Abstract
A case report of rare occurrence of frontoethmoid mucopyocele with Intracranial and orbital extension with complete recovery after endoscopic surgery.
Keywords: Endoscopic marsupialization, Mucopyocele, Proptosis
Introduction
A mucocele is an epithelial lined, mucus containing sac completely filling the sinus and capable of extension all around. Any para nasal sinus can develop a mucocele but, frontal and ethmoid sinuses are most commonly affected followed by sphenoid and maxillary sinus. Expansion may take place over many years or occur rapidly when secondary infection produces a pyocele. Mucocele can encroach on orbit from all sinuses. We report an unusual case of 70 years. Male with frontoethmoid mucopyocele with orbital and intracranial extension managed successfully by endonasal endoscopic approach.
Case Report
A 70 year Male was referred to ophthalmology Department from Peripheral Hospital with complaints of gradually increasing swelling above and medial to left eye involving left upper eyelid and left frontal area since 2 years. Decrease in vision of left eye since 2 years, gradually progressive downward and lateral displacement of left eyeball for 2 months, Headache in left frontal region for 2 months, Nasal obstruction for 2 months and Occasional Pain in the swelling for 2 months. On local examination a Globular shape soft, cystic, mobile mass of size 8 × 7 × 6 cm displacing the left eyeball downward and laterally was present on left side (Fig. 1) with overlying skin free. Left eye examination showed restricted movement of eyeball in upward and medial direction with perception of light close to face only. Fundus Examination (Pre-op.) of Right eye was WNL while in Left eye there was nasal and superior blurring with temporal pallor, Multiple superficial flame shaped haemorrhage and exaggerated reflex with Edema.
Fig. 1.
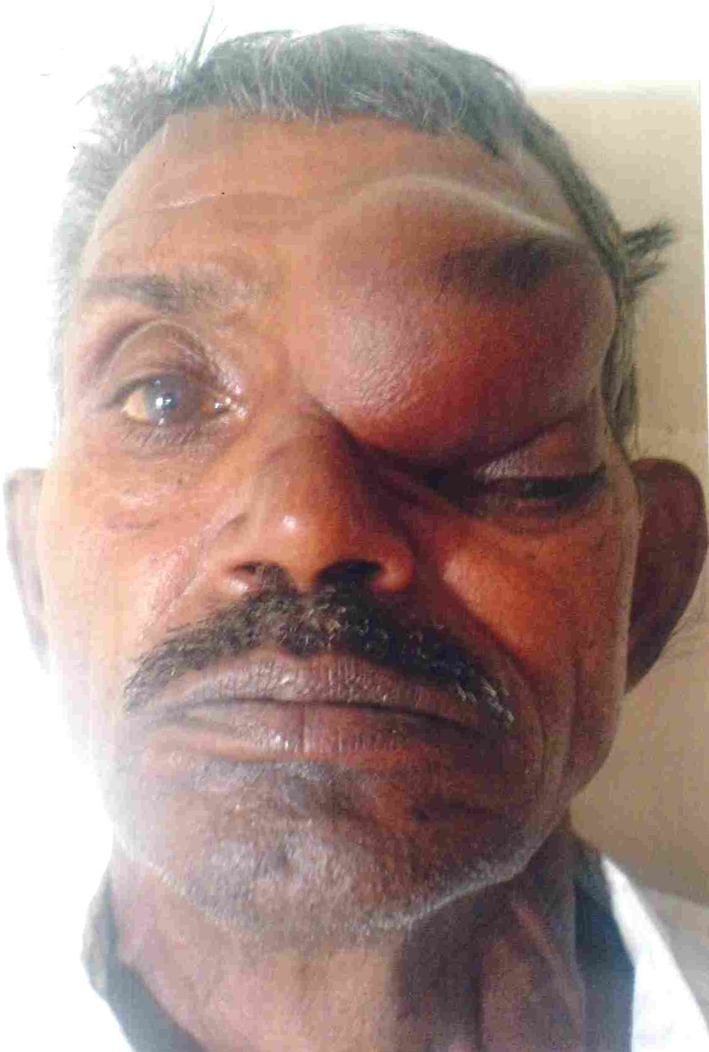
Clinical picture showing a large mucocele
CT scan PNS and Brain of patient (Fig. 2) showed large 6.7 × 6.2 × 5.9 cm destructive mass lesion in left orbit causing bony destruction extending superiorly in the frontal lobe and in the left ethmoid sinus with erosion of left lamina papyracea. Extension was seen also into contra lateral frontal sinus. Patient was then planned for surgical intervention by neuro-surgery department by open approach but, fortunately patient was sent to otorhinolaryngologist for expert opinion before neuro-surgical intervention. Finally, on basis of nasal endoscopy findings and CT scan we made diagnosis of frontoethmoid mucocele with orbital and intracranial extension. Endonasal endoscopic marsupialization of frontoethmoid mucocele was performed under Local Anaesthesia and thick purulent secretions sucked out. Swelling above lt. eye regressed immediately on the O.T. Table with in few minutes (Fig. 3). Post operatively systemic antibiotics (I/V cefotaxim 1 g/8 h, gentamicin 80 mg/12 h and Metrogyl 100 ml/8 h) and anti-inflammatory drugs were started. Post Operative nasal endoscopy day 2 (Fig. 4) showed presence of dural pulsation, orbital periosteum was exposed and henkiwikz sign was present. Subsequently patient was relieved of his headache and proptosis and visual acuity improved in affected eye.
Fig. 2.
CT Scan of the lesion
Fig. 3.

Postoperative profile of the patient
Fig. 4.

Endoscopic view postoperatively showing the exposed orbital perostium
Discussion
The majority of mucocele occur in age between 40 to 70 years. There is slight male preponderance overall but right and left sides are equally affected. The formation of mucocele is attributed to a combination of obstruction of affected sinus and inflammation [1]. Obstruction can be due previous surgery or trauma but, a significant proportion (36%) have no such factor. Expansion of the mucocele generally follows the route of least resistance that is into the orbit. So, the majority of patients of frontoethmoid mucocele, exhibit some degree of proptosis, lateral and inferior displacement of globe, diplopia, limited ocular motility in upward gaze, sometimes with a characteristic ‘egg shell’ cracking sensation due to thinned overlying bone. Conversion to a pyocele, with additional infection will cause rapid expansion, compromising vision [2]. Thus, majority of patients are initially referred to ophthalmic surgeon.
Mucocele or mucopyocele of the post ethmoid and sphenoid sinus cause retro-orbital headache, facial pain and diplopia, proptosis, ophthalmoplegia and visual loss. In severe case, intra cranial extension may produce meningitis and raised intra cranial pressure.
Plain sinus X-rays of a frontoethmoid mucocele show the classical features of an expanded Frontal sinus with loss of the scalloped margin and translucence and depression or erosion of supra orbital ridge. CT scans show an homogenous smooth walled mass, expanding the sinus, with thinning and loss of bone. There may also be evidence of new bone formation or sclerosis. CT with intravenous contrast characteristically shows ring enhancement in the presence of a pyocele.
Lateral sinus X-ray may show expansion of the sphenoid, with elevation or erosion of the floor of Pituitary Fossa. Sphenoid sinus and maxillary sinus mucocele are best seen on CT scan and distinguished from other pathology like acute and chronic Sinusitis, polyps, retention cysts, dermoids and cholesterol granuloma and range of benign and malignant neoplasm.
Until recently, the majority of patient with frontoethmoid mucocele were treated via an external modified Lynch–Howarth approach or radical Frontoethmoidectomy or the osteoplastic flap operation [3]. Now, mucocele can be approached endoscopically, which avoid external incision and associated morbidity and has distinct advantage over external frontoethmoidectomy [4].
The displacement of globe may take several months to resolve completely while bone remodeling occurs.
Conclusion
Frontoethmoid mucopyocele rarely can present with intracranial and orbital involvement because of close proximity of Frontoethmoid sinus to orbit and brain. So, accurate diagnosis and appropriate surgical intervention and a close collaboration between Otolaryngologist, Ophthalmologist and Neurosurgeon is crucial.
References
- 1.Kennedy DW, Josephson JS, Zinreich SJ, Mattox DE, Goldsmith MM. Endoscopic sinus surgery for mucoceles: a viable alternative. Laryngoscope. 1989;99:885–889. doi: 10.1288/00005537-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Canalis RF, Zajchuk JT, Jenkins HA. Ethmoidal mucocoeles. Arch Otolaryngol. 1978;104:286–291. doi: 10.1001/archotol.1978.00790050052012. [DOI] [PubMed] [Google Scholar]
- 3.Lund VJ. Anatomical considerations in the aetiology of fronto-ethmoidal mucocoeles. Rhinology. 1987;25:83–88. [PubMed] [Google Scholar]
- 4.Lund VJ, Rolfe M. Ophthalmic considerations in fronto-ethmoidal mucocoeles. J Laryngol Otol. 1989;103:667–669. doi: 10.1017/S0022215100109673. [DOI] [PubMed] [Google Scholar]



