Abstract
Adenoidectomy and tonsillectomy, indicated for children with recurrent or persistent symptoms of infection or hypertrophy, are among the most frequent operations performed in children. This study was carried out for investigating the microbial flora of the tonsils and adenoids regarding to core and surface microorganisms and also pathogen microrganisms’ beta-lactamase production rate. Cultures were taken from the core and surface of tonsils and adenoids of the 91 patients at the time of the surgery for tonsillectomy and adenoidectomy. Aerobic and anaerobic cultures were inoculated and identified. Beta-lactamase production was detected also. The most frequently isolated aerobic microorganisms were Streptococcus viridans and Neisseria spp. The number of the microorganisms isolated from the tonsil core compared to the surface of the tonsils was found statistically insignificant (P > 0.05). The number of the adenoid surface aerobic microorganisms was found higher from the adenoid core (P < 0.05). The amount of adenoid and tonsil core anaerobic microorganisms were alike. The patients’ preoperative antibiotherapy whether using beta-lactam or beta-lactamase resistant were compared for beta-lactamase producing bacteria production and the number of beta-lactamase producing bacteria were found statistically insignificant (P > 0.05). The togetherness of Staphylococcus aureus and other beta-lactamase producing bacteria was found statistically significant (P < 0.05). This study demonstrates that there is polymicrobial aerobic-anaerobic flora in both adenoids and tonsils. There was a close relationship between the bacteriology of the tonsil and adenoid flora. Staphylococcus aureus and and other beta-lactamase producing bacteria may be responsible for treatment failures in patients with tonsillitis.
Keywords: Bacteriology, Tonsil, Adenoids, Beta-lactamases
Introduction
Recurrent tonsillitis is among the most common diseases of the childhood. These children are prescribed various antimicrobial treatments but these treatments are usually insufficient and surgery is required. Tonsil surface swabs which are commonly used in recurrent tonsillitis do not reflect the real pathogens so that the antibiotics chosen according to the surface swabs are not appropriate [1–5].
Microorganisms other than Group A Beta Haemolytic Streptococcus (GABHS) may be the cause of chronic tonsillitis. Especially in recent years the domination of the beta-lactamase producing bacteria (BLPB) such as Staphylococcus aureus and Haemophilus influenzae in microflora cause penicillin resistance [6, 7]. Several researchers have claimed that the failure of antibiotherapy may be due to the underestimation of the resistant microorganisms [6–8].
The objectives of this study are to determine the core and surface flora of the tonsils and adenoids, the reflection of the core flora by the surface swabs and the pathogen microorganisms’ beta-lactamase production rate.
Patients and Method
This study was performed on 91 pediatric patients who had been subjected to adenotonsillectomy due to recurrent tonsillitis and/or obstructive symptoms during the time period from February 2004 to June 2005 in the Otorhinolaryngology Clinic of Ankara Numune Research and Education Hospital. The criteria such as recurrent tonsillitis and/or obstructive symptoms of the patients, number of recurrent tonsillitis in a year, last antibiotic prescription date and the sort of antibiotics used in last 3 months were noted in patients history. None of the patients used antibiotics in 15 days prior to operation.
Preoperative swabs were taken from the surface of tonsils and adenoids. Afterwards, tonsillectomy and adenoidectomy materials irrigated with sterile saline solution were divided in two parts by a sterile knife, and then aerobic and anaerobic swab samples were taken from the core. Aerobic samples were transported to the laboratory in less than 15 min and incubated immediately. Anaerobic samples were inoculated immediately in the operation room and transported to the laboratory in Genbaganaer packages (BioMerieux/France). Aerobic samples were inoculated on 5% sheep blood agar, Eosin Methylene Blue Agar (EMB) and Haemophilus media (HAEM) (BioMerieux/France) and evaluated after incubation for 24 h at 37°C. All microorganisms isolated from these media were Gram stained and identified conventionally. ApiNH (BioMerieux/France) kit were used for the identification of the Haemophilus spp. Gram stained Candida spp. were identified by using ID32C (BioMerieux/France) kit. Anaerobic samples taken from the core of tonsils and adenoids inoculated on anaerobic sheep blood immediately in the operation room and transported to the laboratory in Genbaganaer packages (BioMerieux/France) were incubated for 48–96 h at 37°C. Growing anaerobic bacteria were identified with VITEK ANI (BioMerieux/France) system. Beta-lactamase production was detected by Nitrocephine (Cefinase/BBL/France) disc method.
Statistical analysis was evaluated using chi-square, Mc Nemar, Wilcoxon and Kruskal–Wallis tests with the SPSS 10.0 program compiled for WINDOWS.
Results
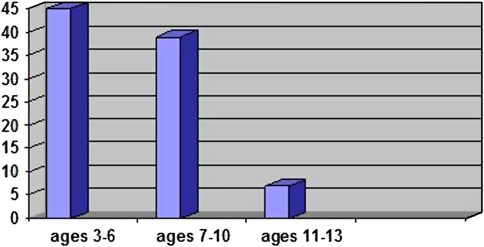
The study includes 91children, 54 males (59.3%), 37 females (40.7%) aged 3–13 years (mean age 6.6 years) The distrubution af the children’s age was shown in Fig. 1.
Fig. 1.
The distribution of the patient’s ages
Statistical analysis done with McNemar test indicates that; Streptococcus viridans and beta-lactamase producing Neisseria spp. were isolated more from the tonsil surface swabs than from the tonsil core samples (P < 0.05); however, Coagulase Negative Stapyhlococci (CNS) were isolated more from the core samples (P < 0.05). There was no significant difference between tonsil surface and core for other microorganisms (P > 0.05).
In adenoid surface swabs S. viridans, Neisseria spp., H. influenzae, and H. parainfluenzae spp. were isolated more as compared to the core samples (P < 0.05). There was no statistically significant difference between the adenoid surface and the core with respect to other microorganisms (P > 0.05).
The most frequently isolated microorganisms from the tonsil surface were S. viridans (30.6%), Neisseria spp. (23.3%), H. influenzae (11%) and from the tonsil core were S. viridans (29.3%), Neisseria spp. (19.7%), H. influenzae (15.7%).
When the number of microorganisms isolated from the tonsil core were compared with the surface of tonsils by using Wilcoxon test; no statistically difference was found (P > 0.05).
The most frequently isolated microorganisms from adenoid surface were S. viridans (26.9%), Neisseria spp. (22.9%) and H. influenzae (16.8%). S. viridans (22.8%), Neisseria spp. (21%) and CNS (14.8%) were isolated most frequently from adenoid core samples. When adenoid surface and core aerob microorganism production were compared by using Wilcoxon test, adenoid surface microorganism production was found statistically significant (P < 0.05).
The amount of isolated aerobic microorganisms from adenoid and tonsil surface were found similar and there was no significant difference (P > 0.05). However, when the amount of anaerobic microorganisms isolated from adenoid and tonsil surface were compared, significantly more microorganisms were isolated from tonsil core cultures (P < 0.05).
The percentages of the microorganisms isolated from tonsil and adenoids surface and core cultures were listed in Table 1. In Table 2 listed were the aerob microorganisms isolated from tonsil and adenoid surface and core cultures with the number and percentage of BLPB.
Table 1.
The percentage of aerobic microorganisms isolated from tonsil and adenoid tissue
| Aerobic bacteria | Tonsil surface* % (n = 88) | Tonsil core* % (n = 88) | Adenoid surface** % (n = 76) | Adenoid core** % (n = 76) |
|---|---|---|---|---|
| S. pneumoniae | 2.7 | 3 | 5.5 | 5.6 |
| S. viridans | 30.6 | 29.3 | 26.9 | 22.8 |
| GABHS | 2.7 | 6.1 | 2.9 | 4.3 |
| NANB BHS | 0.4 | 0.9 | 0.4 | 1.2 |
| CNS | 8.9 | 10.5 | 9.6 | 14.8 |
| S. aureus | 6.6 | 6.1 | 3.9 | 8 |
| H. influenzae | 11 | 15.7 | 16.8 | 13 |
| H. parainfluenzae | 5.6 | 2.6 | 6 | 3.1 |
| Neisseria spp. | 23.3 | 19.7 | 22.9 | 21 |
| Diphteroid | 4 | 3.5 | 3.5 | 5 |
| Micrococcus spp. | 1.1 | 1.3 | 0.4 | – |
| Moraxella catarrhalis | 0.4 | – | 0.4 | – |
| Candida albicans | 1.5 | 0.8 | 0.4 | – |
| Non-albicans candida spp. | 0.4 | – | – | – |
| Bacillus spp | 0.4 | – | – | 0.6 |
| Pseudomanas aeruginosa | 0.4 | 0.9 | 0.4 | 0.6 |
| Total | 100 | 100 | 100 | 100 |
GABHS—Group A Beta Haemolytic Streptococcus; NANB BHS—Non A Non BBeta Haemolytic Streptococcus; CNS—Coagulase Negative Staphylococci
* 3 patients with no bacterial isolation from tonsil surface and core were not included in calculation
** 15 patients with no bacterial isolation from adenoid core culture were not included in calculation
Table 2.
Aerobic microorganisms isolated from tonsil and adenoid tissue along with the number and percentage of beta-lactamase producing bacteria
| Aerob bacteria | Tonsil surface* | Tonsil core* | Adenoid surface** | Adenoid core** |
|---|---|---|---|---|
| No/β-lactamase (%) | No/β-lactamase (%) | No/β-lactamase (%) | No/β-lactamase (%) | |
| S. pneumoniae | 7/3 (42.8) | 7/3 (42.8) | 15/6 (40) | 9/2 (22.2) |
| S. viridans | 83/8 (9.6) | 67/7 (10.4) | 75/9 (12) | 37/1 (2.7) |
| GABHS | 7/0 (–) | 14/0 (–) | 8/0 (–) | 7/0 (–) |
| NANB BHS | 1/0 (–) | 2/0 (–) | 1/0 (–) | 2/0 (–) |
| CNS | 24/16 (66.6) | 24/8 (33.3) | 27/15 (55.5) | 24/16 (66.6) |
| S. aureus | 18/18 (100) | 14/14 (100) | 11/11 (100) | 13/13 (100) |
| H. influenzae | 30/16 (53.3) | 36/16 (44.4) | 47/23 (48.9) | 21/9 (42.8) |
| H. parainfluenzae | 15/6 (40) | 6/2 (33.3) | 17/6 (35.3) | 5/3 (60) |
| Neisseria spp. | 63/33 (52.4) | 45/23 (51.1) | 64/33 (51.5) | 34/19 (55.8) |
| Diphteroid | 11/4 (36.3) | 8/2 (25) | 11/3 (27.2) | 8/1 (12.5) |
| Micrococcus spp. | 3/1 (33.3) | 3/0 (–) | 1/0 (–) | – (–) |
| M. catarrhalis | 1/1 (100) | – (–) | 1/1 (100) | – (–) |
| Total | 267/106 (39.7) | 228/75 (32.8) | 279/107 (38.3) | 160/64 (40) |
GABHS—Group A Beta Haemolytic Streptococcus; NANB BHS—Non A Non BBeta Haemolytic Streptococcus; CNS—Coagulase Negative Staphylococci
* 3 patients with no bacterial isolation from tonsil surface and core were not included in calculation
** 15 patients with no bacterial isolation from adenoid core culture were not included in calculation
The patients who did not use preoperative antibiotherapy, who used beta-lactam antibiotics and who used beta-lactamase resistant antibiotics were compared for BLPB production and the number of BLPB were found lesser in patients who did not use preoperative antibiotherapy but there was no statistical difference (P > 0.05). Likely, there was no correlation between the type of the antibiotics and BLPB production rate (P > 0.05). The togetherness of S. aureus and other BLPB was significant (P < 0.05).
The amount of anaerobic microorganisms isolated from adenoid and tonsil core cultures were similar. In Table 3 the number of isolates from adenoid and tonsil core along with the percentage of BLPB were given.
Table 3.
Anaerobic microorganisms and the percentage of beta-lactamase producing bacteria from the tonsil and adenoid core cultures
| Anaerobic bacteria | Tonsil core | Adenoid core |
|---|---|---|
| No/β-lactamase (%) | No/β-lactamase (%) | |
| Peptostreptococcus | 10/0 (–) | 8/0 (–) |
| Actinomyces odontylicus | 2/0 (–) | 1/0 (–) |
| Peptostreptococcus prevotii | 1/0 (–) | 1/0 (–) |
| Peptostreptococcus anaerobius | 6/0 (–) | 5/0 (–) |
| Peptostreptococcus tetradius | 1/0 (–) | 2/0 (–) |
| P. asaccharolyticus | – (–) | 1/0 (–) |
| Bacteroides spp. | 2/1 (50) | 2/2 (100) |
| Bacteroides eggerthii | – (–) | 1/1 (100) |
| Veillonella parvula | 5/0 (–) | 5/0 (–) |
| TOTAL | 27/1 (3.7) | 26/4 (15.3) |
Discussion
Adenoidectomy and tonsillectomy done because of recurrent infection or obstruction are among the most frequently performed childhood operations [9]. Tonsils and adenoids which play a protective role against infections in healthy individuals, may become a reservoir for pathogenic microorganisms in case of chronic infections [6, 10, 11].
Like other infectious diseases, the determination of the pathogenic agent is important in antibiotic selection for the medical treatment of tonsillitis. The routine practice is the swab culture from the tonsil surface [12–14]. However, the tonsil surface swab mostly does not reflect the pathogenic agent [1–5]. Due to the constant contact of tonsil surface with the bacterial flora of oral secretion, the organisms isolated from the surface swabs may be the surface colonized bacteria instead of the real infectious agent. This situation discredits the reliability of the antibiotherapy chosen according to surface swabs. The therapies chosen according to surface swabs become insufficient to eradicate the pathogenic agent and cause chronic infections with tonsillectomy indication [13, 15].
Various ratios are reported for the diversity of tonsil surface and tonsil core cultures. The studies in the literature show that tonsil surface cultures do not reflect tonsil core microbiology in 30–70% of patients [1, 4, 5, 8, 11, 14–16]. There are also contrary studies in which no qualitative differences are found between tonsil surface and core flora [12, 13].
In our study, the total number of isolates produced, aerobic bacteria production rate and the type of bacteria were found similar in the tonsil surface and in the core; therefore, it can be assumed that tonsil surface cultures reflect the core flora. In adenoid surface cultures, there was a quantitatively more and statistically significant bacteria production compared to the core cultures (P < 0.001). This may be due to the difficulty of sampling adenoid core cultures. The agent pathogens in chronic tonsillitis are usually streptococci predominant mixed flora. However, microorganisms other than GABHS may cause chronic tonsillitis. Uppal et al. [11] studied 64 patients of chronic tonsillitis and the most frequently isolated bacteria was GABHS (39%), followed by S. aureus (36%) on tonsil surface and S. aureus (51.6%), followed by GABHS (34.3%) in tonsil core. Surow et al. [14] isolated S. aureus and GABHS most frequently and H. influenzae (2%) rarely on tonsil surface. From the tonsil core, they isolated S. aureus, H. influenzae and GABHS.
Ünal et al. [15] isolated Neisseria spp. (91.25%), S. pneumoniae (90%) and S. viridans (35%) from tonsil surface and Neisseria spp. (70%), S. pneumoniae (63.75%) and S. aureus (32.5%) from tonsil core. In another study, İnci et al. [8] isolated S. aureus (57.8%), GABHS (26.3%) and H. influenzae (21%) from the tonsil surface and S. aureus (52%), H. influenzae (26%) and GABHS (20%) from the tonsil core.
In our study most frequently isolated aerobic bacteria from the tonsil surface swabs were S. viridans (30.6%), Neisseria spp. (23.3%), H. influenzae (11%) and CNS (8.9%); from tonsil core cultures were S. viridans (29.3%), Neisseria spp. (19.7%), H. influenzae (15.7%) and CNS (10.5%). The most frequently isolated bacteria were S. viridans (26.9%), Neisseria spp. (22.9%), H. influenzae (16.8%), CNS (9.6%) from adenoid surface swabs and S. viridans (22.8%), Neisseria spp. (21%), CNS (14.8%), H. influenzae (13%) from adenoid core cultures.
We found quantitative and qualitative similarities between microorganisms isolated from tonsil and adenoid surface, when compared to the adenoid core, the number of bacteria isolated from the tonsil core was significantly greater (P < 0.05). Brook et al. [10] studied tonsil and adenoid core flora of 25 patients and isolated similar anaerobic microorganisms from both tissues. Mostly isolated anaerobic bacteria were Prevotella spp., Bacteroides fragilis, Fusobacterium spp., Peptostreptococci and Veilonella parvula. In another study, similar anaerobic microorganisms were also isolated from tonsil core in healthy children and in children with recurrent tonsillitis history but encapsulated and beta-lactamase producing Bacteroides spp. were isolated from the recurrent tonsillitis group. Predominant anaerobic microorganisms were Bacteroides spp., and Fusobacterium spp. [17].
In the literature, studies with higher rates of anaerobic microorganisms isolated [10, 18, 19], and also with lower rates which are similar to our study have been reported [1, 3, 20, 21]. The most frequently isolated anaerobic microorganism was peptostreptococcus similar to the literature [10, 13, 17]. Recurrent tonsillitis, resistant to penicillin treatment, is a serious medical problem in all ages. The failure of eradication of the streptococci in recurrent tonsillitis leads to acute romathoid fever and rarely to acute glomerulonephritis [6].
The probable causes of recurrence in chronic tonsillitis are; penicillin resistance due to the variations of the oropharyngeal flora, nonspecific antibiotic treatments, reinfection from the environment, supression of the antibody response due to the previous inappropriate antibiotic therapies [6, 22]. Several ideas explaining this phenomenon are; inappropriate and interrupted antibiotherapy, supression of host immunity due to unnecessary antibiotherapy, penicillin resistant l-form production of beta-haemolytic streptococci, inactivation of antibiotics by BLPB found in oropharyngeal and tonsillar flora such as S. aureus, H. influenzae, Bacteroides spp. and therefore protection of GABHS [6, 7].
The protection of penicillin sensitive bacteria by BLPB was first proven by Simon et al. in 1968 [23]. Kundsin and Miller [24] found higher S. aureus rates in patients with penicillin treatment failure. Brook et al. [7, 25, 26] determined that beta-lactamase producing S. aureus plays a role in transferring beta-lactamase resistance to bacteria formerly having no beta-lactamase resistance. We also found the togetherness of S. aureus with other BLPB statistically significant (P < 0.05).
Bernstein et al. [27] observed that the presence of BLPB before penicillin treatment and after penicillin treatment were 15 and 45% respectively. In our study, BLPB were isolated from all of the patients. Recurrent, multiple antibiotherapies in chronic adenotonsillitis may be the probable cause. We compared the patients who did not use antibiotics, who used beta-lactam antibiotics and who used beta-lactamase resistant antibiotics preoperatively for BLPB production rate. BLPB rate was lower but not statistically significant in patients with no preoperative antibiotic use. This may be due to the insufficient number of those patients. There were no significance between the type of antibiotic used and BLPB production rate as well (P > 0.05). This may be the result of various and multiple antibiotherapy usage history.
We found beta-lactamase production in Bacteroides spp. In 2 patients, Bacteroides spp. were isolated from tonsil core cultures and one was beta-lactamase positive. Also all 3 patients whom Bacteroides spp. had been isolated from, adenoid core cultures were beta-lactamase positive (Table 3). This data supports the theories lately discussed in the literature as; S. aureus, H. influenzae and Bacteroides spp. inactivate the penicillin and might shield penicilin susceptible pathogens like GABHS [6, 7, 28]. The significant togetherness of S. aureus and other BLPB in our study also supports these theories. It will be appropriate to investigate the rapidly progressing beta-lactamase resistance and resistance mechanisms and to confirm with suitable study designs.
Key Messages
Isolation of beta-lactamase producing bacteria in all patients shows that these pathogens often play a role in the etiology of recurrent tonsillitis and penicillin treatment for GABHS is ineffective. This situation leads to chronic tonsil and adenoid infections and to surgical therapy requirement. Furthermore the togetherness of S. aureus and other beta-lactamase producing bacteria, confirms the theory of S. aureus and other BLPBs may protect GABHS from penicillin by inactivating. Therefore, it may be appropriate to use beta-lactamase resistant antibiotics for the medical treatment of recurrent tonsillitis.
References
- 1.Brook I, Yocum P. Bacteriology of chronic tonsillitis in young adults. Arch Otolaryngol Head Neck Surg. 1984;110:803–805. doi: 10.1001/archotol.1984.00800380033009. [DOI] [PubMed] [Google Scholar]
- 2.DeDio RM, Lawrence WCT, McGowan KL, Wetmore RF, Handler SD, Potsic WP. Microbiology of the tonsils and adenoids in a pediatric population. Arch Otolaryngol Head Neck Surg. 1988;114:763–765. doi: 10.1001/archotol.1988.01860190067025. [DOI] [PubMed] [Google Scholar]
- 3.Gaffney RJ, Timon CI, Freeman DF, Walsh MA, Cafferkey MT. Bacteriology of tonsil and adenoid and sampling techniques of adenoidal bacteriology. Respir Med. 1993;87:303–308. doi: 10.1016/0954-6111(93)90028-X. [DOI] [PubMed] [Google Scholar]
- 4.Özek O, Eğilmez S, Ang O, Savaş I. A bacteriological study of chronic tonsillitis. Acta Otolaryngol. 1967;63:455–461. doi: 10.3109/00016486709128779. [DOI] [PubMed] [Google Scholar]
- 5.Timon CI, McAllister VA, Walsh MA, Cafferkey MT. Changes in tonsil bacteriology of recurrent acute tonsillitis: 1980 vs 1989. Respir Med. 1990;84:395–400. doi: 10.1016/S0954-6111(08)80074-1. [DOI] [PubMed] [Google Scholar]
- 6.Brook I. The role of beta-lactamase producing bacteria in the persistance of streptococcal tonsillar infection. Rev Infect Dis. 1984;6(5):601–607. doi: 10.1093/clinids/6.5.601. [DOI] [PubMed] [Google Scholar]
- 7.Brook I, Yocum P, Foote PA., Jr Changes in the core tonsillar bacteriology of recurrent tonsillitis: 1977–1993. Clin Inf Dis. 1995;21:171–176. doi: 10.1093/clinids/21.1.171. [DOI] [PubMed] [Google Scholar]
- 8.İnci E, Kakakullukçu B, Aygün G, Özdoğan A. Tonsil surface and core microflora in children undergone tonsillectomy for recurrent tonsillitis. Turkish Otolaryngol Arch. 2002;40(4):247–251. [Google Scholar]
- 9.Wiatrak BJ, Woolley AL. Pharyngitis and adenotonsillar disease. In: Cummings CW, Frederickson JM, Harker LA, Krause CJ, Schüller DE, editors. Otolaryngology Head and Neck Surgery. 2. St. Louis: Mosby Year Book, Inc; 1993. pp. 2795–2801. [Google Scholar]
- 10.Brook I, Shah K. Bacteriology of adenoids and tonsils in children with recurrent adenotonsillitis. Ann Otol Rhinol Laryngol. 2001;110:844–848. doi: 10.1177/000348940111000908. [DOI] [PubMed] [Google Scholar]
- 11.Uppal K, Bais AS. Tonsillar microflora, superficial surface versus deep. J Laryngol Otol. 1989;103:175–177. doi: 10.1017/S0022215100108370. [DOI] [PubMed] [Google Scholar]
- 12.Kielmovitch IH, Keleti G, Bluestone CD. Microbiology of obstructive tonsillar hypertrophy and recurrent tonsillitis. Arch Otolaryngol Head Neck Surg. 1989;115:721–724. doi: 10.1001/archotol.1989.01860300075021. [DOI] [PubMed] [Google Scholar]
- 13.Mitchelmore IJ, Reilly PG, Hay AJ, Tabaqchali S. Tonsil surface and core cultures in recurrent tonsillitis: prevalence of anaerobes and beta-lactamase producing organisms. Eur J Clin Microbiol Infect Dis. 1994;13(7):542–548. doi: 10.1007/BF01971304. [DOI] [PubMed] [Google Scholar]
- 14.Surow JB, Handler SD, Telian SA, Fleisher GR, Baranak CC. Bacteriology of tonsil surface and core in children. Laryngoscope. 1989;99:261–266. doi: 10.1288/00005537-198903000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Ünal A, Kürkçüoğlu S, Aslan A, Işıldak İ, Nalça Y. Tonsil surface and core flora in chronic recurrent tonsillitis. ENT Head Neck Surg. 1998;6(1):33–36. [Google Scholar]
- 16.Kumai A, Gupta V, Chandra K, Gupta P, Varshney S. Clinico bacteriological evaluation of surface and core microflora in chronic tonsillitis. Indian J Otolaryngol Head Neck Surg. 2005;57(2):118–120. doi: 10.1007/BF02907664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brook I, Foote P. Microbiology of the tonsils and adenoids. Arch Otolaryngol. 1989;115:528–530. doi: 10.1001/archotol.1989.01860280126033. [DOI] [PubMed] [Google Scholar]
- 18.Brodsky L, Koch R. Bacteriology and immunology of normal and diseased adenoids in children. Arch Otolaryngol Head Neck Surg. 1993;119:821–829. doi: 10.1001/archotol.1993.01880200021003. [DOI] [PubMed] [Google Scholar]
- 19.Brook I, Yocum P, Shah K. Surface vs core tonsillar aerobic and anaerobic flora in recurrent tonsillitis. JAMA. 1980;224:1696–1698. doi: 10.1001/jama.244.15.1696. [DOI] [PubMed] [Google Scholar]
- 20.Maw RA, Speller DCE. Are the tonsils and adenoids a reservoir of infection in otitis media with effusion? Clin Otolaryngol. 1985;10:265–269. doi: 10.1111/j.1365-2273.1985.tb00253.x. [DOI] [PubMed] [Google Scholar]
- 21.Teele DW, Healy GB, Tally FP. Persistant effusions of the middle ear. culture for anaerobic bacteria. Ann Otol Rhinol Laryngol. 1980;89(Suppl A):102–103. doi: 10.1177/00034894800890s327. [DOI] [PubMed] [Google Scholar]
- 22.Soylu L, Özşahinoğlu C, Aydoğan LB (1992) The inflamatory diseases of tonsil and adenoid tissue and tonsillectomy. Archive (1)157–165
- 23.Simon HJ, Sukai W. Staphylococcal antagonism to penicilin-G therapy of hemolytic streptococcal pharyngeal infection: effect of oxacillin. Pediatrics. 1968;31:463–469. [PubMed] [Google Scholar]
- 24.Kundsin RB, Miller JM. Significance of the Staphylococcus aureus carrier state in the treatment of disease due to group A streptococci. N Engl J Med. 1964;271:1395–1397. doi: 10.1056/NEJM196412312712705. [DOI] [PubMed] [Google Scholar]
- 25.Brook I. Direct and indirect pathogenicity of Branhamella catarrhalis. Drugs. 1986;31(suppl 3):97–102. doi: 10.2165/00003495-198600313-00021. [DOI] [PubMed] [Google Scholar]
- 26.Brook I. Infections caused by beta-lactamase producing Fusobacterium spp. in children. Pediatr Infect Dis J. 1993;12:532–533. doi: 10.1097/00006454-199306000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Bernstein SH, Stillerman M, Allerhand J. Demonstration of penicilin inhibition by pharyngeal microflora in patients treated for streptococcal pharyngitis. J Lab Clin Med. 1964;63:14–22. [PubMed] [Google Scholar]
- 28.Brook I. Failure of penicilin to eradicate Group A Beta-Hemolytic Streptococci tonsillitis: causes and management. J Otolaryngol. 2001;30:324–329. doi: 10.2310/7070.2001.19359. [DOI] [PubMed] [Google Scholar]