. Eur Radiol. 2006;16:1964–1972. doi: 10.1007/s00330-006-0262-x. [DOI] [PubMed] [Google Scholar]
- 12.Ferencik M, Nomura CH, Maurovich-Horvat P, et al. Quantitative parameters of image quality in 64-slice computed tomography angiography of the coronary arteries. Eur J Radiol. 2006;57:373–379. doi: 10.1016/j.ejrad.2005.12.023. [DOI] [PubMed] [Google Scholar]
- 13.Cademartiri F, Mollet NR, Runza G, et al. Improving diagnostic accuracy of MDCT coronary angiography in patients with mild heart rhythm irregularities using ECG editing. AJR. 2006;186:634–638. doi: 10.2214/AJR.04.1797. [DOI] [PubMed] [Google Scholar]
- 14.Jakobs TF, Becker CR, Ohnesorge B, et al. Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol. 2002;12:1081–1086. doi: 10.1007/s00330-001-1278-x. [DOI] [PubMed] [Google Scholar]
- 15.Hausleiter J, Meyer T, Hadamitzky M, et al. Radiation dose estimates from cardiac multislice computed tomography in daily practice: impact of different scanning protocols on effective dose estimates. Circulation. 2006;113:1305–1310. doi: 10.1161/CIRCULATIONAHA.105.602490. [DOI] [PubMed] [Google Scholar]
- 16.Hsieh J, Londt J, Vass M, Li J, Tang X, Okerlund D. Step-and-shoot data acquisition and reconstruction for cardiac X-ray computed tomography. Med Phys. 2006;33:4236–4248. doi: 10.1118/1.2361078. [DOI] [PubMed] [Google Scholar]
- 17.Horiguchi J, Kiguchi M, Fujioka C, et al. Radiation dose, image quality, stenoses measurement and CT densitometry using prospective electrocardiograph-triggered coronary 64-MDCT angiography—a phantom study. AJR. 2008;190:315–320. doi: 10.2214/AJR.07.2191. [DOI] [PubMed] [Google Scholar]
- 18.Hirai N, Horiguchi J, Fujioka C, et al. Prospective electrocardiography-triggered versus retrospective electrocardiography-gated 64-slice coronary CT angiography: image quality, stenoses assessment and radiation dose. Radiology. 2008;248:424–430. doi: 10.1148/radiol.2482071804. [DOI] [PubMed] [Google Scholar]
- 19.Dewey M, Hoffmann H, Hamm B. Multislice CT coronary angiography: effect of sublingual nitroglycerine on the diameter of coronary arteries. Rofo. 2006;178:600–604. doi: 10.1055/s-2006-926755. [DOI] [PubMed] [Google Scholar]
- 20.Horiguchi J, Shen Y, Hirai N, et al. Timing on 16-slice scanner and implications for 64-slice cardiac CT: do you start scanning immediately after breath-hold? Acad Radiol. 2006;13:173–176. doi: 10.1016/j.acra.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Zhang J, Fletcher JG, Harmsen WS, et al. Analysis of heart rate and heart rate variation during cardiac CT examinations. Acad Radiol. 2008;15:40–48. doi: 10.1016/j.acra.2007.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paul JF, Abada HT. Strategies for reduction of radiation dose in cardiac multislice CT. Eur Radiol. 2007;17:2028–2037. doi: 10.1007/s00330-007-0584-3. [DOI] [PubMed] [Google Scholar]
- 23.Stillman AE, Oudkerk M, Ackerman M, et al. Use of multidetector computed tomography for the assessment of acute chest pain: a consensus statement of the North American Society of Cardiac Imaging and the European Society of Cardiac Radiology. Eur Radiol. 2007;17:2196–2207. doi: 10.1007/s00330-007-0677-z. [DOI] [PubMed] [Google Scholar]
- 24.Liu X, Zhao X, Huang J, et al. Comparison of 3D free-breathing coronary MR angiography and 64-MDCT angiography for detection of coronary stenosis in patients with high calcium scores. AJR. 2007;189:1326–1332. doi: 10.2214/AJR.07.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]